White and Red lesions
The oral cavity is lined by oral mucosa which is composed of epithelium (stratified squamous epithelium) and lamina propria Submucosa is found beneath mucosal layer which is a relatively vascular connective tissue containing minor salivary gland in some areasOral mucosa is divided into:1. Masticatory mucosa: mostly located in gingiva and hard palate, it is paler in color than the other lining mucosa and it is firmly attached to the underlying tissue.2. Lining mucosa: most common sites are the buccal mucosa, floor of the mouth, ventral surface of the tongue. It is pinkish in colour due to reflection of the underlying vascular bed3. Specialized mucosa: located on the dorsum of the tongue (due to the presence of taste buds)The reddish colour of mucosa is due to the underlying vascular bed and semitransparent colorless epithelium, so any obstruction in this reflection may change colour of mucosa.
Why does oral mucosa appear white sometimes?1. Increased thickness of epithelium covering the mucosa with increased production of keratin (keratotic white lesions) ex.: lichen planus, leukoplakia, traumatic keratosis2. Imbibition of water by upper layers of mucosa .3. Tissue necrosis: This is characterized by formation of pseudomembrane composed of dead epithelium, body cells, food debris, microorganisms, and fibrin. Ex.: Thrush
Classification of white and red lesions (Memorize it before proceeding)A. Normal : leukoedema, fordyce’s granule, lineae albaB. Developmental: white spongy nevus, median rhomboid glossitisC. Infection: oral candidiasis, syphilis, measlesD. Traumatic: nicotine stomatitis, traumatic keratosis, papillary hyperplasiaE. Blood dyscrasias: anemia, Plummer Vinson syndromeF. Drugs: aspirin, vitamin A, drug reactionsG. Dermatological: lichen planus, lupus erythematosus, psoriasisH. Premalignant: leukoplakia, erythroleukoplakia, s.m fibrosisI. Miscellaneous: oral skin graft, geographic tongue, hairy tongue
A. Normal (Leukoedema\ Fordyce’s granules \Lineae Alba)1. Leukoedema: it is a normal anatomical variation discovered during routine oral examination. The mucosa appears milky, white and thin, which usually disappears upon stretching to distinguish it from other lesions.Dx. Clinical examination and histopathologyRx. Reassurance
Leukoedema
2. Fordyce’s granules: it is an ectopic sebaceous glands present in the buccal mucosa and lips, appears as collection of submucosal yellowish plaque or clumpy areaDx. Clinical examinationRx. Reassurance
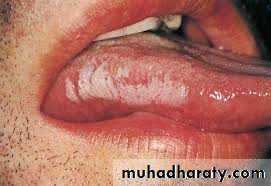
3. Lineae Alba: horizontal streaks on buccal mucosa at the level of occlusal plane, extend from the commissure of lips to the posterior teeth, associated with pressure, frictional irritation or secondary to trauma from facial surface of teeth (bruxism), usually bilateralDx. Clinical examinationRx. Treat underlying cause, prescribe keratolytic agent (retinal) which is a derivative of vitamin A: 0.01~0.025 mg (for skin 0.1 mg is used for acne)
Lineae Alba
B. Developmental (White spongy nevus and Median rhomboid glossitis)1. White spongy nevus: hereditary condition due autosomal dominant gene, characterized by white folds which is thickened with corrugated patches and irregular spongy texture. Starts from infancy to the adolescence, affects floor of the mouth and nasal mucosaDx. History, clinical examination and histopathologyRx. Reassurance
White spongy nevus
2. Median rhomboid glossitis: was formerly considered as developmental condition but recently they’ve found that some cases respond well to antifungal treatment, so it may also be considered as infection-caused lesion. This lesion is located anterior to the circumvallate papillae, appears as reddish area with smooth depapillated surface, usually asymptomatic but may cause burning sensation in some casesDx. Clinical examination + other investigation for candida (discussed later)Rx. Antifungal therapy, soothing agent for burning sensation
Median rhomboid glossitis
C. Infective lesions (Candidiasis\ Syphilis\ Measles)1. Candidiasis (candidosis): infection by Candida albicans, it is present in 30~50% of population as normal flora or weak pathogen, considered as opportunistic pathogen.Predisposing factors for candidiasis1. Xerostomia2. Diabetes mellitus3. Endocrine disorders4. Anemia (iron deficiency)5. Broad spectrum antibiotic administration6. Infancy (immature immune system)7. Old age (due to decrease immune function)8. Acidic saliva, due to carbohydrate rich food9. Decrease in immunity of body as in AIDS or chemotherapy
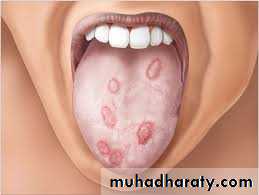
Classification (Burket’s)a. Acute pseudomembranous candidiasis (thrush): removable creamy white patch affecting buccal mucosa or soft palate. It is easily removed by scraping which may result in reddish area or pinpoint bleeding,Occur in infancy due to immature immune system and in old age due to decrease in immune system function. It is usually associated with burning sensationb. Acute atrophic candidiasis (antibiotic sour mouth): occur due to administration of broad spectrum antibiotic, redness of the oral mucosa and depapillation of tongue.c. Chronic hyperplastic candidiasis (candidal leukoplakia): it is a mixed red and white lesion (speckled) associated with severe epithelia dystrophy. So, it is premalignant.
d. Chronic atrophic candidiasis:1. Denture stomatitis: seen in patients wearing dentures at night, usually affecting maxillary arch.2. Angular cheilitis: characterized by lesions affecting corner of the mouth which appear as reddish cracked and inflamed area, associated with reduced vertical dimension of denture, causative microorganisms are: 20% Candida albicans, 20% Staphylococcus aureus or 60% mixed3. Median rhomboid glossitis (mentioned before)e. Chronic multifocal candidiasis: characterized by lesion affecting tongue (median rhomboid glossitis) and posterior part of palate with angular cheilitisf. Mucocutaneous candidiasis: this type is inherited type affecting skin, nail and m.m.
Dx. of candidiasis1. History and Clinical features2. Swab for gram stain and periodic acid Schiff to show candidal hyphae3. Culturing on Sabouraud dextrose agar4. Biopsy (candidal hypha at right angle to oral epithelium)Rx. for candidiasis1. Search for underlying local or systemic conditiona. Correct vertical dimension of the denture (for angular cheilitis)b. Reline ill-fitting denture and instruct patient not to wear it at night2. using antifungal drugs like (Nystatin , Ketoconazole, Itraconazole, Fluconazole, Amphotericin B).
Candidiasis
2. Syphilis: (bacterial infection caused by treponema pallidum) secondary syphilis is characterized by mucous patches which appear as superficial white to yellow ulcer (snail tract ulcer), seen on palate, tonsils, buccal mucosa, in addition to associated systemic manifestation such as generalized lymphadenopathy and maculopapular rash.Tertiary syphilis is characterized by:a. Gumma: swelling affecting palate followed by necrosis and destruction and perforation of the palate.b. Syphilitic leukoplakia of the tongue (premalignant)c. Atrophic glossitis: depapillation of tongue in addition to shrinkage due to endarteritis obliteransDx.a. History and clinical featuresb. Serum tests.
Syphilis
3. Measles or rubeola: acute contagious viral infection mostly affecting children, characterized by fever, lymphadenopathy, cough, nausea, photophobia, development of rash affecting head, hair line, back of the ear, chest, back and extremitiesIntraorally appears as greyish to white spot surrounded by red zone, mostly affecting buccal mucosa seen in 97% of cases called (Kopeck’s spots), treated by bed rest.
D. Traumatic white lesion:1. Traumatic keratosis: occur in an isolated area of oral mucosa, appears whitish and thickened, occur due to local irritation or an identifiable cause, such as: clasp, denture flange, sharp edge, orthodontic appliance, malposed teeth (upper and lower wisdom teeth) Treatment: remove the cause and follow up, biopsy should be taken if lesion persists
2. Nicotinic stomatitis (not premalignant): Localized to the palate in heavy smoker (cigarette, cigar and pipe)Early lesion appear reddish subsequently develops into whitish thickened fissured lesion affecting mainly the palate, sometimes local thickening around orifice of salivary gland with sometimes red spot at the center (Inflamed minor salivary gland), sometimes may stain brown due to tarDx.: clinical, historyTreatment: stop smoking and follow up
3. Papillary hyperplasia of palate: seen in denture (ill-fitting or rocky), usually symptomless, polypoid granulated erythematous elevationsDx: presence of irritant(denture)Treatment: remake denture and follow up, biopsy should be taken if lesion persists
E. Blood Dyscrasias1. Anemia: oral examination shows pallor in oral mucosa + atrophic glossitis (depapillation)2. Plummer Vinson syndrome (premalignant condition) (Paterson Brown Kelly syndrome, Sideropenic dysphagia): Affecting mid age female and is a triad of:a. Fe deficiency anemiab. Dysphagia due to post cricoid web (oral, pharyngeal and esophageal carcinoma may occur)c. GlossitisDx. Clinically (glossitis, burning, angular cheilitis, spoon shaped nails- and other symptoms of Fe deficiency anemia) Investigations : Barium swallow-shows esophageal web-Treatment: refer to physician to treat underlying cause
F. Drugs (Vit. A def, Aspirin, Drug reactions)1. Vitamin A deficiency: white lesion or leukoplakic lesion in oral cavity and other parts ( retina-Night blindness- and skin)Treatment: supplements, Found in vegetable (Carotene, found in carrot)2. Aspirin burn: chemical burn happens when aspirin comes accidentally in contact with mucobuccal fold and sulcus to relief pulpitis, periapical abscess and periosteitis.Dx. History of pain + using aspirin clinically: irregular pseudomembranous white lesion, painful, adjacent to offending area the entire cheek mucosa is affected
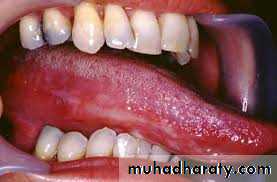
G. Dermatological (lichen planus, Psoriasis, LE)1. Lichen Planus: mucocutaneous disorder, affecting mouth and other parts of the bodyBoth oral and skin lesion might be seen together, oral may precede skin lesion or vice versaVarieties of lichen planus (10 varieties)a) Reticular..... as network lace like of elevated white lines on buccal mucosa bilaterally Chief complaint: roughness, brownish pig (pigmented l. planus)b) Erosive..... Either minor or major.. diffuse erosion with well demarcated white lines at periphery, painful, burning ... premalignantc) Desquamative gingivitis... diffuse desquamation, very painful, resist treatment
d) Papular.... aggregation of many papules within o. cavitye) Bullous.... represent acute phase of disease... may rupturef) Atrophic glossitis...... depapillated dorsum of the tongueg) Atrophic..... painful , chronic red lesionh) Leukoplakia-like.... appear as w. patchi) Annular... circle likej) Linear lesionEtiology of lichen planus :I. hyper sensitivity reaction,II. Immunological reaction, recently …is associated with lichen planus antigen,III. Hepatitis C
DX.: Clinical feature, HistopathologyTreatmentI. Reassurance in asymptomaticII. Topical corticosteroid (Kenalog in Orabase)III. Keratolytic agent: Tretinoin(retinoic acid)0.025 mg 1x2……. Also used for Acne 0.1 mgIV. In resistant cases... cyclosporine(cytotoxic)V. Cryotherapy or LASER
lichen planus
lichen planus
3. Lupus Erythematosus: Autoimmune ,three types (Discoid, sub-acute and SLE)a. Discoid: common form occurs in 3rd and 4th decades, characterized by:• Oral lesion: oral ulceration on erythematous base with white radiating lesion at periphery and is not well demarcated• Skin lesion: erythematous macule affecting malar region and bridge of the nose (Butterfly lesion) considered diagnostic for LEb. Subacute: mild form of lupus, involves legs & trunkc. Systemic LE: middle form, skin+ oral+ internal organs (joints, blood vessels, bone marrow)
Dx. of lupus :1- History,2-Clinical features (butterfly lesion)3-Biopsy: ( H&E )& Immunofluorescence (antibodies attached to basement membrane)Treatment: corticosteroid
Lupus Erythematosus
H. Premalignant (leukoplakia, erythroleukoplakia, s.m. fibrosis)1. Leukoplakia: White patch or plaque that cannot be characterized clinically or pathologically for any other diseaseClinical features: affecting middle and older aged people (majority in 40's)Predisposing factors1-Chemical and mechanical irritation2-Tobacco (all types) the main cause is smoking3-Alcohol4-Infection: chronic hyperplastic candidiasis, syphilis,5- Avitaminosis A&B6-Hormonal
Clinically: whitish or greyish small well circumscribed lesion on cheek mucosa and tongue (mainly), lip, palate and the floor of the mouth.
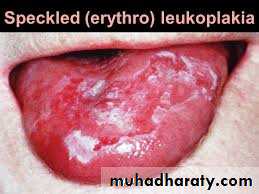
Varieties: homogenous, Nodular, Verrucous, Proliferativea. Homogenous (thick): Well defined white patch, localized or generalized more extensive slightly elevated fissured or corrugated on tongue.b. Nodular (speckled): Non homogenous mixed red and white lesion in which keratotic white patch or nodules are distributed over an erythematous background and is associated with high malignancy transformation ratec. Verrucous (verruciform): thick white lesion with papillary surfaced. Proliferative verrucous leukoplakia (P.V.L) extensive papillary white plaque involving multiple mucosal sites, may transform into Squamous cell carcinoma or verrucous carcinoma or severe dysplasia.If dysplastic changes involve all layers of epithelium called ca in situ
Dx. Clinical, biopsyTreatment :1-remove any local factor and underlying systemic condition2-Surgical excision of small lesion (dx and treatment)3-Keratolytic agent4-Gingival leukoplakia: by cryotherapy, LASER*NO TREATMENT SHOULD BE GIVEN BEFOR BIOPSY
Leukoplakia
2. Erythro leukoplakiaBright red plaque or patch that cannot be diagnosed clinically and pathologically as any other condition, sometime slightly depressed so called (erythroplasia) *Red lesions are due to allergy or infectionUncommon in mouth, but caries highest risk of malignant transformation, sometimes lesion is already malignant on first biopsyClinical types: 1. Homogenous 2. Granular (speckled) 3. Leukoplakia interspersed with patches of ErythroplakiaDx:Clinical: Occur in old man 6th and 7th decade of lifeSites: floor of the mouth, ventrum of the tongue, soft palate, tonsillar regionHistopathological study shows sever epithelial dysplasia, carcinoma in situ and squamous cell carcinomaTREATMENT depends on biopsy
Erythro leukoplakia
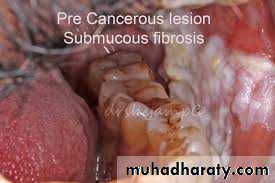
3. Submucosal fibrosis: Slowly progressive chronic fibrotic disease of oral cavity and oropharyngeal region, characterized by: fibroelastic changes, inflammation of mucosa, progressive inability to open mouth, swallow, or speak*Is a premalignant oral lesionEtiology: spicy food, betel nuts.Dx.1. History (search for abnormal dietary habit)2. Clinically: burning, Increase or decrease salivation, vascular lesion, submucosal whitish opaque band, limitation in mouth opening3. Biopsy