د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Tachyarrhythmias
• Tachyarrhythmias• Key points
• Consider electrical cardioversion for an arrhythmia if there are signs of haemodynamic compromise, chest pain, or heart failure .Always presume that a broad complex arrhythmia is ventricular tachycardia, even if it is haemodynamically well tolerated.Patients who have had atrial flutter and fibrillation for more than 48 hours should not be chemically or electrically cardioverted until they have had adequate anticoagulation or you have excluded intracardiac thrombus with
• a transoesophageal echocardiogram.
Clinical tips
Use vagal manoeuvres or intravenous adenosine to slow atrioventricular (AV) conduction and help to distinguish a supraventricular tachycardia from ventricular tachycardia.Try and obtain a previous ECG in sinus rhythm to look for clues about the mechanism of the presenting arrhythmia.
Check serum electrolytes - in particular potassium, magnesium, and calcium - and correct imbalances as soon as possible
Tachycardia is defined as a heart rate greater than 100 beats a minute. Pathological tachycardia, or tachyarrhythmia, results from disorders of:
• The mechanism of generation of the cardiac impulse.
• Conduction of the cardiac impulse.
Classification of tachyarrhythmias according to ECG appearance
AVNRT = atrioventricular nodal re-entrant tachycardia; AVRT = atrioventricular re-entrant tachycardia; VT = ventricular tachycardia; AF = atrial fibrillationTachyarrhythmias may also be classified according to the localisation of the circuit
Classification of arrhythmias by locationAtrial arrhythmias
• Inappropriate sinus tachycardia• Sinus node re-entry
• Atrial flutter
• Atrial fibrillation
• Focal atrial tachycardia
• Multifocal atrial tachycardia
Ventricular arrhythmias
• Scar related monomorphic ventricular tachycardia
• Normal heart VT (outflow tract and fascicular ventricular tachycardia)
• Polymorphic ventricular tachycardia
Arrhythmias involving the AV node
• Atrioventricular nodal re-entrant tachycardia (AVNRT)
• Atrioventricular re-entrant tachycardia (AVRT)
The QRS complex in the ECG may be regular or irregular, narrow or broad when the QRS complex is longer than 120 milliseconds. This gives rise to four groups of tachyarrhythmia:
• Irregular narrow complex
• Regular narrow complex
• Irregular broad complex
• Regular broad complex.
Arrhythmia circuits may arise solely from the atria or the ventricles and are described as atrial and ventricular tachycardias respectively. Atrioventricular nodal re-entrant tachycardia (AVNRT) and atrioventricular re-entrant tachycardia (AVRT) require the participation of the AV node as part of their circuit.
The symptoms common to tachyarrhythmias include:
PalpitationsShortness of breath
Chest pain
Dizziness
Syncope.
You should attempt to record an ECG at the time of the symptoms occurrence to help with the correct diagnosis and treatment.
When you take a history from a patient suspected of having a tachyarrhythmia, you should ask about:
A family history of sudden cardiac death. This may raise the suspicion of an inherited condition related to abnormal cardiac ion channel function, such as the long QT syndrome (LQTS) or Brugada syndrome
A past history of coronary artery disease, cardiac surgery, structural heart disease, or left ventricular dysfunction.
This may raise the possibility of atrial fibrillation or ventricular arrhythmias
A full drug history of both prescribed and non-prescribed medication. Some drugs may cause QT prolongation, predisposing patients to intermittent polymorphic ventricular tachycardia.Clinical examination during a broad complex tachycardia may provide a clue to the diagnosis. You should assess for signs of AV dissociation, such as a variable intensity of the first heart sound and intermittent cannon waves in the jugular venous pressure, which may suggest a diagnosis of ventricular tachycardia.
Tachyarrhythmias may be well tolerated, although a rapid heart rate may impair ventricular function and thereby reduce cardiac output, blood pressure, and coronary blood flow. A sustained arrhythmia may therefore lead to the circulation being compromised or heart failure.
Signs of AV dissociation, such as a
• variable intensity of the first heart sound and• intermittent cannon waves in the jugular venous pressure, which may suggest a diagnosis of ventricular tachycardia.
You should refer patients with these symptoms to a cardiologist for further investigation. These investigations include:
• Holter monitoring
• Implantation of a loop recorder if the symptoms are brief and infrequent
• An invasive intracardiac electrophysiology study, which may be necessary to define the mechanism of the arrhythmia and allow curative ablation.
Treatment
If there are signs of haemodynamic compromise, chest pain, or heart failure in a patient with an arrhythmia, then immediate synchronised electrical cardioversion should be performedLearning bite
1.Electrical cardioversion should be performed for any arrhythmia if there are signs of haemodynamic compromise, chest pain, or heart failure.Other available treatment options include 2.antiarrhythmic drugs,
3.overdrive electrical pacing, and percutaneous 4.catheter ablation.
Regular narrow QRS tachyarrhythmias
Sinus tachycardia and sinus node re-entry tachycardia
Sinus tachycardia
This is usually a physiological response to autonomic stimuli such as exercise, hypotension, sepsis, thyroid disease, or sympathomimetic drugs.
The ECG will show a P wave prior to every QRS complex, with a normal P wave axis, and it will be positive in lead II.
Occasionally, it may be difficult to distinguish the P wave from the preceding T wave.
Sinus tachycardias accelerate and decelerate gradually, unlike paroxysmal tachyarrhythmias, which tend to have a sudden onset and termination.Inappropriate sinus tachycardia is a paroxysmal arrhythmia that can be sustained and may not have any apparent precipitant. It is not common and the mechanism is not completely known.
Sinus node re-entry tachycardia
This is a rare paroxysmal tachycardia with the P wave morphology identical to sinus rhythm, having a rate of 130 to 140 beats a minute. It has an abrupt onset and termination, and it can be initiated with programmed electrical stimulation during an electrophysiology study.Management
Sinus tachycardia and sinus node re-entry tachycardia seldom require treatment. If the patient is symptomatic, you should consider treatment with beta blockers. Catheter ablation, however, is rarely required and carries the risk of sinus node dysfunction and bradycardia.
Focal and multifocal atrial tachycardia
Atrial tachycardias arising from ectopic foci account for 10% of narrow complex tachycardias, as shown in figure 2A.They may originate from a single focus when they are described as unifocal; they have a single P wave morphology and axis
Alternatively, they may arise from several foci and are described as multifocal. Multifocal atrial tachycardia is common amongst elderly patients and those with respiratory disease. Rarely, multifocal atrial tachycardia may result from digoxin therapy. These tachycardias have variable P wave morphologies, PR intervals, and degrees of AV block
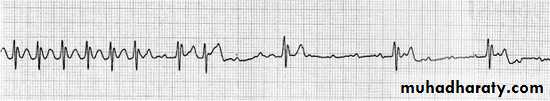
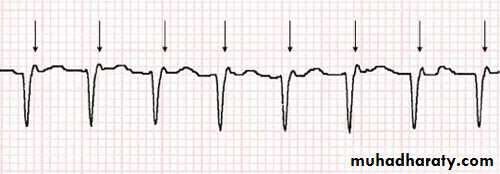
Figure 2A: Rhythm strip of a regular narrow complex tachycardia during administration of adenosine, which has revealed an atrial tachycardia
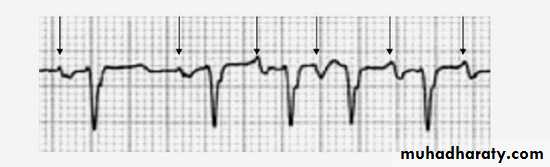
Figure 2B: Rhythm strip of multifocal atrial tachycardia. The black arrows denote P waves of variable morphology and PR intervals
The atrial rate in both these arrhythmias is usually 150 to 250 beats a minute, and the ventricular rate depends on the degree of AV conduction.
Atrial tachycardias may cause a dilated cardiomyopathy and heart failure if they are not treated.
Management
Control the ventricular rate using:Drugs that slow AV node conduction such as beta blockers, calcium channel blockers, and digoxin
Alternate drugs include sotalol, amiodarone, flecainide, or propafenone, usually prescribed with a low dose AV blocking drug to prevent acceleration of AV conduction,2 in the absence of ischaemic or structural heart disease.
Also consider treating patients with unifocal atrial tachycardias by means of percutaneous catheter ablation, which has been shown to have good long term results.
Atrial flutter
This is a right atrial arrhythmia where the atria contract at a rate of approximately 300 beats a minute but the ventricular rate is usually approximately 150 beats a minute when there is 2:1 AV node block. Other ratios of conduction block can also occur. Flutter with 1:1 AV conduction may be associated with haemodynamic collapse.The ECG of the more common or “typical” atrial flutter shows P waves that are upright in V1 and negative in the inferior leads, creating a saw tooth pattern (as shown in figure 3A).
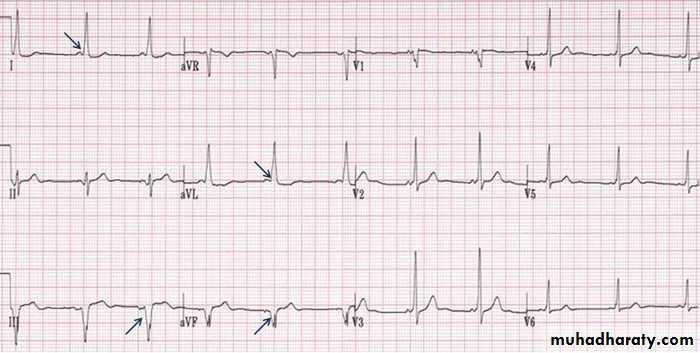
Figure 3A: ECG appearance of typical atrial strip showing atrial flutter with negative P waves inferiorly (leads II, III, and aVF) and a positive P wave in lead V1
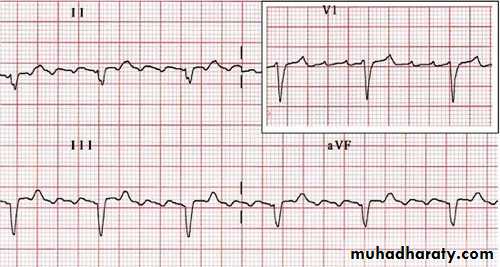
The QRS complexes may be regular or irregular if there are variable ratios of AV block. The less common “reverse typical” atrial flutter produces positive P waves inferiorly and a negative P wave in lead V1, as shown in figure 3B.
Figure 3B: 12 lead ECG of “reverse typical” atrial flutter with positive P waves inferiorly (leads II, III, and aVF) and a negative P wave in lead V1
Management
Once atrial flutter has been diagnosed, the ventricular rate can by slowed by drugs acting on the AV node, such as beta blockers, calcium channel blockers, or digoxin.Atrial flutter is associated with an increased risk of atrial thrombus formation and thromboembolism, which may lead to ischaemic stroke. All patients with atrial flutter should be treated with anticoagulant drugs and offered curative ablation therapy, given that the recurrence of atrial flutter is extremely high despite treatment with antiarrhythmic drugs.
Ablation therapy involves the application of radiofrequency energy or cryothermy to a region of the myocardium between the tricuspid valve and inferior vena cava, which is critical to the circuit of atrial flutter. It is a relatively safe and straightforward procedure. There is a 1% risk of complete heart block, requiring permanent pacing, but the success rate is high (approaching 95% cure).
You should refer patients who have atrial flutter with 1:1 AV conduction for urgent ablation following initial emergency treatment.
Atrioventricular nodal re-entry tachycardia (AVNRT)
Responsible for approximately 60% of narrow complex tachycardias. This arrhythmia occurs in people who have two atrial conduction paths into their AV node. A perpetual circuit is formed involving these pathways with passive excitation of the atria and ventricles, which occurs near simultaneously. Therefore, the ECG has the appearance of a narrow complex tachycardia with a retrograde inverted P wave, either hidden in the QRS complex or visible shortly afterwards, particularly in lead V1, as shown in the rhythm strip in figure 4.Figure 4: Rhythm strip from lead V1 demonstrating retrograde P wave activity occurring shortly after the QRS complex (arrows)
Management
You should attempt to terminate AVNRT by performing the vagal manoeuvres. These include:The Valsalva manoeuvre, which is the safest manoeuvre and is simple to perform
Carotid sinus massage, but only in the absence of a history of carotid disease and used with caution in the elderly .Application of an ice pack to the face may be effective for children.These manoeuvres may slow or block AV nodal conduction and terminate AVNRT.
A bolus of intravenous adenosine (6 to 18 mg), infused rapidly over a few seconds, followed by a rapid saline flush, has a similar effect.
Given that dipyridamole potentiates adenosine's effects, adenosine should be avoided in patients taking dipyridamole, and intravenous verapamil can be used instead.
If adenosine and verapamil are unsuccessful, you should consider an intravenous class IC drug such as flecainide if the patient has a structurally normal heart.
Once the arrhythmia has terminated you should start the patient on an AV nodal blocking drug, such as a beta blocker or calcium channel blocker at a low dose. This will need to be continued long term in order to reduce the risk of recurrence of the arrhythmia.
Curative catheter ablation has a high success rate, but does carry a 1% risk of AV node damage that will require permanent pacing. So if your patient declines ablation, they can be managed medically.
Atrioventricular re-entrant tachycardia (AVRT)
Atrioventricular re-entrant tachycardia, or AVRT, is maintained by a circuit involving the native conduction system and an accessory pathway between the atria and ventricles.Accessory pathways are anomalous strands of conducting myocardial tissue that bridge the annulus of the AV valve, and they are capable of rapid conduction.
There are two types of AVRT:
Orthodromic : anterograde conduction to the ventricles occurs via the AV node and retrograde conduction to the atria via the accessory pathway
Antidromic : anterograde ventricular activation occurs via the accessory pathway and retrograde atrial activation via the AV node. This causes a regular broad QRS tachycardia.
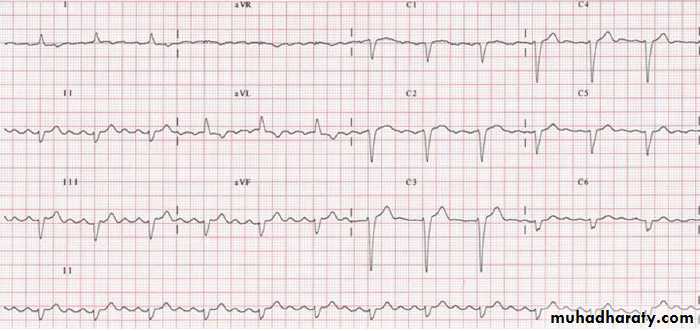
During sinus rhythm the PR interval can be short and ventricular pre-excitation may be seen in the form of a delta wave, as shown in this ECG.
Figure 5: Ventricular pre-excitation on a 12 lead ECG with a short PR interval and delta wave visible in several leads (see arrows)
The ECG may be normal in some patients with AVRT. This includes patients where:
• There is a concealed accessory pathway which only conducts retrogradely from the ventricle to the atrium, and therefore does not cause ventricular pre-excitation and a delta wave.• The accessory pathway is far from the sinoatrial node, as in a left lateral pathway, in which case the ventricles are predominantly activated via the AV node.
The ECG appearance in these types of tachycardia may be indistinguishable from an atrial tachycardia or AVNRT. In some cases retrograde activation is seen in between QRS complexes, as shown in this rhythm strip.
Figure 6: Rhythm strip from a patient during AVRT. Note the clearly discernable retrograde atrial activity (arrows) midway between QRS complexes
Management
Termination of AVRT can be achieved by blocking conduction through the AV node. This can be accomplished with:Vagal manoeuvres
Adenosine (if this fails you should consider alternative drugs, such as flecainide or propafenone, which increase the refractory period of the anterograde part of the accessory pathway and terminate the arrhythmia)
Intravenous amiodarone is another option, but requires a prolonged infusion
Electrical cardioversion should be considered if drugs have failed or if there is evidence of your patient being haemodynamically compromised Maintenance of sinus rhythm in patients with recurrent, symptomatic episodes may be achieved with one of the following drugs:
• A beta blocker
• A calcium channel blocker
• Class IC antiarrhythmics (for example, flecainide and propafenone)
• Amiodarone
Ablation of the accessory pathway. This is an effective way of treating AV re-entrant tachycardias, with a success rate of greater than 95%.8 Serious complications are rare and include:
• Irreversible block of the AV node that will require permanent pacing, particularly in AVNRT ablations and where the accessory pathway lies close to the AV node
• Cardiac tamponade
• Ablation of left sided pathways carries a small risk of stroke of less than 1%.
Learning bite: Wolff-Parkinson-White syndrome
Wolff-Parkinson-White syndrome refers to the clinical presentation of the association between ventricular pre-excitation and palpitations due to AVRT. Patients may present with syncope, rather than palpitations, when atrial arrhythmias are conducted rapidly over the accessory pathway to the ventricles, bypassing the AV node and resulting in haemodynamic collapse. All patients with evidence of ventricular pre-excitation on their ECG should therefore be referred to an electrophysiologist to assess the conduction properties of the accessory pathway, in particular the risk of pre-excited atrial fibrillation.For those patients with evidence of ventricular pre-excitation and a delta wave on their ECG, you can use the ECG to find the approximate location of the accessory pathway. You can localise it to the left or right side of the heart by assessing the polarity of the delta wave in lead V1:
A left sided pathway may give rise to a positive delta wave in V1 and may cause right bundle branch morphology
A right sided pathway may give rise to a negative delta wave in V1 and may cause left bundle branch morphology. This is because septal activation is initiated from the right side of the septum.
Although detailed algorithms have been published, the precise location of the accessory pathway is generally defined with internal mapping catheters.
If a patient with suspected Wolff-Parkinson-White syndrome develops a broad complex tachycardia, then you should avoid AV nodal blocking drugs. This is because these may increase ventricular activation over the accessory pathway and cause a dangerously fast heart rate.
Instead, you should give an intravenous class IC drug such as flecainide, or a class III drug such as amiodarone.
Irregular narrow complex tachyarrhythmias
Atrial fibrillation
Atrial fibrillation is the most common arrhythmia in clinical practice. It is thought to be caused by the interaction between ectopic atrial triggers within the pulmonary veins and alterations to the electrical and structural properties of the atrial myocardium.11 Atrial fibrillation is a progressive disease with an increase in stability of the arrhythmia over time, so the chances of restoring sinus rhythm diminish the longer it is sustained. The common causes of atrial fibrillation are outlined in table 2.
Table 2: Causes of atrial fibrillation
Cardiac• Hypertensive heart disease
• Ischaemia
• Rheumatic heart disease
• Cardiomyopathy
• Sick sinus syndrome
Non-cardiac
Thyrotoxicosis
Infection
Electrolyte abnormalities
Alcohol
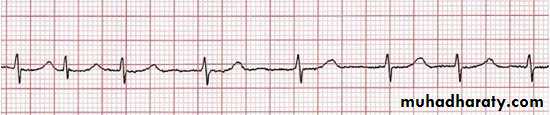
Figure 7: Rhythm strip from a patient during atrial fibrillation
During atrial fibrillation there is disorganised atrial activity with no P waves, as shown in this rhythm strip.
During atrial fibrillation the atria discharge with a rate of 400 to 600 beats/min. There are irregular QRS complexes, with a rate that is usually less than 200 beats/min.
There are three main categories of atrial fibrillation:
Paroxysmal - when it is intermittent, recurrent, and self terminating
Persistent - when the duration is greater than seven days. It will not self terminate, but can be cardioverted to sinus rhythm
Permanent - when atrial fibrillation has been accepted and attempts to cardiovert to sinus rhythm have been abandoned.
Occasionally, the ventricular rate may become regular when there is complete heart block, leading to a junctional escape rhythm. This is sometimes described as slow atrial fibrillation with regular rhythm.
Management of paroxysmal atrial fibrillation
Acute managementEither electrical or chemical cardioversion to sinus rhythm can be considered. If the onset of atrial fibrillation is unknown, or more than 48 hours prior to presentation, therapeutic anticoagulation is compulsory for six weeks before cardioversion due to the risk of a stroke. Patients should therefore have their rate controlled while awaiting cardioversion.
Where cardioversion is required urgently,
atransoesophageal echocardiogram can be performed to exclude thrombus in the left atrium.When cardioversion is successful, anticoagulation should be continued for a minimum of six weeks because the risk of thrombus formation in the left atrium persists despite restoring sinus rhythm
If the onset of atrial fibrillation is less than 48 hours prior to presentation, the patient does not require anticoagulant therapy or a transoesophageal echocardiogram.
Intravenous flecainide should be considered for patients with good ventricular function.
Intravenous amiodarone is safer in patients with a history of structural heart disease or coronary disease. Oral drugs such as sotalol may be used, but their effect is slower.
Long term management
Drug treatment to maintain sinus rhythm:
Maintenance of sinus rhythm following cardioversion to sinus rhythm can be achieved with the prescription of regular beta blockers, sotalol, or flecainide. Amiodarone is more effective than these drugs and is safest in the context of structural heart disease or ischaemia. However, it has a number of side effects and you need to monitor the patient’s thyroid and lung function carefully, so it is generally reserved for short term use
Curative ablation:
Ablative strategies for atrial fibrillation can be percutaneous or surgical. The aim is to either isolate triggers within the pulmonary veins or to alter the atrial substrate with atrial ablation. This procedure has a high success rate in paroxysmal atrial fibrillation, but is less successful for the ablation of persistent atrial fibrillation.Although repeat procedures are frequent, studies suggest that after one or two procedures the proportion of patients who no longer have atrial fibrillation after one year is approximately 60% to 70% in selected centres.
The most serious risks associated with catheter ablation are stroke, cardiac tamponade, and oesophageal fistula, which occur in approximately 2% to 5% of cases.
Surgical ablation involves the removal of the left atrial appendage, which is the place where clots form in the left atrium, in addition to pulmonary vein isolation18
Stroke prophylaxis:
The risk of thromboemboli can be reduced with antiplatelet and warfarin therapy. You should treat high risk patients with anticoagulant therapy according to the CHADS2 scoring system. In this system patients are allocated a score based upon the presence of the following risk factors:• Congestive cardiac failure
• Age over 75 years
• Hypertension
• Diabetes
• Stroke
The history of stroke is allocated two points and each of the other risk factors is allocated a single point. Patients are considered high risk for stroke and should be treated with anticoagulant therapy if they have a score of two points or more. Patients with a single point can be offered aspirin for stroke prophylaxis.
Management of persistent or permanent atrial fibrillation
Acute management
If a patient with persistent or permanent atrial fibrillation presents with a fast ventricular rate, you should aim to achieve control of this with the use of beta blockers, with or without the aid of calcium channel blockers such as diltiazem or verapamil, unless there is evidence of heart failure or hypotension .
Verapamil should not be prescribed for patients taking beta blockers due to the risk of profound AV block and hypotension.
Digoxin is widely used for control of the ventricular rate, but is not recommended as a first line drug because it does not control the heart rate in ambulant patients.
Long term management
Rate control:You should control the patient’s heart rate with the use of beta blockers, calcium channel blockers, and digoxin to maintain a mean heart rate of less than 80 beats a minute.
Ablate and pace:
You may be able to manage patients with paroxysmal or permanent atrial fibrillation, who are unable to tolerate medication or do not respond to other approaches, with ablation of the AV node and implantation of a permanent pacemaker. This is known as the “ablate and pace” strategy. Although it may improve symptoms, it will render the patient dependent on a pacemaker. You must also persist with anticoagulant therapy because the atria continue to fibrillate, and thus the risk of stroke is unchanged.
Ablate and pace:
You may be able to manage patients with paroxysmal or permanent atrial fibrillation, who are unable to tolerate medication or do not respond to other approaches, with ablation of the AV node and implantation of a permanent pacemaker. This is known as the “ablate and pace” strategy. Although it may improve symptoms, it will render the patient dependent on a pacemaker. You must also persist with anticoagulant therapy because the atria continue to fibrillate, and thus the risk of stroke is unchanged.Stroke prophylaxis:
These patients are managed in the same manner as those with paroxysmal atrial fibrillationBroad QRS tachyarrhythmia
Causes of broad complex tachycardia• Ventricular tachycardia, monomorphic or polymorphic
• Accessory pathway mediated antidromic AVRT, where the circuit involves ventricular activation via the pathway and atrial activation via retrograde AV node conduction
• Atrial tachycardia, AVNRT, or AVRT conducted with an aberrant right bundle branch block or left bundle branch block .
• Atrial tachycardia, AVNRT, or AVRT conducted via an accessory pathway.
• Atrial tachycardia which is being tracked by a pacemaker (pacemaker mediated tachycardia).
Regular broad QRS complex tachyarrhythmia
Ventricular tachycardia
Ventricular tachycardia is defined as:
Three or more ventricular extrasystoles in succession at a rate of greater than 120 beats/min.
The QRS complex is typically very wide, longer than 140 milliseconds, because the ventricular myocardium conducts at a slow conduction velocity relative to the AV node. It often originates from the left ventricle, so has right bundle branch block morphology.
Most cases of ventricular tachycardia occur in the context of structural heart disease, which provides a substrate for re-entrant arrhythmias. Approximately 10% of ventricular tachycardias occur in the absence of structural heart disease, and these can include outflow tract ventricular tachycardia and idiopathic left ventricular tachycardia.
Ventricular tachycardia may degenerate into ventricular fibrillation and accounts for approximately 80% of sudden cardiac deaths due to fatal arrhythmia.
Ventricular tachycardia can be defined according to duration, site of origin
(left or right ventricle), or morphology (monomorphic or polymorphic):Ventricular tachycardia lasting for
less than 30 seconds is defined as “non-sustained”
Ventricular tachycardia is described as having:
Right bundle branch block morphology - if the terminal portion of the QRS complex in V1 is positive and suggests activation from the left ventricle or septumLeft bundle branch block morphology - if the terminal portion of the QRS complex in V1 is negative and suggests activation from the right ventricle
An inferior axis (positive QRS in aVF, negative in V1) - suggests activation from the outflow tracts
A superior axis (negative QRS in aVF, positive in V1) - suggests activation from the apex
A relatively narrow QRS (100 to 120 ms) implies a septal focus
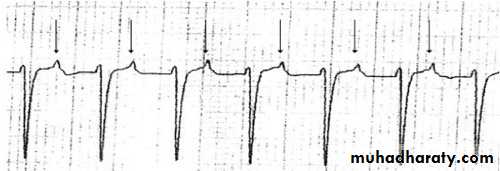
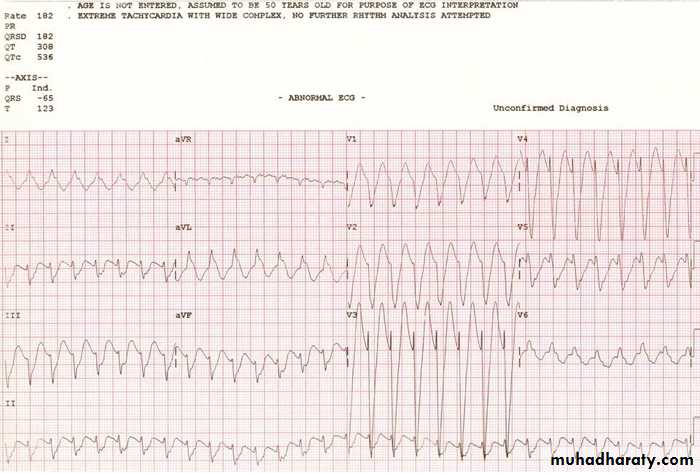
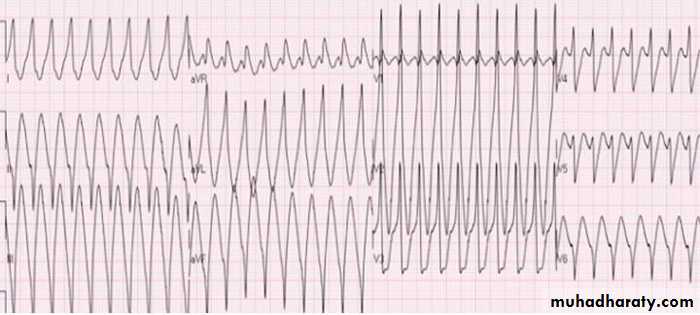
Monomorphic ventricular tachycardia has a constant QRS morphology that is consistent with a single re-entrant circuit, as shown in the ECG in figure 8.
Figure 8: ECG showing monomorphic ventricular tachycardia
It can be difficult to distinguish ventricular tachycardia from other causes of a broad complex tachycardia, and electrophysiological testing may be required in order to make a definitive diagnosis. Table 3 lists features that make ventricular tachycardia likely.21
Table 3: Features that make a broad complex tachycardia likely to be ventricular tachycardia
History
Advanced ageA history of myocardial infarction, coronary artery disease, structural heart disease, or left ventricular dysfunction each mean that a diagnosis of ventricular tachycardia is likely
Examination
Evidence of AV dissociation, as shown by cannon waves in the jugular venous pulse
ECG features
QRS width >140 ms
Evidence of AV dissociation: independent P waves marching through the ventricular rhythm
Evidence of fusion or capture beats
QRS concordance in leads V1 to V6 (complexes all positive or all negative in polarity)
Axis shift of more than 40 degrees from sinus rhythm frontal axis
Other features
No termination or slowing of tachycardia with adenosine (other than right ventricular outflow tract ventricular tachycardia)
ECG diagnosis of ventricular tachycardia
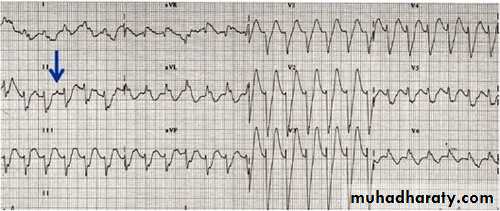
Features that are diagnostic of ventricular tachycardia include AV dissociation with independent P wave activity, as shown in the ECG in figure 9.
Figure 9: ECG showing ventricular tachycardia with AV dissociation and independent P wave activity, as shown by the blue arrow
The following types of beats are also diagnostic of ventricular tachycardia:
Capture beats - intermittent narrow complex beats conducted from the atria to the ventricles via the AV nodeFusion beats - QRS complexes composed of both normally conducted beats and the abnormal complexes of ventricular tachycardia. Fusion beats have morphology features of both normal complexes and ventricular tachycardia complexes.
If there remains any doubt about the diagnosis, it is safest to assume the rhythm is ventricular tachycardia until proved otherwise. Haemodynamic stability does not exclude ventricular tachycardia.
Types of ventricular tachycardia
Outflow tract ventricular tachycardiaThis is the most common idiopathic form of ventricular tachycardia, occurring predominantly in structurally normal hearts.
Of all cases, 90% arise from the right ventricular outflow tract and result in a left bundle branch block and inferior axis morphology,
Outflow tract ventricular tachycardia tends to be related to exertion and is unique in that it may respond to adenosine and the Valsalva manoeuvre. It may be haemodynamically well tolerated and less likely to cause sudden cardiac death than other ventricular arrhythmias. You should aim to suppress right ventricular outflow tract tachycardia with the use of beta blockers and verapamil.
Flecainide is an alternative medication, although catheter ablation of the abnormal outflow tract focus is also popular.
Arrhythmogenic right ventricular cardiomyopathy, a disease characterised by replacement of myocardial tissue by fat and fibrous tissue, can cause an outflow tract ventricular tachycardia, which may result in sudden cardiac death. In this case a cardiologist might suggest that an implantable cardiac defibrillator is required.
Idiopathic left ventricular tachycardia
This ventricular tachycardia originates from the left bundle branches, most commonly the posterior fascicle. It is characterised by:
A relatively narrow morphology of 100 to 140 milliseconds
Right bundle branch morphology
A left superior axis in 90% of cases (a right axis in 10%)
Possible sensitivity to verapamil or beta blockers.
Bundle branch re-entry tachycardia
This ventricular tachycardia arises from the distal conduction system. It typically has left bundle branch block morphology with a left axis deviation. Patients will also tend to have an ECG with a left bundle branch block pattern whilst in sinus rhythm. They will often need treating with ablation of the right bundle branch with subsequent pacing.Pharmacological management of ventricular tachycardia
Ventricular tachycardia may lead to cardiac arrest. You must give immediate external direct current cardioversion to sinus rhythm if the patient is unstable and has any of the following symptoms:• Reduced consciousness
• A systolic blood pressure that has fallen to less than 90 mm Hg
• Chest pain
• Signs of heart failure.
If the patient is stable, you may try pharmacological cardioversion:
Intravenous amiodarone is the first choice of drug
Intravenous lignocaine is an alternative to amiodarone, although there are no randomised controlled studies to support its efficacy.
In patients with torsades de pointes, correction of serum potassium levels and infusion of intravenous magnesium is mandatory.
Temporary pacing might be indicated in those patients whose arrhythmia is triggered by bradycardia. Beta blockers may then maintain sinus rhythm and prevent further episodes of polymorphic ventricular tachycardia.
It is important to avoid the use of verapamil in patients with ventricular tachycardia as they will become profoundly hypotensive and may suffer a cardiac arrest.
Implantable cardiac defibrillators, overdrive pacing, and ablation therapy
The prognosis for patients with recurrent ventricular tachycardia is improved if they are treated with an implantable cardioverter defibrillator. This is implanted in the same way as a permanent pacemaker. It continuously monitors the cardiac rhythm and can deliver an appropriate electric shock when ventricular tachycardia or ventricular fibrillation develops.In those patients who have had a previous cardiac arrest, an implantable cardioverter defibrillator reduces mortality by up to 50%. UK national guidelines from the National Institute for Health and Clinical Excellence (NICE) about treatment with an implantable cardioverter defibrillator are summarised in table 4.
Table 4: Indications for an implantable cardioverter defibrillator (excludes non-ischaemic dilated cardiomyopathy)
Secondary prevention
that is, for patients who present with one of the following conditions and no treatable cause:• A previous cardiac arrest due to either (VT) or (VF)
• Spontaneous sustained VT causing syncope or significant haemodynamic compromise
• Sustained VT without syncope or cardiac arrest, with an LVEF of less than 35% (no worse than class III of the NYHA
Primary prevention
for patients with a history of previous myocardial infarction for more than four weeks and:
Either
• Left ventricular dysfunction, with an LVEF of less than 35% (no worse than class III NYHA), and
• Non-sustained VT on Holter (24 hour ECG) monitoring, and
• Inducible VT on electrophysiological (EP) testing
• Left ventricular dysfunction, with an LVEF of less than 30% (no worse than class III NYHAand
• A QRS duration of equal to or more than 120 ms.
Alternatively, in patients with a familial cardiac condition that carries a high risk of sudden death, including the long QT syndrome, HOCM ,Brugada syndrome, or arrhythmogenic right ventricular dysplasia (ARVD), or in those who have undergone surgical repair of congenital heart disease.
In patients who are acutely unwell, you may try overdrive or antitachycardia pacing when pharmacological or electrical cardioversion treatment fails
Ablation therapy (radiofrequency or cryothermy to the myocardium to eliminate re-entrant arrhythmia circuits) for ventricular tachycardia is suitable in less than 20% of stable cases.
When ventricular tachycardia is related to scarring, it is associated with multiple possible re-entrant circuits, making ablation difficult. Electrophysiological studies are of limited value in patients with non-sustained ventricular tachycardia, polymorphic ventricular tachycardia, or primary ventricular fibrillation.
Antidromic AVRT
In this type of AVRT the ventricles are activated directly by an accessory pathway, and the atria are activated retrogradely over the AV node. During tachycardia, the ECG demonstrates maximal pre-excitation, with wide QRS complexes shown as an exaggerated delta wave and a broad complex tachyarrhythmiaThe management is similar to orthodromic AVRT, and you may be able to use adenosine to terminate the arrhythmia. In patients with atrial fibrillation and Wolff-Parkinson-White syndrome, rapid ventricular conduction across the accessory pathway from the atrium to the ventricle may result in ventricular fibrillation.
Atrial tachycardia conducted via an accessory pathway
A regular atrial tachycardia that is conducted to the ventricles via an accessory pathway may cause a broad complex tachycardia. Adenosine will not terminate this arrhythmia, which does not use the AV node in its circuit. Treatment is the same as for atrial tachycardias.Aberrantly conducted broad tachyarrhythmias
Patients with an aberrantly conducted broad tachyarrhythmia may have previous ECGs in sinus rhythm showing a QRS pattern similar to that seen during tachycardia. Alternatively, they may have a functional bundle branch block that is rate related, and so is present only during tachycardia. A useful way of differentiating these arrhythmias from ventricular tachycardia is with the use of intravenous adenosine. These arrhythmias can be irregular, as in the case of an aberrantly conducted atrial fibrillationIt can be difficult to distinguish ventricular tachycardia from other causes of a broad complex tachycardia, and electrophysiological testing may be required in order to make a definitive diagnosis. Table 3 lists features that make ventricular tachycardia likely.
Types of ventricular tachycardia
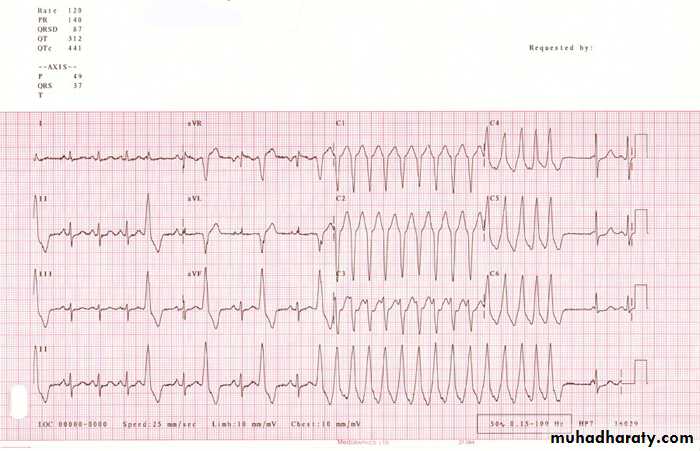
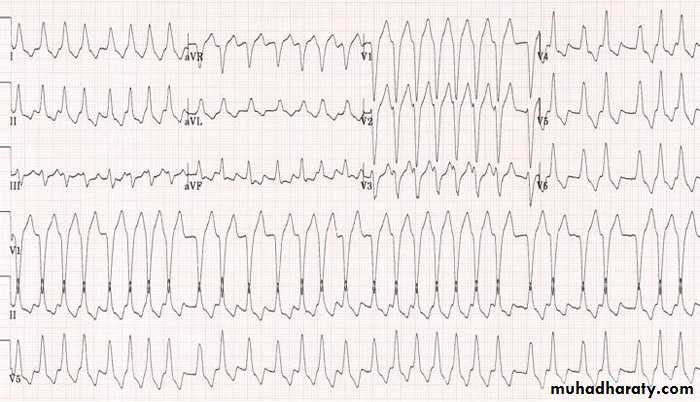
Outflow tract ventricular tachycardiaThis is the most common idiopathic form of ventricular tachycardia, occurring predominantly in structurally normal hearts. Of all cases, 90% arise from the right ventricular outflow tract and result in a left bundle branch block and inferior axis morphology, as shown in the ECG in figure 10.
Figure 10: ECG showing right ventricular outflow tract ventricular tachycardia
Figure 11: ECG of idiopathic left ventricular tachycardia
In patients who are acutely unwell, you may try overdrive or antitachycardia pacing when pharmacological or electrical cardioversion treatment fails
Ablation therapy (radiofrequency or cryothermy to the myocardium to eliminate re-entrant arrhythmia circuits) for ventricular tachycardia is suitable in less than 20% of stable cases.
When ventricular tachycardia is related to scarring, it is associated with multiple possible re-entrant circuits, making ablation difficult. Electrophysiological studies are of limited value in patients with non-sustained ventricular tachycardia, polymorphic ventricular tachycardia, or primary ventricular fibrillation.
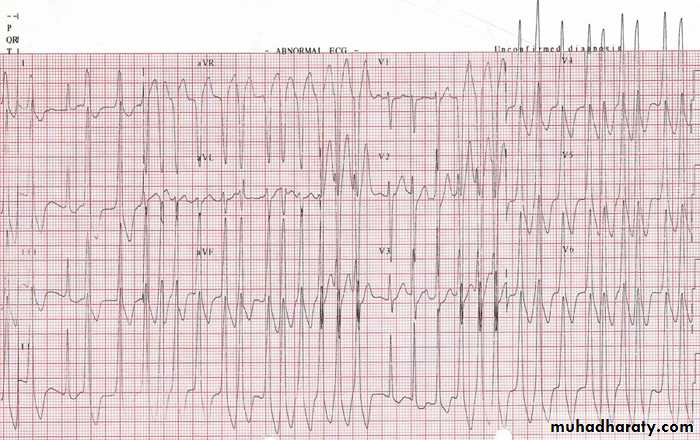
Antidromic AVRT
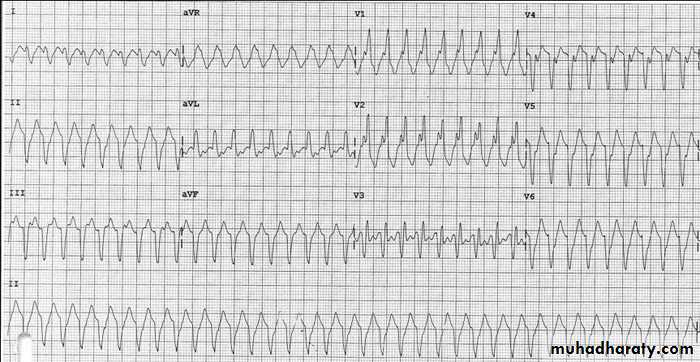
In this type of AVRT the ventricles are activated directly by an accessory pathway, and the atria are activated retrogradely over the AV node. During tachycardia, the ECG demonstrates maximal pre-excitation, with wide QRS complexes shown as an exaggerated delta wave and a broad complex tachyarrhythmia, as in the ECG in figure 12.Figure 12: ECG showing a broad complex tachyarrhythmia in antidromic AVRT
The management is similar to orthodromic AVRT, and you may be able to use adenosine to terminate the arrhythmia. In patients with atrial fibrillation and Wolff-Parkinson-White syndrome, rapid ventricular conduction across the accessory pathway from the atrium to the ventricle may result in ventricular fibrillationFigure 13: ECG showing irregular arrhythmia due to an aberrantly conducted atrial fibrillation
Irregular broad QRS tachyarrhythmia
Some ventricular tachycardias may be irregular. The most likely cause of this type of tachyarrhythmia is atrial fibrillation with conduction to the ventricles via an accessory pathway, a condition known as pre-excited atrial fibrillation. Atrial fibrillation conducted with left bundle branch block or right bundle branch block aberration may also be broad and irregular.Pre-excited atrial fibrillation
Rapid conduction of atrial fibrillation to the ventricles may be fatal if ventricular fibrillation occurs. The ECG in figure 14 shows a chaotic broad complex tachycardia with an irregular ventricular rate which may exceed 200 beats/min.Figure 14: ECG showing pre-excited atrial fibrillation
If a patient with irregular broad QRS tachyarrhythmia is haemodynamically stable, and the minimum RR interval is greater than 250 ms, then you should consider treating them with intravenous flecainide, procainamide, propafenone, sotalol, or amiodarone.Flecainide is especially important as it may terminate the atrial fibrillation and slow conduction in the accessory pathway.
If the patient is haemodynamically unstable, immediate cardioversion is indicated. Treatment of this tachycardia with drugs which block the AV node - such as beta blockers, calcium channel blockers, and digoxin - must be avoided due to the risk of accelerating the ventricular rate.
If conduction to the ventricles via the AV node is inhibited, there may be increased ventricular activation via the accessory pathway, resulting in a rapid heart rate.
Once sinus rhythm has been restored, you should make an urgent referral to a cardiac electrophysiologist for consideration of curative percutanous ablation of the pathway.
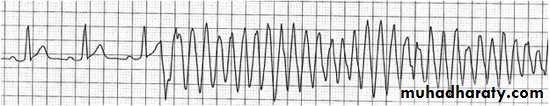
Polymorphic ventricular tachycardia
The ECG in a patient with polymorphic ventricular tachycardia typically shows a broad complex irregular tachycardia, where QRS complexes differ in morphology from their neighbouring complexes. The arrhythmia, resulting from triggered activity, is also known as torsades de pointes and is shown in the rhythm strip in figure 15.Figure 15: Rhythm strip showing
torsades de pointes
Polymorphic ventricular tachycardia can occur with a normal QT interval in:
Ischaemia.Arrhythmogenic right ventricular dysplasia
Rare familial cases of the genetic condition catecholaminergic polymorphic ventricular tachycardia
Polymorphic ventricular tachycardia is also associated with prolongation of the QT interval. Some cases are congenital, whereas others are due to drugs and electrolyte imbalances.
Sustained polymorphic ventricular tachycardia is, in almost all cases, an inherently unstable rhythm with haemodynamic compromise and the risk of degeneration to ventricular fibrillation.
The treatment of polymorphic ventricular tachycardia should involve the following measures:
Electrical cardioversion is first line treatment
Correction of the serum electrolytes, particularly potassium and magnesium
Performing temporary pacing to prevent further episodes of ventricular tachycardia
Most authorities recommend the use of beta blockers for polymorphic ventricular tachycardia with a normal QT interval, especially in ischaemia
Adenosine may be useful in differentiating ventricular tachycardia from supraventricular tachycardia if the patient is haemodynamically stable.
A response to oral amiodarone therapy may not be seen until three weeks after starting the drug.
Verapamil should be avoided if ventricular tachycardia is a possibility because it may cause profound hypotension. It should also be avoided in the treatment of supraventricular tachycardia in the setting of hypotension.
Beta blockers may improve this patient’s prognosis and suppress ventricular arrhythmias, as well as reduce the risk of subsequent myocardial infarction, but trials have shown beta blocker therapy to be inferior to treatment with an ICD. Treatment with an ICD is superior to antiarrhythmic therapy for improvement of the long term prognosis of patients with ventricular arrhythmias.