د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Management of asymptomaticmitral regurgitation
Heart 2010Nowadays, mitral regurgitation (MR) already
represents a major health problem, and has beenrecognised as the most frequent valvular disease in the USA and the second most common form of
valve disease requiring surgery in Europe. In the
future, due to the ageing and growth of the general
population, the negative impact of MR on patients’
health is expected to increase further.
As healthcare providers, we will thus be more and more frequently called upon to challenge this disease, which is indeed extremely heterogeneous in terms of prognosis and treatment options.
This article aims to provide a practical, step-bystep
approach to the daily management of
asymptomatic MR in the light of the most recent
diagnostic and therapeutic advances.
STEP 1
Essential knowledge required to approach anypatient presenting with any amount of MR
A diagnosis of MR should be made in the presence
of a pathological amount of blood regurgitating
from the left ventricle (LV) into the left atrium (LA)
because of an incompetent mitral valve (MV).
The mere detection of MR is not sufficient for diagnosis, and for correct decision making we also need to assess:
• the aetiology;
• the mechanism (ie,how the disease prevents the MV from being competent); and
• the severity of the regurgitation.
An appropriate and comprehensive diagnosis
not only enhances communication, but more
importantly leads to a different prognostic assessment
and therapeutic management
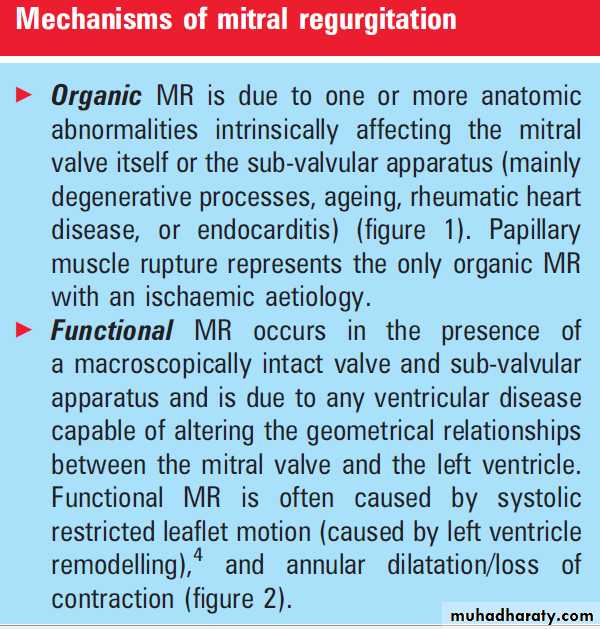
The numerous aetiologies of MR can be roughly
grouped into either
Ischaemic (ie, due to coronary artery disease) or non-ischaemic (all other causes),
and the mechanisms into organic or functional.
In the present paper, we will focus only on nonischaemic, organic MR.
Certainty of MR severity A possible reason for a patient with MR to be asymptomatic is that volume overload is not severe enough to cause symptoms and/or ventricular or atrial dysfunction.
The evaluation of MR severity, as for any other
valvular lesion, should be based on the combinationof clinical and instrumental findings.
Clinical examination plays an important role in
the detection of MR in asymptomatic patients, and
represents the first step in the diagnosis of its
severity.
A low intensity murmur is rarely associated with severe organic MR, whereas a loud murmur is
frequently a sign of significant incompetence.
Unfortunately, many patients present with
a murmur of medium intensity, which can begenerated either by severe or moderate MR.
The presence of a third heart sound (S3) detected at physical examination is also considered helpful in
assessing the severity of MR.
Nevertheless, the specificity of S3 is quite low due to the fact that it can also be diagnosed in aortic disease, mitral stenosis, and in young healthy individuals. An ECG and chest x-ray are usually performed alongside clinical examination and may provide relevant information.
For example, a significant cardiac enlargement and/ or pulmonary congestion detected at chest x-ray should raise doubts about the real functional
capacity in a patient claiming to be asymptomatic.
Similarly, detection of atrial fibrillation (AF) on the ECG should make us search even more actively for
the presence of symptoms.
Doppler echocardiography represents the tool of
choice for the diagnosis of MR. This tool can
provide non-invasive information on the presence, aetiology, mechanism of the lesion, consequences of
volume overload on cardiac size and function, and
the condition of the pulmonary circulation,
tricuspid valve, and right ventricle.
A reliable assessment of MR severity can be obtained only by integrating bi-dimensional and Doppler findings (table 1) and verifying their consistency with the other clinical/instrumental features.
STEP 2
The rationale on which to base the distinctionbetween asymptomatic versus symptomatic mitral
Regurgitation Studies which enrolled patients both in Europe and the USA showed that although MR is associated with notable mortality and cardiac morbidity,this valvular lesion is still underdiagnosed (especially in women), and undertreated.
Although percutaneous repair is a promising option (which deserves further investigation), timely conventional surgery currently remains the cornerstone of treatment for organic MR.
The rationale to advocate surgery in symptomatic patients is based on the poor outcome under medical management experienced by patients in New York Heart Association (NYHA) functional class III and IV.
Conversely, when MV surgery (and specifically MV
repair) is performed early during the natural history
of the disease that is, in patients with no or
minimal symptoms (NYHA class I or II) postsurgical outcome is significantly more favourable,
and the expected survival of operated patients is
comparable to the expected survival of the general
population (figure 3).
In addition, in the management of asymptomatic MR, it is also worth remembering that waiting for symptoms to appear (often associated with LV dysfunction) could lead to an increased surgical risk. Unfortunately, any surgical complication is difficult to accept in ‘asymptomatic patients’, for whom it is easier to perceive the immediate risk rather than the potential benefits which will only be evident in the future.
With respect to the surgical methods, although
surgery is indicated in the presence of symptomseven though it may not be possible to repair the
valve, there is general agreement that repair is
superior to replacement in most settings (figure 4), and repair should therefore be considered the
preferred surgical option whenever achievable. This
is due to the better preservation of ventricular
functional and the avoidance of prosthetic related
complications associated with MV repair.
STEP 3
Asymptomatic patients with complications fromvolume overload
LV dysfunction
The process of adaptation of the LV in response to
organic MR can be roughly simplified as:
• The acute phase;
• the chronic compensated phase;
(3) the chronic decompensated phase.
Briefly, during the ‘acute phase’ (which immediately
follows the onset of the regurgitation), the LV
function appears ‘super normal’, since the afterload
is reduced due to the possibility of the ventricle
ejecting blood both forward (into the aorta) and
backward (into the LA).
The ‘chronic compensated
phase’ follows the acute phase and is characterisedby the development of eccentric hypertrophy with
a further increase of the end-diastolic volume. The
LA progressively dilates, eventually limiting the
increase in LA pressure.
During the ‘decompensated phase’, the LV is no longer able to provide an efficient contraction, ventricular volume increases, and forward cardiac output decreases. While LV dysfunction in the advanced stages almost unavoidably causes symptoms, early LV dysfunction can be asymptomatic due to the reduction of the afterload. Unfortunately, even a moderate reduction of preoperative LV ejection fraction (LVEF) significantly impairs postoperative outcome, and its detection is therefore particularly important.
In the hypothesis that LVend-systolic dimension
(LVESD) may be less load dependent than LVEF,this parameter has been indicated as a complementary
index to optimise the timing of MV surgery.
Due to the lack of strong evidence, the European
Society of Cardiology (ESC) guidelines set the
threshold of LVESD for recommending surgery in
asymptomatic patients at 45 mm, whereas the
American College of Cardiology/American Heart
Association (ACC/AHA) guidelines threshold is 40 mm.
Our group recently analysed the long term outcome of 739 patients with degenerative MR showing that, irrespective of the presence of symptoms, an LVESD >40 mm represents an independent risk factor for adverse outcome, both under medical management and after MV surgery.
Taken together, our findings support surgery in patients with LVESD ≥40 mm, but also
suggest that the best preservation of survival is
achieved in patients operated on before LVESD
reaches 40 mm (figure 5A,B).
With respect to future developments aiming at
an early detection of LV dysfunction complicatingnon-ischaemic organic MR, exercise echocardiography
is gaining increasing consideration. Lee et al
showed that in asymptomatic MR the lack of
contractile reserve (defined as ≥4% increase of
LVEF) was a predictor of postoperative LV
dysfunction; of note, baseline echocardiographic
characteristics of patients with/without contractile
reserve were largely similar, indicating that the
assessment of contractile reserve may provide
additional information.
Pulmonary hypertension
Pulmonary hypertension (PH) is a well knownadverse consequence of non-ischaemic organic MR.
Besides the possibility that PH could represent
only a marker of severity of the underlying left
heart disease, abnormal values of pulmonary artery systolic pressure (PASP) could independently affect prognosis by inducing right ventricular dysfunction and subsequent functional tricuspid regurgitation.
Furthermore, previous studies suggested that PH
can exert direct unfavourable effects on prognosis
via neurohumoral activation and/or impairment of
pulmonary ventilation. Unfortunately, available
studies on PH complicating MR are single centre
and characterised by limited sample size, and/or
include varying degrees of regurgitation, and/or
addressed only mild PH.
The overall magnitude of these uncertainties is exemplified by the fact that in current guidelines, the threshold to define the value of PASP triggering MV surgery is largely based on experts’ opinions. In addition, although invasive measurements of PASP are no longer suitable for routine surveillance, the feasibility and prognostic implications of PASP measured by Doppler echocardiography in MR have yet to be confirmed.
Atrial fibrillation
AF is strictly linked to MR because MR producesLA enlargement, a precursor of AF, and also because MR is common particularly in the elderly, who are also at high risk for AF.
Our group showed that the onset of AF is frequent
in severe non-ischaemic organic MR, occurring ata rate of approximately 5% per year under nonsurgical management, with a risk increasing with
advancing age and larger LA dimension.
Furthermore, we found that under non-surgical management the onset of AF leads to increased cardiac mortality and morbidity (figure 6).
Unfortunately, previous data show that when surgery is performed in patients who have already developed AF, post-surgical outcome is less favourable as compared to when surgery is performed in
those who are in sinus rhythm. Furthermore,
when MV surgery is performed in those who have
not yet developed AF but in whom MR has already
resulted in significant LA enlargement (LA
>50 mm), patients encounter a higher risk of AF
after surgery, which as expected increases the
risk of stroke or heart failure.
Although the definitive role of surgical ablation
has still to be fully determined, this procedureseems to offer the possibility of restoring sinus
rhythm in 75-90% of cases in patients with
a history of AF who undergo MV repair, with
a potential reduction of the risk of stroke in long
term follow-up. Furthermore, by ablating AF, patients who undergo MV repair or replacement
with a tissue valve and remain in sinus rhythm can
often avoid anticoagulation, making it possible to
take the greatest advantage that can be derived
from these therapeutic strategies.
Taken together, these studies suggest that LA
protection is characterised by an important role
within clinical decision-making regarding patients
with MR.
Multicentre studies (possibly using LA volume as a measure of LA remodelling) are needed to confirm these findings.
Abnormal exercise test
Depending on the expectations of any individualpatient, the same functional capacity may be
perceived as normal by some and significantly
blunted by others. Notably, about 20% of patients with MR show significant impairment of cardiopulmonary
capacity despite claiming to have no symptoms.
As regards potential therapeutic implications of the
exercise test, previous authors suggested thatasymptomatic patients lacking any additional
established criteria to recommend MV surgery, who
were unable to exercise for at least 15 min on
a treadmill using a modified Bruce protocol, were
characterised by a significantly higher incidence of
cardiac events.
A simple and widely available treadmill test may thus be useful in discriminating true asymptomatics. Useful information for the management of asymptomatic MR can also be derived from the cardiopulmonary exercise test.
Areduced cardiopulmonary capacity (defined as <84% of the expected value of peak oxygen consumption at cardiopulmonary exercise test) has been indicated as a predictor of adverse clinical
events in severe organic MR.
Elevated natriuretic peptides
B-type natriuretic peptide (BNP) and its inactiveamino-terminal portion (NT-proBNP) result from
the breakdown of proBNP and have vasodilator and
diuretic effects.
Interestingly, these hormones are antagonists of the renineangiotensin and adrenergic systems, and are released in response to myocardial wall stress.
Pizzarro et al recently published their prospective experience with 269 consecutive asymptomatic patients with non-ischaemic organic MR, and with LVEF >60%. A cut-off point of 105 pg/ml of BNP was able to discriminate patients at higher risk of adverse events
STEP 4
Asymptomatic patients without complications fromvolume overload
While asymptomatic patients presenting with one
or more of the above mentioned consequences
from volume overload may be considered for
surgery with different levels of evidence (particularly
in the presence of low comorbidities and
a high likelihood of durable repair), the need for
a surgical approach in asymptomatic patients
without ventricular dysfunction, AF or pulmonary
hypertension remains the most controversial issue.
Rosenheck et al21 found that asymptomatic patients can be safely followed up until the occurrence of symptoms and/or ventricular dysfunction and/or pulmonary hypertension, but other authors have not confirmed these findings, instead highlighting the advantages of earlier surgical treatment.
Due to the lack of prospective randomised trials, these controversies remain without a definitive answer, and healthcare providers should probably inform patients about the risks and benefits of the different options
The ESC registry on valvular heart disease shows that current practice is often characterised by an
underuse of intervention even in symptomatic
patients, who have a well established benefit from
MV surgery;
therefore, even just the correct application of recognised indications will likely result in a significant improvement in the quality of care.
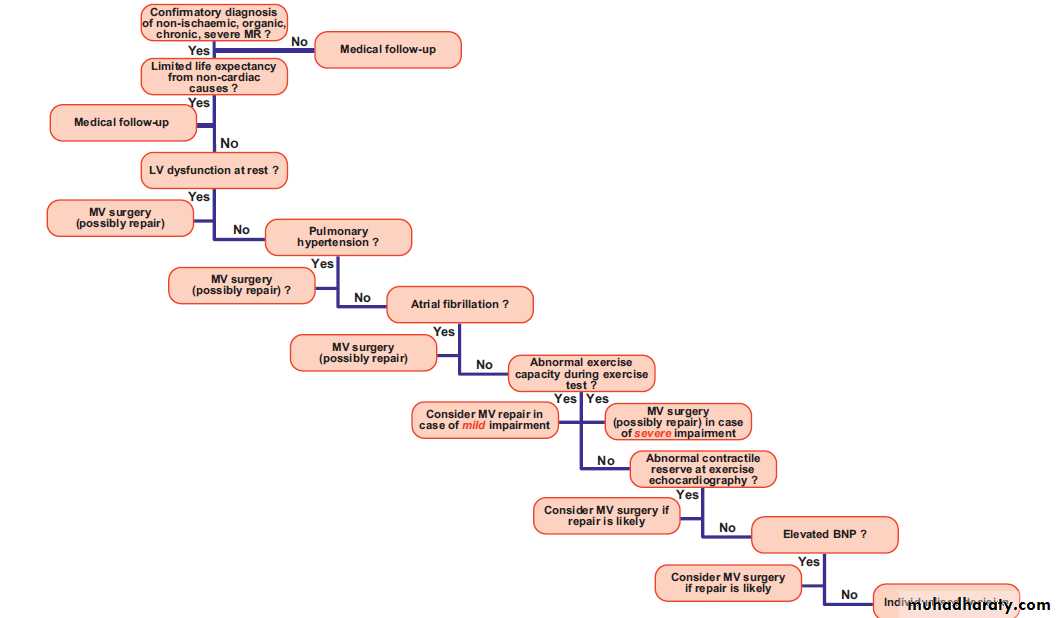
The other consideration we could raise is that many of the asymptomatic patients indeed present with one or more of the consequences from volume overload reported above, and should therefore be considered as candidates for surgery anyway (figure 7).
Recent data showed that the lack of a local
surgeon expert in MV repair may influence therapeutic decision making.ACC/AHA guidelines recommend referring patients elsewhere if a conservative surgeon is not available locally, but the feasibility of this approach still needs to be verified.
What is worth considering is that repair is superior to replacement in the vast majority of settings, and consequently a positive approach versus MV repair should be strongly advocated regardless of whether the patient is asymptomatic or not.
The percentage of repair currently approaches 50% for MV surgery in European registries and can be as high as ≥90% in experienced centres; all efforts should therefore be made in order to make use of this technique more frequently and to improve its durability.
STEP 5
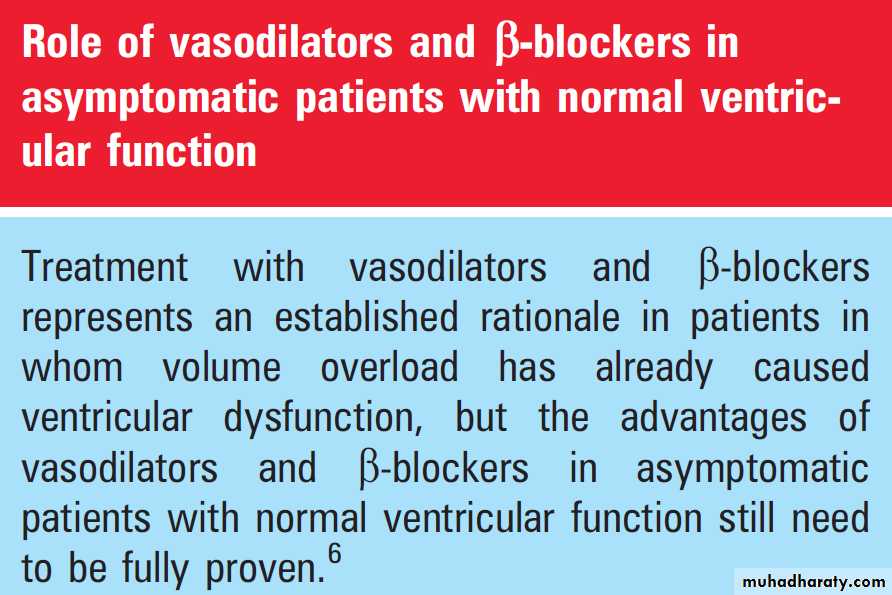
Insights on selected topicsMedical treatment
Endocarditis prophylaxis is required in every
patient with MR. Anticoagulation should be
administered in patients with MR complicated by
permanent or paroxysmal AF in order to achieve an
international normalised ratio (INR) range between
2 and 3, and during at least the first 3 months
following MV repair in asymptomatic patients
with severe organic MR.
Age and comorbidities
Age and comorbidities are strictly related to MR,
since the prevalence of both MR and comorbidities
increases with age.
Comorbidities particularly in the elderly can play a role in the genesis of the dyspnoea, raising uncertainties as to what extent the symptoms are indeed due to the MR itself or to the associated disease (patient with MR associated with chronic pulmonary disease).
Furthermore, patients may not experience cardiac symptoms because comorbidities do not allow them to engage in physical activity intense enough to reveal them (for example, in MR associated with a peripheral neurological or muscular disorder).
In these settings, the extent of the consequences of volume overload on cardiac size and function (and their time related changes), as well as BNP assessment may be of particular value.
By increasing the operative risk, comorbidities
and/or very advanced age may also directly influence the indications for surgery, potentiallydiscouraging the surgeon from operating on an
asymptomatic patient with normal LVEF
(this could be the case of a patient with significant renal impairment).
Finally, while very advanced age and/or comorbidities are expected to impair life expectancy in the short term (as in the case of an
incurable cancer), the potential benefits deriving
from a surgical treatment should be carefully
considered (figure 7).
Ventricular arrhythmias
While the relationships between MV prolapse andarrhythmias have been attributed among other
Factors to autonomic nervous abnormalities, several data suggest that a higher degree of MR in degenerative MR is an important determinant of complex ventricular arrhythmias. Our group analysed the outcome of 348 patients who received a diagnosis of non-ischaemic organic MR at the Mayo Clinic from 1980 to 1994; we found a linearised rate of sudden unexpected death (SUD) reaching 1% per year in asymptomatic patients, and 0.8% per year in those who were asymptomatic and also showed sinus rhythm and LVEF >60%.
Although the rate of SUD was lower after surgery
than in patients treated medically, in the absence of
prospective randomised studies any therapeutic
implications derived from these data need to be
cautious. Nevertheless, in our series SUD was
preceded by an episode of heart failure in more than half the patients, but symptoms did not trigger
surgery; it is quite likely that in this particular group
of patients timely surgery could have been beneficial in preventing the arrhythmic complications which can derive from LV dysfunction.
Figure 7 Proposal of a practical algorithm for the management of asymptomatic mitral regurgitation (MR). BNP, B-type natriuretic peptide; LV, left ventricle; MV, mitral valve