Diagnosis, classification, and treatment of diabetes
BMJ 2011د. حسين محمد جمعة
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
A recent report from the Royal College of General Practitioners and NHS Diabetes suggests that the diagnostic classification of 10-15% of patients with diabetes in general practice may be inaccurate, and that this may have a considerable effect on
patient care.
The report proposes a new approach to the classification of different types of diabetes and calls for greater efforts in checking the accuracy of diagnoses, along with efforts to improve education and classification in primary care. Are these concerns justified, and are the solutions proposed practical?
The stereotypes of the older obese patient with gradually rising blood glucose and the younger non-obese patient presenting acutely and requiring immediate treatment with insulin are no longer sufficient to classify people as having type 1 or type 2 diabetes. Conventional criteria for diagnosis include age of diagnosis, presence of ketoacidosis, and body mass index.
However, with increasing obesity in younger people, the wider use of insulin for type 2 diabetes, and an awareness of the existence of genetic forms of diabetes, there is concern about the risk of misclassification and misdiagnosis, with adverse consequences. The report provides evidence that these concerns are justified.
The report provides two strands of evidence that suggest an important problem. The first is a systematic review on the miscoding and misclassification of diabetes. Studies provided examples of the misdiagnosis of type 1 diabetes as type 2,leading to delays in starting insulin and inappropriate use of oral antihyperglycaemic drugs. They also provided examples of the mislabelling of type 2 diabetes as type 1, particularly in those taking insulin, and the relabelling of type 1 diabetes as type 2 diabetes in older people. Such errors may lead to incorrect management decisions.
The second strand of evidence comes from a series of studies that investigate the extent of misclassification in two research databases and through an audit of computerised primary care medical records. In a practice of 10 000 people, between 410 and 500 patients are likely to have diabetes. Between 60 and 65 of these patients will have some form of error that needs further review.
Seven to 16 of these patients will be misclassified—most will be patients with type 2 diabetes who are recorded as having type 1 diabetes. About 21 people will have been misdiagnosed as having diabetes when they do not have diabetes at all, and 24-37 people will have been miscoded so that it is not possible to determine what type of diabetes they have.
The complexity of classifications based on the cause of diabetes may contribute to the problem. Current guidelines define type 1 diabetes as an autoimmune disease and type 2 diabetes as acondition with a relative deficit of insulin and insulin resistance.
Nine further categories reflect genetic defects associated with β cells and insulin action, pancreatic disease, endocrinopathies,drugs, infections, immune mediated conditions, other genetic conditions, and gestational diabetes.
It is not currently feasible to use this approach to classification for diagnostic testing. For example, although it is possible to test for markers of the autoimmune destruction of β cells, it is impractical to use the results as a basis for treatment decisions because of both false positive and false negative results.
Specific tests are now available for some forms of monogenic diabetes, but the costs of using them routinely are prohibitive, and the continuing discovery of further genetic variants means that negative testing cannot confidently exclude the diagnosis. The report therefore outlines a simplified categorisation based on clinical features that provides a starting point for clinical staff when assessing a patient.
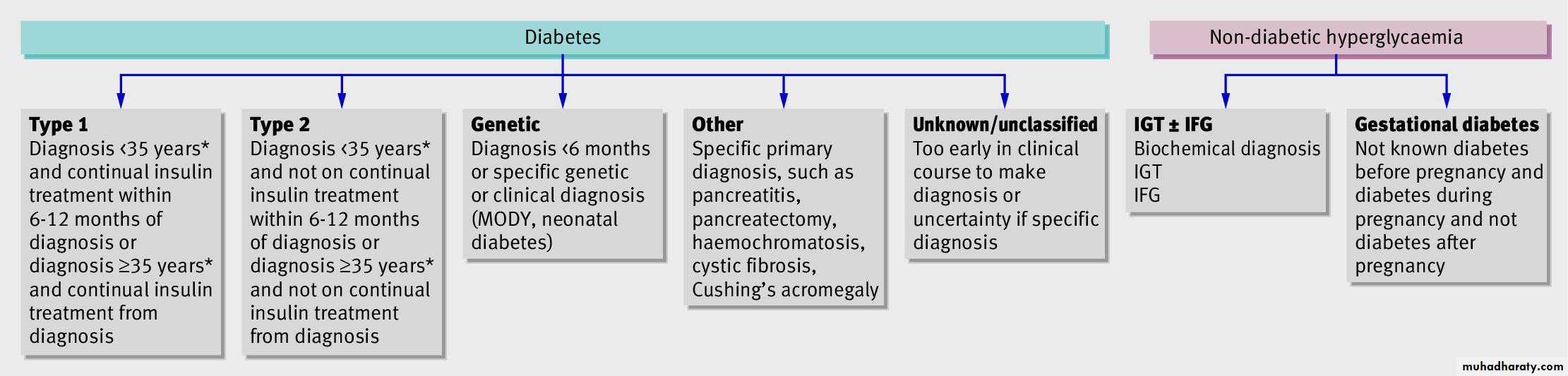
The report sets out pragmatic guidelines for classifying diabetes .Diabetes is separated from non-diabetic hyperglycaemia. A starting point is suggested for diagnosingtype 1 and type 2 diabetes, and the genetic and secondary forms of diabetes are separated into broad categories. A category is proposed for when the diagnosis is unclear, and continuing review of the diagnosis over a period of time may lead to a
revised assessment.
The major concerns of this report are the problems of misclassification of type 1 and type 2 diabetes, but there are also continuing concerns about the identification of genetic forms of diabetes in primary care. Review of all patients with diabetes in specialist centres is not feasible, so awareness of the need for expertise in clinical assessment, particularly in those diagnosed between the ages of 25 and 45 years, and appropriate testing for the cause in specific circumstances are required.
For example, there are probably around 5000 patients with one form of genetic diabetes—maturity onset diabetes of the young caused by mutation of the HNF1A gene—in the United Kingdom, but only 10% are diagnosed. Many of those who are not diagnosed may be unnecessarily receiving treatment with insulin. Although the use of universal genetic testing for young onset diabetes remains prohibitively expensive, promising low cost screening tests are being evaluated.
There is a need to ensure that the small
but important minority of patients with the less common forms of diabetes receive appropriate care. If these sensible proposals for general practice care are not implemented, people withdiabetes will continue to be misclassified, misdiagnosed, and miscoded across the UK.
Practical classification guidelines. *In high risk racial
groups a cut off of 30 years should be used.MODY=maturity onset diabetes of the young; IGT=impaired
glucose tolerance; IFG=impaired fasting glucose
BMJ 2011