د. حسين محمد جمعة
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2012
Resistant hypertension
Heart 2012High blood pressure is one of the leading risk factors
influencing the global burden of cardiovasculardisease, resulting in increased incidence of all-cause
and cardiovascular mortality, sudden death, stroke,
coronary heart disease, heart failure, atrial fibrillation, peripheral artery disease, and renal insufficiency.
Hypertension affects about 25% of adults around the world and is estimated to lead to over
seven million deaths each year that is, about 13%of the total number of deaths worldwide. Lifestyle
changes are able to lower blood pressure and
prevent the development of hypertension, and
antihypertensive drug treatment has been shown
to reduce blood pressure and cardiovascular
complications in hypertensive patients.
Despite current knowledge on the management of hypertension and the availability of numerous effective
antihypertensive drugs and combinations of drugs,
hypertension remains inadequately controlled in
many patients and a number of them are considered
to have so-called ‘resistant hypertension’.
The following issues will be discussed in this article on resistant hypertension: definition; prevalence;
causes; target organ damage and cardiovascular
complications; patient evaluation; and management. It is of note, however, that much of the knowledge on resistant hypertension is observational in nature, and that hard evidence is scarce, apart from a number of recent randomised controlled trials. This article will highlight new developments, with due respect for current generally accepted knowledge.
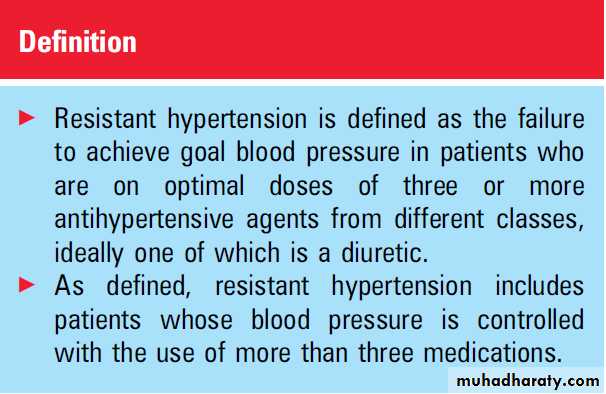
DEFINITION
Although the wording varies in different publications,resistant hypertension is conventionally
defined as the failure to lower systolic and diastolic
(office) blood pressure to goal in patients who
are adhering to lifestyle measures and to the
optimal doses of an appropriate regimen of three
antihypertensive drugs from different classes, one
of which is a diuretic.
The goal blood pressure is usually defined as <140 mm Hg for systolic blood pressure and <90 mm Hg for diastolic blood pressure;
in some studies the goal is lowered to <130/
80 mm Hg for patients with diabetes mellitus or
renal dysfunction, or even for all high and very high risk patients.
Sometimes the diuretic is not an absolute requirement. It should be recognised that the definition is in fact arbitrary and imprecise, and,if taken literally, includes patients whose blood pressure is controlled with the use of four or more medications. Whereas these patients may not be truly resistant to therapy, they deserve
special attention because of the seriousness of the
condition, the high risk of having reversible causes
of hypertension, and because they may benefit
from special diagnostic and therapeutic measures.
Resistant hypertension should not be confounded
with uncontrolled hypertension, which involvespatients who are not at goal with fewer than three
drugs, or with an inadequate treatment regimen.
Finally, it is of note that the lack of blood pressure
control is most often due to persistence of elevated
systolic blood pressure, particularly at higher age
when isolated systolic hypertension is prevalent.
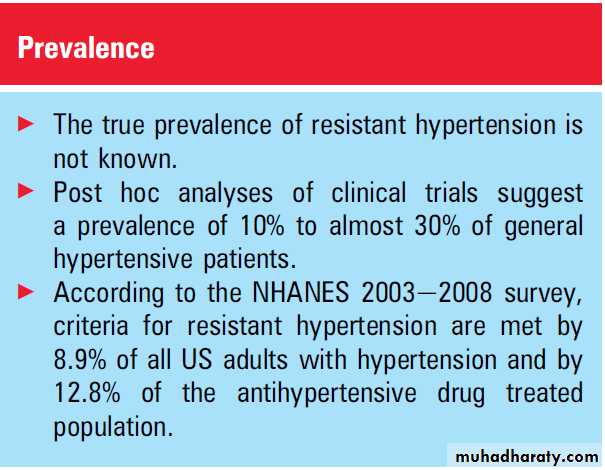
PREVALENCE
The true prevalence of resistant hypertensionremains unknown because of the absence of
a specifically designed large prospective study with
forced titration. The prevalence has mainly been
derived from clinical trials and has been estimated
to range from 10% to almost 30% of general
hypertensive patients in different studies.
However, these estimates are certain to be inaccurate because of specific inclusion and exclusion criteria, and
restricted treatment regimens in the various trials.
In a recent community based observational study
the prevalence of resistant hypertension was relatively
modest.
Persell used data collected from 2003 through 2008 in the National Health and Nutrition Examination Survey (NHANES), which uses standardised assessments of blood pressure and
of prescription medications. Non-institutionalised
non-pregnant adults with hypertension were classified
as resistant if their blood pressure was
≥140 mm Hg (systolic) or ≥90 mm Hg (diastolic),
and if they reported using antihypertensive
medications from three different classes or drugs
from ≥4 antihypertensive drug classes in the past
month, regardless of blood pressure.
These criteria for resistant hypertension were met by 8.9% of all US adults with hypertension and by 12.8% of the antihypertensive drug treated population. It is
of note that 30% of these patients were controlled on ≥4 medications.
The study also identified some characteristics of patients with resistant hypertension.
Compared to those with controlled hypertensionusing one to three medication classes, adults
with resistant hypertension were more likely to be
older, obese and black, and to have reduced renal
function, albuminuria and self reported diabetes
mellitus, coronary heart disease, heart failure and
stroke.
The authors concluded that, although not rare, resistant hypertension is currently found in only a modest proportion of the general hypertensive population.
However, if the possible contributions of poor adherence to treatment and of the white coat effect are taken into account, the true prevalence may even be less than the observed prevalence of 8.9% in the general hypertensive population.
On the other hand, a number of patients with uncontrolled hypertension on one or two
antihypertensive medications would probably notbe controlled on ≥3 medications and might have
been labelled as having resistant hypertension if
their medications had been properly titrated to ≥3
drugs.
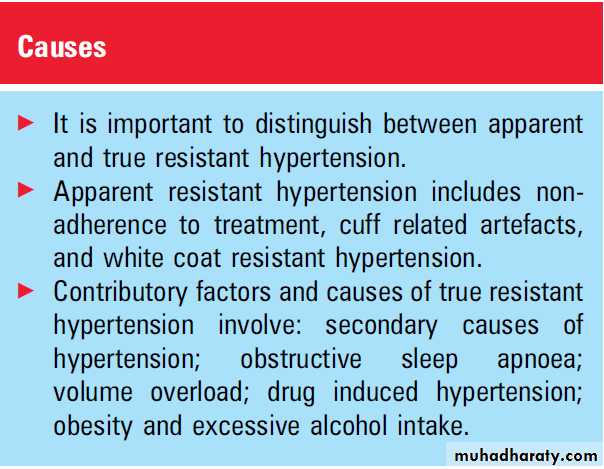
CAUSES
Resistant hypertension can be arbitrarily dividedinto two broad categories:
true resistance, and
apparent, spurious or false resistance.
The prevalence of apparent resistance appears to be considerably higher than that of true resistance.
Apparent resistant hypertension
Non-adherence to treatmentAn important cause of apparent resistance is
patient non-adherence to recommended lifestyle
measures and/or drug treatment. A substantial
number of patients discontinue their antihypertensive
treatment, which may be due to a number of reasons, such as side effects and cost of medications,lack of consistent and continuous primary care, lack of strong physician motivation, poor understanding of instructions, and social and cultural barriers.
Also the physician may be nonadherent and fail to follow guidelines for the management of hypertension. Surveys have indeed shown that physicians often fail to increase the number of drugs or the doses of drugs despite inadequate blood pressure control. The dosing
schedule may be inconvenient, chaotic and not
optimal, and may not include a diuretic or the most
appropriate diuretic.
Finally, the patient should be allowed to sit quietly for 5 min before blood pressure is measured.
Cuff related artefacts
The physician should be aware of cuff relatedartefacts. The cuff should be large enough so that
the air bladder encircles at least 80% of the upper
arm circumference and extends at least two thirds
of its length. Blood pressure is overestimated when
the cuff is too small for the arm. A rare cause of cuff
related artefact is so-called pseudo-hypertension due to non-compressibility of severely arteriosclerotic or calcified brachial and radial arteries.
White coat resistant hypertension
Approximately 20-25% of patients with persistentoffice blood pressures ≥140/90 mm Hg have
normal blood pressure on home blood pressure
measurement or ambulatory monitoring, usually
defined as awake blood pressure <135/85 mm Hg.
Similarly, patients with resistant hypertension in
the office may have normal out-of-office blood
pressure.
About a decade ago, Brown and colleagues
reported that 28% of 118 patients with
resistant hypertension, taking at least three antihypertensive drugs in combination, had normal
awake ambulatory blood pressure as defined above.
In the Spanish Ambulatory Blood Pressure Monitoring
Registry, 12.2% of 68 045 treated patients
had resistant hypertension, defined as office blood
pressure≥140 mm Hg and/or 90 mm Hg while
being treated with ≥3 antihypertensive drugs, one
of them being a diuretic.
After ambulatory blood pressure monitoring, 62.5% of them were classified as having true resistant hypertension and the remaining 37.5% as having white coat resistance. Asignificant white coat effect should be suspected in patients who show signs of over treatment, such as orthostatic hypotension, and in patients with chronically high office blood pressure without target organ damage.
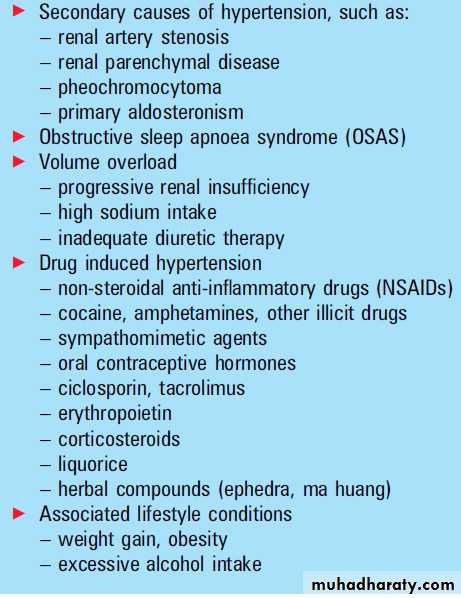
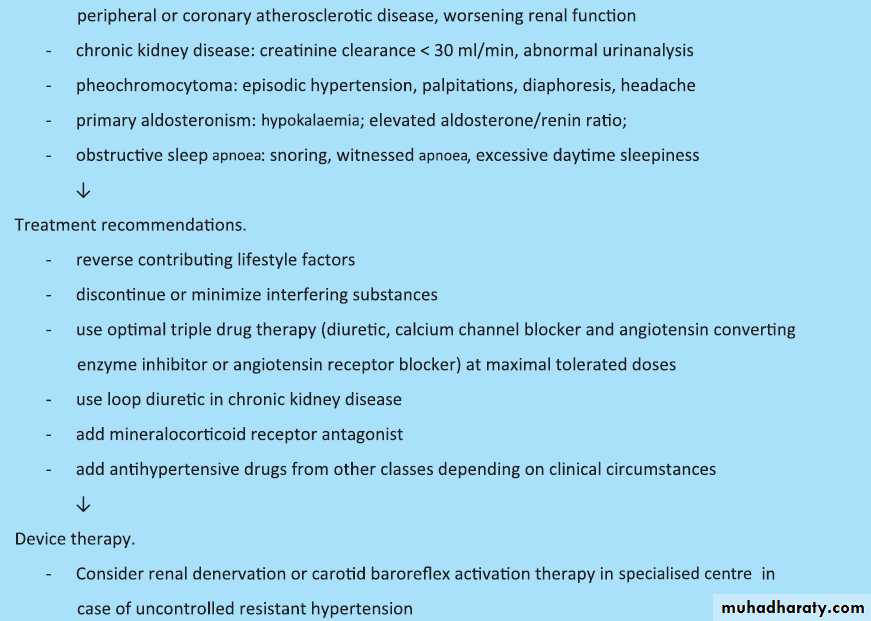
True resistant hypertension
A number of causes of true resistant hypertensionare listed in box 1. Resistant hypertension may be due to an unsuspected, specific, potentially curable
secondary cause of hypertension, such as renal
artery stenosis and pheochromocytoma. Recent
studies have indicated that primary aldosteronism
is more common in hypertension than generally
accepted and prevalence rates of about 20% have
been reported in resistant hypertension.
Obstructive sleep apnoea has been identified in 83% of 41consecutive patients with treatment resistant hypertension, and was both more common and more severe in men than in women. These
patients are usually obese, short necked, and fall
asleep at various time of the day. Volume overload
is frequently associated with resistant hypertension,
due to renal insufficiency, inadequate diuretic
therapy or high salt intake.
Salt sensitive patients are particularly prone to the effects of excessive salt. Furthermore, a number of illicit drugs such as cocaine and amphetamines, and other substances such as non-steroidal anti-inflammatory agents, pressor agents, and some non-traditional remedies may directly raise blood pressure or blunt the blood pressure lowering effect of antihypertensive
medications, or both. Finally, resistant hypertension
may be associated with obesity and heavy alcohol intake. Whether or not genetic factors play a role in resistance to treatment is currently under investigation.
TARGET ORGAN DAMAGE AND CLINICAL
COMPLICATIONSIn the NHANES survey, patients with resistant
hypertension were compared to patients with
controlled hypertension using one to three medications.
They were more likely to have reduced renal function and albuminuria. The prevalence of
the self reported medical histories of coronary heart
disease, heart failure, and stroke amounted to,
respectively, 22%, 10%, and 10% in resistant
hypertension, and to 9.4%, 4.1%, and 3.8% in
controlled hypertension (p<0.001 for all comparisons).
It should be noted that the age difference
was not taken into account in these univariable
analyses, whereas age averaged, respectively, 66.4
and 59.5 years in resistant and controlled hypertension.
In the Spanish study, patients with true
resistant hypertension were compared to those
with white coat resistant hypertension.
Patients with true resistant hypertension were younger,
comprised more men, had a worse risk profile withgreater prevalence of diabetes and smoking, more
organ damage, such as left ventricular hypertrophy,
reduced renal function and microalbuminuria, and
more cardiovascular complications.
In a prospective follow-up study, Salles and
colleagues investigated the importance of ambulatory blood pressure as a predictor of cardiovascular morbidity and mortality in 556 patients with resistant hypertension, representing 17% of patients in the outpatient clinic.Whereas office blood pressure showed no independent prognostic value, daytime and night-time systolic and diastolic blood pressure predicted a composite of fatal and non-fatal cardiovascular events after full adjustment, including office blood pressure, traditional
risk factors, and cardiovascular diseases at baseline.
The diagnosis of true resistant hypertension was
also an independent predictor of the composite end
point and all cause mortality, with a fully adjusted
hazard ratio of about 2 in comparison with white
coat resistant hypertension, and night-time
blood pressures were better predictors than daytime blood pressures, as also observed in the general hypertensive population.
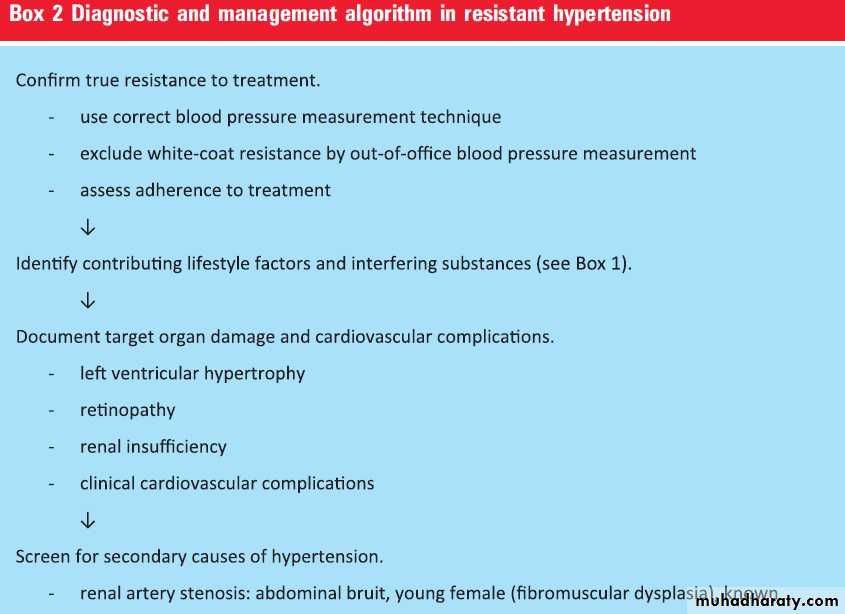
PATIENT EVALUATION
A first step in the evaluation of the patient withresistant hypertension is to confirm true resistance
to treatment by use of the correct blood pressure
measurement technique, and exclude apparent
resistance, such as white coat resistant hypertension,
by home or ambulatory blood pressure monitoring, and accurate assessment of treatment adherence.
Next, contributing lifestyle factors should be identified and reversed, and interfering substances should be discontinued or minimised.
Target organ damaged such as left ventricular
hypertrophy, retinopathy, and renal insufficiency
and clinical cardiovascular complications need to be
documented and patients should be screened for
secondary causes of resistant hypertension by
medical history, physical examination, biochemical
evaluation, and/or non-invasive imaging, with
particular attention paid to a number of symptoms
and signs as summarised in the algorithm in box 2.
Biochemical evaluation of the patient with treatment resistant hypertension should routinely include a metabolic profile including sodium, potassium, glucose, and creatinine; urinalysis; and plasma aldosterone and renin or renin activity. A24 h urine collection is useful to estimate dietary sodium and potassium intake, calculate creatinine clearance, and measure aldosterone excretion.
Urinary or plasma metanephrines/catecholamines
are indicated when pheochromocytoma issuspected. Non-invasive imaging is reserved for
patients in whom there is a suspicion of renal
artery stenosis or adrenal adenoma or tumour.
TREATMENT RECOMMENDATIONS
Treatment of patients with resistant hypertensionincludes appropriate lifestyle changes, discontinuation or minimisation of interfering substances, and use of effective multidrug regimens and device therapy. Although not specifically evaluated in patients with resistant hypertension, lifestyle changes to lower blood pressure include weight loss in case of overweight or obesity; moderate intensity exercise for a minimum of 30 min on most days of the week.
dietary salt reduction, ideally to
<100 mEq of sodium/24 h; and moderation ofalcohol intake to no more than two drinks per day
for most men and one drink per day for women or
lighter-weight persons. A high fibre, low fat diet is
also recommended. Specific treatment of secondary
causes of hypertension and obstructive sleep apnoea
is beyond the scope of the current review (box 2).
Drug therapy
Diuretic therapy
Resistant hypertension is often at least partly
related to lack of, or underuse of, diuretic therapy
necessary to control occult inappropriate volume
expansion. This condition would require adding
a diuretic, increasing the dose, or changing the
diuretic class.
The long acting thiazide diuretic chlorthalidone should be preferentially used in patients with resistant hypertension because it has
been shown to produce greater 24 h ambulatory
blood pressure reduction than hydrochlorothiazide,
with the largest difference occurring during the
night. Loop diuretics are usually reserved for
patients with chronic kidney disease, but may help
to increase blood pressure control in other patients.
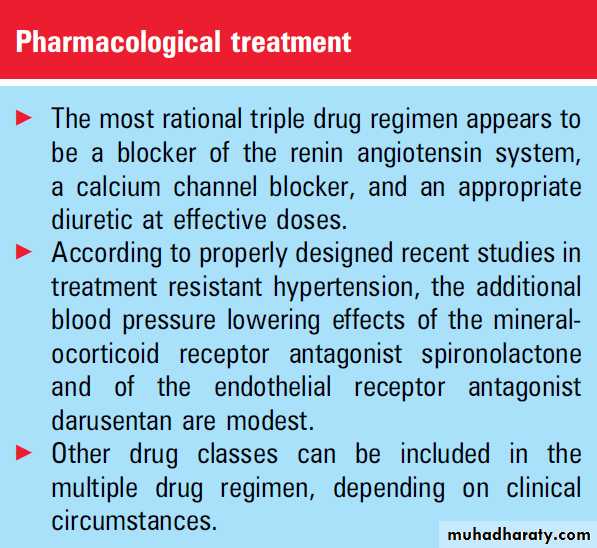
Drug combinations
Most combinations of two antihypertensive drugsproduce additive antihypertensive benefit. In recent
guidelines the following combinations are considered
most suitable because of their pronounced
blood pressure lowering effect, cardiovascular
protection, and optimal tolerability: thiazide
diuretic or calcium channel blocker with an ACE
inhibitor or angiotensin receptor blocker.
Although there are no hard scientific data, the combination of a thiazide diuretic, a calcium channel blocker, and a converting enzyme inhibitor or angiotensin receptor blocker, which act by complementary mechanisms, is probably the most rational triple drug regimen.
Other drugs, such as b-blockers, a-blockers, centrally acting agents, or potent vasodilators such as hydralazine or minoxidil, may be included in the multiple drug approach depending on the clinical circumstances, though adverse effects may be common.
The combined use of a b-blocker and a thiazide diuretic may potentiate the development of diabetes mellitus, particularly in the overweight or obese patient. The combination of a converting enzyme inhibitor and an angiotensin receptor blocker is not recommended because of the increased incidence of adverse effects and even some harm observed in the high risk patients of the ONTARGET trial.
Two types of drug the
mineralocorticoid receptor antagonist spironolactone and theendothelin receptor antagonist
darusentan have been evaluated as additional treatment in resistant hypertension and are discussed separately.
Mineralocorticoid receptor antagonists In the past decade a number of small uncontrolled trials have shown the beneficial effect of small doses of spironolactone in the lowering of blood pressure in patients with resistant hypertension.
For example, spironolactone 12.5-50 mg daily
lowered blood pressure by an additional 25/12 mm Hg in 76 patients with poorly controlledhypertension. In the non-randomised post hoc
analysis of the Anglo-Scandinavian Cardiac
Outcomes Trial Blood Pressure Lowering arm,
the addition of spironolactone to a triple drug
treatment regimen led to a significant decrease of
21.9/9.5 mm Hg.
However, the results of a properly designed placebo controlled trial were more modest. Vaclavik
and colleagues14 randomly assigned 117 patients
with resistant hypertension, defined as office blood
pressure >140/90 mm Hg despite treatment with
at least three antihypertensive drugs including
a diuretic, to receive 25 mg spironolactone or
a placebo as add-on therapy to their antihypertensive
medications.
The primary end point was daytime ambulatory blood pressure. After 8 weeks, the difference in mean blood pressure fall was 5.4 mm Hg for systolic blood pressure (p¼0.02) and 1.0 mm Hg for diastolic blood pressure (p¼0.36) in favour of the spironolactone group.
The difference amounted to 9.8 (p<0.01)/1.0 (p¼0.40) mm Hg for average 24 h blood pressure and to 6.5 (p¼0.01)/2.5 (p¼0.08) mm Hg for office blood
pressure. With regard to predictors of the response
to spironolactone, the authors observed that the
reduction of systolic 24 h blood pressure was
significantly greater in patients with low plasma
renin activity (p<0.01) or high aldosterone-to-renin
ratio (p¼0.02), and tended to be better in those
with low serum potassium (p¼0.07), but was not
related to serum aldosterone (p¼0.61).
The authors note that the appropriate dosing range for spironolactone has not been well defined in resistant hypertension, and that it is possible that a higher dose of the drug could have led to a greater blood pressure decrease.
Endothelin receptor antagonists
Two recent randomised, double blind, placebo controlled trials assessed the potential role of the new vasodilatory, selective endothelin type A antagonist darusentan in, respectively, 379 and 849 patients with systolic blood pressure ≥140 mm Hg (≥130 mm Hg in case of diabetes or chronic kidney disease) who were receiving at least three blood pressure lowering drugs, including a diuretic, at full or maximum tolerated doses.In the first study15 patients were randomly assigned to 14 weeks’ treatment with placebo or darusentan 50 mg, 100 mg or 300 mg taken once daily. The mean reductions in office blood pressure were 9/ 5 mm Hg with placebo and 17/10, 18/10 and 18/ 11 mm Hg with the three doses of darusentan (p<0.001 for all effects).
Oedema or fluid retention occurred in 27% of the patients given darusentan compared with 14% given placebo; five patients on darusentan had cardiac related serious adverse events. In the second trial,16 patients were randomised to darusentan, placebo or the central α2agonist guanfacine.
Decreases from baseline to week 14 in office blood pressure (the primary end point) for darusentan (15 mm Hg) were greater than for guanfacine (12 mm Hg, p<0.05) but not greater than for placebo (14 mm Hg).
Darusentan, however, reduced mean 24 h systolic
blood pressure (9 mm Hg) more than placebo
(2 mm Hg) or guanfacine (4 mm Hg) (p<0.001
for each comparison).
Fluid retention/oedema was present in 28% of the patients on darusentan versus 12% in each of the other groups. The overall results suggest that selective endothelial receptor antagonists may have a role in the treatment of resistant hypertension, but there is concern about volume retention and potential exacerbation of heart failure, and the long term benefit is not known.
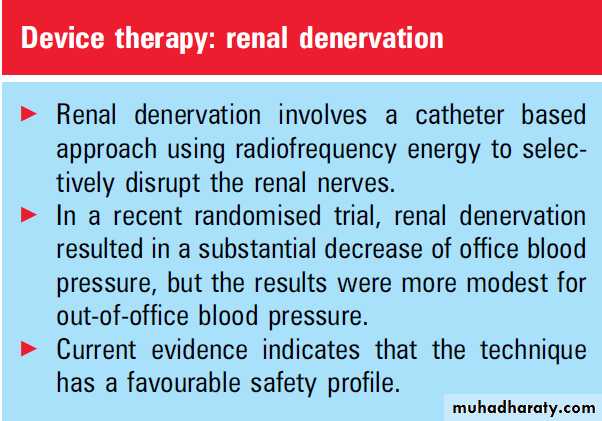
Device therapy
Renal denervationEfferent sympathetic outflow to the kidney stimulates renin release, increases tubular sodium
reabsorption, and reduces renal blood flow; afferent
signals from the kidney modulate central sympathetic
outflow and contribute to neurogenic hypertension.
Based on the evidence of the role of renal sympathetic nerves in various aspects of blood pressure control, a catheter based approach using radiofrequency energy to selectively target and disrupt the renal nerves has been developed.
Following observational safety and feasibility studies, the Symplicity HTN-2 Trial, a multicentre, prospective randomised trial,18 was performed in patients who had a baseline systolic blood pressure ≥160 mm Hg (≥150 mm Hg for patients with type 2 diabetes) despite taking three or more antihypertensive drugs.
Patients were taking a median of five medications, and diuretics, including spironolactone, were used in more than 89% of them.
Secondary hypertension and white coat hypertension
were not defined as exclusion criteria. One
hundred and six patients were randomised to
undergo renal denervation with previous treatment
(n¼52) or to maintain previous treatment (n¼54);
the control group did not undergo a sham procedure, which would have provided double blinding.
After 6 months, office blood pressure was reduced by 32/12 mm Hg from the baseline value of 178/
96 mm Hg (p<0.001) in the renal denervation
group, whereas blood pressure in the control group
changed by 1/0 mm Hg from 178/97 mm Hg at
baseline (p>0.75).
Between-group differences in blood pressure at 6 months amounted to 33/11 mm Hg (p<0.001). Systolic blood pressure was <140 mm Hg in 39% and 6% of the patients, respectively (p¼0.04). Results on home blood pressure and 24 h ambulatory blood pressure in smaller numbers of patients were roughly concordant, although less pronounced.
For example, 24 h blood pressure recordings, available in 20 patients in the renal denervation group, showed a mean decrease of 11/7 mm Hg, whereas blood pressure did not change significantly for the 25 patients in the control group (3/1 mm Hg). There were no serious procedure related or device related complications and occurrence of adverse events did not differ between groups.
There were no adverse effects on the kidney, and this was also the case for patients with impaired renal function In summary, the available evidence indicates that catheter based renal denervation has a favourable safety profile and results in potentially substantial and sustained blood pressure reduction in patients with drug resistant hypertension. In pilot studies, no loss of antihypertensive response was evident with follow-up of
2 years. Effects on cardiovascular morbidity and
mortality are currently unknown.
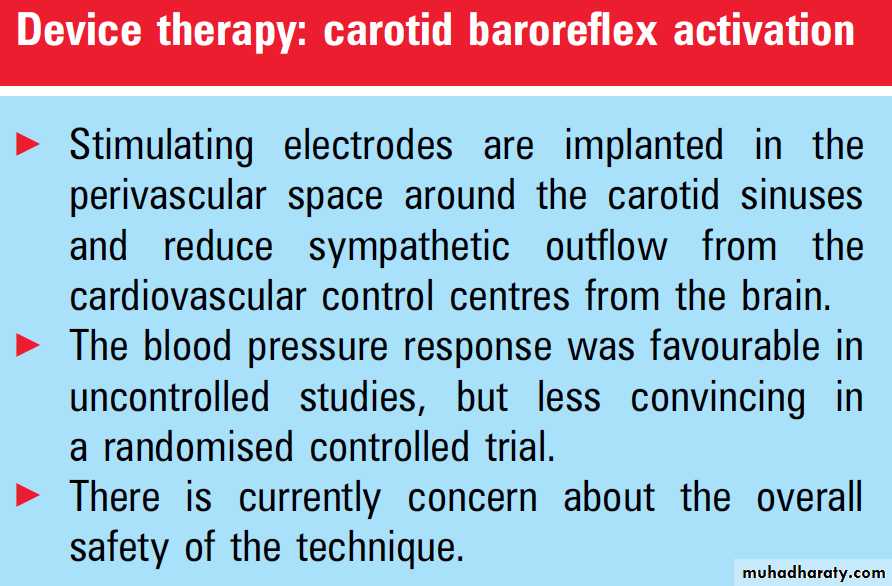
Carotid baroreflex activation
Another device based therapy of resistant hypertension is carotid baroreflex activation, in which stimulating electrodes are implanted in the perivascular space around the carotid sinuses. The Rheos Baroreflex Hypertension Therapy System enhances afferent nerve traffic from the baroreceptors to the cardiovascular control centres of the brain, which subsequently reduce sympathetic outflow and blood pressure.The Device Based Therapy in Hypertension Trial was a multicentre, prospective, non-randomised feasibility study. Its purpose was to assess the safety and efficacy of the Rheos system over 3 months in 45 patients with resistant hypertension, defined as blood pressure ≥160/90 mm Hg despite receiving at least three antihypertensive agents including a diuretic;the median number of medications was five.
Medications were kept constant for 2 months
before entry and during the first 3 monthsof therapy, except when medically necessary. In the
37 evaluable patients after 3 months, the change
in office blood pressure averaged 21/12 mm Hg
from a baseline value of 179/105 mm Hg, and
heart rate decreased by 8 beats/min (bpm) from
80 bpm at baseline.
The reduction in 24 h systolic and diastolic blood pressure, and heart rate, monitored in 26 subjects, amounted to, respectively, 6 mm Hg (p¼0.10), 4 mm Hg (p¼0.04), and 5 bpm (p<0.001). Seventeen subjects completed 2 years of device therapy, at which time office blood pressure had decreased by 33/22 mm Hg (p<0.01) and 24 h blood pressure by 24/13 mm Hg (p<0.05).
The non-randomised cohort of 10 eligible patients who had declined participation in the trial failed to show a significant change in office blood pressure. With regard to safety, seven patients experienced a procedure related serious adverse event and one patient a device related serious adverse event. Serum creatinine remained unchanged after 3 months and increased significantly after 12 months in 22 participants. There was no evidence of orthostatic hypotension.
In a multicentre randomised study, presented at the 61st Annual Scientific Session of the American
College of Cardiology in April 2011,20 the Rheos
system was implanted in 265 patients with resistant
hypertension ≥160/80 mm Hg. All patients,whose office blood pressure averaged 178/103 mm Hg, were implanted with the device, and then randomised in a 2:1 ratio to baroreflex activation therapy for 12 months (group A) or control treatment for the first 6 months, with the system switched off, followed by baroreflex activation therapy for the following 6 months (group B).
At the end of the 6 month double blind period, the
percentage of patients with ≥10 mm Hg systolicblood pressure reduction was 54% in group A and
46% in group B (p¼0.97); the difference of 7.7% did
not achieve the goal difference of >20%. Systolic
blood pressure was 140 mm Hg or less in, respectively,
42% and 24% (p¼0.005) at 6 months.
Of the 97 responders in group A after 6 months, 88% were considered sustained responders after 12 months.
When groups A and B were combined, systolic
blood pressure was 140 mm Hg or less in over 50%
of the patients after 12 months.
With regard to safety, the authors concluded that the end point of long term device safety was met whereas the end point of short term procedure related adverse
events was not.
Only 75% of patients were free of procedural adverse events at 30 days, but 76% of adverse events fully resolved. The authors concluded that the results justify further development and investigation of baroreflex activation therapy.
PERSPECTIVES
Because of some variability in the definition of treatment resistant hypertension in different studies, which limits their comparability to some extent, there is need for one and the same universal definition.
The prevalence of resistant hypertension varies among studies but the true prevalence will probably remain unknown because a prospective study with forced and flexible drug titration may never be performed in the general hypertensive population.
The techniques to distinguish between apparent and true resistant hypertension are available and the causes of true resistance are well known, but more work is needed to determine whether or not genetic factors are involved. Apart from the management of
specific causes of resistant hypertension, an armamentarium of antihypertensive drug classes and
drugs are available for the treatment of primary
resistant hypertension.
Rational combinations of three complementary drug classes have been proposed, but have in fact never been tested in randomised controlled trials or outcome studies.
The potential of higher doses of spironolactone
and of newer more selective endothelin type A
receptor antagonists as add-on therapy should be
further explored.
Because of the heterogeneous pathophysiology of hypertension, development of drugs which target new mechanisms are still welcome.
Renal denervation and carotid baroreflex activation therapy have recently been shown to decrease blood pressure on top of multiple drug therapy in resistant hypertension; however, there is still a need for a properly designed double blind trial for renal denervation therapy and the safety concern for carotid baroreflex activation therapy should be resolved. Furthermore it would be of interest to know if the blood pressure lowering effects of the two types of device therapy are additive, which would be helpful in case of
persistent resistance after application of one of them.