TREATING PATIENTS WITHVENTRICULAR ECTOPIC BEATS
Heart 2006د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
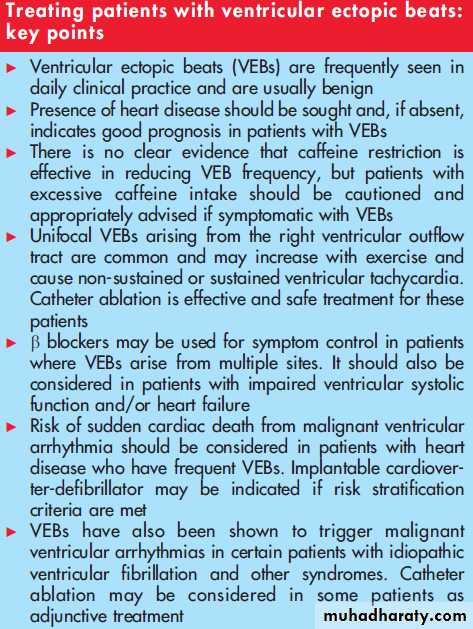
Ventricular ectopic beats (VEBs) are commonly seen in daily clinical practice. They are largely asymptomatic but can cause upsetting symptoms in some patients. In normal hearts, their occurrence is usually associated with no clinical significance. However, there are occasions where the presence of VEBs signifies a susceptibility towards more sinister arrhythmias, especially when heart disease is present.
VEBs have been described in 1% of clinically normal people as detected by standard ECG and
40–75% of apparently healthy persons as detected by 24–48 hour ambulatory (Holter) ECGrecording. Early studies had been criticised as the presence of heart disease was not investigated
with stress testing, echocardiography or invasive tests.
The study by Kostis et al3 in 1981 in subjects free of recognisable heart disease, verified by the above list of investigations including right- and left-heart catheterisation and coronary arteriography, showed that 39 out of 101
subjects had at least one VEB over a 24 hour period and four subjects had . 100/24 hours, with five having . 5 VEBs in any given hour and four having multiform VEBs.
Even frequent (60/h or 1/min) and complex VEBs occur in apparently healthy subjects, with an estimated prevalence of 1–4% of the general population.
These latter phenomena are often seen in patients with heart disease and are widely accepted as markers of increased risk of malignant arrhythmias and death.
However, the study by Kennedy in 1985 suggested that in the absence of structural heart disease,
even frequent and complex VEBs are associated with a benign prognosis.4 Later, the study on a
cohort of the Multiple Risk Factor Intervention Trial (MRFIT),5 reported that the presence of VEB
identified on a rest two-minute ECG rhythm strip was associated with a high risk for sudden death in apparently healthy subjects over a 7.5 year follow-up.
Furthermore, results of the Cardiac Arrhythmia Suppression Trial (CAST) published in 1989 questioned the causal importance of VEBs in increasing risk and revolutionised the thinking behind the necessity to suppress VEBs.
CAST was a randomised, placebo-controlled study which tested the hypothesis that suppression of asymptomatic or minimally symptomatic VEBs after myocardial infarction would reduce arrhythmic death.
Although the class Ic drugs,encainide and flecainide, were effective in suppressing VEBs,
arrhythmic death was more common in those treated with the drugs (4.5%) than placebo with a relative risk of 3.6. This study further highlights the proarrhythmic effect of these drugs in patients with heart disease and disputes the notion of using drugs simply for the sake of suppressing VEBs.It has been shown in early clinical studies that VEBs occur frequently in patients with hypertension. In the MRFIT population cohort of over 10 000 men aged 35–57 years, the level of systolic blood pressure was linked with the prevalence of VEBs. More recent data in the Atherosclerosis Risk in Communities (ARIC) study of more than 15 000 African American and white men and women extended these findings to show that frequent or complex VEBs are also associated with hypertension.
HYPERTENSION
CAFFEINE AND VENTRICULAR ECTOPICS
Caffeine is a central stimulant which can increase sympathetic activity. It is not illogical to assume that caffeine usage can increase the frequency of ventricular ectopics, especially if they may be fuelled by sympathetic activity. Clinical impression and anecdotes often associate arrhythmias with consumption of caffeine, alcohol and tobacco, and caution against these ‘‘pleasures’’ has been widely practised inmanaging patients with palpitation despite the relative lack of direct evidence.
Dobmeyer and colleagues performed
electrophysiologic study in the presence of caffeine in seven normal volunteers and 12 heart disease patients. Caffeine did not affect cardiac conduction but did alter some of the electrophysiologic measurements with the conclusion that it might aggravate an existing predilection to arrhythmia.
Many subsequent negative studies supported the notion that moderate ingestion of coffee does not increase the frequency or severity of cardiac arrhythmias.
Remarkably, one study by Graboys et al examined the effects of caffeine in 50 patients with known recurrent ventricular tachycardia, ventricular fibrillation and symptomatic non-sustained VT in whom no changes were seen with a modest dose of 200 mg of caffeine.
On the other hand, caffeine restriction does not appear to have any significant effect on VEB frequency. DeBacker et al failed to demonstrate the efficacy of a ‘‘hygienic’’ intervention programme involving normal men with frequent VEBs.
Total abstinence from caffeine and smoking, reduction of alcohol intake along with exercise conditioning did not alter the occurrence or frequency of VEBs.
VENTRICULAR ECTOPIC BEATS AND EXERCISE
Exercise testing is an established procedure widely used to diagnose myocardial ischaemia and to risk stratify patients with known coronary disease. It has also been used to evaluate ventricular arrhythmias as early as 1927. The conventional impression is that VEBs that are not provoked by exercise or reduce in activity during exercise can be regarded as ‘‘benign’’ and not of clinical significance.However, this notion has not been subjected to detailed scientific examination. What has been tested is the prognostic significance of VEBs induced either during or even after exercise.
The study by Jouven et al15 in 2000 was the first comprehensive study to demonstrate an association between the occurrence of frequent VEB during exercise and a long-term increase in
cardiovascular death. A total of 6101 asymptomatic French men free of clinically detectable cardiovascular disease were exercised and persons with frequent VEBs, defined as having. 10% of all ventricular depolarisations in any 30 s recordings
during exercise, were found to have an increase in
cardiovascular deaths by a factor of 2.67 after 23 years of follow up.
It is interesting to note that 4.4% of all subjects
had an ischaemic response to exercise and only 3% of these had frequent VEBs. Among subjects with frequent VEBs during exercise (2.3% of all subjects), only 5.8% had an exercise test positive for ischaemia. Multivariate analysis also demonstrated that the ischaemic response to exercise and occurrence of frequent VEBs were independently associatedwith cardiovascular deaths.
A recently published study in 2885 subjects who are offspring of the original Framingham study participants also presented similar findings.
Participants with VEBs at rest and chronic obstructive lung disease, in addition to other pre-existing cardiac conditions and usage of cardiac glycosides or b blocking agents, were excluded from the study, which may explain the low (0.1%) incidence of exercise-induced VEBs that exceeded 10% of all
ventricular depolarisations.
Hence, VEBs were defined as frequent when they exceeded the median of 1 VEB per4.5 minutes of exercise (0.22 VEBs/min). Although it was
concluded that exercise-induced VEBs were not associated with hard coronary heart disease events, both infrequent and frequent VEBs on exercise were associated with an increase
in all-cause mortality over 15 years of follow-up.
The study by Frolkis et al17 focused on the recovery period of the exercise test and showed that frequent VEBs after exercise were a better predictor of increased risk of death than VEBs occurring only during exercise. Frequent VEBs were defined by
• > 7 VEBs per minute,
• ventricular bigeminy or
• trigeminy,
• ventricular couplets or triplets,
• torsade de pointes, ventricular tachycardia,
• flutter or fibrillation.
RIGHT VENTRICULAR OUTFLOW TRACT TACHYCARDIA AND VENTRICULAR ECTOPIC BEATS (RVOT)
It belongs to the group of ‘‘idiopathic’’ ventriculartachycardias (VTs) or ‘‘normal heart’’ VTs—in the
absence of overt structural heart disease—which arises from the RVOT. It is a common condition, with symptom onset between the second and fourth decade, being more common in women, and represents up to 10% of all VTs evaluated at
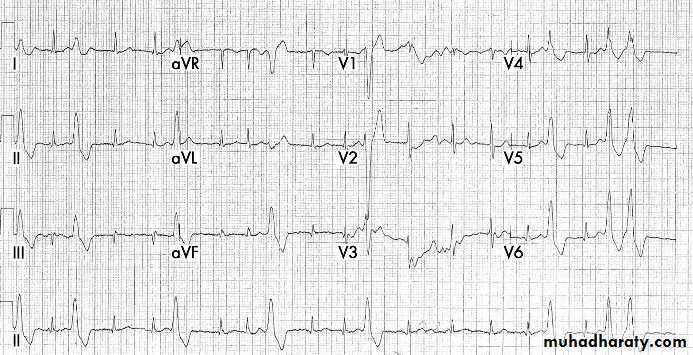
specialised arrhythmia services. VEBs originating from the RVOT have a distinctive ECG appearance with QRS complexes assuming a left bundle branch block, inferior axis morphology .
The arrhythmia mechanism is believed to be caused by cyclic AMP (adenosine monophosphate) mediated triggered activity. Exercise and emotional
stress can increase the frequency of the VEBs or even induce non-sustained or sustained VT .Many reports have suggested that long-term prognosis in patients with truly idiopathic RVOT-VT is excellent despite frequent episodes of VT, and sudden death is rare in patients with good biventricular function.
Indeed, right ventricular ectopics are more common than left ventricular ectopics in previous reports in patients with normal hearts and it is likely that amajority of these right-sided VEBs were from the RVOT.
Arrhythmogenic right ventricular dysplasia (ARVD) is a form of right ventricular cardiomyopathy where progressive,patchy fibrofatty infiltration of the right ventricle and subsequent ventricular dilatation provides an ideal arrhythmogenic substrate. VT occurring in ARVD may mimic that of idiopathic RVOT tachycardia but prognosis is much less favourable.
It is important to distinguish between the two as
RVOT tachycardia is now treated with curative catheter ablation, whereas VTs in ARVD are best managed with the implantable cardioverter-defibrillator (ICD) as long-term results with catheter ablation are disappointing.‘‘MALIGNANT’’ VENTRICULAR ECTOPIC BEATS
The ability of frequent VEBs originating from a focal source in triggering idiopathic ventricular fibrillation (VF) in seemingly normal hearts was first reported by Haissaguerre et al. The VEBs were mappedto sites at the RVOT and also along the distal Purkinje system in both left and right ventricles. Catheter ablation was shown to be effective in acutely eliminating VEBs and reducing the incidence of further VF recurrence.
Similar triggers have been shown in selected patients with long QT and Brugada syndromes with report of successful elimination of VEBs with catheter ablation. Further studies in large numbers of patients with longer follow up are required to assess the full
prognostic benefit of this approach.
Catecholaminergic polymorphic ventricular tachycardia is arare condition whereby mutations in the cardiac ryanodine receptor and calsequestrin, which are key calcium handling proteins in the cardiac ventricular myocyte, cause malignant ventricular arrhythmias induced by catecholamines.
Progressive VEBs are induced with exercise or stress which can cause syncope or sudden death with polymorphic VT or VF. Treatment is usually with b blockers and ICD implantation.
APPROACH TO TREATING PATIENTS WITH
VENTRICULAR ECTOPICS
Patients with VEBs often describe ‘‘missing a beat’’ or‘‘feeling the heart has stopped’’, being aware of the compensatory pause following VEBs, as well as ‘‘extra beats’’or ‘‘thumps’’. The frequency and severity of these symptoms should be assessed. The presence, duration and frequency of any fast palpitation should be noted and any association with pre-syncope or syncope recorded. Patients should be asked about any triggering factors, especially exercise.
The presence of ischaemic or structural heart disease should be considered, taking clues from past medical history and other cardiac symptoms, especially those suggesting the presence of heart failure. Caffeine, alcohol, and drug intake should be noted as
well as smoking habits. Family history may be relevant
especially if there has been sudden death or other clues
towards a genetic syndrome or cardiomyopathy. Clinical
examination should be aimed at identifying any structural heart disease and/or heart failure.
In the absence of heart disease or significant risk factors, patients with symptoms of VEBs that are self-limiting or respond to lifestyle modifications may simply be reassured while patients with ongoing or worsening symptoms should undergo further investigations. These include a resting 12-lead ECG, echocardiography, ambulatory Holter recording and exercise tolerance test (ETT).
Echocardiography is important as both ventricular function and the presence or absence of structural heart disease are important considerations
in assessing the need for further intervention and
treatment. The morphology of VEBs should be assessed in all the available rhythm recordings including 12-lead ECG, Holter recording and ECG during ETT. It should be determined if the VEBs are coming from a single focus (unifocal) or from many sites (multifocal).
Repetitive unifocal activity, especially associated with exercise, is suggestive of triggered activity primed by catecholamines, and the presence of monomorphic VT, whether nonsustained (<30 s) or sustained (>30 s), should be sought.
VEBs which reduce in frequency on exercise are generally regarded as ‘‘benign’’ while multifocal VEBs provoked on ETT may signify an underlying risk of cardiac disease even in the absence of conventional ischaemic changes .
Treatment for patients with VEBs
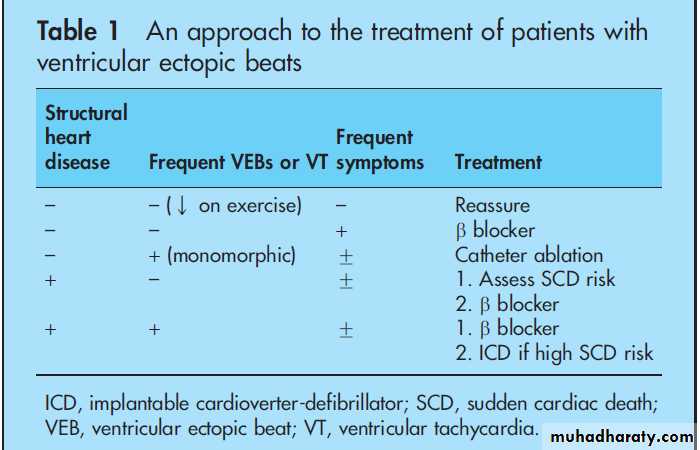
In considering the need for further intervention and planning treatment for patients with VEBs, it is important to consider:• whether there is underlying heart disease;
• The frequency of the VEBs and if VT has been documented; and
(3) the frequency and severity of symptoms.
In the absence of heart disease and if VEBs are infrequent or reduce in frequency on ETT, with no documented VT, patients should be reassured and no specific treatment is required—especially if they are relatively asymptomatic. The same patients with significant symptoms should have their blood pressure checked and investigated and treated if high.
Patients with high caffeine intake should be advised to try decaffeinated drinks and/or reduce caffeine consumption to assess the impact on symptoms.
If these measures fail b blockers may be considered, but a balance should be struck between the level of symptoms and the possibility of side effects, given that VEBs in the absence of heart disease carry
a good prognosis.
There is no evidence to support the use of other antiarrhythmic agents simply for the sake of suppressing VEBs, especially considering their proarrhythmic (for example, flecainide) and other side effects (for example, amiodarone).
In patients with normal hearts where there are frequent
unifocal VEBs, especially if salvos or VT are induced onexercise, catheter ablation should be considered. Results are favourable especially if the VEBs arise from the RVOT.
Similar focal VEBs may also originate from other parts of the right ventricle and also the left ventricular outflow tract and sinuses of Valsalva which are also amenable to catheter ablation.