د. حسين محمد جمعة
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Primary Hyperparathyroidism
NEJM december 22, 2011A 62-year-old woman is found on routine laboratory testing to have a serum calcium level of 10.8 mg per deciliter (2.7 mmol per liter) (normal range, 8.4 to 10.4 [2.1 to 2.7]).
The serum intact parathyroid hormone (PTH) concentration is 70 pg per milliliter (normal range, 15 to 75). Her history is notable only for hypertension that is well controlled with an angiotensin-receptor blocker; there is no history of kidney stones or fractures. Her family history is negative for hypercalcemia or endocrine tumors. Her 24-hour urinary calcium and creatinine levels are 280 mg and 1050 mg, respectively,and the ratio of calcium to creatinine clearance is 0.025. Bone densitometry shows T scores at the lumbar spine of −1.8, at the total hip of −2.2, and at the distal third of the radius of −3.0. How should she be further evaluated and treated?
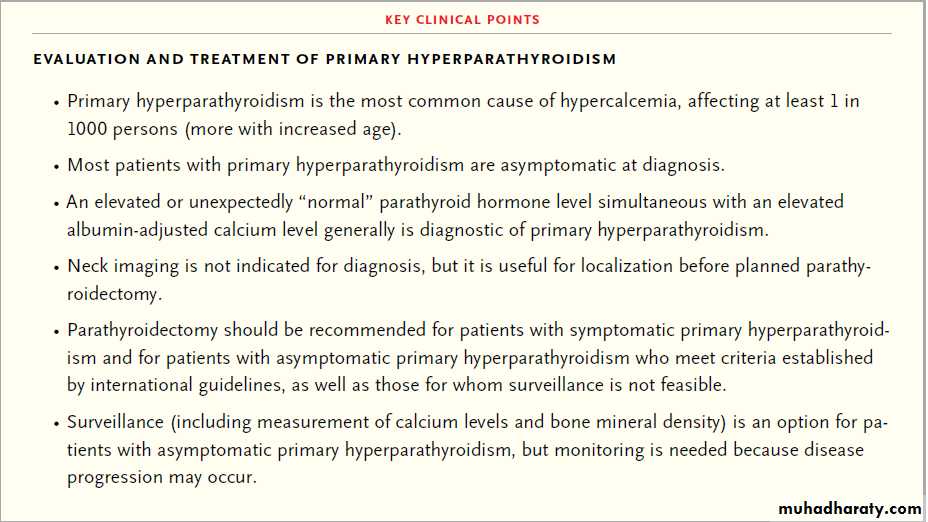
Primary hyperparathyroidism is the most common cause of hypercalcemia and should be considered in any person with an elevated serum calcium level. In the
1970s, the estimated prevalence of primary hyperparathyroidism ranged from 1 case per 1000 persons in the United States2 to 4.3 cases per 1000 persons in Sweden. In Sweden, there was an estimated prevalence of 2.1 cases per 100 women between the ages of 55 and 75 years in the early 1990s.
Data from the Rochester Epidemiological Project showed that the incidence of primary hyperparathyroidism increased sharply in the United States in July 1974, when the serum calcium level was included in the standard chemistry panel; from 1993 to 2001, the estimated incidence was approximately 22 cases per 100,000 persons per year.
With increased detection by means of routine calcium screening, the clinical profile of primary
hyperparathyroidism in Western countries has shifted from a symptomatic disease, characterized by hypercalcemic symptoms, nephrolithiasis, overt bone disease, and neuromuscular symptoms to one with subtle or no specific symptoms (“asymptomatic”
primary hyperparathyroidism). In the developing world, the symptomatic variant still dominates.
The incidence of primary hyperparathyroidism peaks in the seventh decade.
Most cases occur in women (74%), but the incidence is similar in men and women before 45 years of age.Etiologic Factors
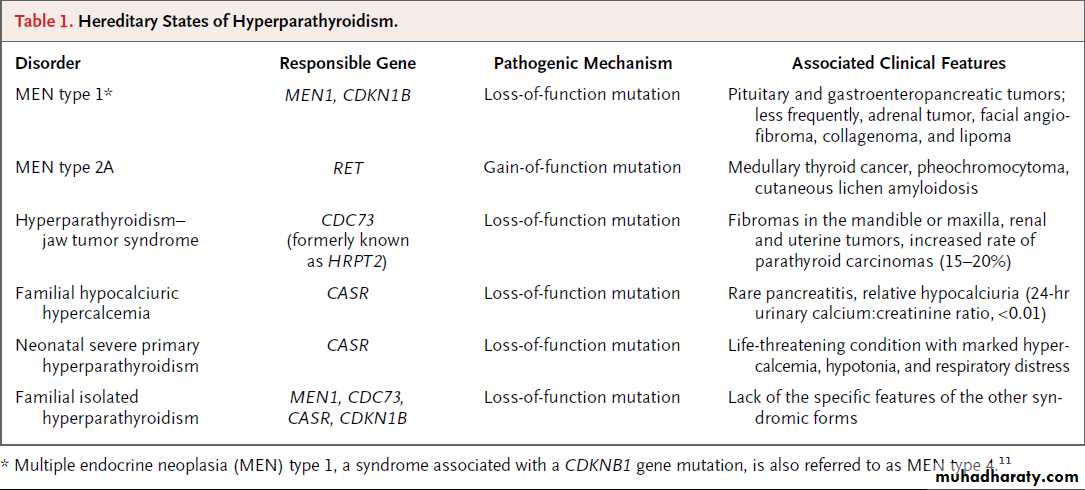
Head and neck irradiation in childhood and long-term lithium therapy10 are associatedwith a greater prevalence of primary hyperparathyroidism. Primary hyperparathyroidism,
which is most often caused by a single adenoma (80 to 85%) or four-gland hyperplasia (10 to 15%), mainly occurs as a sporadic disease, but it may
be part of a hereditary syndrome (e.g., multiple endocrine neoplasia types 1 and 2A) (Table 1).
Clinical Presentation
Classic symptoms and signs of primary hyperparathyroidism are rare today, but nephrolithiasisstill occurs in 4 to 15% of cases. Patients may have weakness, easy fatigability, anxiety, and cognitive impairment even when the level of serum calcium is modestly increased. Associated insulin resistance, hyperglycemia, and dyslipidemia (decreased levels of high-density lipoprotein cholesterol and increased levels of total triglycerides) have been reported, but it remains unclear how often these are attributable to the hyperparathyroidism and whether they are ameliorated by surgery.
Hypertension is also common and, with sophisticated testing (which is not routinely performed), subtle cardiovascular changes (i.e., increased vascular stiffness and endothelial dysfunction) may be detected. Low bone mineral density, particularly at sites enriched in cortical bone (e.g., the distal third of the radius) is common. Cross-sectional studies show an increased rate of fractures among persons with primary hyperparathyroidism; in one prospective study, the rate of morphometric (but not clinical) vertebral fracture was increased among asymptomatic postmenopausal women with primary hyperparathyroidism, as compared with age-matched controls.
Normocalcemic primary hyperparathyroidism
(increased PTH concentration in the absence ofhypercalcemia) has been recognized, typically
among persons evaluated for low bone mineral
density (whose assessment may include measurement
of both calcium and PTH). This diagnosis
should be made only after all causes of secondary
hyperparathyroidism have been ruled out.
Natural History
The natural history of primary hyperparathyroidismvaries according to its severity. Symptomatic
patients who do not undergo surgery usually
have worsening disease (particularly recurrent
nephrolithiasis). Conversely, long-term observational
studies have shown stability up to 8 years in biochemical measures (serum calcium,PTH, creatinine, and urinary calcium) and in bone mineral density in the majority of asymptomatic patients, whose serum calcium level is typically within 1 mg per deciliter (0.25 mmol per liter)
above the upper normal range.
However, about one third of patients have worsening of hypercalcemia, hypercalciuria, and decreases in bone mineral density at cortical sites, with progression
more likely among those with the longest followup
and those who are younger at study entry.
Short-term follow-up (1 to 3 years) of asymptomatic
patients with mild primary hyperparathyroidism
has indicated stability of markers of bone turnover, lipid and glucose levels, and echocardiographic indexes.
The natural history of normocalcemic primary hyperparathyroidism is not known, but, in a longitudinal study with amean follow-up of 3 years, hypercalcemia developed in 7 of 37 patients (19%).
The risk of death from cardiovascular causes
is increased among patients with moderate-to severe primary hyperparathyroidism and persists long after successful parathyroidectomy,suggesting that there may be irreversible cardiovascular damage. Most studies
suggest that patients with asymptomatic primary
hyperparathyroidism do not share this risk.
Evaluation
The finding of hypercalcemia on routine biochemicaltesting or in the evaluation of postmenopausal
women with osteoporosis is typically the initial clue to the diagnosis of primary hyperparathyroidism.
The total serum calcium level,which combines both the free and albumin-bound components of circulating calcium, should be adjusted for the level of albumin as follows: corrected or adjusted total calcium = (measured total
calcium in mg per deciliter) + [0.8 × (4.0 − patient’s
serum albumin concentration in g per deciliter)].
Measurement of ionized calcium may be useful
in selected cases, such as in patients with• hyperalbuminemia,
• thrombocytosis,
• Waldenström’s macroglobulinemia, and
• myeloma; these patients
may have elevated levels of total serum calcium,
but normal levels of ionized serum calcium
(artifactual hypercalcemia).
Measurement of serum PTH is the next step in the evaluation of hypercalcemia. An elevated level
of PTH (or a level that is in an unexpected “normal” range) simultaneous with an elevated calcium level generally indicates a diagnosis of primary hyperparathyroidism. However, these laboratory findings may also occur with lithium or thiazide use, tertiary hyperparathyroidism associated with end-stage renal failure, and familial hypocalciuric hypercalcemia, and a medical and family history should be obtained to assess these possibilities.
The finding of a normal level of albumin-adjusted or ionized serum calcium and an elevated level of PTH in patients with no other causes of secondary hyperparathyroidism is consistent with normocalcemic primary hyperparathyroidism.
A low or undetectable PTH level rules out primary hyperparathyroidism and raises the possibility of cancer-associated hypercalcemia, often mediated by PTH-related protein,which does not cross-react with the PTH assay.
If the PTH level is elevated in a person with aknown malignant condition, the most likely diagnosis is concomitant primary hyperparathyroidism; ectopic production of PTH from a tumor is extremely rare.
Once the diagnosis of primary hyperparathyroidism
has been established, a familial form,accounting for about 5% of cases, should be considered. Young age (<30 years) at diagnosis;a family history of hypercalcemia, neuroendocrine tumors, or both; the presence of skin lesions associated with multiple endocrine neoplasia syndromes (Table 1); or the presence of all these factors increases the likelihood of familial primary hyperparathyroidism; in such cases, thelevel of serum calcium should be measured in
all first-degree relatives.
A palpable neck mass (which is not expected in primary hyperparathyroidism),markedly elevated levels of serum
calcium (>14 mg per deciliter [3.5 mmol perliter]) and PTH (3 to 10 times the upper limit of normal), or both, especially in men, suggest the possibility of parathyroid carcinoma, although this is rare (<1% of cases of primary hyperparathyroidism).
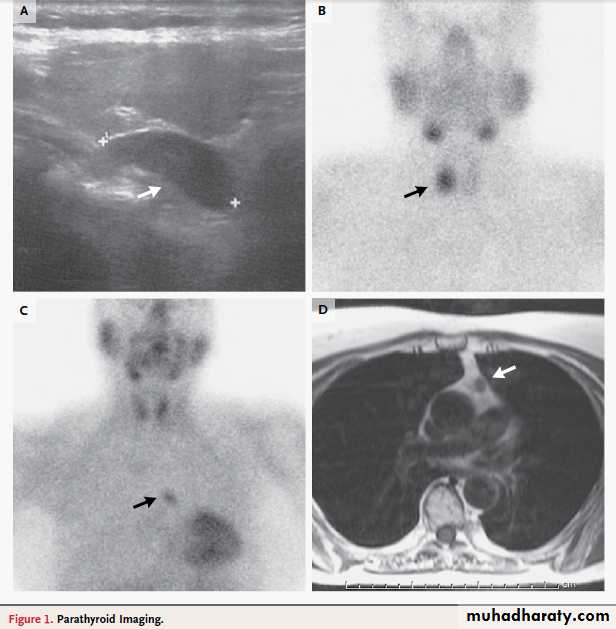
Panel A shows a longitudinal ultrasonographic image of the right thyroid lobe of the patient described in the vignette.
An enlarged parathyroid gland appears homogeneously solid and markedly more hypoechoic than the adjacent thyroid
tissue (arrow). Panel B shows a delayed-phase planar sestamibi scan indicating a marked uptake at the level of the right thyroid lobe, where the ultrasound localized the parathyroid lesion (arrow) in the patient described in the vignette. Panels C and D show a mediastinal parathyroid adenoma in a 65-year-old woman with primary hyperparathyroidism.
In Panel C, a delayed-phase sestamibi scan shows a marked uptake at the level of the middle mediastinum
(arrow). In Panel D, a magnetic resonance imaging scan (T1-weighted image) of the chest shows a lesion in the aortopulmonary window (arrow). The patient underwent a sternotomy, and a parathyroid adenoma was excised.
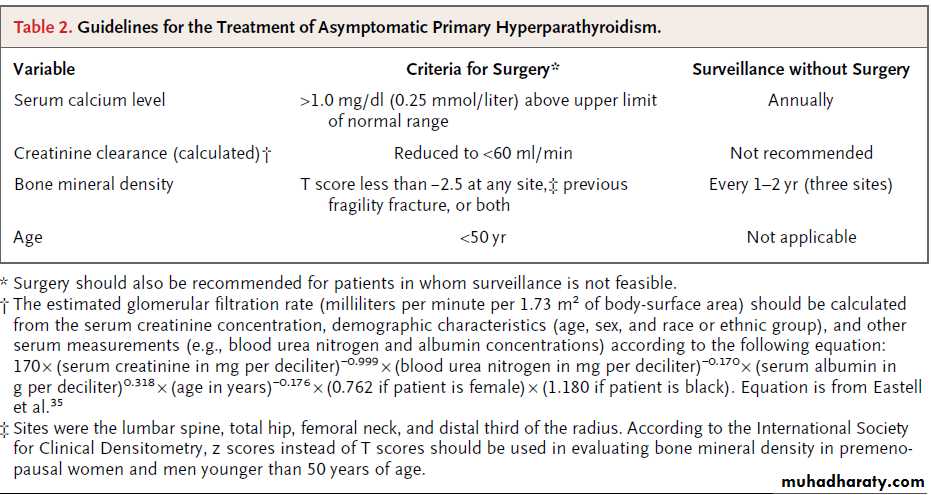
Laboratory testing should include assessment of renal function (Table 2)35 and the level of serum
25-hydroxyvitamin D. Levels of 25-hydroxyvitamin
D below 50 nmol per liter (20 ng per milliliter) are
common, probably because of its increased conversion
to 1,25-dihydroxyvitamin D and accelerated
catabolism in patients with primary hyperparathyroidism,
and this may further aggravate the disease by increasing PTH secretion.
The 24-hour urinary calcium and creatinine level should be measured to rule out familial hypocalciuric hypercalcemia;a calcium:creatinine clearance ratio
below 0.01 suggests this diagnosis, and hypercalcemia
in one or more first-degree relatives also supports it. Sequencing the calcium-sensing receptor gene, which is mutated in familial hypocalciuric hypercalcemia, may be helpful when family screening is inconclusive.
In selected cases (e.g., in young patients with a family history of a syndrome-associated tumor), genetic
testing may be warranted to determine the cause
of primary hyperparathyroidism and the risk of
other tumors.
Renal ultrasonography is recommended if the
history suggests nephrolithiasis, but it may also
be considered in the absence of such a history to
rule out kidney stones or nephrocalcinosis ,the presence of which would alter management recommendations.
Renal ultrasonographic evaluations have shown nephrolithiasis in 7% of patients with asymptomatic primary hyperparathyroidism.38 Bone mineral density
should be measured at the lumbar spine, hip, and
distal third of the forearm. PTH has a catabolic
effect on cortical bone, and sites enriched in
cortical bone are preferentially reduced.
Indeed, most patients have a reduction of bone mineral density at the distal third of the forearm and
relative preservation at the lumbar spine, with
intermediate values at the hip; a small subgroup
(15%) of patients may have vertebral osteopenia
or osteoporosis.39 Plain-film radiography of the
skeleton is not recommended, except in rare cases
of severe disease in which osteitis fibrosa cystica
is suspected.
Neck imaging is not indicated for diagnosis,
but it is useful for disease localization beforeplanned parathyroidectomy (Fig. 1). Sestamibi
scanning and ultrasonography are used most
commonly.
The main advantage of sestamibi scanning is that it may localize ectopic parathyroid.
Treatment
Parathyroid Surgery
When intervention is indicated, the goal of treatment
is to cure the disease by removing the abnormal
parathyroid tissue. Parathyroidectomy should be recommended in all patients with symptomatic primary hyperparathyroidism. Patients presenting with relatively mild hypercalcemia (serum calcium level <12 mg per deciliter [3 mmol per liter]) (the majority of patients with primary hyperparathyroidism) can proceed directly to surgery.
In the rare patients with higher calcium levels, preoperative treatment is required with saline infusion, followed by loop diuretics,and intravenous bisphosphonates or calcimimetics (cinacalcet)to reduce the serum calcium level and minimize the risk of complications associated with more severe hypercalcemia. These complications include hypovolemia, acid−base abnormalities, and cardiac-rhythm disturbances.
Parathyroidectomy should also be considered
for some patients with asymptomatic primaryhyperparathyroidism. According to the Third International Workshop on the Management of
Asymptomatic Primary Hyperparathyroidism, surgery
is recommended for patients meeting any
of the criteria for surgery listed in Table 2, as
well as those for whom surveillance is not feasible.
However, these are guidelines, not rules,
and decisions should take into account patient
preferences, the presence of coexisting conditions,
and the expertise of available surgeons.
In experienced hands, parathyroidectomy is
associated with a cure rate of 95 to 98% and alow rate (1 to 3%) of complications (laryngeal nerve
palsy and, less frequently, postoperative
hypocalcemia).
As compared with open procedures, minimally invasive approaches are associated with a shorter operating time, a more rapid postoperative recovery, and lower complication rates.
Minimally invasive surgery is increasingly used, although it is generally not performed in patients with a large goiter or previous neck surgery.
Intraoperative PTH monitoring may be helpful; a decrease of 50% or more in the PTH level 10 minutes after adenoma resection, as compared with the highest value before excision,suggests that all hyperfunctioning parathyroid
tissue has been removed.
Histologic analysis usually shows a single, benign, chief-cell adenoma.
When histologic findings are equivocal,molecular studies may help to identify parathyroidcancer.34 Recurrence is rare in sporadic primary
hyperparathyroidism, but the risk is higher
in familial cases, unless total parathyroidectomy
is performed.
Successful surgery is followed by aprompt normalization of the PTH level and serum
and urinary calcium levels and gradual increases in bone mineral density (up to 10%),mostly during the first few postoperative years
at the lumbar spine and hip, and later at the
distal radius.
Recurrence of nephrolithiasis is rare. Hypertension generally persists after successful
parathyroidectomy. Randomized trials showing short-term outcomes (1 to 3 years) suggest that surgery, as compared with surveillance, also may be of benefit for bone mineral density and quality of life in patients who do not meet the criteria for surgerySurveillance
For patients who do not undergo parathyroidectomy,annual monitoring of serum calcium and
creatinine levels and assessment of bone mineral
density every 1 or 2 years is recommended
(Table 2),40 although data are lacking to inform appropriate. testing strategies and frequencies of follow-up.Maintenance of adequate levels of 25-hydroxyvitamin
D (>50 nmol per liter [20 ng per milliliter])
and an adequate dietary calcium intake are recommended,since low vitamin D levels and low
calcium intake may exacerbate parathyroid overactivity.
Medical Therapy
At present, there is no definitive medical therapy
for primary hyperparathyroidism. However, treatment
options are available and should be considered
in patients who are not eligible for or are unwilling to undergo parathyroidectomy but in whom there is an indication to reduce the level of serum calcium, increase the bone mineral density,or both.
Placebo-controlled trials have shown improvement
in bone mineral density in postmenopausal women with primary hyperparathyroidism and mild hypercalcemia who are treated with antiresorptive therapy. In one trial, estrogen therapy (conjugated estrogen at a dose of 0.625 mg plus medroxypro-gesterone at a dose of 5 mg daily for 2 years) increased bone mineral density at the femoral neck and lumbar spine; however,long-term estrogen use is no longer recommended,given the associated cardiovascular and breast-cancer risks.In another study involving patients with mild disease, the bisphosphonate alendronate (at a dose of 10 mg daily for 2 years) reduced bone-turnover markers and increased bone mineral density at the lumbar spine and
hip, but not at the distal radius; levels of serum
calcium and PTH did not change significantly.
No long-term data on the efficacy and safety of
antiresorptive therapy in primary hyperparathyroidism
are available.
For patients in whom bone mineral density is not low, but in whom the serum calcium level is more than 1 mg per deciliter above the normal range, cinacalcet may be considered. Cinacalcet is approved in Europe and the United States for the treatment of moderate-to-severe hypercalcemia in patients with primary hyperparathyroidism who are unable to undergo parathyroidectomy.
It has been shown to decrease serum calcium levels across a broad range of severity in primary hyperparathyroidism. In clinical studies, normocalcemia was achieved in 70 to 100% of patients with asymptomatic primary
hyperparathyroidism and in 28 to 68% of
those with more severe disease.
However, PTH levels decreased only modestly and generally remained elevated. In an uncontrolled study involving treatment for up to 5.5 years, bone mineral
density did not change significantly at any site.48
Cinacalcet is generally initiated at a dose of 30 mg
once or twice daily, and the dose is adjusted according to the serum calcium level, with median
doses of 60 mg daily in patients with asymptomatic
primary hyperparathyroidism48,49 and 120 mg
daily in patients with more severe primary hyperparathyroidism.
Once normocalcemia is achieved or the maximum tolerated dose is reached, the serum calcium level should be monitored every 2 to 3 months. Adverse events are generally mild or moderate. The most common events are headache and gastrointestinal symptoms; the rare event of hypocalcemia is managed by withdrawing medication for a few days and restarting at a lower dose.
Areas of Uncertainty
Long-term data from randomized trials are lackingto compare outcomes of parathyroidectomy
with conservative (nonsurgical) management in
patients with asymptomatic primary hyperparathyroidism.
The frequency and clinical significance of subtle cardiovascular and neurocognitive abnormalities in patients with otherwise asymptomatic primary hyperparathyroidism and the effects of parathyroidectomy on these manifestations
warrant further study.
Longitudinal data are needed to better define
the incidence of fractures in primary hyperparathyroidism before and after successful parathyroidectomy, to inform the natural history of normocalcemic primary hyperparathyroidism, and to assess the safety of the prolonged use of cinacalcet.It is uncertain whether a T score of −2.5 is the appropriate bone-mineral-density criterion for surgery in primary hyperparathyroidism. Moreover, the appropriate level of 25-hydroxyvitamin
D in patients with primary hyperparathyroidism
followed without parathyroidectomy and the effects of vitamin D supplementation on disease progression remain uncertain.
Guidelines
There are no formal guidelines from professionalsocieties for the management of primary hyperparathyroidism.
Updated international guidelines for the management of asymptomatic primary
hyperparathyroidism were published in
2009.40 The recommendations in this article are
generally concordant with these guidelines.
Conclusions and
RecommendationsThe woman described in the vignette has asymptomatic
primary hyperparathyroidism associated
with a bone mineral density T score of less than −2.5 at the distal third of the radius. Further evaluation should include assessment of the level of 25-hydroxyvitamin D and creatinine clearance.
The ratio of urinary calcium to creatinine clearance
is not in the range suggestive of familial
hypocalciuric hypercalcemia (<0.01), and the family history does not suggest a familial form of primary hyperparathyroidism.
Given the patient’s bone mineral density T score, we would recommend parathyroidectomy, performed by
means of a minimally invasive approach if available,
if preoperative imaging studies localize the abnormal parathyroid gland or glands. If the patient declines surgery, we would advise adequate calcium intake (as for patients without primary hyperparathyroidism)40 and vitamin D supplementation if serum levels of 25-hydroxyvitamin D are less than 20 ng per milliliter.
To assess disease stability, serum calcium and creatinine levels should be followed yearly, and bone mineral density should be tested every 18 to 24 months, and we would strongly recommend
parathyroidectomy if evidence of disease progression is detected.