The ECG in patients with chest pain: diagnostic picture tests
د. حسين محمد جمعهاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
Percutaneous coronary intervention is the most effective single treatment for acute myocardial infarction complicated with cardiogenic shock
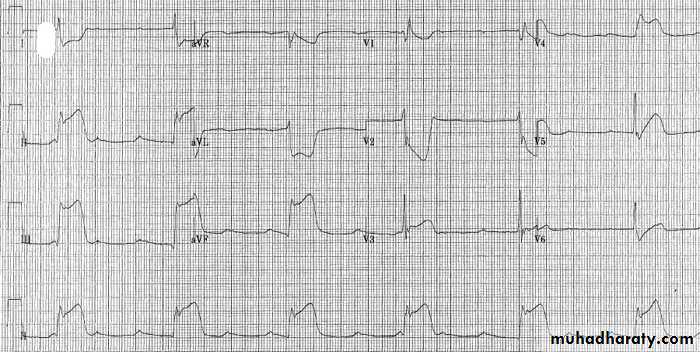
This ECG shows prominent ST elevation in the inferior leads (II, III, aVF). There is also marked ST depression in the lateral leads (I, aVL). Posterior extension is likely with the reciprocal ST depression in leads V1 and V2. Also complete heart block - a common finding in inferior myocardial infarction (it may also occur in large anterior myocardial infarctions).
Supraventricular tachycardia with aberrance will typically conform to a right or left bundle branch block appearance.
Ventricular tachycardia
Regular broad complex tachycardia may show evidence of dissociated p waves, capture or fusion beats, or concordance (similar axis throughout the chest leads).
Torsades de pointes is a rare form of polymorphic ventricular tachycardia with a changing axis.
Sedation and synchronised DC 200 J shock is the first line treatment of Ventricular tachycardia in grave haemodynamic state .
Urgent assistance from an anaesthetist may be required, although the procedure can also be performed using sedation, for example with intravenous midazolam. Subsequent management should determine the underlying cause - this is commonly due to ischaemia or infarction, but may also be due to electrolyte disturbance or drug toxicity, starting with a further 12-lead ECG.
ECG changes of hyperventilation are not uncommon, including tachycardia, prolonged QT interval, ST depression or elevation, or T-wave inversion.
Pulmonary embolism may cause a range of ECG abnormalities (or be associated with a normal ECG). Most commonly, sinus tachycardia is seen, but other ECG findings may include atrial fibrillation or flutter and supraventricular tachycardias. Right heart strain may be evident as right bundle branch block or, uncommonly, with an acute right heart strain pattern (the SI QIII TIII pattern). Pulmonary embolism is suggested by the finding of
hypoxia with clear lung fields, tachycardia, Cardiac troponin rises are not uncommon
Boerhaave syndrome (oesophageal rupture) classically presents with vomiting, sudden onset lower thoracic pain, and subcutaneous emphysema and will not resolve without major intervention, usually surgical. Hypotension is usual.
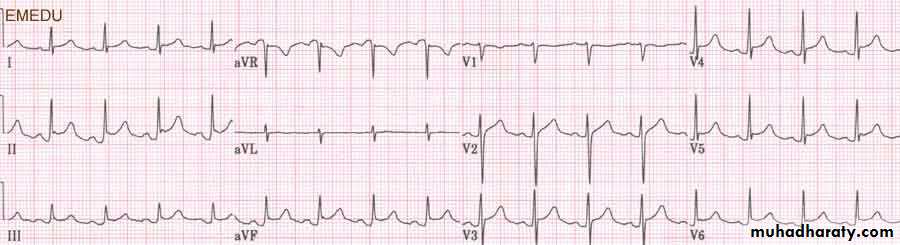
Acute pericarditis causes ST elevation - which is often described as saddle shaped or concave up - that is often widespread. This will not correspond to a particular coronary artery distribution. Such ST changes are seen in this ECG in almost all the leads. A pathognomonic finding of acute pericarditis is PR segment depression,6 as seen in leads II, III, and aVF above. This is not found in most patients however. Pericardial pain is typically pleuritic in nature, worse on lying flat, and relieved by sitting forward. An abnormal cardiac troponin has been reported in up to 50% of patients with idiopathic pericarditis.7 A rub may be heard, although this is often a transient finding and its absence in no way rules out the diagnosis.
In the absence of adverse prognostic indicators (cardiac tamponade, temperature >38°C, immunosuppression, trauma, oral anticoagulation, or myopericarditis), such as in this woman, outpatient management is safe. Non-steroidal medication is the main therapy, although colchicine can be helpful if episodes are prolonged (for more than two weeks). In most idiopathic or viral episodes, the disease is self limiting. A raised troponin per se does not carry an adverse prognosis.
What would be the appropriate treatment for pericarditis
If bacterial infection (is usually secondary to haematogenous spread, for example from pneumonia)is suggested in the clinical history, cultures should be taken, including of any pericardial fluid, to guide antibiotic therapy. Low molecular weight heparin and intravenous opiate analgesia would not be appropriate treatment for pericarditis unless it was clearly related to a recent myocardial infarction. Anticoagulation in the context of pericarditis increases the risk of haemorrhage into the pericardial space, which may precipitate tamponade.