د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
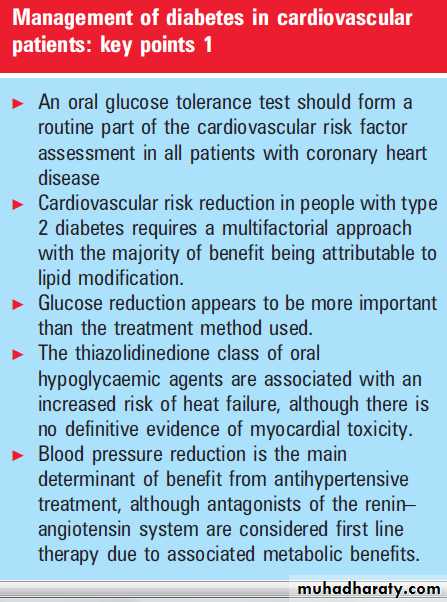
Management of diabetes incardiovascular patients
Heart 2008©BMJ Learning 2011
Type 2 diabetes mellitus (T2DM) is a common
disease affecting ,3–5% of people living in thewestern world. Cardiovascular disease (CVD)
((coronary heart disease (CHD), stroke and peripheral
vascular disease)) is the most important cause
of mortality and morbidity among patients with
T2DM. Compared with a non-diabetic individual,
a person with T2DM has a two- to fourfold
increased risk of dying from a myocardial infarction
(MI) or astroke and a 10- to 15-fold
increased risk of a lower extremity amputation.
More recently Tuomelhto’s
group similarly reported that in patients presenting
with acute stroke only ,20% had normal glucose
values.
Norhammar et al in 2002 reported that on the basis
of an oral glucose tolerance test, ,65% of patientsadmitted with acute MI but without known
history of diabetes had either frank diabetes or
impaired glucose tolerance, with glucose values
after day 4 post-event being highly predictive of
incident diabetes.
It may thus be considered that presentation
with an acute coronary event represents an
indication for formal diabetes screening with a 75 g
oral glucose tolerance test conducted at day 4 postevent.
Haffner et al first reported that middle aged
subjects with diabetes but without a history of MIhad the same risk for an ischaemic event over a
7 year observation period as a group of subjects
without diabetes but with a past history of MI.
In another study in patients hospitalised with a
confirmed MI, those with diabetes manifested a
higher mortality during a mean follow up of
3.7 years. The magnitude of the effect of diabetes
on mortality was similar to that produced by a
history of previous MI.
Although there is some debate around the issue of T2DM as a cardiovascular disease equivalent, it is clear that diabetes is a potent cardiovascular risk factor, and once CVD becomes manifest, patients with diabetes have a poorer prognosis than patients without diabetes. In the Valsartan in Acute Myocardial Infarction (VALIANT) trial involving 14 703 patients with acute MI, patients with either previously known diabetes or newly diagnosed diabetes had an increased risk of mortality compared to those without diabetes after 1 year.
The management of people with T2DM is thus
no longer glucocentric but focuses on multiple riskfactor intervention. In the landmark Steno-2 trial,
160 people with T2DM and microalbuminuria
were randomised to conventional treatment or
intensive treatment with lifestyle modification and
pharmacological interventions. Hyperglycaemia,
hypertension, dyslipidaemia, microalbuminuria
and prevention of CVD with aspirin were targeted in the intensive treatment arm.
Over the 7.8 years of follow-up, it was found that patients receiving intensive therapy had a significantly lower risk of CVD (hazard ratio (HR) 0.47, 95% confidence interval (CI) 0.24 to 0.73; p=0.008) compared to the conventionally treated group.
GLYCAEMIA AND PREVENTION OF
CARDIOVASCULAR EVENTSThe first reports on glucose as a risk factor for
cardiovascular complications were published in
1965 in the UK (the Bedford study) and the USA (the Tecumseh study). These cross-sectional analyses suggested that elevation of glucose was associated with CHD mortality. Numerous prospective studies have demonstrated a correlation between the risk for CVD and either plasma glucose values or HbA1c.
It has also become apparent that subjects
with plasma glucose and HbA1c in the upper rangeof normal but still in the non-diabetic range have
an increased independent risk for CVD. In fact,
current epidemiological evidence indicates that
plasma glucose is a continuous variable with respect
to risk for CVD with no apparent threshold.
The relationship between hyperglycaemia and
CVD in people with T2DM was further illustrated
in the UK Prospective Diabetes Study (UKPDS).
However, improving glycaemic control with insulin
or sulphonylurea had only marginal outcome
benefits (a non-statistically significant reduction of
˜16%).9 The reasons for this could be many,
including: CVD is multifactorial; HbA1c concentrations
achieved in the intensive control arm may
have been insufficient; and postprandial hyperglycaemia
was not addressed—a concept which is
currently attracting much attention.
In the Kumomoto study where both fasting plasma
glucose and postprandial hyperglycaemia were targeted with intensive insulin treatment, thereduction in macrovascular events was halved,
although the limited absolute number of events did
not reach statistical significance. An ongoing trial,
the Action to Control Cardiovascular Risk in
Diabetes (ACCORD), will again evaluate the effect
of tight glucose control on CVD end points in
approximately 10 000 patients with T2DM followed
for 6 years, with additional secondary randomisation to aggressive blood pressure and lipid control.
Glucose control is also an important factor in determining outcome following coronary
intervention in people with diabetes. Corpus et al
studied 60 patients with diabetes and 179 patients
without diabetes undergoing elective percutaneous
coronary intervention. At 12 months, patients
with diabetes and HbA1c >7% had a significantly
higher rate of target vessel revascularisation compared with patients with diabetes and HbA1c <7% (34% vs 15%; p=0.02).
Isolated postprandial hyperglycaemia may also
be a clinically significant risk factor for CVD.Postprandial glycaemia in non-diabetic individuals
carries a greater risk than increased fasting glycaemia.
A meta-analysis of 20 studies in over 80 000
non-diabetic subjects by Coutinho et al found a
progressive relationship between fasting plasma
glucose and 2 h glucose and CVD mortality, with
no real threshold.
In the DECODE study, a metaanalysis of 13 prospective European cohort studies with almost 25 000 subjects without a history of diabetes, it was found that 2 h post-challenge hyperglycaemia after an oral glucose tolerance test was associated with increased mortality and was
also a better predictor of mortality than fasting
plasma glucose. The Diabetes Intervention
Study is thus far the only published intervention
study to demonstrate that controlling postprandial
hyperglycaemia (1 h after breakfast) has a greater
impact on cardiovascular and all cause mortality
than controlling fasting plasma glucose concentration.
Based on current evidence, probably what matters most is that blood glucose is brought within the normal range, not how that is done.
This is well illustrated in patients presenting with
acute MI as shown by the Diabetes Mellitus
Insulin-Glucose infusion in Acute Myocardial
Infarction (DIGAMI) 2 trial. DIGAMI 2 concluded
that for similar glycaemic control, insulin
treatment was not superior to the use of other
therapeutic options to lower blood glucose, as
regards mortality outcome.
Hence, subjects with T2DM presenting after an acute MI should have intensive glucose control by whichever means as long as glucose control is efficient.
A convenient way would be to start patients presenting with an acute MI and blood glucose >11.0 mmol/l on a 24 h insulin–glucose infusion followed by either
insulin treatment, oral hypoglycaemic agents or
dietary advice depending on blood glucose values.
Subcutaneous insulin treatment, if needed after
the 24 h insulin–glucose infusion, could be in theform of either a basal bolus regimen (short acting
insulin before meals and intermediate/long acting
insulin at bedtime) or pre-mixed insulin twice a
day before morning and evening meals.
A reasonable goal to aim for would be fasting blood glucose of 5–7 mmol/l.
A target for postprandial glucose remains contentious. The American Diabetes Association (ADA) recommends a value <10.0 mmol/l after subjects have achieved their
pre-meal glucose target, while the American
Association of Clinical Endocrinologists (AACE)
recommends a postprandial target <7.8 mmol/l. The European Association for the Study of Diabetes (EASD/IDF) has set a postprandial target of ≤7.5 mmol/l. Both the AACE and Joint British Society (JBS 2) guidelines recommend HbA1c ≤6.5%.
ORAL HYPOGLYCAEMIC THERAPY AND
CARDIOVASCULAR DISEASEMetformin, sulphonylureas and the thiazolidinediones
are the three most commonly used oral
hypoglycaemic agents.
Metformin
a biguanide derivative that reduces blood glucose values by attenuating hepatic gluconeogenesis.Metformin is also associated with a
variety of potentially beneficial cardiovascular
effects including weight stabilisation, improved
insulin sensitivity, improved endothelial function
and enhanced fibrinolysis. It has, however, been
considered that myocardial ischaemia represents a
contraindication to metformin due to a proposed
increased risk of lactic acidosis.
However, in large observational studies there is a lack of any cases of metformin associated lactic acidosis, while metformin concentrations do not correlate with lactate concentrations in individuals who develop lactic acidosis. Such considerations support the view that metformin may only be a bystander in sick patients, rather than a causal factor in the pathogenesis of lactic acidosis.
Hyperlactateaemia and lactic acidosis occur in the context of cardiogenic shock, and other illnesses that decrease tissue perfusion; in such patients it would thus be prudent to discontinue metformin treatment. In the metformin arm of the UKPDS (mean HbA1c 7.4%), overweight subjects treated with metformin had risk reductions of 32% (95% CI 13% to 47%; p=0.002) for any diabetes related end point, 42% for diabetes related death (95 % CI 9% to 63%; p=0.017) and 36% for all cause mortality (95% CI 9% to 55%;p=0.011).
Metformin is renally cleared and as long as its use is avoided in patients with significant renal impairment, it is reasonable to consider it as a first line oral hypoglycaemic agent in people with T2DM with or without myocardial ischaemia.
Sulphonylureas
produce reductions in blood glucose and HbA1c of a similar order of magnitude to that seen with metformin (1–2% fall in HbA1c and2–4 mmol/l in fasting plasma glucose) via a direct action on insulin production from b cells through amechanism involving activation of the sulphonylurea receptor (SUR-1); this is part of a transmembrane complex, the activation of which results in closure of potassium channels, membrane depolarisation, calcium influx and thus insulin release via calcium dependent channels.Questions relating to the cardiovascular effects of the sulphonylureas have been raised by the identification of isoforms of the sulphonylurea receptor on both vascular and cardiac smooth muscle.
Sulphonylureas that contain a benzamido group (glibenclamide, gliclazide, glimeparide) can
bind to these receptors and block the effects of the
K+ channel opener nicorandil. The clinical implications
of this action are unclear; however, there is atendency
to minimise the use of sulphonylurea treatment in high risk patients with coronary disease.
Thiazolidinediones
(TZDs) are agonists for the nuclear hormone receptor PPAR-c, which modulates gene expression, resulting in blood glucose reductions primarily by increasing insulin sensitivity in muscle liver and adipose tissue. The effect of any oral hypoglycaemic therapy on cardiovascular outcomes is particularly important,since more than 65% of deaths in patients with
T2DM are from cardiovascular causes.
Insulin resistance is recognised as a cardiovascular risk factor and numerous small studies have demonstrated that the TZD class of drugs may improve avariety of risk factors and surrogate markers of cardiovascular disease including blood pressure, microalbuminuria, carotid intima–media thickness, and coronary restenosis.
Trials
The only large scale outcome trial to date, theProspective Pioglitazone Clinical Trial in
Macrovascular Events (PROACTIVE), demonstrated
a relatively small but significant benefit,
but at the cost of an increase in heart failure.
However, a recent meta-analysis by Nissen et al17
suggests an increase in the risk of MI (OR 1.43,
95% CI 1.03 to 1.98; p=0.03) and an increase in
deaths due to CVD (OR 1.64, 95% CI 0.98 to 2.74;
p=0.06) associated with treatment with rosiglitazone.
These observations are, however, based on limited trial data (42 out of 116), with many contributing studies being small scale and short term, primarily designed to evaluate glycaemic control, with no event adjudication and an imbalance in follow-up, with more patients in
the control group withdrawing due to hyperglycaemia.
Furthermore, trials with no MIs were excluded and overall rates of events are low.
The actual number of events are relatively small (MI 86
vs 72; cardiovascular death 39 vs 22); thus, evensmall changes in the classification of these events,
which are not entirely robust since the data source
was not specifically designed to evaluate cardiovascular events, could lead to significantly different odds ratios.
The Rosiglitazone Evaluated for Cardiovascular and Regulation of Glycaemia in Diabetes (RECORD) trial is a long term multicentre,randomised open label study that compares cardiovascular outcomes in patients with T2DM treated with rosiglitazone plus metformin or sulphonylurea with outcomes in patients treated
with metformin plus sulphonylurea.
The results of UKPDS suggested that the comparators metformin and sulphonylurea reduced the MI rate by 39% and 16%, respectively, as compared with conventional treatment and diet.
Following the recent metaanalysis of the cardiovascular safety of rosiglitazone, an interim report evaluating the cardiovascular outcomes from this study has been presented.
A total of 4447 patients who had inadequate
glycaemic control (baseline HbA1c 7.9%) whilereceiving metformin or sulphonylurea monotherapy
were randomly assigned to receive add on
rosiglitazone (2220) or a combination of metformin
plus sulphonylurea (2220).
If the HbA1c exceeded 7.0% after 8 weeks of treatment the doses of study drugs were increased to maximum (8 mg rosiglitazone, 2550 mg metformin, 15 mg glyburide, 240 mg gliclazide and 4 mg glimeparide).
If HbA1c exceeded 8.5%, a third agent was
added in the rosiglitazone group, while insulin wasinitiated for patients in the control group.
If patients in the rosiglitazone group receiving triple
therapy had HbA1c values>8.5%, then rosiglitazone
was discontinued and insulin commenced.
The primary end point was hospitalisation or death from cardiovascular causes, with a mean follow up of 3.75 years. A total of 217 patients in the rosiglitazone group and 202 in the control group had the adjudicated primary end point (HR 1.08, 95% CI 0.89 to 1.31), with no statistical difference between the rosiglitazone and control groups regarding MI and death from cardiovascular causes.
Approximately 10% of patients in both groups were lost to follow up; this, coupled with the low event rate (3.1% per year), which may reflect the impact of concomitant cardioprotective therapies or potential difficulties with event ascertainment, limited the statistical power of this analysis as reflected by the relatively wide 95% confidence intervals.
Patients in the rosiglitazone group had a significantly higher risk of congestive heart failure, with 32 versus 17 adjudicated events; 6.5% of patients in the rosiglitazone group began to receive insulin as opposed to 10.9% in the control group, with 1476 patients in the rosiglitazone group and 1476 in the control group still receiving their allocated treatment at 3.75 years.
The results of this analysis at least partly address
some of the cardiovascular safety concerns raisedby Nissen and Wolski. The Record study has
several strengths in that it was a large randomised
long term study designed to assess the cardiovascular safety of rosiglitazone in the context of dual agent combination therapy, with all reported cardiovascular end points undergoing independent adjudication. This study also has some deficiencies, in that it is non-blinded, with a low event rate and significant drop out rate (around 10%), and is designed as a non-inferiority study, all of which may limit the statistical power of the study to
detect differences.
The overall cardiovascular safety profile of rosiglitazone is unclear, with potential mechanisms relating to any increased risk of coronary events reflecting the effects of an increase in intravascular volume on myocardial oxygen demands. Pioglitazone is also associated with fluid retention, yet the results of the PROactive study
suggested a cardiovascular benefit for pioglitazone.
The apparent discrepancy between rosiglitazone
and pioglitazone on cardiovascular events is
unlikely to be produced by the reported lipid
differences between the two agents.
The current cardiovascular data for both rosiglitazone and pioglitazone is based on patient populations of
notably different cardiovascular risk, which raises
the question as to whether there is a threshold
cardiovascular risk effect which impacts on the
potential outcome benefits of the thiazolidinediones.
It is, however, currently impossible to
assess the ‘‘class’’ effect of the thiazolidinediones
on cardiovascular disease, and the results of several
large ongoing end point studies are eagerly awaited
to address this issue.
HYPERTENSION AND CARDIOVASCULAR DISEASE
IN DIABETESNumerous trials have demonstrated the benefit of
blood pressure control for reducing cardiovascular
end points in patients with diabetes. Trial data also
seem to indicate that the greater the blood pressure
lowering, the greater the benefit, with no apparent
lower threshold.
In the UKPDS, subjects were randomised to either intensive blood pressure lowering treatment which achieved 144/82 mm Hg, or less intensive therapy which achieved 154/87 mm Hg. Reductions in risk in the group assigned to tight control were 24% in diabetes related end points (95% CI 8% to 38%; p=0.0046), 32% in deaths related to diabetes (95% CI 6% to 51%; p=0.019) and 44% for strokes (95% CI 11% to 56%; p=0.013). There were also 21% fewer MIs in the intensively treated group, but this reduction was not statistically significant. Atenolol and captopril were equally effective.
Various trials used a number of different antihypertensive drugs including (ARBs), (ACEIs),
b blockers, diuretics and calcium channel blockers (CCBs).
The ABCD, FACET and HOPE trials all showed
that ACEIs prevent cardiovascular events in
diabetes.
An important issue that affects the selection of
antihypertensive medication in patients withdiabetes relates to the metabolic side effects of
these agents. Several trials, including the largest
randomised comparison of b blockers/thiazide
diuretic combination against CCBs/ACEIs in primary
prevention of CVD (Anglo-Scandinavian
Cardiac Outcomes Trial-Blood Pressure Lowering
Arm (ASCOT-BPLA)),18 have all revealed an
increased risk of developing diabetes in people
treated with b blockers, especially when combined
with thiazides.
On the other hand, data from both animal and human studies have suggested afavourable metabolic profile for ACEIs and ARBs.
In one study, treatment of dyslipidaemic hypertensive
patients with losartan led to increased
circulating adiponectin concentrations and
improved insulin sensitivity. These effects have
an important bearing as most hypertensive
patients with diabetes have a high prevalence of
insulin resistance.
The JBS 2 guidelines recommend attaining a
blood pressure of 130/80 mm Hg for reducingcardiovascular risk in patients with diabetes.
Young (age ,55 years) white diabetic subjects
tend to have relatively higher renin values and
hence ACEIs are more effective as first line blood
pressure reducing agents.
In older subjects or those of African Caribbean descent, CCBs or thiazide diuretics tend to be more effective. Doxazosin increased the risk of congestive cardiac failure in the large Antihypertensive and Lipid Lowering treatment to prevent Heart Attack Trial (ALLHAT), so a blockers are not recommendedfor first line use.
Microalbuminuria is not only aprecursor to renal failure from diabetic nephropathy but also indicates a high risk of CHD and premature death. In these patients ACEIs and ARBs may be combined, but the importance of checking renal function after initiating either class of drug cannot be overemphasised, especially when combined.
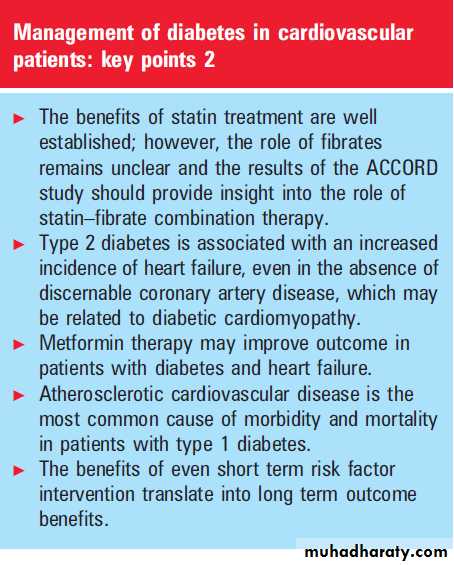
DYSLIPIDAEMIA AND CARDIOVASCULAR DISEASE
IN DIABETESThe treatment of hyperlipidaemia has a well
established role in reducing cardiovascular end
points in patients with diabetes. There are suggestions that the most effective single intervention to reduce cardiovascular risk in individuals with diabetes is lipid lowering with a statin. Indeed 70% of the risk reduction seen in the STENO-2 study was attributable to the lipid changes.
T2DM patients have an atherogenic lipid profile characterised by hypertriglyceridaemia, low high density lipoprotein (HDL) cholesterol, small, dense low
density lipoprotein (LDL) particles, and abnormal
apolipoprotein A1 (apoA1) and apoB metabolism.
These lipoprotein abnormalities improve with
good diabetes control, but remain abnormal even
when normoglycaemia is achieved.
Evidence for the use of statins to decrease
cardiovascular risk in subjects with diabetes comesfrom two large scale clinical trials.
The Heart Protection Study (HPS) included 5963 patients with diabetes who were prospectively randomised to treatment with simvastatin or placebo. Active treatment was associated with a 27% reduction (95% CI 15% to 38%; p,0.0001) in coronary events after a mean follow up of ,5 years.
The benefit of statin treatment was independent of
baseline LDL cholesterol values and subjects withan LDL cholesterol ,3.0 mmol/l gained the same
benefit as those 3.5 mmol/l .
Furthermore, subjects with diabetes benefited to the same extent as individuals who had previously had an MI.
In the Collaborative Atorvastatin Diabetes Study
(CARDS), 2838 patients with T2DM and noprevious history of CVD were randomised to
placebo or treatment with atorvastatin. After
3.9 years follow-up, treatment with atorvastatin
reduced acute CHD events by 36%, coronary
revascularisations by 31%, stroke by 48% and
overall death rate by 27%.
Based on the evidence from these two large scale studies, all individuals with T2DM should be considered for statin treatment irrespective of their baseline LDL cholesterol concentration.
The use of fibrates in subjects with T2DM, in
terms of reducing cardiovascular risk, is unclear.
Fibrates effectively decrease triglyceride concentrations by enhancing lipoprotein lipase activity, raising HDL cholesterol and increasing LDL particle size from dense to more buoyant.
Fibrates also increase the synthesis of apoA1, apoA2, scavenger receptor B1 (a hepatic receptor for B lipoproteins), and adenosine triphosphate binding membrane cassette transporter-1, which permits efflux of cholesterol from cells, thereby increasing HDL
concentrations. Subgroup data analysis from the
Veterans Affairs High Density Lipoprotein
Intervention Trial (VA-HIT) indicated that gemfibrozil
treatment was associated with a significant
32% reduction in major cardiovascular events.
It was unclear from these results whether increases in HDL cholesterol values, decreases in triglyceride
concentrations, or both, were responsible for the
beneficial effect on cardiovascular outcomes.
The Fenofibrate Intervention and Event
Lowering in Diabetes (FIELD) study was hence
designed, but the results were rather disappointing.
Fenofibrate did not appear to reduce significantly
the risk of the primary outcome of coronaryevents. These findings may have been confounded
by the fact that significantly more people in the
placebo group were allocated other lipid lowering
medications, predominantly statins, than in the
fenofibrate group (17% vs 8%; p,0.0001).
The ongoing ACCORD trial—in addition to studying
the effect of tight glucose control on CVD end
points in approximately 10 000 patients with
T2DM followed for 6 years—will also evaluate
whether combination therapy with statin and
fibrate is superior to statin alone in reducing
cardiovascular end points.
The Atorvastatin in Factorial with Omega-3 fatty acids Risk Reductionin Diabetes (AFORRD) is another ongoing randomised controlled trial assessing the degree to which LDL cholesterol and triglyceride lowering reduces
the estimated risk of CHD in subjects with T2DM.
The results should also provide insights into the
role of triglycerides in the development of CHD
and triglyceride lowering with omega-3 fatty acids
and CHD risk in people with T2DM.
The ADA guidelines now recommend a target
LDL cholesterol ,2.6 mmol/l, but the JBS 2guidelines have more stringent targets with total
cholesterol ,4.0 mmol/l and LDL cholesterol
,2.0 mmol/l. Based on current evidence, statins remain the drug of first choice.
Statins are recommended for all people with diabetes (type 1or type 2) aged >40 years and in younger people (18–39 years) with at least one other risk factor,including retinopathy, nephropathy, hypertension or features of the metabolic syndrome.
If targets are not reached on maximum tolerated doses of statin, then other agents including fibrates, omega 3 fatty acids, nicotinic acid or ezetimibe may be added; however, there are as yet no studies with
hard outcome data showing that lowering cholesterol
with a statin in addition to any of these
agents is better than a statin alone in reducing
cardiovascular risk.
Hence, the decision on which agent to add to a statin will depend on the dyslipidaemic profile and tolerability. Although there are currently no outcome data to support interventions that increase HDL cholesterol or decrease triglyceride concentrations, these parameters should not be ignored and must be
addressed once statins have been initiated for
LDL cholesterol control.
NON-TRADITIONAL CARDIOVASCULAR RISK
FACTORS AND DIABETESFactors other than hyperglycaemia, hypertension
and lipid disorders may contribute to the increase
in cardiac events in diabetic patients. Circulating
levels of fibrinogen and other coagulation factors
are raised in diabetes. Platelets from diabetic
subjects show increased adhesiveness, and also
fibrinolytic activity is often suppressed via the
inhibitory actions of plasminogen activator inhibitor.
Aspirin inhibits platelet function and its role in secondary prevention is well established.
However, the evidence for its benefit in primary
prevention in individuals with diabetes is limited.
A Study of Cardiovascular Events in Diabetes
(ASCEND) will compare aspirin and omega-3 fatty
acids both in combination and individually with
placebo in primary prevention in 10 000 people
with diabetes.
Smoking greatly increases the risk of macrovascular disease and stopping smoking may be as beneficial as any other intervention discussed in this review. Obesity is clearly linked to T2DM and CHD, and diet and exercise lowers glucose concentrations and raises insulin sensitivity.
Cardiac denervation due to neuropathy may also
play a part.
Vagal denervation of the heart results
in tachycardia and decreased diastolic filling ofcoronary arteries because of a shortened diastole
and myocardial ischaemia.
In addition, autonomic neuropathy is associated with failure of night time dips in blood pressure.
HEART FAILURE AND DIABETES
People with diabetes have an increased risk ofdeveloping heart failure, both as a consequence of
coronary artery disease and as a result of cardiomyopathy, which may be due to a microangiopathy or primary cardiomyocyte dysfunction. Indeed, diastolic left ventricular dysfunction is a consistent observation through all levels of glucose intolerance.
In a study examining electronic records of ,8500
patients with T2DM, the prevalence of heart failure
was found to be 11.8% compared with 4.5% in age
and sex matched controls.
Once heart failure develops in individuals with diabetes mellitus, they appear to have a poorer prognosis than patients without diabetes.
A number of factors contribute to the risk of developing heart failure in diabetes,
including duration of diabetes, age, presence of CHD,
elevated serum creatinine and poor glycaemic control,
with an 8% increase in relative risk for every 1%
increase in HbA1c.
Cardiomyocytes in diabetes are insulin resistant and insulin sensitising therapy may thus be considered as a rational treatment option in people with diabetes and heart failure. Indeed, improved clinical outcomes have been associated with metformin in patients with diabetes and heart failure.
TZDs are contraindicated in patients with any evidence of heart failure caused by potential fluid retention, and caution must be exercised with the use of metformin as many patients with heart failure also have concomitant renal impairment. The current management of patients with heart failure and diabetes is thus focused on optimal risk factor management and metabolic control.
SUMMARY
Although this review has focused predominantly on T2DM, CVD is also the most common cause of morbidity and mortality in people with type 1diabetes, with duration of diabetes, blood pressure,dyslipidaemia and glucose control all being important determinants of outcome.Hence multiple risk factor intervention is an integral part of the management of cardiovascular disease in people with both type 1 and type 2 diabetes.
Therapeutic strategies, along with increasingly aggressive treatment goals, should have an impact on the cardiovascular burden associated with diabetes.
A 1% reduction in HbA1c reduces CHD risk by approximately 16%.
Post-myocardial infarction intensive blood glucose control irrespective of means is the important therapeutic target.
The benefits of cholesterol reduction in people with type 2 diabetes occur independent of pre-treatment cholesterol values.
A 75 gram oral glucose tolerance test should be conducted between 4-7 days following an acute coronary event .
A blood pressure target of <130/80 mm Hg is advocated in people with type 2 diabetes