د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Unstable angina and non-ST segment elevation myocardial infarction (NSTEMI) - in association with NICE
Learning bite
As soon as the diagnosis of unstable angina or NSTEMI is made, and aspirin and antithrombin therapy have been offered, formally assess individual risk of future adverse cardiovascular events using an established risk scoring system that predicts six month mortality (for example, Global Registry of Acute Cardiac Events (GRACE)).Include in the formal risk assessment:
A full clinical history (including age, previous myocardial infarction (MI), and previous percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG))A physical examination (including measurement of blood pressure and heart rate)
Resting 12-lead electrocardiography (ECG) (looking particularly for dynamic or unstable patterns that indicate myocardial ischaemia)
Blood tests (such as troponin I or T, creatinine, glucose, and haemoglobin).
Predicted six month mortality
Risk of future adverse cardiovascular events
1.5% or below
Lowest
>1.5 to 3.0%
Low
>3.0 to 6.0%
Intermediate
>6.0 to 9.0%
High
over 9.0%
Highest
• Record the results of the risk assessment in the patient's care record.
• Use risk assessment to guide clinical management, and balance the benefit of a treatment against any risk of related adverse events in the light of this assessment.
• Use predicted six month mortality to categorise the risk of future adverse cardiovascular events as follows:
The NICE Guideline Development Group selected six month mortality as the outcome measure for risk stratification because:
Mortality is a hard endpoint, which is available for most clinical trials
Mortality cannot be misinterpreted (as can an endpoint such as myocardial infarction, the definition of which has evolved over time, and varies between trials).
A six month time frame captured the majority of clinical events that occur after presentation with unstable angina or NSTEMI, and which may be influenced by an in hospital intervention (pharmacological or interventional). Shorter follow up intervals may miss events related to the index acute coronary syndrome event, and longer follow up may become increasingly influenced by other factors such as the effects of post-discharge secondary prevention interventions. Moreover, trials often do not report findings beyond the six month follow up period.
As soon as the risk of adverse cardiovascular events has been assessed, offer a loading dose of 300 mg clopidogrel in addition to aspirin to patients with a predicted six month mortality of more than 1.5% and no contraindications (for example, an excessive bleeding risk). You should also offer a 300 mg loading dose of clopidogrel to all patients with no contraindications who may undergo percutaneous coronary intervention (PCI) within 24 hours of admission to hospital. For patients with aspirin hypersensitivity, clopidogrel monotherapy (300 mg loading dose then 75 mg daily) should be considered .
Current NICE guidance for drug eluting stents does not recommend any specific duration of clopidogrel therapy in addition to aspirin. However, NICE refers to the recommendations from the American College of Cardiologists/American Heart Association PCI guidelines and the British Cardiovascular Intervention Society advising a duration of at least 12 months, after which time continuation of clopidogrel should be reviewed taking into account the risk of further ischaemic events (particularly the risk of subsequent stent thrombosis) and potential bleeding complications on an individual patient basis.
A 2010 interim analysis of data from two studies (Park S-J, et al. Duration of dual antiplatelet therapy after implantation of drug-eluting stents. N Engl J Med 2010. Published online 15 March (doi: 10.1056/NEJMoa1001266) suggests no benefit for continuing to use clopidogrel in addition to aspirin for more than 12 months after implantation of drug eluting stents. However, because of limitations, further studies are required to confirm or refute these findings. The findings of this analysis are insufficient to recommend a change in practice.
• Learning bite
• Consider discontinuing clopidogrel treatment five days before CABG in patients who have a low risk of adverse cardiovascular events. For patients at intermediate or higher risk of adverse cardiovascular events, discuss the continuation of clopidogrel before CABG with the cardiac surgeon and base the decision on the balance of ischaemic and bleeding risk.A 47 year old woman presents with a non-ST elevation myocardial infarction. You assess her to have a low bleeding risk and provide a 300 mg aspirin loading dose and prescribe a continuing 75 mg dose for life. She is listed for angiography in 72 hours and her renal function is normal. What should you prescribe next?
Low molecular weight heparins (including enoxaparin) are not recommended in the NICE guideline.
Unfractionated heparin is recommended for patients undergoing angiography within 24 hours, or those with significant renal impairment.
Offer fondaparinux to patients who do not have a high bleeding risk, unless coronary angiography is planned within 24 hours of admission. Based on the OASIS-5 trial, the NICE guideline advocates fondaparinux as the routine antithrombin.
A 64 year old woman has had a non-ST elevation myocardial infarction. She receives antiplatelet therapy. You think that she is at intermediate or high risk (predicted six month mortality above 3.0%). She is scheduled to have angiography in the next 96 hours. She is not at risk of bleeding and is no longer in any pain. Which of the following treatments would you add?
Consider intravenous eptifibatide or tirofiban as part of the early management for patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%), and who are scheduled to undergo angiography within 96 hours of hospital admission. Consider abciximab, usually in the catheter laboratory, as an adjunct to PCI for patients at intermediate or higher risk of adverse cardiovascular events who are not already receiving a glycoprotein IIb/IIIa inhibitor. Balance the potential reduction in a patient's ischaemic risk with any increased risk of bleeding, when determining whether a GPI should be offered.
Learning bite
Carefully consider the choice and dose of antithrombin in patients who have a high risk of bleeding associated with any of the following:• Advancing age
• Known bleeding complications
• Renal impairment
• Low body weight.
Offer systemic unfractionated heparin (50-100 U/kg) in the cardiac catheter laboratory to patients receiving fondaparinux who are undergoing PCI.
As an alternative to the combination of a heparin plus a GPI, consider bivalirudin for patients who:
Are at intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%), and
Are not already receiving a GPI or fondaparinux, and Are scheduled to undergo angiography (with follow on PCI if indicated) within 24 hours of admission.
Clinical tip
All anticoagulants are necessarily associated with a risk of bleeding complications and weighing this risk against the potential benefits of such agents requires an understanding of the factors associated with bleeding risk, measures by which the magnitude of this risk can be estimated, and the potential for benefit from these agents in reducing the rate of ischaemic events. Close attention to appropriate dosing of these agents is particularly important.It is logical to assess LV function in all people with unstable angina and NSTEMI so that specific treatment for LV dysfunction can be offered to improve symptoms and outcome. Left ventricular function may improve after an acute ischaemic event with the resolution of myocardial stunning and the onset of healing. It may also deteriorate because of myocardial remodelling or progression of coronary disease. It may therefore also be important to monitor LV function during follow up, because of this potential for change with time.
Learning bite
To detect and quantify inducible ischaemia, consider ischaemia testing before discharge for patients whose condition has been managed conservatively and who have not had coronary angiography.If untreated, the prognosis of patients with non-ST elevation myocardial infarction is poor and mortality high, particularly in people who have had myocardial damage.
Key points
When advising patients about the choice of revascularisation strategy (PCI or CABG), take account of coronary angiographic findings, comorbidities, and the benefits and risks of each intervention. When the role of revascularisation or the revascularisation strategy is unclear, resolve this by discussion involving an interventional cardiologist, cardiac surgeon, and other healthcare professionals relevant to the needs of the patient. Discuss the choice of revascularisation strategy with the patient.To detect and quantify inducible ischaemia, consider ischaemia testing before discharge for patients whose condition has been managed conservatively and who have not had coronary angiography
Before discharge offer patients advice and information about:
Their diagnosis and arrangements for follow up
Cardiac rehabilitation
Management of cardiovascular risk factors and drug therapy for secondary prevention
Lifestyle changes
Clinical tips
NICE Technology Appraisal 182 states "Prasugrel in combination with aspirin is recommended as an option for preventing atherothrombotic events in people with acute coronary syndromes having percutaneous coronary intervention, only when:
• Immediate primary percutaneous coronary intervention for ST-segment-elevation myocardial infarction is necessary
• Stent thrombosis has occurred during clopidogrel treatment
• The patient has diabetes mellitus."
Prasugrel is currently a black triangle medicine. A black triangle is assigned to a product if the drug is an active substance which has been newly licensed for use in the UK. The black triangle symbol is not removed until the safety of the drug is well established. The MHRA wishes to receive all reports of suspected adverse reactions associated with black triangle products, in order to:
Confirm risk/benefit profiles established during the premarketing phase .
Increase our understanding of the safety profiles of new medicines.
Ensure that previously unrecognised side effects are identified as quickly as possible
Specific contraindications to prasugrel are:
Hypersensitivity to the active substance or to any of the excipients• Active pathological bleeding
• History of stroke or transient ischaemic attack (TIA)
• Severe hepatic impairment (Child-Pugh class C).
Full details of caution in use and side effects are included in the makers SPC available at http://www.medicines.org.uk/emc/
The common side effects of clopidrogel include bruising, haematoma (normally seen associated with a procedure, surgery, or trauma),
epistaxis,
gastrointestinal haemorrhage,
diarrhoea, abdominal pain, dyspepsia, bleeding at puncture site.
Safety in patients with acute coronary syndrome undergoing PCI was evaluated in one clopidogrel controlled study (TRITON) in which 6741 patients were treated with prasugrel (60 mg loading dose and 10 mg once daily maintenance dose) for a median of 14.5 months (5802 patients were treated for over six months, 4136 patients were treated for more than one year). The rate of study drug discontinuation due to adverse events was 7.2% for prasugrel and 6.3% for clopidogrel. Of these, bleeding was the most common adverse reaction for both drugs leading to study drug discontinuation (2.5% for prasugrel and 1.4% for clopidogrel).
Cardiac rehabilitation should be equally accessible and relevant to all patients after an MI.
Before discharge offer patients advice and information about:
Their diagnosis and arrangements for follow up
Cardiac rehabilitation
Management of cardiovascular risk factors and drug therapy for secondary prevention
Lifestyle changes.
All patients who smoke should be advised to quit and be offered support and advice, and referral to an intensive support service.
Although no evidence exists specifically for people with unstable angina, it is part of the same pathophysiological continuum as NSTEMI and so the recommendations would logically apply to both groups.
It is vital that information and education is delivered in an appropriate format to people prior to discharge from hospital given the importance of establishing people on appropriate medication, and the value of people understanding the indications and actions of these medications, and the underlying nature of their cardiac condition and any effect of comorbidity.
Rehabilitation, in its most general sense, actually starts from the moment of diagnosis because from this time onwards there is potential benefit to people from being well informed and psychologically supported, and therefore the distinction between in hospital and post-discharge intervention is somewhat arbitrary. The overriding consideration should be to ensure that the process is continuous and that responsibility for delivery of the components of rehabilitation (education, information, psychosocial support, structured exercise, etc) should be clearly attributed.
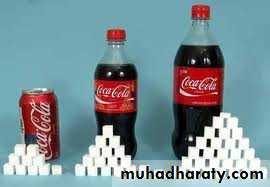
When the National Service Framework (NSF) for Coronary Heart Disease was published in 2000 it was estimated that in England 1.4 million people suffer from angina, 300 000 have heart attacks, and more than 110 000 die of heart disease every year. Much has improved since then; mortality from myocardial infarction and other cardiovascular causes has declined and inequalities between socioeconomic groups have decreased. However, the number of people admitted with non ST-segment elevation myocardial infarction has shown less of a decline and with worrying trends in the incidence of obesity and diabetes, and lifestyles that involve less exercise, the management of these conditions remains a high priority.
Over the last 10 years it has become clear that people with acute coronary syndromes of all sorts (STEMI and NSTEMI) have quite widely varying outcomes, and much work has gone into defining the clinical components which individually predict this poor outcome. Scoring systems have been established in an attempt to risk stratify patients and more recent trials of drugs and other interventions have analysed the effect of an intervention by patient risk group.
Broadly speaking, clinical trials have shown that, as risk increases, the potential for an intervention to give benefit also increases. However, the increasing number of drugs available that affect blood clotting (and thus reduce ischaemic events) also cause bleeding, which itself is an important determinant of poor outcome. This has left those managing patients with NSTEMI with a dilemma: should they offer a particular cocktail of drugs, each with individual evidence of benefit, to an individual patient, or will the amount of the cocktail's benefit be offset by associated complications?
This guideline formally addresses the risk stratification of patients, and the relevance of various clinical trials, to the risk profile of an unselected population with non-ST segment elevation ACS. In this way the guideline defines those who are likely to have a net benefit from an intervention and those where the benefit is either absent, uncertain, or not cost effective. The optimum outcome for those suffering with ACS depends on them receiving evidence based management throughout the duration of their clinical episode. Correct management of such patients is vital and can prevent much morbidity and mortality - in the short and long term.
One significant change is the use of fondaparinux as the routine antithrombin for patients with ACS.
An episode of unstable angina/NSTEMI starts with prompt and accurate diagnosis, and this is addressed as part of the NICE guidance on undifferentiated chest pain (see NICE Clinical Guideline: Chest pain of recent onset: assessment and diagnosis of recent onset chest pain/discomfort of suspected cardiac origin), which is the subject of a separate BMJ Learning module.
The episode continues with appropriate care in hospital, the subject of this guidance, but then continues after discharge from hospital with access to rehabilitation, lifestyle changes, secondary preventive medication, and maintenance of vascular checks in general practice.