Chest pain and ST elevation
BMJ 27 June 2012د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
A 53 year old Vietnamese man developed chest pain at rest and dialled the emergency services. The ambulance service identified ST elevation on 12 lead electrocardiography (ECG) and according to local protocol brought him direct to our cardiac
centre with a suspected ST elevation myocardial infarction. On arrival he reported a three hour history of central chest pain without radiation or associated symptoms. He was a current smoker but had no other risk factors for coronary artery disease.
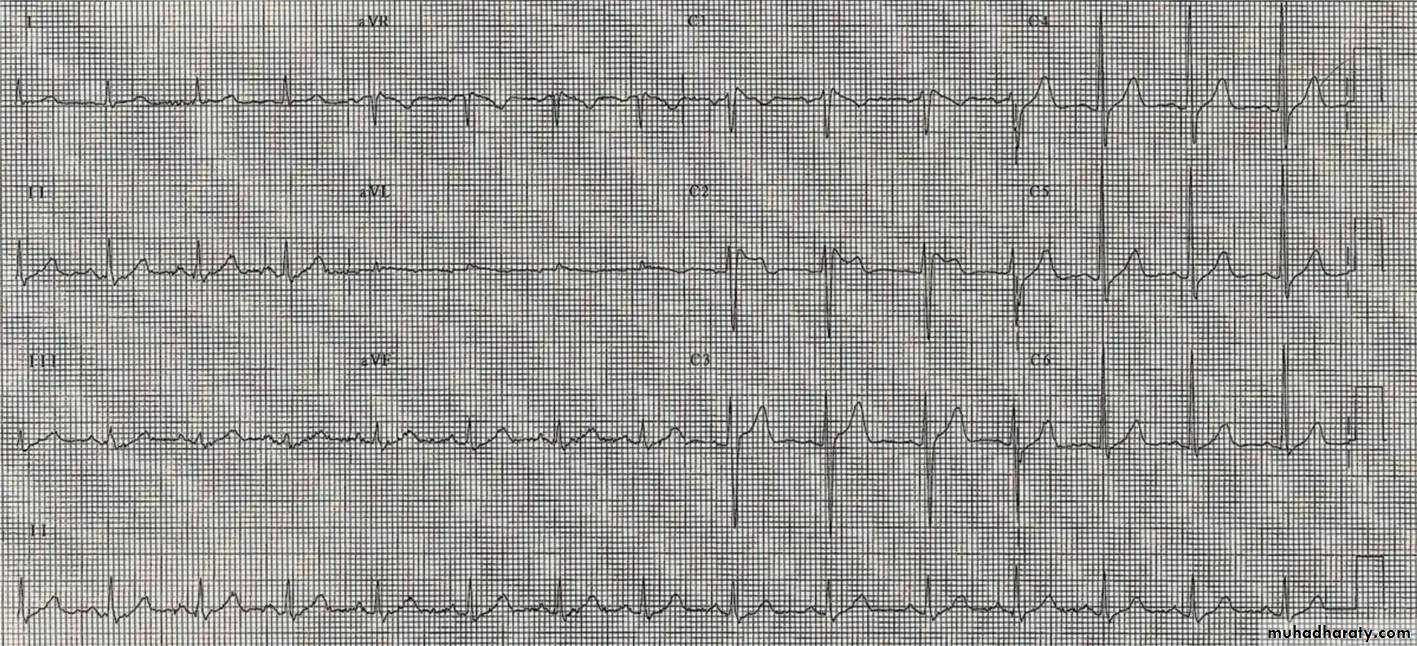
Examination was unremarkable and an ECG was performed on arrival. In lead V1 there was 2 mm of coved J point elevation, with an inverted T wave. In V2 there was 4 mm of J point elevation, with a saddle shaped ST segment and an upright T wave. In V3 the J point, ST segment, and T wave were within
normal limits. He underwent immediate coronary angiography,which showed mild atheroma in the left anterior descending artery, but no obstructive lesions, and transthoracic echocardiography showed normal cardiac structure with good biventricular function.
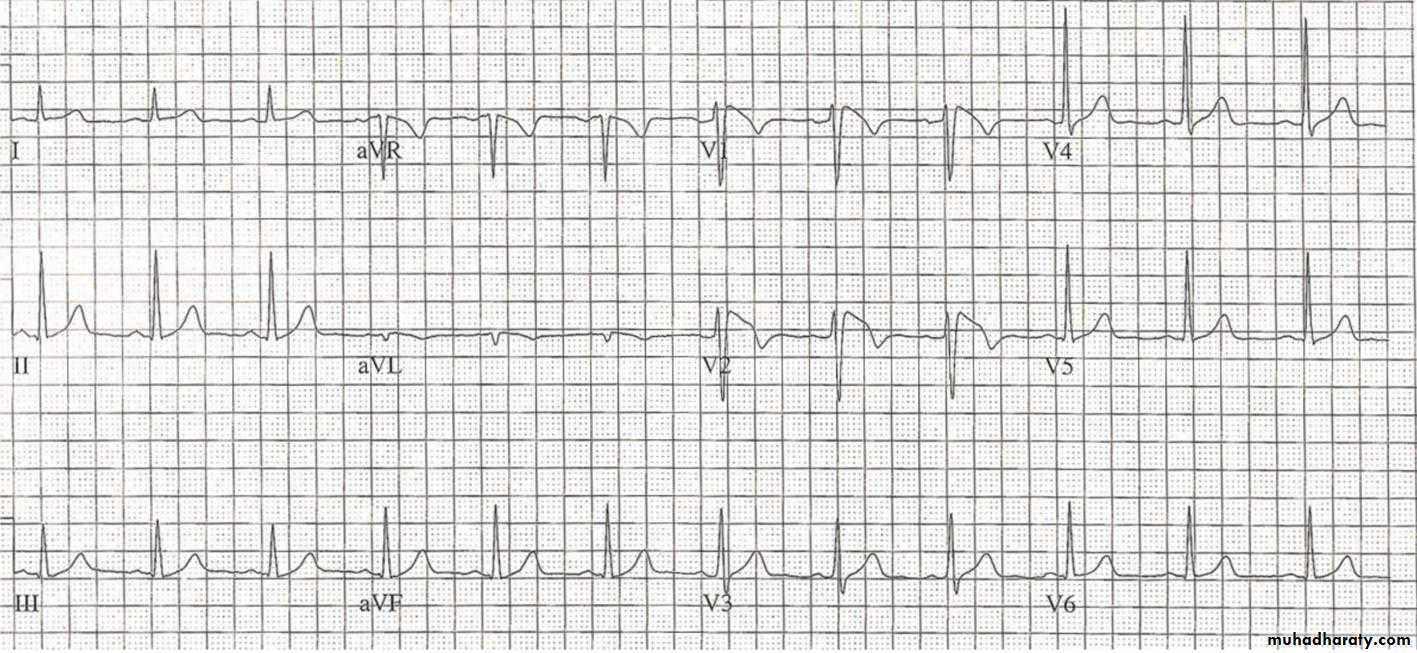
Overnight he developed a productive cough associated with a fever. Serial ECGs were recorded while he was febrile and
showed 3 mm of coved J point elevation in lead V1 and 5 mm of coved J point elevation in V2, with associated T wave inversion.
On further questioning he admitted to a history of well tolerated intermittent palpitations of up to an hour’s duration. His father had died suddenly and unexpectedly by falling from a bridge, but otherwise his family history was unremarkable. He was
started on oral antibiotics and monitored in hospital until his fever had resolved. A loop recorder was subsequently implanted to investigate his palpitations. He was also advised to stop smoking and treated with aspirin and statins for coronary atheroma.
Questions
1 What are the causes of ST elevation?2 What is the clinical diagnosis?
3 What specific advice would you give?
Answers
1 What are the causes of ST elevation?Short answer
The most important immediate cause of ST elevation is acute myocardial infarction. Other causes include pericarditis, early repolarisation, left bundle branch block, left ventricular hypertrophy, coronary spasm, hyperkalaemia, and Brugada syndrome.
Long answer
When evaluating patients with chest pain the most important immediate cause of ST elevation to consider is ST elevation myocardial infarction (STEMI). The ST segments are typically convex and are often associated with reciprocal changes elsewhere. Concave ST elevation is a normal finding in many people, especially young men. Pericarditis can cause diffuse non-specific ST segment abnormalities but classically causeswidespread saddle shaped elevation and may be association with depression of the PR interval.
Early repolarisation describes elevation of the J point (the intersect between the QRS complex
and the ST segment) and may be either notched or slurred. Early repolarisation is common and considered a normal variant, although it is more common in people who have survived a
cardiac arrest. Left bundle branch block, left ventricular hypertrophy (fixed), and coronary spasm (transient) may also be associated with ST elevation. Finally Brugada syndrome is an inherited condition characterised by J point ST elevation and is associated with a risk of syncope and sudden death.
2 What is the clinical diagnosis?
Short answer
The ECG appearances on presentation are non-specific (fig 1), but the subsequent ECG pattern of coved ST elevation and T wave inversion in the right precordial leads is typical of a type 1 Brugada pattern ECG (fig 2).
Long answer
Brugada syndrome is an inherited arrhythmogenic disorder characterised by a typical ECG pattern of incomplete right bundle branch block and ST elevation associated with an increased risk of ventricular arrhythmias and sudden cardiac death. It is more common in South East Asia and more commonin males. In about 30% of cases a pathogenic mutation may be identified in the sodium channel gene (SCN5A) on chromosome.
The diagnostic hallmark of the condition is the so called type 1 ECG pattern of J point elevation of 2 mm or more, and a coved ST segment in more than one precordial lead (V1-V3), but technically it requires either symptoms (such as syncope, nocturnal agonal respiration, or previous cardiac arrest), a type
1 ECG in a family member, or a family history of sudden death to diagnose the syndrome.
The ECG pattern of ST elevation is highly variable, fluctuating between diagnostic and non-diagnostic patterns. Other patterns of ST elevation are
non-specific and non-diagnostic. A type 2 pattern is
characterised by 2 mm or more saddleback ST elevation, atrough of 1 mm or more, and either a positive or biphasic T wave. A type 3 pattern is characterised by either saddleback or coved ST elevation of less than 1 mm. Although a type 2 ortype 3 pattern may be suggestive of Brugada syndrome, only atype 1 pattern is specific for the diagnosis.
3 What specific advice would you give?
Short answerPatients with Brugada syndrome should be provided with a list of drugs to avoid and be advised to take antipyretic agents in the event of a fever. Family screening should also be
recommended.
Long answer
Many drugs—including anaesthetics, tricyclic antidepressants,and class 1c antiarrhythmic drugs—may exacerbate J point elevation and increase the risk of arrhythmia.2 People with
Brugada syndrome should be counselled about these drugs and provided with a list of drugs to avoid (a list can be downloaded from ww.brugadadrugs.org). Fever may have a similar effect, unmasking diagnostic ECG changes and precipitating ventricular arrhythmias in adults and children; such ventricular arrhythmias can be mistaken for febrile convulsions in children.
Patients should be advised to take regular antipyretic agents such as paracetamol or ibuprofen in the event of a febrile illness, and they may require admission for ECG monitoring if the fever persists. Electrolyte disturbances, such as hypokalaemia (as aresult of diuretics and diarrhoea, for example), must be avoided because they can exacerbate the phenotype and increase the risk of ventricular arrhythmias.
Currently, Brugada syndrome is considered to be a monogenic condition with an autosomal dominant pattern of inheritance.
First degree relatives should be invited for clinical screening with ECG or a provocation test with a sodium channel blocker such as ajmaline, which is a sensitive diagnostic test for people who do not manifest a type 1 Brugada pattern ECG spontaneously.
Long term management is aimed at the identification of patients at risk of ventricular arrhythmias and sudden cardiac death, as well as avoidance of precipitating agents and prolonged fever.
Although implantable cardioverter defibrillators are a class 1 indication those with syncope and survivors of cardiac arrest, their use in asymptomatic patients with inducible arrhythmias during programmed ventricular stimulation remains controversial. Atrial fibrillation is also prevalent in patients with Brugada syndrome.
Patient outcome
The patient remains well two years later. No arrhythmias have been detected despite ongoing palpitations. Cascade screening has been undertaken to identify other family members potentially at risk.Electrocardiogram on presentation
Electrocardiogram with maximal J point elevation