د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
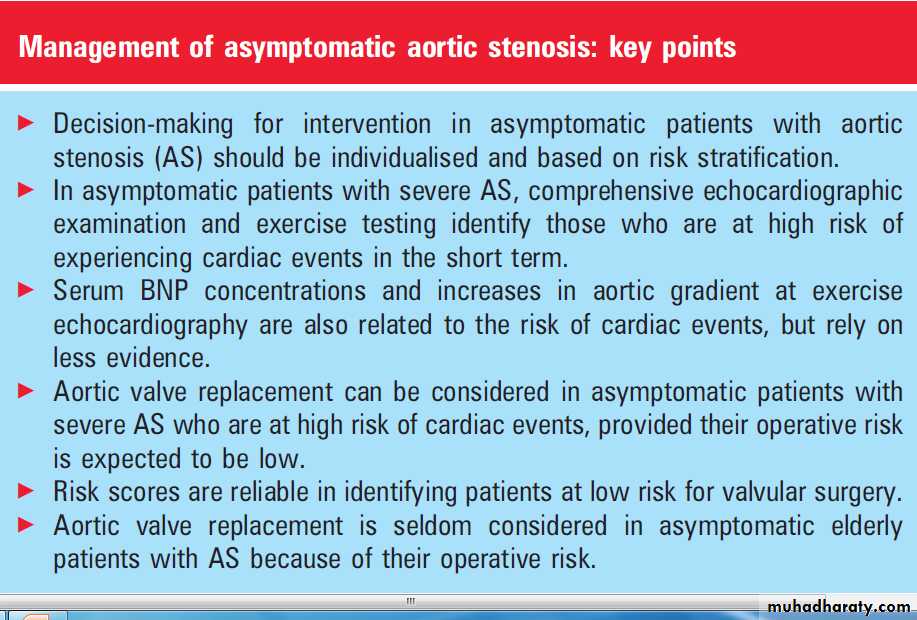
Management of asymptomaticaortic stenosis
Heart 2011The management of asymptomatic patients with
aortic stenosis (AS) is a frequent situation, asattested by the 23% of patients in New York Heart
Association (NYHA) functional class I referred for
AS in the Euro Heart Survey on valvular disease.
This is the consequence of an increased awareness of
AS, which is the most frequent heart valve disease in
western countries, and of the widespread use of
echocardiography.
Symptomatic severe AS is a class I recommendation for surgery in guidelines.
Conversely, asymptomatic AS was initially considered as justifying only follow-up.
A better insight into the prognosis of asymptomatic AS now makes it possible to identify asymptomatic patients with AS in whom intervention can be considered.
NATURAL HISTORY OF ASYMPTOMATIC
AORTIC STENOSISOverall prognosis
The landmark paper of Ross and Braunwald
published in 1968 reported a dramatic increase in the
mortality of patients with AS after the onset of
severe symptoms. For a long time this has been the
rationale for not operating on patients with
asymptomatic AS.
However, this study from the pre-echo era did not include any evaluation of either AS severity or its left ventricular consequences.
In addition, rheumatic AS was still prevalent and
mean age at death was 63 years, which does not
correspond to contemporary AS epidemiology.
Prospective studies focusing on asymptomatic
AS have been performed since the 1990s and thesehave progressively led to an individualised prognostic assessment. From nine prospective series
totalling 1125 asymptomatic patients, the linearised
rate of sudden death is estimated at 0.8% per
year (table 1).
4e12 A series of 622 patients identified
retrospectively reported a 0.3% yearly rate of
sudden death over a mean follow-up of 5.4 years.
At first sight, this could be an incentive for not
intervening before symptom onset, since the risk of
sudden death is lower than the operative risk.
However, these studies also showed that patients
became rapidly symptomatic, thereby facing
a yearly risk of sudden death of approximately 4%.
Since symptom onset is subjective and often
progressive, patients are likely not to report
symptom onset at an early stage. In addition, even
symptomatic patients with severe AS are not always
referred for surgery.
Thus, waiting for symptom onset may expose such patients to a higher risk of sudden death, which also increases when surgery is delayed because of a waiting list. These considerations, in addition to the inter-individual variability in the progression of AS, justify the attempts to identify among asymptomatic patients with AS those who are likely to become rapidly symptomatic and who, therefore, will be candidates for surgery in the near future.
Risk stratification
Echocardiographic variablesThe first step towards risk stratification followed
the publication of the paper by Otto et al which
reported the prospective follow-up of 123 patients
with AS and a peak aortic jet velocity (Vmax)
≥2.5 m/s. Annual stress tests ensured that
patients remained truly asymptomatic. This study
identified Vmax as the best predictor of eventsd
that is, death or surgery.
Patients with Vmax <3 m/s had a 5 year event-free survival rate >80%,
whereas those with Vmax ≥ 4 m/s had a 2 year
event-free survival rate <30%.
The prospective follow-up of 128 patients with
Vmax ≥ 4 m/s enabled a subgroup of asymptomatic patients at particularly high risk to be identified.
Patients who had moderate or severe valve calcification and rapid AS progression, defined as an increase in Vmax ≥ 0.3 m/s/year, had a 2 year
event-free survival <20%. A particularly relevant
finding was that those patients had a high risk of
very early event, since death or surgery occurred in
30% of them at 6 months and in >65% at 1 year.
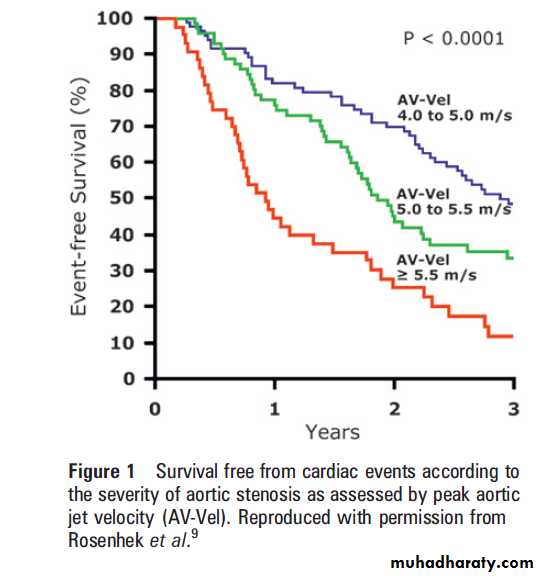
More recently, Vmax ≥5.5 m/s was found to be
associated with a high risk of events in asymptomatic patients: rates of death or surgery were 56% at 1 year, 75% at 2 years, and 89% at 3 years.It should be noted that very severe AS was a marker of poor outcome only when using Vmax, whereas there was no significant difference in outcome according to whether the aortic valve area was ≤ or >0.6 cm2 (figure 1).
Exercise testing
The obvious advantage of exercise testing is itsability to overcome the subjectivity of symptom
evaluation. However, the frequency and prognostic
impact of objective dyspnoea occurring at exercise
in patients who claim to be asymptomatic was
only recently shown in 2005. In a study of 125
patients with AS of diverse severity (mean valve
area≤1.4 cm2), 29% of patients reporting no
symptoms spontaneously experienced limiting
symptoms during exercise testing.
These patients had a 49% rate of 1 year symptom-free survival ascompared with 89% in truly asymptomatic patients. Limiting symptoms during exercise was the strongest factor related to 1 year event-free survival in multivariate analysis.
The positive predictive accuracy of limiting symptoms during exercise testing for the occurrence of symptoms was 57% in the general population, 65% in patients with severe AS, and 79% in patients aged under 70 years.
Exercise testing is also useful for risk stratification
of asymptomatic AS in patients who do notexperience dyspnoea. The occurrence of other
symptoms (angina or near syncope), inadequate
rise in blood pressure, complex ventricular
arrhythmias or repolarisation abnormalities at
exercise were reported in two thirds of patients
with severe AS and were associated with an event free survival rate of <20% at 2 years, whereas this rate was >80% at 5 years in those who had normal exercise tolerance.
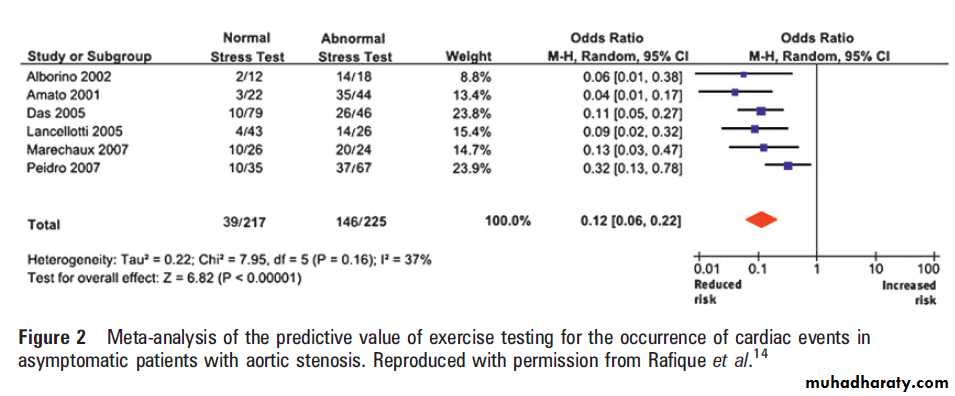
A meta-analysis of exercise testing in asymptomatic
AS, pooling 442 patients, showed a highlysignificant relationship between abnormal exercise
test and the risk of cardiac events (figure 2).
Normal exercise tolerance was associated in
particular with a very low risk of sudden death.
Exercise echocardiography enables valvular function and its consequences to be assessed. The
increase in aortic gradient during exercise is related
to the occurrence of cardiac events in asymptomatic
patients, with a threshold of 20 mm Hg increase
proposed recently in a large multicentre series.
Biomarkers
Serum B-type natriuretic peptide (BNP) concentration
is related to NYHA functional class in AS and to event-free survival and survival. When considering specifically asymptomatic patients, serum BNP is associated with the occurrence of symptoms. A study showed that the combination of serum BNP concentration with Vmax and gender achieved a good discrimination between those patients who experienced cardiac events during a 2 year follow-up and those who did not. However, no consistent threshold of serum BNP concentration can be proposed to select potential candidates for surgery.
Perspectives to improve risk stratification Other imaging variables may contribute to risk stratification in asymptomatic AS, but are in need of additional clinical validation at the present time.
Indices of diastolic function (left atrial area
index, late diastolic annular velocity as assessed by
tissue Doppler imaging, left ventricular diastolic
filling pattern from Doppler mitral flow) were
associated with occurrence of cardiac events in
patients with asymptomatic AS in one series.
Indices of left ventricular systolic function derived from stain imaging or tissue Doppler seem to be related to exercise tolerance, but their clinical prognostic value has not been proven so far.
CT enables valve calcification to be more reliably
assessed and quantitated than when using echocardiography.
Calcium score was related to the progression of aortic valve area in AS but its impact on clinical outcome of asymptomatic patients has not been proven.
EVALUATION OF THE RISK OF SURGERY
By definition, the aim of surgery in asymptomaticpatients is not to improve functional status, but
to improve life expectancy.
Therefore, the assessment of immediate and late survival after aortic valve replacement is an important component in decision-making in asymptomatic patients.
Patients in NYHA class I have a low operative
mortality. This is partly related to less severe
consequences of valvular disease itself. Low
mortality is also explained by the fact that patients
in NYHA class I present with favourable characteristics regarding predictive factors of operative morality that is, younger age and less frequent comorbidities than symptomatic patients.
Assessment of comorbidities, including coronary
artery disease, thus has a strong impact on decision making in asymptomatic AS. In addition, intervention is never performed in an emergency in asymptomatic patients.Different risk scores are available to estimate the
individual operative risk. There is now evidence
that risk scores lack accuracy in the prediction of
operative mortality in high risk patients. However,
risk scores allow for a good discrimination between
low risk and high risk patients and their accuracy is
relatively good in low risk patients with AS.
Given the low mortality rate of asymptomatic
patients with AS, surgery is generally consideredonly in patients who are at high risk for cardiac
events and who have a low expected operative
mortality. Decision-making in asymptomatic
patients should also take into account prosthetic
related complications, which contribute to late
cardiovascular mortality, in particular in patients
who underwent valvular surgery at an early stage
of their disease.
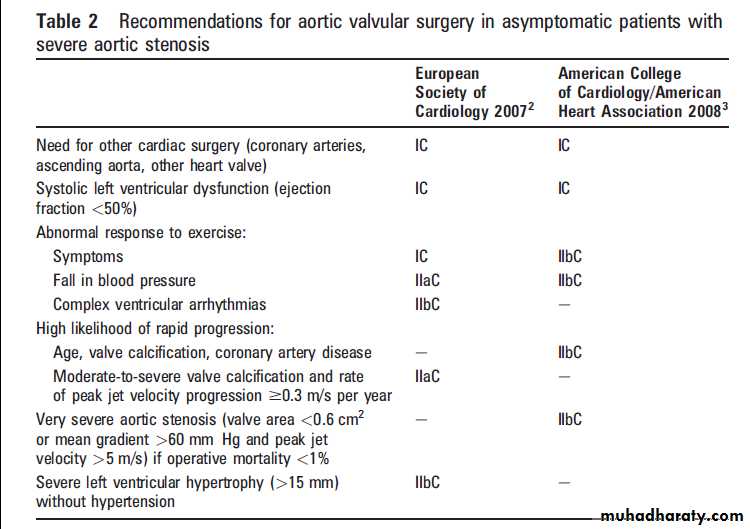
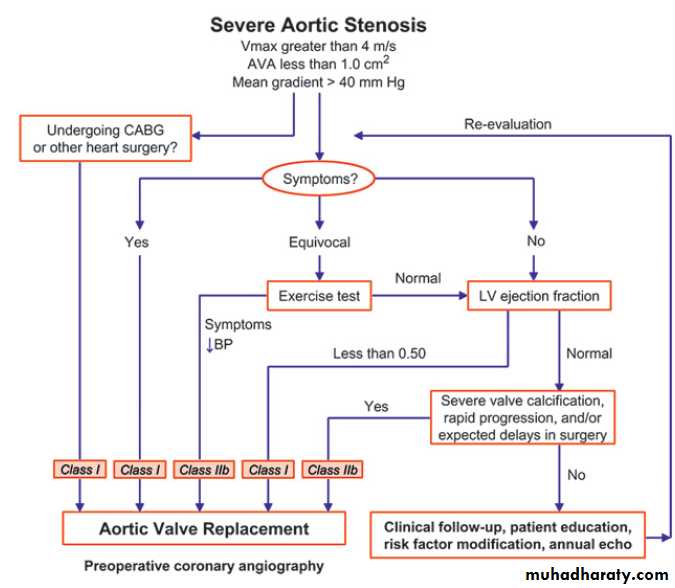
GUIDELINES
The European Society of Cardiology (ESC) and the
American College of Cardiology/American Heart
Association (ACC/AHA) guidelines for intervention
in asymptomatic patients are summarised in table 2
and figures 3 and 4. Aortic valve replacement is
considered only in selected patients who have severe AS, as defined by Vmax ≥4 m/s peak aortic jet velocity, mean gradient≥40-50 mm Hg, and/or aortic valve area ≤1.0 cm2 or 0.6 cm2/m2 body surface area. Although Vmax and mean gradient are flow
dependent indices, they should be checked for
consistency with valve area, which is more subject
to errors of measurements and inaccuracy.
Besides the need for other cardiac intervention,
both guidelines recommend surgery in asymptomaticpatients with left ventricular ejection fraction
(LVEF) <50%, although this is not supported by
the literature and concerns a small number of
asymptomatic patients. Despite certain differences
in criteria, intervention is also recommended in
patients in whom there is a high likelihood of rapid
progression of AS.
The main difference between the ESC and ACC/AHA guidelines concerns the use of exercise testing, which is recommended for risk stratification of asymptomatic patients with severe AS in the ESC guidelines, and only in patients with equivocal symptoms in the ACC/AHA guidelines.
The development of symptoms during exercise
testing is a class I recommendation for intervention
in the ESC guidelines and a class IIb recommendation
in the ACC/AHA guidelines.
It should be stressed that all recommendations are associated with levels of evidence C, which illustrates the low level of evidence on which they rely.
The identification of asymptomatic patients who are at high risk of cardiac events is important even in those who are not considered for surgery, since they require a frequent follow-up (≤6 months), in particular to detect symptoms which are not always reported spontaneously. Close follow-up is also important to reinforce patient education, in particular the need to report any new symptom.
No medical treatment has been shown to reduce
the progression of AS so far.
EVALUATION OF PRACTICES
An evaluation of the practices utilised in the management of asymptomatic AS was performed in the Euro Heart Survey. Of 1197 patients with AS, 809 had severe AS and 84 did not have any symptoms. Although there was a lower level of evidence supporting exercise testing than today, an abnormal response to exercise testing was already an indication for intervention in the 1998 ACC/AHA guidelines, which were the only international guidelines available at that time.However, exercise testing was performed in only 2.4% of asymptomatic patients with severe AS.
A decision to operate was taken in 45 of the 84 patients (54%),and the decision to operate or not was in accordance with the 1998 ACC/AHA guidelines in 68% of cases.
Of the 27 patients who were considered
for surgery in accordance with guidelines, the most
frequent reason for intervention was a valve area
≤0.6 cm2, which was a class IIb recommendation.
In the light of recent studies, Vmax seems a more
appropriate echocardiographic variable than aortic
valve area to identify high risk asymptomatic
patients with very severe AS.
No patient was considered for intervention because of abnormal response to exercise. Although there was a relatively good concordance between guidelines and
practice, the decision to operate was based on class
IIb recommendations in 70% of cases.
IMPACT AND LIMITATIONS OF DIFFERENT
CRITERIA OF RISK STRATIFICATION ONDECISION-MAKING
Different criteria can now be used to identify
asymptomatic patients with AS who are at high
risk of reaching the end point of death or surgery
within 1-2 years. However, the different criteria
for risk stratification have been tested separately
and their respective predictive value for the occurrence of cardiac events is not known.
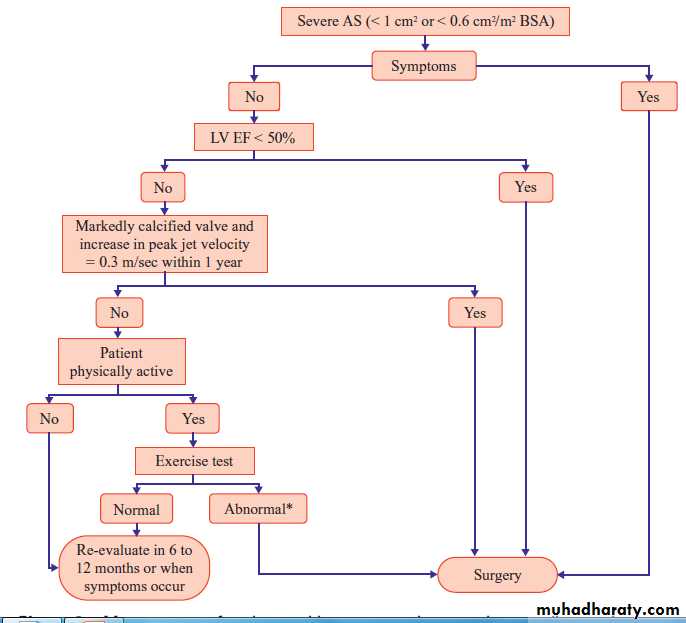
Rather than combining all criteria, a practical stepwise approach may be proposed in asymptomatic
patients with AS.
The first step is to consider surgery in the rare
asymptomatic patients with LVEF <50%.
The second step is to assess the severity of AS,
combining Vmax, mean gradient, and valve area.
Patients with Vmax≥5.5 m/s may be considered
for surgery without additional investigation.
Although this indication relies on only one study, it may be justified by the high risk of short term cardiac events and the potential reluctance to exercise patients with very severe AS. This is likely to be applied in practice since the Euro Heart Survey showed that practitioners are prone to consider surgery for very severe AS.
In patients with severe AS but Vmax <5.5 m/s,
the third step is to perform exercise testing if
they are physically active.
Patients who develop symptoms or have a fall in blood pressure should be considered for surgery. There is no reason for performing routine exercise echocardiography at this stage since conventional exercise testing is easier to perform and enables >25% of asymptomatic patients to be identified as being at high risk of cardiac events.
In patients who remain asymptomatic after
exercise testing, the fourth step can be to searchfor indices whose prognostic value is less well
established and/or require additional investigations:
– rapid progression defined by an increase of
Vmax ≥0.3 m/s per year in patients with
moderate or severe valve calcification.
– increase in mean gradient ≥20 mm Hg during
exercise echocardiography– a score combining Vmax, serum BNP concentration,
and gender >16.
Thus, a simple approach combining comprehensive
baseline echocardiographic examination and
exercise testing enables most high risk patients
with severe AS to be identified.
Aortic valve replacement is considered in moderate AS only in patients who need surgery on another valve, coronary arteries or ascending aorta,
which is a rare occurrence in asymptomatic
patients. They should be informed of the
potential for progression of moderate AS, even
more so in elderly patients, in those with severe
valve calcification or associated coronary artery
disease who are likely to experience a more rapid
progression from moderate to severe AS.
Improvement in risk stratification does not solve
all the problems of the management of asymptomatic AS.The translation from the identification of a high risk of developing cardiac events to the benefit of surgery lacks supporting data. Only one
prospective non-randomised study compared
intervention to conservative management in
patients with asymptomatic AS.
Among 197 patients with asymptomatic AS defined by Vmax ≥4.5 m/s, mean gradient ≥50 mm Hg, or aortic
valve area ≤0.75 cm2, 102 patients underwent early
surgery within 3 months of evaluation and 95 were
managed conservatively that is, they underwent
surgery when they became symptomatic. Six year
cardiac and non-cardiac mortality rates were lower
after early surgery as compared to conservative
management, including in two subgroups of 57
propensity matched patients.
However, the lack of exercise testing raises concerns about the absence of symptoms. This is reinforced by the high cardiac mortality (24% at 6 years) in patients managed conservatively, with the occurrence of seven deaths due to heart failure and nine sudden deaths. Such figures are unexpected in closely followed patients with asymptomatic AS, even with initial Vmax ≥4.5 m/s.
In contrast, there were no cardiac deaths, including no operative mortality, in the 105 patients who underwent early surgery.
The findings of this study cannot lead to the recommendation for systematic surgery in
asymptomatic patients with AS without taking
into account the criteria of risk stratification.
Available evidence strongly suggests that decision making for aortic valve replacement in symptomatic
AS should be individualised, and weighs the
risk of cardiac events according to echocardiographic
examination, exercise testing, and other
investigations if needed, and the risk of surgery.
PARTICULAR SITUATIONS
Bicuspid aortic valve is frequently associated with a dilatation of the ascending aorta independently of valve function.Surgery may be indicated in asymptomatic patients with a bicuspid aortic valve when the maximum diameter of the ascending aorta is ≥50 mm.
Thus, echocardiographic examination should comprise standardised measurements of the ascending aorta when a bicuspid aortic valve is present or even
Suspected for example, in young patients since
the diagnosis of bicuspid valve may be difficult,
particularly when highly calcified. This is of
particular importance when the dilatation
predominates above the sinotubular junction, since
it can be missed if the echocardiographer does not
pay specific attention to the aorta.
Elderly Aortic valve replacement is generally not considered in asymptomatic elderly patients with AS because of the increase in the operative risk with age. No age limit can be given and surgery may be considered in selected physically active patients without comorbidities; exercise testing is feasible and useful in these cases. Conversely, elderly patients in whom objective exercise capacity is difficult to assess
because of reduced activity and/or comorbidities are
generally not considered for early surgery.
A relatively frequent situation is the need for noncardiac surgery in an asymptomatic patient with
severe AS.
Non-cardiac surgery can be performed in most asymptomatic patients without prior valvular
surgery.
Indications for valvular surgery before
non-cardiac surgery are restricted to selected
patients when non-cardiac surgery is at high risk
and if the risk of aortic valve replacement is low.
At present, the use of transcatheter aortic valve
implantation (TAVI) is targeted towards symptomaticpatients who are at high risk for conventional
valvular surgery. In the future, it is possible
that TAVI will expand the indications of interventions
for AS to low risk patients, including asymptomatic patients. Such extension of indications
could be considered only when the long term
durability of devices has been demonstrated, and
when TAVI is proven to be feasible with a very low
risk in asymptomatic patients.
Low flow, low gradient AS due to impairment of
LVEF is unlikely to be encountered in asymptomatic
patients.
Patient management relies on risk
stratification including low dose dobutamine stress
echocardiography.
Low flow, low gradient AS with preserved LVEF
has been identified more recently and is associatedwith an increase in valvuloarterial impedance.
Valvuloarterial impedance reflects the global
haemodynamic load of the left ventricle and has an
impact on survival in asymptomatic patients with
moderate or severe AS. However, indications for
interventions are not well defined in patients with
low flow, low gradient AS and preserved LVEF, and
surgery is thus currently not considered in asymptomatic patients.
CONCLUSION
Prospective series on asymptomatic AS confirm thatthe risk of sudden death is low, but not zero, and
consistently show that certain patients have a high
risk of becoming symptomatic in the short term
and, thus, of being put at high risk of cardiac
complications. Most high risk patients can be
identified using comprehensive echocardiographic
examination and exercise testing.
Patients with normal exercise tolerance are particularly at low risk of sudden death.
Decision-making for aortic valve replacement should be individualised in asymptomatic patients with severe AS, weighing the risk of cardiac events against the operative risk to select
patients for early surgery or closer follow-up.
Figure 3 Management of patients with severe aortic stenosis according to the guidelines of the European Society of Cardiology. AS, aortic stenosis; BSA, body surface area; EF, ejection fraction; LV, left ventricle.