Insulin-Pump Therapy for Type 1Diabetes Mellitus
nejm. org april 26, 2012د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
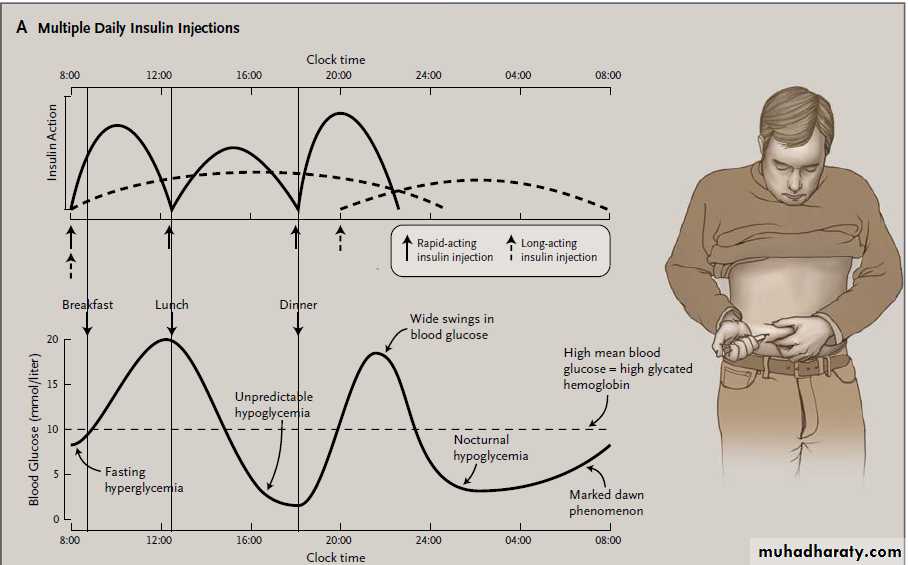
The Clinical Problem It is now well established that the serious microvascular complications of diabetes are linked to the duration and severity of hyperglycemia; there have therefore been renewed efforts to help patients achieve near-normal blood glucose levels. The mainstay of current management of type 1 diabetes is “physiological insulin replacement,”
the main example of which is the practice of administering multiple daily injections of insulin.
Several organizations have set targets for glycemic
control; for example, the American Diabetes Association recommends a general goal for glycated hemoglobin levels of less than 7%, though it recommends less stringent targets for some persons.However, in everyday clinical practice, it is
widely recognized that such targets are easier to set than to achieve.4 In a Scottish registry of 24,750 patients with type 1 diabetes,5 only 7% had a glycated hemoglobin level of less than 7%, and in an Australian survey of patients with type 1 diabetes, 4 13% had a glycated hemoglobin level of less than 7%.As glycemic control improves with intensified insulin regimens, the frequency of hypoglycemia tends to increase. Hypoglycemia is the cause of considerable stress and anxiety, impaired well-being, and poor quality of life in patients with type 1 diabetes, and 35 to 40% of patients with type 1 diabetes regularly have an episode of severe hypoglycemia (an episode necessitating third-party assistance).
About 25% have blunting of the symptoms of hypoglycemia — known as hypoglycemia unawareness — and such patients have a risk of severe hypoglycemia that is increased by a factor of up to 6.7-9 Hypoglycemia has been called the single greatest barrier to achieving and maintaining good glycemic control in patients with diabetes.
PATHOPHYSIOLOGY AND EFFECT OF THERAPY
One reason for continued poor glycemic controlin patients with type 1 diabetes is the erratic absorption
and action of subcutaneously injected
insulin,10 which lead to unpredictable swings in
blood glucose concentrations, and those swings,
in themselves, are associated with elevated glycated
hemoglobin levels11 and hypoglycemia12,13 (Fig. 1).
It is likely that patients with high variability in glycemic levels maintain an elevated glycated hemoglobin level because they fear that hypoglycemia will occur more frequently or will be more severe if glycemic levels are reduced.
Another reason for continued poor glycemic control is that the dose of long-acting insulin analogues cannot be modulated after injection — for example, to provide greater insulin delivery from the previously injected depot in the prebreakfast hours, in order to counter the increase in blood glucose levels at that time of day
(“dawn phenomenon”).
At meals, errors in estimating the size and composition of the meal and in the timing and magnitude of the preprandial insulin dose can cause excessive hyperglycemia or late hypoglycemia. Adjustment of
the insulin dose to account for exercise is daunting
for many patients. The frequency of hypoglycemia
unawareness and the risk of subsequent
hypoglycemia are highest among patients who
have had hypoglycemia most frequently in the
past. Finally, nonadherence to recommended
therapy is a contributor to poor control in a substantial
number of patients.
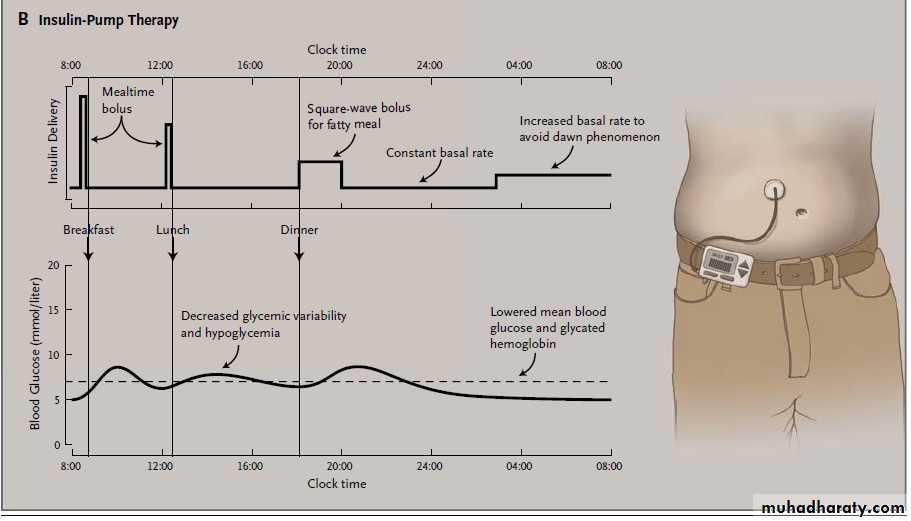
Insulin-pump therapy, or continuous subcutaneous
insulin infusion, was introduced more than
30 years ago as a procedure for improving
glycemic control in patients with type 1 diabetes
by mimicking the insulin-delivery patterns that
are present in persons without diabetes. A portable
pump infuses rapid-acting insulin at a slow
basal rate, 24 hours a day, through a fine cannula
implanted in the subcutaneous tissue, with
patient-activated insulin boosts (boluses) administered
at mealtimes (Fig. 1).
With insulin pumps in current use, the basal rate can either be altered on demand or preset to change at any time (e.g., during the night), and an onboard bolus
calculator can advise the patient regarding the
appropriate insulin dose at mealtime, as estimated
on the basis of carbohydrate intake, premeal and target blood glucose levels, insulin sensitivity,and a calculation of the insulin remaining since the previous bolus.18 Currently available pumps also have the capability for downloading data to a computer.
Insulin-pump therapy can improve glycemic control in patients with type 1 diabetes because it can reduce the within-day and between-day glycemic variability that is seen with insulin injections.
This effect may be related to the smaller subcutaneous depot of insulin during pump therapy (about 1 unit) and the low coefficient of variation for absorption during the basal-rate infusion — about ±3%, as compared with about ±50% for a large dose of injected isophane insulin. The reduction in glycemic
fluctuations allows patients to reduce glycated hemoglobin levels without increasing the risk of
hypoglycemia.
Insulin-pump therapy may also lessen the problems of glycemic control associated with injections because it allows for more flexible, preprogrammable basal insulin rates and extended-wave insulin profiles that can reduce the risk of hyperglycemia after fatty meals; because it includes a bolus calculator23; and because it includes the capability for computer downloads, which may identify control problems and aid in the adjustment of doses. In addition, one may
speculate that the increased flexibility of diabetes
management and the improved feeling of wellbeing
in patients who have an insulin pump may increase adherence to intensified therapy.
CLINICAL EVIDENCE
Several meta-analyses of randomized, controlledtrials of glycemic control with multiple daily insulin
injections as compared with insulin-pump therapy
have shown that mean glycated hemoglobin levels
are significantly lower with insulin-pump therapy
— with a mean difference of about 0.3 to 0.6%
between treatments — and this reduction in gly cated hemoglobin levels is accompanied by a 10 to20% reduction in the dose of insulin.
Among patients who switch from insulin injections to
insulin-pump therapy, the most important determinantof the benefit of pump therapy with respect
to glycemic control is the baseline glycated
hemoglobin level, with the greatest effect seen in
patients with the worst control at baseline.
For example, the expected mean decrease in the
glycated hemoglobin level is about 2 percentage
points when the baseline glycated hemoglobin is
10%, whereas it is 0 percentage points when the
baseline glycated hemoglobin is 7%.11
In a 2008 meta-analysis, the frequency of severe
hypoglycemia was compared among patients
receiving insulin-pump therapy and those
receiving multiple daily insulin injections; the
selected trials had a duration of 6 months or
more, were published between 1996 and 2006
(when monomeric insulin was used in the
pump), and included a study population that had
a high initial rate of severe hypoglycemia.
The meta-analysis showed that the frequency of severe
hypoglycemia was significantly higher with multiple daily insulin injections than with insulin-pump therapy (rate ratio, 4.19; 95% confidence interval, 2.86 to 6.13).28 The greatest reduction was seen among patients who had had the greatest number of episodes of severe hypoglycemia while they were receiving injection therapy. Among these patients, the rate of severe hypoglycemia was higher by a factor of about 30 with multiple daily insulin injections than withinsulin-pump therapy.
Several trials have also evaluated quality of life
among patients receiving insulin-pump therapy,with the use of a variety of measures. Although
the findings differ across trials and a metaanalysis
was not appropriate because of the use
of different scales, a Cochrane review concluded
that in many studies, pump therapy was preferred
over multiple-dose insulin injections with
respect to treatment satisfaction, quality of life,
and perception of general and mental health.
CLINICAL USE
Most people with type 1 diabetes can achieve acceptable control with multiple daily insulin injections when this therapeutic approach is applied sufficiently rigorously. It is therefore best to reserve the use of insulin-pump therapy for patients who have indications for which there is robust evidence for benefit (Table 1). In adults, these indications generally include poor control of hyperglycemia or disabling hypoglycemia, despite best efforts to achieve glycemic control with multiple daily insulin injections, although the specific criteria for these indications vary.
For example, the U.K. National Institute for Health and Clinical Excellence (NICE) recommends consideration of insulin-pump therapy for patients with persistent glycated hemoglobin levels of 8.5% or higher, whereas the Société Francophone du
Diabète uses a threshold of 7.5% or higher.
Although the same indications generally apply
to children, many pediatricians consider multipledaily insulin injections to be impractical or inappropriate for some children, because the children
may be unable or unwilling to inject insulin at
school and may need assistance from parents during
the day. Some experts therefore suggest that
children may be considered for pump therapy
without having first failed to have adequate glycemic
control with insulin injections.
Particular challenges in the treatment of adolescents, with respect to both multiple daily insulin injections and insulin-pump therapy, include nonadherence, insulin resistance, and changing activity and sleep patterns.
Though these variables are often managed
more effectively with pump therapy than with multiple daily insulin injections, some studies haveshown that teenagers are the population that is
most likely to have elevated glycated hemoglobin
levels while receiving insulin-pump therapy and
subsequently to discontinue the treatment.
Insulin-pump therapy may be used during
pregnancy. However, the consequences of
ketoacidosis during pregnancy (for example, if
pump failure were to occur) are of particular
concern. Nonetheless, it is reasonable to apply
the above criteria for initiating pump therapy to
pregnant women also, but with adjustment for the lower target levels of glycated hemoglobin
that are needed during pregnancy.
Insulin-pump therapy should be initiated by a
specialized hospital team comprising a physician,a diabetes nurse, and a dietitian trained in
pump procedures. Initiation of pump therapy by
primary care physicians is not recommended. It
is important for the patient to be willing and
motivated to use the insulin pump.
The necessary commitments include frequent self-monitoring of blood glucose levels (four to six times daily),
carbohydrate counting (adjustment of the insulin
dose according to the estimated amount of carbohydrate
in an intended meal), and working with the pump team to learn pump procedures.
Starting insulin-pump therapy is generally contraindicated when a clinical team that specializes
in this treatment is not available, when the patient
is unwilling or unable to use the pump, or
when the patient has major psychiatric problems.
Commercially available insulin pumps contain
a reservoir that holds about 200 to 300 units of
insulin, a battery with an effective life of several
weeks, and electronic controls for the operation
of the pump.
Pumps usually have a display screen and controls to allow the user to enter information on dose and time. Most pumps deliver insulin through a flexible plastic tube, typically 60 or 110 cm in length and terminating in a Teflon cannula or stainless-steel needle, which is inserted into the subcutaneous tissue. The cannula may be implanted manually or automatically with the use of a spring-loaded device.
One currently available pump is “tubeless,” with the cannula integrated into the pump and a hand-held controller that is used to adjust rates.
Other small “patch pumps” of this type, in which the pump is attached to the body with an adhesive patch (some including a remote-control device), are in development.
Monomeric, rapid-acting insulin analogues
(aspart, lispro, or glulisine) are now consideredto be the insulins of choice for pumps. For selecting
the initial basal rate, the total daily injected
dose is calculated and then is usually reduced
by 20%. The basal rate is then calculated
as 50% of that value; initially, only one rate is
used for the entire 24-hour period, with varying
rates introduced later. The overnight rate should
be adjusted to maintain the prebreakfast blood
glucose concentration in the target range.
Carbohydrate counting is used to determine the
bolus dose before a meal, which is based on
the carbohydrate content of the intended meal;
the patient’s insulin sensitivity at meals (“insulinto-
carbohydrate ratio”); and a correction dose that is based on the blood glucose level before the meal, how far that level deviates from the target blood glucose level, and the insulin sensitivity factor.
There are formulas that can be used to estimate the insulin-to-carbohydrate ratio (e.g., 500 ÷ total daily insulin dose = grams of carbohydrate for each unit of insulin) and the insulin sensitivity factor (100 ÷ total daily insulin dose = blood glucose lowering [in millimoles per liter] for each unit of insulin; this calculation is also used to correct unexplained hyperglycemia between meals).
When the blood glucose is expressed in milligrams per deciliter, the insulin sensitivity factor is calculated as 1800 ÷ total daily insulin dose. Many patients now use bolus calculators to estimate insulin doses before meals.
The anterior abdominal wall is the most common
infusion site; the outer thighs, arms, hips, and buttocks can be used but generally have slower insulin absorption.
Areas of broken skin, lipodystrophy, or scarring should be avoided.
The infusion cannula should be changed every 2 to3 days and rotated to a new anatomical site —
just as the site of insulin injections should be
varied — to avoid lipohypertrophy. Keeping the
same infusion set in place for longer than 3 days
is associated with deterioration in glycemic control
and an increased risk of infection at the site.
After an initial start-up phase of approximately
6 months, when clinic visits or contact with health care professionals may be more frequent,
most patients who are receiving insulinpump
therapy do not need to be followed in the
outpatient clinic more often than was necessary
when they were receiving multiple daily insulin
injections — approximately every 6 months.
When patients receiving insulin-pump therapy
are admitted to the hospital as inpatients foremergency or elective treatments and investigations,
most prefer to continue receiving pump
therapy; however, since the hospital staff may be
inexperienced with continuous subcutaneous insulin
infusion, advice from the local insulin-pump
team and adherence to specific insulin-pump
protocols are strongly recommended.
Continuous subcutaneous insulin infusion is more expensive than multiple daily insulin injections:
insulin pumps cost about $5,000 to $7,000,
depending on the manufacturer and the country
of purchase, with additional costs (about $2,500
per year) for pump supplies (infusion sets, reservoirs,
and batteries) and for staff time and training.
Cost-effectiveness studies indicating that insulin-pump therapy may be considered to be cost-effective.
About 20% of patients who are receiving insulin-
pump therapy continue to have problematic
hypoglycemia or hyperglycemia. Such patients
may have further improvement with the addition of continuous glucose monitoring.
For this approach, a needle-type or wire-type
glucose sensor is implanted subcutaneously and
replaced about every 5 to 7 days. The sensor
measures interstitial glucose concentrations on
a nearly continuous basis. Data are transmitted
wirelessly to a portable meter or (in the case of
some models) to an insulin pump for display of
glucose values and trends.
In consultation with the patient, insulinpump
therapy should be discontinued if there isno sustained improvement in glycated hemoglobin
levels or the frequency or severity of hypoglycemia,
if psychiatric or other contraindications
emerge after the initiation of pump treatment,
or, possibly, if the patient has recurrent skin
infections. In addition, pump therapy should, of
course, be discontinued if the patient wishes to
return to the regimen of multiple daily insulin
injections. However, at most centers the rate of
discontinuation is only about 5% or less.
ADVERSE EFFECTS
Because there is a smaller subcutaneous depot of
insulin at any time with the insulin pump, there
is a greater risk that ketoacidosis will develop
with insulin-pump therapy than with multiple
daily insulin injections if, for example, insulin
delivery is interrupted because of a pump malfunction
or insulin demand is increased because
of an intercurrent illness. However, in practice,
the frequency of ketoacidosis is similar with the
two treatments, probably because regular
self-monitoring of blood glucose levels and a
prompt response to hyperglycemia are key parts
of modern pump practice.
Among patients at experienced centers, the frequency of ketoacidosis can be lower with insulin-pump therapy than with multiple daily insulin injections. Localized skin infections at the infusion site occasionally occur with insulin-pump therapy, but they
are rarely serious. Current pumps are robust
and reliable, but malfunctions can still occur.
Patients and health care professionals need achecklist of possible reasons for unexplained hyperglycemia, with the list including problems with the cannula (kinked, blocked, or leaking cannula or failure of the cannula to prime after change), problems at the infusion site (infection, lipohypertrophy, dislodgment of the infusion set, or a set that has been left in place for longer
than 3 days), malfunction of the pump (low battery,
inactive insulin or insulin past the expiration date, or mechanical or electrical failure with alarms), and patient-associated issues (missed bolus, incorrect basal rates, overcorrection of hypoglycemia, illness, use of drugs such as steroids,or menstruation).
Similarly, a checklist for unexplained hypoglycemia may include incorrect bolus or basal rates, performance of exercise without consumption of extra carbohydrates or reduction of the bolus or basal rate, delayed effect
of exercise, target levels that are set too low,
consumption of alcohol, gastroparesis, and inadequate
self-monitoring of blood glucose levels.
Areas of Uncertainty
It is unclear to what extent structured diabeteseducation programs such as the Dose Adjustment
for Normal Eating (DAFNE) program48 and
more enthusiastic input from health care professionals
would lessen the proportion of patients
who have elevated glycated hemoglobin levels
and hypoglycemia while they are receiving insulin-
injection therapy and who are thus candidates
for insulin-pump therapy.
There are relatively few randomized, controlled trials of insulin-pump therapy as compared with multiple daily insulin injections of the long-acting analogue insulins glargine and detemir, and more research into these regimens as part of DAFNE-type programs
would be helpful.
The expansion of patient groups selected for insulin-pump therapy beyond those with grossly elevated glycated hemoglobin levels and frequent episodes of hypoglycemia is also the subject of debate. The enhanced quality of life noted by many patients who are receiving pump therapy includes improvements in lifestyle flexibility, energy, wellbeing, family relationships, and the ability to perform effectively and confidently at work.These aspects are not easily captured by osteffectiveness studies.
Poor quality of life is mentioned in some guidelines as a criterion for selection of insulin-pump therapy (see below), but it is likely that increasing attention will be paid in the coming years to lifestyle issues and personal preference as indications for pump therapy.
Guidelines
The NICE guidelines recommend insulin-pumptherapy for adults when, despite the best attempts
to achieve target blood glucose levels with multiple
daily insulin-injection therapy, disabling hypoglycemic episodes continue to occur or glycated
hemoglobin levels remain high (≥8.5%) and
for children younger than 12 years of age whenever
multiple daily insulin injections are considered
to be impractical or inappropriate.
The guidelines for insulin pumps from the American
Association of Diabetes Educators notably alsoinclude “frequent and unpredictable fluctuations
in blood glucose” and “patient perceptions that
diabetes management impedes the pursuit of personal
or professional goals” as criteria for starting
pump therapy, and other guidelines cite similar
indications. However, many consider these indications
to be inadequately defined and believe
that they should be used as criteria only if there
is strong evidence that they have been associated
with hyperglycemia or hypoglycemia.
Recommendations
The patient described in the vignette has been
unable to achieve acceptable glycemic control
with multiple daily insulin injections — despite
having recently attended a diabetes education
course — because of disabling, severe hypoglycemia.
The hypoglycemia is probably due in part to
unpredictable glycemic fluctuations, which have
also prevented the lowering of glycated hemoglobin
to target levels.
If, after undergoing an assessment at a specialized center and discussing the options with a team that is experienced in insulin-pump therapy, the patient is willing and able to undergo a trial of such therapy, this should be arranged. It is to be expected that the
frequency of severe hypoglycemia will be reduced
and glycated hemoglobin levels will be lowered
and that the patient’s quality of life will improve.
His body-mass index may also be reduced, since
there will be less need for him to eat in order to
avoid hypoglycemia, and improved control may
be attained with a lower dose of insulin.