Hypotension
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
Blood pressure is the force of the blood pushing against the walls of the arteries. The word hypotension is a hybrid of the Greek " Greek "hypo" meaning "under" and the Latin "tensio" meaning "to stretch." In French, "la tension" is "the blood pressure.
Hypotension is abnormally low blood pressure lower than 90/60 mmHg.
you need to have only one number in the low range for your blood pressure to be considered lower than normal.
What Is Hypotension?
Some people have low blood pressure all the time. They have no signs or symptoms and their low readings are normal for them.
In other people, blood pressure drops below normal because of some event or medical condition.
Hypotension is a medical concern only if it causes signs and/or symptoms such as dizziness, fainting, or, in extreme cases, shock
MBP = DBP + (SBP - DBP)/3
blood pressure isn't static.
It can vary considerably in a short amount of time sometimes from one heartbeat to the next, depending on body position, breathing rhythm, stress level, physical condition, medications you take, what you eat and drink, and even time of day. Blood pressure is usually lowest at night and rises sharply on waking. The heart is the prime mover of the circulatory system; with each beat it launches your blood on a journey through 60,000 miles of arteries, veins and capillaries, ultimately circulating about 2,000 gallons of blood each day.
Other Names for Hypotension
Low blood pressureOrthostatic hypotension
Postprandial hypotension
Postural hypotension
Neurally mediated hypotension
Neurogenic orthostatic hypotension
Shock
Types of Hypotension
• chronic asymptomatic hypotension,• happens in people who always have low blood pressure. They have no symptoms and need no treatment. Their low blood pressure is normal for them.
• Other types of hypotension happen only sometimes, when blood pressure suddenly drops too low. symptoms and effects can be mild or severe.
• The three main types of this kind of hypotension are
• orthostatic hypotension,
• neurally mediated hypotension (NMH),
• severe hypotension associated with shock
Orthostatic Hypotension
Orthostatic hypotension is low blood pressure that occurs upon standing up from a sitting or lying down position. if a person changes from a lying position to standing, he or she will lose about 700 ml of blood from the thorax.
It can cause a person to feel dizzy, lightheaded or even to faint It occurs when the body is not able to adjust blood pressure and blood flow fast enough for the change in position.
A fall in systolic blood pressure of at least 20 mm Hg or in diastolic blood pressure of at least 10 mm Hg within 3 minutes after standing, or a head-up tilt on a tilt table is a classic manifestation of sympathetic vasoconstrictor (autonomic) failure is diagnostic of orthostatic hypotension.
In many (but not all) cases, there is no compensatory increase in the heart rate, despite hypotension; with milder autonomic failure, the heart rate may increase, but not to a rate sufficient to maintain blood pressure. A variant of orthostatic hypotension is delayed orthostatic hypotension, which occurs after 3 minutes of standing; this condition may represent a mild or early form of sympathetic adrenergic dysfunction .
In some cases, orthostatic hypotension occurs within 15 seconds of standing (so-called initial orthostatic hypotension); this may represent a transient mismatch between cardiac output and peripheral vascular resistance rather than autonomic failure.
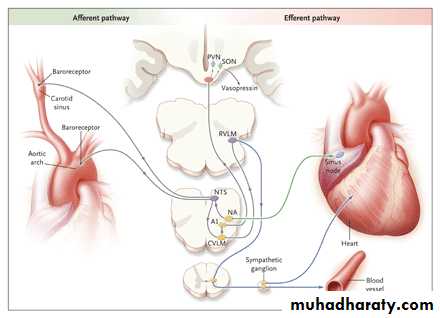
Standing results in pooling of 500 to 1000 ml of blood in the lower extremities and splanchnic circulation. There is a decrease in venous return to the heart and reduced ventricular filling, resulting in diminished cardiac output and blood pressure. These hemodynamic changes provoke a compensatory reflex response, initiated by the baroreceptors in the carotid sinus and aortic arch, that results in increased sympathetic outflow and decreased vagal-nerve activity (Figure 1). This reflex increases peripheral resistance, venous return to the heart, and cardiac output, thereby limiting the fall in blood pressure. If this response fails, orthostatic hypotension and cerebral hypoperfusion occur.
The Baroreflex.
A decrease in arterial pressure unloads the baroreceptors — the terminals of afferent fibers of the glossopharyngeal and vagus nerves that are situated in the carotid sinus and aortic arch. This leads to a reduction in the afferent impulses that are relayed from these mechanoreceptors through the glossopharyngeal and vagus nerves to the nucleus of the tractus solitarius (NTS) in the dorsomedial medulla.The reduced baroreceptor afferent activity produces a decrease in vagal nerve input to the sinus node that is mediated by the neuroanatomical connections of the NTS to the nucleus ambiguus (NA). There is an increase in sympathetic efferent activity that is mediated by the NTS projections to the caudal ventrolateral medulla (CVLM) (an excitatory pathway) and from there to the rostral ventrolateral medulla (RVLM) (an inhibitory pathway).
The activation of RVLM presympathetic neurons in response to hypotension is thus predominantly due to disinhibition. In response to a sustained fall in blood pressure, vasopressin release is mediated by projections from the A1 noradrenergic cell group in the ventrolateral medulla. This projection activates vasopressin-synthesizing neurons in the magnocellular portion of the paraventricular nucleus (PVN) and the supraoptic nucleus (SON) of the hypothalamus. Blue denotes sympathetic neurons and green parasympathetic neurons.
Characteristic symptoms of orthostatic hypotension include light-headedness, dizziness, presyncope, and syncope in response to sudden postural change. However, symptoms may be absent or nonspecific, such as generalized weakness, fatigue, nausea, cognitive slowing, leg buckling, or headache. Visual blurring may occur, probably because of retinal or occipital-lobe ischemia.
Neck pain may occur, typically in the suboccipital, posterior cervical, and shoulder region (called the coat-hanger headache), which is most likely due to ischemia in the trapezius and neck muscles.
Patients may report orthostatic dyspnea (thought to reflect ventilation–perfusion mismatch due to inadequate perfusion of ventilated lung apexes) or angina attributed to impaired myocardial perfusion even in patients with normal coronary arteries.
One or more of these nonspecific symptoms may be the presenting or only symptom of orthostatic hypotension. Symptoms may be exacerbated by exertion, prolonged standing, increased ambient temperature, or eating.
Supine hypertension is common in patients with orthostatic hypotension, affecting more than 50% of patients in some series. Orthostatic hypotension may occur after therapy for hypertension, and supine hypertension may follow treatment of orthostatic hypotension. In other cases, however, the association of the two conditions is unrelated to therapy and may be explained in part by baroreflex dysfunction in the presence of residual sympathetic outflow, particularly in patients with central autonomic degeneration.
Orthostatic hypotension increases in prevalence with age; aging is associated with reduced baroreflex responsiveness, decreased cardiac compliance, and attenuation of the vestibulosympathetic reflex. Orthostatic hypotension is more common in elderly people living in care facilities (54 to 68%) than in those living in the community6%, an observation most likely explained by the greater prevalence of predisposing neurologic disorders, physiological impairment, and medication use among people living in care facilities.
Postprandial hypotension occurs in up to one third of older people but virtually never occurs in younger people. It is more likely to occur in people who have high blood pressure or disorders that impair the brain centers controlling the autonomic nervous system (which regulates internal body processes). Examples of such disorders are Parkinson's disease, multiple system atrophy (Shy-Drager syndrome), and diabetes.
Pharmacological treatment of orthostatic hypotension is often limited because of troublesome supine hypertension.
treatment using acetylcholinesterase inhibition, based on the theory that enhanced sympathetic ganglion transmission increases systemic resistance in proportion to orthostatic needs. Acetylcholinesterase inhibition appears effective in the treatment of neurogenic orthostatic hypotension.
Orthostatic symptoms and orthostatic blood pressure are improved, with only modest effects in the supine position. This novel approach may form an alternative or supplemental tool in the treatment of orthostatic hypotension, specially for patients with a high supine blood pressure. In most patients, orthostatic hypotension is of neurogenic origin, resulting from impaired cardiovascular adrenergic function. The lesion can be postganglionic, as in pure autonomic failure and the autonomic neuropathies, or preganglionic, as in multiple system atrophy.
Orthostatic hypotension can occur in all age groups, but it is more common in older adults, especially those who are frail or in poor health.
Orthostatic hypotension can be a symptom of other medical conditions, and treatment generally focuses on treating the underlying condition(s). Some people can have orthostatic hypotension but also have high blood pressure when lying down.
A form of orthostatic hypotension called postprandial hypotension is a sudden drop in blood pressure after a meal. Postprandial hypotension most commonly affects older adults. It also is more likely to affect those with high blood pressure or diseases such as Parkinson disease.
Neurally Mediated Hypotension
standing for a long time. faces an unpleasant,upsetting, or frightening situation affects children
and young adults more often than other age
groups.
Children often outgrow this form of hypotension.
A person may feel dizzy, faint, or sick to the
stomach as a result.
Vasovagal faints
are often associated with prolonged standing with resultant pooling of venous blood with reduced venous return to the heart. When due to pain, emotional stress or site of blood, there is central reflex activation. Affects all age groups varying from infrequent attacks with an obvious trigger to frequent episodes with no apparent cause.Consciousness returns relatively quickly. May be brief period of sweating and pre-syncope symptoms before collapse.Diagnosis is confirmed by tilt-table testing.Postprandial hypotension
This is even more common than postural hypotension (30-40% elderly patients in residential homes) and mainly occurs in the elderly and those with autonomic neuropathy.Cause is unclear but is associated with high carbohydrate meals.Defined as fall in BP 20 mmHg 15 to 90 minutes after meals .Symptoms are same as those for postural hypotension.Severe Hypotension Associated With Shock
Shock is a life-threatening condition in whichblood pressure drops so low that the brain, kidneys,
and other vital organs can’t get enough blood to work
properly. It is different from the other forms of
hypotension because blood pressure drops
much lower, and it is life threatening if not
treated immediately.
There are many causes of shock, including
• major loss of blood,
• certain severe types of infection,
• severe burns,
• severe allergic reactions
• poisoning.
What Causes Hypotension
• Orthostatic Hypotension
• A-Dehydration
• is the most common cause. occurs when the body
• loses more water than it takes in. People can
• become dehydrated because of:
• Not drinking enough fluids
• Fever
• Vomiting
• Severe diarrhea
• Excessive sweating from strenuous exercise
• B-Some medicines used to treat high blood pressure and heart disease can make it more likely that a person will develop orthostatic hypotension. These medicines include:
• Diuretics
• Calcium channel blockers
• Angiotensin-converting enzyme (ACE) inhibitors
• Angiotensin II receptor blockers
• Nitrates
• narcotics
• Beta blockers
• Also, medicines used to treat certain other medical conditions, such as anxiety, depression, erectile dysfunction, and Parkinson disease, can make it more likely that a person will develop orthostatic hypotension.
• Other substances that can contribute to orthostatic hypotension include alcohol, barbiturates, and some prescription and over-the-counter medicines, when taken in combination with high blood pressure medicines.
• sildenafil (Viagra), particularly in combination with nitroglycerine;
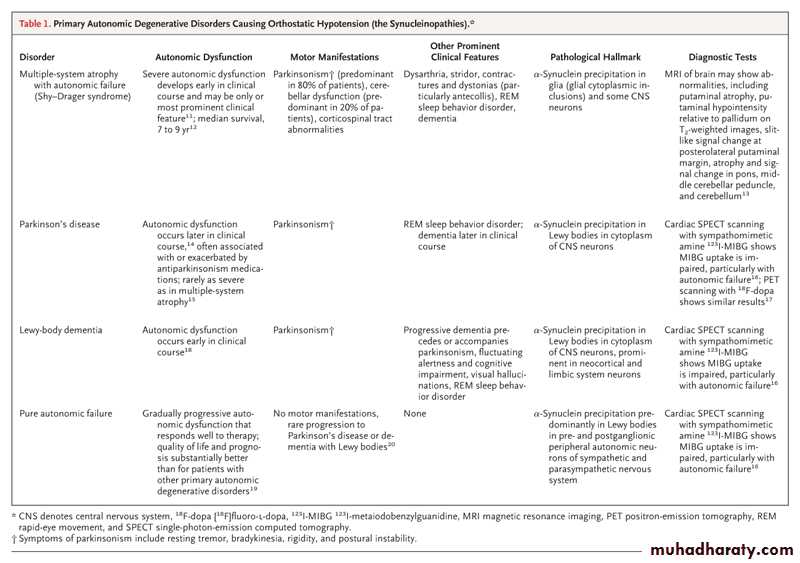
• C- Certain medical conditions
• Anemia (low red blood cell count).• Heart conditions leading to heart failure, such as a heart attack.. Cardiomyopathy Arrhythmias Constrictive pericarditis Aortic stenosis
• Heart valve disorders.
• Severe infections.
• Endocrine conditions, hypothyroidism, hyperthyroidism ,Addison’s disease ,ldiabetes. Postgastrectomy dumping syndrome, Primary hypoaldosteronism ,Phaeochromocytoma
• 6. Parkinson disease, multiple systems atrophy (Shy-Drager syndrome), and amyloidosis. defective autonomic reflex arc Syringomyelia,Spinal cord lesions,SympathectomyTabes dorsalis
• 7. Pulmonary embolism
• 8. Pregnancy.
• 9. Severe varicose veins
occurs when the brain and heart don’t communicate with each other properly.
For example, when a person stands for a long time, blood begins to pool in the legs. This causes the person’s blood pressure to drop. Instead of telling the brain that blood pressure is low, the body mistakenly tells the brain that blood pressure is high. In response, the brain slows the person’s heart rate, which makes the blood pressure drop even further, causing dizziness and other symptoms.• Neurally Mediated Hypotension
Severe hypotension associated with shock can be caused by many conditions or events.. The difference in shock is that the blood pressure doesn’t return to normal by itself, and it is at dangerously low levels. Shock is a medical emergency that must be treated immediately.
Severe Hypotension Associated With Shock
hypovolemic shock
Major bleedingSignificant loss of body fluids from severe burns
Severe inflammation of the pancreas
Severe diarrhea
Severe kidney disease
Excessive use of diuretics
cardiogenic shock.
It can be caused by a heart attack, pulmonary embolism, or arrhythmia.vasodilatory shock. It can happen because of:
Severe head injury
Reaction to some medicines
Liver failure
Poisoning
Severe allergic reaction (anaphylactic shock (
• Who Is At Risk for Hypotension?
• Older adults are more likely to have orthostatic and postprandial hypotension.• Children and young adults are more likely to have neurally mediated hypotension.
• People who take certain medicines, such as high blood pressure medicines, have a higher risk of hypotension.
• People with Parkinson disease and some heart conditions also have a higher risk of hypotension.
• postpartum mothers
• those who have been on bedrest
• People suffering from anorexia nervosa and bulimia nervosa
Signs and symptoms
• Dizziness or lightheadedness
• Fainting (syncope(
• Lack of concentration
• Blurred vision
• Nausea
• Cold, clammy, pale skin
• Rapid, shallow breathing
• Fatigue
• Depression
• Thirst
Some of the other signs and symptoms of shock vary,depending on the cause.
The skin becomes cold and sweaty. It often looks blue or pale. If pressed, the color returns more slowly than normal. A bluish network of lines can be seen under the skin.The pulse becomes weak and rapid.
The person begins to breathe very quickly.
When shock is caused by extreme widening or stretching of blood vessels (such as in septic shock), a person feels warm and flushed at first. Later, the skin becomes cold and clammy, and the person feels very sleepy.
How Is Hypotension Treated
Treatment depends on the cause of the hypotension and how severe the signs and symptoms are.Hypotension in a healthy person that does not cause signs or symptoms usually does not need to be treated.Severe hypotension associated with shock is a medical emergency.
Making lifestyle changes:
• Drinking plenty of fluids, like water
• Drinking little or no alcohol
• Standing up slowly Take a deep breath and flex your
• abdominal muscles while rising to maintain blood and
• oxygen in the brain.
• Gradually sitting up for longer periods of time if
• you’ve had to stay in bed for a long time
• Advise elderly on standing slowly, dorsiflexing the
• feet first, and even crossing the legs whilst upright.
• When the condition is caused by prolonged bed rest,
• improvement may occur by sitting up with increasing
• frequency each day. In some cases, physical
• counterpressure such as elastic hose or whole-body
• inflatable suits may be required.
Using compression stockings
that apply pressure to the lower body. These garments drive blood from the legs to the heart and brain and help blood circulate through the body.Stopping a medicine or changing the dose if the medicine is causing the hypotension.
Taking medicine to raise blood pressure reduce signs and symptoms, and treat related conditions. Medicines include ephedrine, phenylephrine, fludrocortisone, and nonsteroidal anti-inflammatory medicines.
• Treating Neurally Mediated Hypotension
• Making lifestyle changes, such as:
• Avoiding situations that trigger symptoms. For example, don’t stand for long periods of time, and avoid frightening or upsetting situations.
• Drinking plenty of fluids, like water.
• Increasing salt intake. through sodium supplements or electrolyte-enriched drinks. A suggested value is 10 g per day; overuse can lead to hypertension and should be avoided.
• Learning to recognize symptoms that occur
• before fainting, and taking action to raise• blood pressure crossing the legs and
• squeezing them together or lying down
• Stopping a medicine or changing the
• dose if the medicine is causing the hypotension.
• Taking medicines, such as fludrocortisone, to treat the hypotension if symptoms are very bad.
• Children with NHM often outgrow it.
Treating Severe Hypotension Associated With Shock
Shock is a life-threatening emergency that usually requires treatment in a hospital The goals of treating shock are to restore blood flow to the organs as quickly as possible, to prevent organ damage, and to find and reverse the cause of the shock.Medicines can be given to raise the blood pressure or make the heartbeat stronger. Depending on the cause of the shock, other treatments such as antibiotics or surgery may be required.
• Living With Hypotension
• If you have hypotension, it’s important to try and prevent or minimize symptoms, such as dizzy spells and fainting. Steps to take may include the following:• Get up slowly after sitting or lying down if you have orthostatic hypotension.
• Don’t stand for long periods of time if you have neurally mediated hypotension.
• Eat small, low-carbohydrate meals if you have postprandial hypotension.
• Drink plenty of fluids, like water.
• Drink little or no alcohol.
• Increase salt intake, if appropriate.
• Use compression stockings.
• Get regular exercise, as appropriate for your state of health.
• Learn to take your own blood pressure to find out what’s normal for you.
• When to seek medical advice
• In many instances, low blood pressure isn't serious. If you have consistently low readings but feel fine, your doctor is likely to monitor you during routine exams. Even occasional dizziness or lightheadedness may be relatively minor — the result of mild dehydration, low blood sugar or too much time in the sun or a hot tub, for example. In these situations, it's not a matter so much of how far, but of how quickly, your blood pressure drops. Still,
• it's important to see your doctor if you experience any signs or symptoms of hypotension because they sometimes can point to more serious problems.
• It can be helpful to keep a record of your symptoms, when they occur and what you were doing at the time. If these occur at times that may endanger you or others, you should talk to your doctor.
• Complications
• Even moderate forms of low blood pressure can seriously affect quality of life, leading not only to dizziness and weakness but also to fainting and a risk of injury from falls. And severely low blood pressure from any cause can deprive your body of enough oxygen to carry out its normal functions, leading to damage to your heart and brain.The standard treatment for OH is a drug called midodrine, which helps to alleviate symptoms. However, standard doses of midodrine also raise blood pressure when people lie down. Now, researchers led by Phillip Low, M.D., of the Mayo Clinic in Rochester, Minnesota, have shown that another drug called pyridostigmine can alleviate many of the symptoms of OH, either alone or in combination with a low dose of midodrine.
Midodrine and pyridostigmine both work by causing blood vessels to constrict. Midodrine causes this constriction continuously while it is in the bloodstream. On the other hand, pyridostigmine is thought to work by slowing breakdown of the nerve-signaling chemical acetylcholine, which is used by a cluster of nerve cells called the autonomic ganglion. The autonomic ganglion transmits signals from the central nervous system to the peripheral nervous system.
Signals from the autonomic ganglion are minimal when people are lying down, but increase dramatically whenever they stand up or undergo other "orthostatic stress" that causes the body to adjust to maintain normal blood pressure. Therefore Dr. Low and his colleagues theorized that pyridostigmine would increase blood pressure only when people stand up, and that it would work in proportion to the amount of orthostatic stress they experience with different activities.
• Tilt table test: Why is it performed.
• A tilt table test is used to evaluate the cause of unexplained fainting or severe lightheadedness.• During the test, your blood pressure and heart rate are monitored. You begin by lying flat on a table. Then, the table is tilted to raise the upper part of your body — simulating a change in position from lying down to standing up. This test allows doctors to evaluate your body's cardiovascular response to this change in position.
• When you stand up, gravity causes blood to pool in your leg veins, reducing the amount of blood that returns to your heart. This causes your blood pressure to drop (orthostatic hypotension). Normally, your autonomic nervous system rapidly accommodates this effect by narrowing (constricting) your blood vessels and increasing your heart rate. But if these mechanisms don't work normally, the drop in blood pressure can be severe enough to cause fainting.
• The tilt table test can help detect orthostatic hypotension. Causes of orthostatic hypotension may include diseases that affect the autonomic nervous system, such as diabetic autonomic neuropathy and Shy-Drager syndrome.
Hypotension is abnormally low blood pressure. that is lower than 90/60 mmHg.
Some people have low blood pressure all the time. They have no signs or symptoms and their low readings are normal for them. In other people, blood pressure drops below normal because of some event or medical condition.
Key Points
In a healthy person, low blood pressure without signs or symptoms is usually not a problem and requires no treatment.
The three main forms of hypotension with signs and symptoms are orthostatic hypotension, neurally mediated hypotension (NMH), and severe hypotension associated with shock.
Orthostatic hypotension is low blood pressure that occurs upon standing up from a sitting or lying down position. NMH is low blood pressure that results from standing for too long or in reaction to severe emotional stress.
Shock is a life-threatening condition in which blood pressure drops so low that the brain, kidneys, and other vital organs can’t get enough blood to work properly. Shock can result from a major trauma to the body, such as serious bleeding, severe burns, heart attack, severe allergic reaction, or an infection in the blood.
People of all ages can have hypotension. Older adults are more likely to have orthostatic and postprandial hypotension. Children and young adults are more likely to have NMH.
Signs and symptoms of orthostatic hypotension and NMH include dizziness, blurry vision, weakness, nausea, and fainting. Both of these types of hypotension can be dangerous if a person falls because of the dizziness or fainting.
Signs and symptoms of shock include confusion, sweating, weak and rapid pulse, and warm and flushed skin that becomes cold and clammy. If shock progresses, the person can lose consciousness. Shock can be fatal if not treated immediately.
Treatments for orthostatic hypotension and NMH are intended to relieve symptoms and manage underlying conditions. They include medicines and use of compression socks or inflatable pants to improve circulation. Lifestyle changes also are important, such as standing up slowly, drinking lots of fluids, and learning to recognize symptoms to prevent fainting.
Treatment for shock includes restoring blood flow to the organs through special fluids or blood. Medicines can be given to raise the blood pressure or make the heartbeat stronger. Depending on the cause of the shock, other treatments such as antibiotics or surgery may be required.
Prognosis
The prognosis for individuals with hypotension depends on the underlying causePostural orthostatic tachycardia syndrome
A rare disorder where a persons heart rate increases on standing up but little or no fall in blood pressure.. The severity, prognosis and response to treatment is variable.
EPIDEMIOLOGY The postural tachycardia syndrome (POTS) is the most prevalent form of orthostatic intolerance. It is estimated that 500,000 Americans suffer from this disorder .
It is the most common syndrome of young people seen in autonomic dysfunction clinics . Patients present at a relatively young age 14 to 45 years.
Symptoms of Postural orthostatic tachycardia syndrome
Rapid heartbeatLightheadedness
Headache
Chronic fatigue
Chest pain