د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Defining myocardial infarction: awork in progress
Heart 2008Few disorders have as broad implications for public
health and cardiovascular medicine as myocardialinfarction. Herrick’s first description in living man
in 1912 was populated by a combination of clinical
symptoms and electrocardiographic changes.
In this prescient description of six cases, the diagnosis
was confirmed at autopsy in one who died 3 days
after his clinical diagnosis.
Interestingly, a period of relative quiescence ensued after Herrick’s original description.
In 1959, the World Health Organization contributed to the definition of myocardial infarction with the admonition that it
consist of a combination of two of the following
three characteristics:
• Typical symptoms.
• A rise in cardiac enzymes
• An evolutionary ECG pattern which involved
Q wave development.
Subsequently, major interest and animated debate emerged concerning the frequency, causes,
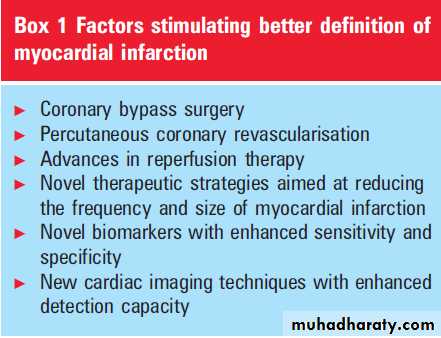
preferred treatment, and prognosis of acute myocardial infarction.A convergence of factors, including those listed in box 1, helped to galvanise interest in better defining myocardial infarction with a view to both greater sensitivity and specificity.
Given this global significance of myocardial
infarction and these multifactorial factors, it wasdecided that the European Society of Cardiology
and American College of Cardiology should convene a consensus conference in July 1999 to
examine potential new definitions of myocardial
infarction.
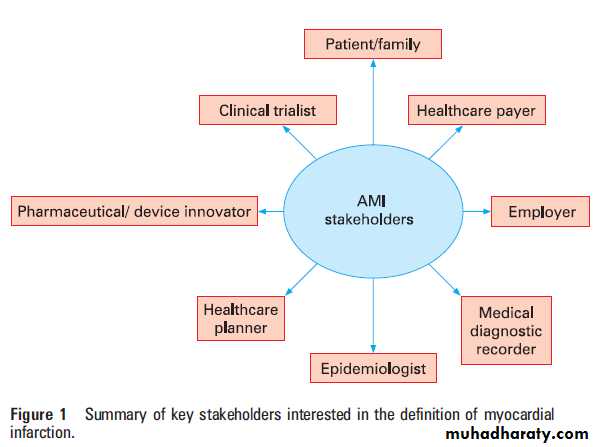
The International Task Force set upon its work recognising that any change in the definition of such an important diagnostic entity might have profound and different implications depending on a particular interest of the individual
or group.
Figure 1 summarises some of the
stakeholders and constituencies so affected.
The key elements of the 2000 consensus document emerging from a rich multidisciplinary effort were, in brief:
The incorporation of cardiac troponins (T or I) as the preferred biomarker of myocardial necrosis and the assertion that if maximal concentration of troponin T or I exceeded the decision limits (99th centile of values for reference control group) on at least one occasion during the first 24 h after clinical presentation.
This would constitute sufficient evidence—in conjunction with either symptoms, ECG changes (Q wave development or ST depression or elevation), or coronary intervention with angioplasty or bypass surgery—to warrant the diagnosis of myocardial infarction.
The recognition of the need for defining myocardial
infarction in the specific clinical settings
of coronary angioplasty or bypass surgery.
The 2000 consensus document acknowledged that controversy existed over what threshold should be used to identify myocardial infarction, particularly when percutaneous coronary intervention or coronary bypass surgery were employed in clinical trials.
However, it opined that any increase of cardiac biomarkers in the context of such procedures had prognostic implications, notwithstanding the acceptance that the early hazard from revascularisation
might constitute a legitimate risk given the long term benefit that could be anticipated in appropriately selected patients.
It was also appreciated that systematic use of cardiac troponins in the diagnosis of myocardial infarction would transpose a substantial proportion (subsequently estimated to be approximately 30%) of those patients previously diagnosed with unstable angina into the non-ST elevation acute myocardial infarction category.
That said, this development would be expected to result in not only enhanced estimation of prognosis but also more appropriate application of evidence based treatments with aresultant enhancement in patient outcomes.
Moreover, the enhanced specificity of cardiac
troponins would be expected to reduce the likelihood of false positive diagnoses of myocardial
infarction, with the potential of either avoidance of
unnecessary hospital admission or reduced length
of stay with resulting additional medical expenses.
The 2000 consensus document generated substantial
interest, discussion, and controversy,
especially within the epidemiologic community.
In particular there were concerns about the
adequacy of the definition relative to longitudinal
epidemiologic observations and the failure to
address the problem of sudden out-of-hospital
cardiac death.
Whereas this is usually attributable to ischaemic heart disease in the western world, it is noteworthy that stroke is assumed to be the cause in Japan.
As expected, over the 7 years subsequent to the initial report, enhanced diagnostic sensitivity and new confidence in the role of novel myocardial imaging techniques unfolded,prompting a reconvening of a new consensus task force.
This time it met under the auspices of the
European Society of Cardiology, the American
College of Cardiology, the American Heart
Association, and the World Heart Federation.
The task force was ably chaired by Drs Thygesen,
Alpert, and White and organised into severalgroups including ECG imaging, clinical investigation,
global perspective, and implementation.
After a secondary review conducted by international experts, the new document was approved by the sponsoring organisations.
The 2000 and 2007 definitions are provided in table 1 in order to see the alterations that have
occurred.
It should be noted that whereas myocardial necrosis remains reportable for any rise in biomarker
above the 99th centile, when this occurs in the
context of PCI or CABG a threefold rise in biomarker with PCI and a fivefold rise with CABG now represents the agreed upon definition of periprocedural myocardial infarction.
A new element in the definition relates to the use of
myocardial imaging to identify the new loss ofviable myocardium or new regional wall motion
abnormality. This addition relates not only to
enhanced quantification in imaging methodology,
with previously established techniques such as
echocardiography and radionuclide imaging, but
also the advent of magnetic resonance imaging and
x ray computed tomography.
Table 1 Definition of myocardial infarction
Criteria for acute myocardial infarction (2007)The term ‘‘myocardial infarction’’ should be used when there is evidence of myocardial necrosis in a clinical setting consistent with myocardial ischaemia. Under these conditions any
one of the following criteria meets the diagnosis for myocardial infarction:
1. Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99th centile of the upper reference limit (URL) together with evidence of myocardial ischaemia with at least one of the following:
(a) Symptoms of ischaemia
(b) ECG changes indicative of new ischaemia (new ST–T changes or new (LBBB)
(c) Development of pathological Q waves in the ECG
(d) Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
2. Sudden, unexpected cardiac death, involving cardiac arrest, often with symptoms suggestive of myocardial ischaemia, and accompanied by presumably new ST elevation, or new LBBB, and/or evidence of fresh thrombus by coronary angiography and/or at autopsy, but death occurring before blood samples could be obtained, or at a time before the appearance of cardiac biomarkers in the blood.
3. For percutaneous coronary interventions (PCI) in patients with normal baseline troponin values, evaluations of cardiac biomarkers above the 99th centile URL are indicative of periprocedural myocardial necrosis.
By convention, increases of biomarkers greater than
99th centile URL have been designated as defining PCI related myocardial infarction.
A subtype related to a documented stent thrombosis is recognised
4. For coronary artery bypass grafting (CABG) in patients with normal baseline troponin of
periprocedural myocardial necrosis. By convention, increases of biomarkers greater than 99th centile URL plus either new pathological Q waves or new LBBB, or angiographically documented new graft or native coronary artery occlusion, or imaging evidence of new loss of viable myocardium, have been designated as defining CABG related myocardial infarction5. Pathological findings of an acute myocardial infarction
Criteria for acute, evolving or recent myocardial infarction
Either one of the following criteria satisfies the diagnosis for an acute, evolving orrecent myocardial infarction:
1. Typical rise and gradual fall (troponin) or more rapid rise and fall (CK-MB) of
biochemical markers of myocardial necrosis with at least one of the following:
(a) Ischaemic symptoms
(b) Development of pathologic Q waves on the ECG
(c) ECG changes indicative of ischaemia (ST segment elevation or depression) or
(d) Coronary artery intervention (for example, coronary angioplasty)
2. Pathologic findings of an acute myocardial infarction
Definition of myocardial infarction (2000)
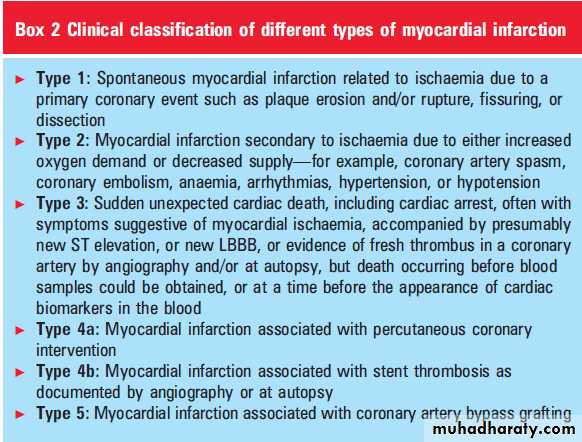
Another major addition to the new definition is
an accompanying clinical classification of thedifferent types of myocardial infarction (box 2).
Importantly, this classification recognises various
types of myocardial infarctions, highlighting
those naturally occurring myocardial infarctions
(so called ‘‘wild type’’ events) resulting from a
primary spontaneous coronary vascular event.
Distinguishing this so called type 1 infarction from
those that occur secondary to clinical syndromes,
such as severe hypotension or major increases in
myocardial oxygen demand, is encouraged. The
issue of sudden unexpected out-of-hospital cardiac
death has now provided a separate type 3 category.
Finally, the clinical classification defines myocardial
infarctions occurring in association withcoronary revascularisation: these consist of coronary
artery bypass grafting, percutaneous coronary
intervention, and an important new category—
infarction associated with the catastrophic occurrence of coronary stent thrombosis.
One classification of myocardial infarction not
included in the new document is that of abortedmyocardial infarction. In approximately 10% of
patients treated with fibrinolytic therapy there is a
failure to develop a rise in creatine kinase-MB (CKMB),
and in approximately 25% of patients treated
within 1 h of symptom onset not only is there
minimal evidence of myocardial necrosis but there
is complete ST resolution without Q wave development.
This entity may deserve broader recognition in the future and even inclusion as an end point in clinical trials of patients with ST elevation acute coronary syndrome, given declining mortality
rates. In the course of studying this entity, it is also clear that a number of patients with apparent acute myocardial infarction—that is, the clinical syndrome and an index ECG consistent with the diagnosis—do not ultimately unfold the picture of infarction and may be considered as a masquerading myocardial infarction. This occurs in a small
(2%) subset of patients treated with fibrinolysis
and it is important to recognise since they are
expected to have no benefit but yet be exposed to
the risks of this therapeutic intervention.
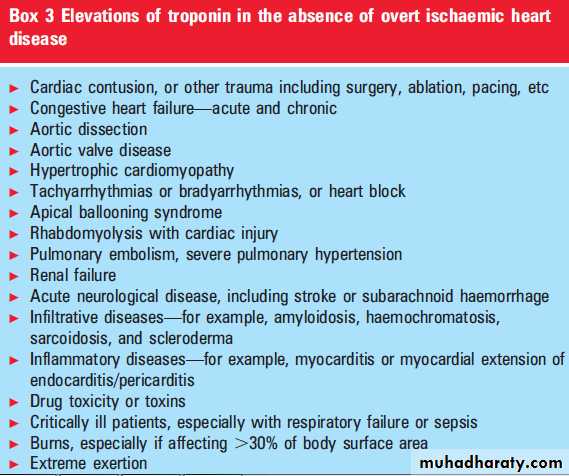
Contemporary cardiovascular practitioners are
increasingly alert to the imposition on their workloadassociated with enhanced biomarker sensitivity—
in particular, the finding of elevated cardiac
troponins discovered in the absence of a meaningful
clinical context or electrocardiographic
pattern suggestive of myocardial infarction.
They will welcome the new report’s excellent summary
of the circumstances where myocardial necrosis
may occur in the absence of myocardial infarction (box 3).
The pattern of a typical rise and fall in sequential
biomarker measures amid the clinical setting andconcomitant electrocardiographic evolutionary
changes remain key differentiating points. Since
reinfarction is a common complication of myocardial
infarction and an increasingly important
metric within clinical trials, the new document adds to the previous recommendation around CKMB measurements to include cardiac troponin and suggests that a 20% rise in the previously established value be applied to qualify for this diagnosis.
The key role that both myocardial infarction and reinfarction play in clinical trials of novel therapies received considerable attention by the clinical investigation group of the task force. Hence, a clear recommendation emerged to discourage
heterogeny around clinical trial definitions
and endorse the concept that the same decision
limit for each biomarker be used, with a clear
preference for cardiac troponin T or I as opposed to
additional CK-MB or other biomarkers.
Since both the presence of myocardial infarction and the extent of myocardial necrosis are relevant end
points, uniform presentation of such data according
to multiples of the 99th centile of the upper limit of normal is recommended to enable comparisons
of myocardial infarction occurrence across
differing clinical trials. Although the new definition of myocardial infarction is expected to have important public policy as well as other broad implications with its implementation, it was also recognised that challenges will exist concerning the availability of cardiac troponins and the application of these definitions in developing countries.
Cultural, financial, structural, and organisational issues within differing countries around the world require appropriate attention so that the gap between therapeutic and diagnostic advances in acute ischaemic heart disease can be appropriately
addressed. Finally, as was the case with the initial
2000 definition, the joint task force is cognisant
that future scientific advances guarantee a need for
future refinement and revisiting of the definition of
myocardial infarction.