GIT
د. حسين محمد جمعة
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
Daily Bisacodyl Effective for Chronic Constipation
The over-the-counter laxative bisacodyl has been available for decades. Intestinal enzymes convert this agent into an active metabolite, bis-(p-hydroxyphenyl)-pyridyl-2-methane (BHPM). BHPM stimulates fluid secretion and also has a direct prokinetic effect. Gastroenterologists often recommend bisacodyl — but primarily for short-term use, out of concern that patients will develop tolerance and then require either higher doses or a different laxative. Whether it should be used in chronic constipation remains uncertain: Few data are available from controlled trials.Investigators recently addressed this issue in a manufacturer-sponsored, multicenter, double-blind trial conducted in the U.K. among adults who fulfilled Rome III criteria for chronic constipation. During a 2-week baseline period, all had fewer than three complete spontaneous bowel movements (CSBMs) per week on average and at least one additional symptom — straining, incomplete evacuation, or lumpy or hard stools — more than 25% of the time. A total of 368 participants (75% women; mean age, 55) were randomized in a 2:1 ratio to receive oral bisacodyl (10 mg daily) or placebo for 4 weeks.
Comment: These findings suggest that bisacodyl at 10 mg daily is an effective treatment for patients with chronic constipation. Clearly, some of the patients could have been managed adequately with a lower dose. Although this 4-week study provides valuable information, chronic constipation is a problem that can require years of treatment. It will be important to know whether tolerance develops with more-prolonged therapy and whether intermittent treatment might produce a more-sustained and better-tolerated effect for some patients.
Journal Watch Gastroenterology August 5, 2011
A tissue transglutaminase IgA and/or IgG test is used as part of an evaluation for certain autoimmune conditions, most notably celiac disease. in the case of people with celiac disease, gluten, a protein found in wheat, barley, rye, and oats — as a foreign invader and attacks it. This immune system response in celiac disease also involves the production of antibodies directed against an enzyme normally present in the intestines called tissue transglutaminase (tTG).
In celiac disease, the body produces two types of antibodies that attack tTG: immunoglobulin A (IgA) and immunoglobulin G (IgG). Measuring the IgA form of tTG antibody in the blood is more useful in detecting celiac disease because it's made in the small intestine, where gluten causes inflammation and irritation in sensitive people.
Levels of the IgG form of tTG antibody, on the other hand, are less specific to celiac disease, but may still be useful in diagnosing the condition in people who are unable to make normal amounts of IgA antibodies.
Preparation
For accurate results, your child must currently be eating a diet that includes gluten-containing foods, such as breads, pastas, and baked goods. The body will only produce antibodies when it's exposed to gluten. If gluten has been removed from the diet, there won't be an antibody response to measure.Travellers’ diarrhoea
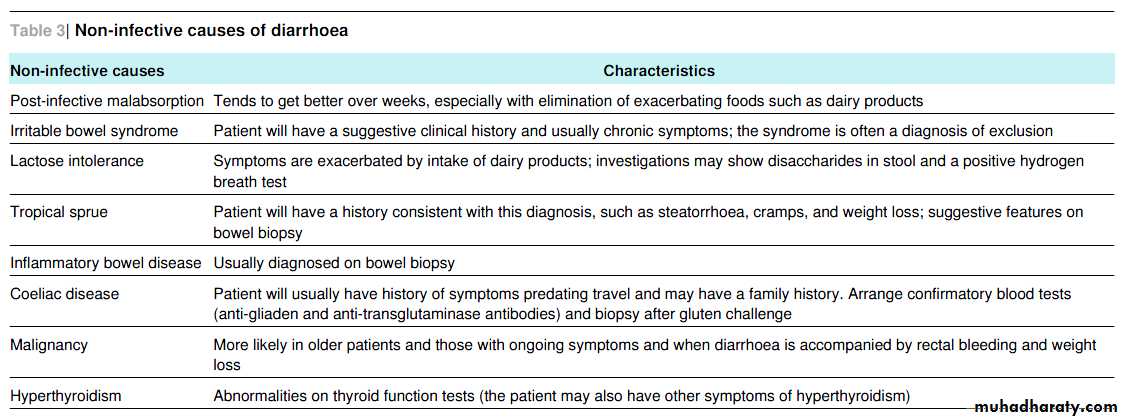
The causes of diarrhoea in travellers can be both infective and non-infective. The duration of symptoms is an important factor in thinking about the likely cause.About 50-75% of acute cases of travellers’ diarrhoea (duration less than two weeks) are caused by bacteria. The most common bacterial cause is enterotoxic Escherichia coli.
BMJ 2011;342:
Other common bacterial causes include
campylobacter, salmonella, and shigella. Viruses, most commonly rotaviruses and noroviruses, account for 10-20% of cases, and parasitic agents such a giardia, cryptosporidium, and cyclospora account for up to 5% of cases.Vibrio cholerae is an uncommon cause of acute travellers’ diarrhoea but is worth considering if the patient has travelled in the area of an outbreak.
When diarrhoea has been present for more than two weeks, the spectrum of possible causes is wider and non infective causes become increasingly important. Taking a good travel and clinical
history is paramount. Features of the stool may be of help. Blood and mucus is characteristic of dysentery, which can be caused by a range of pathogens including shigella and amoeba. Bulky stools suggest giardia or malabsorption. However, stool
microscopy and culture is the key investigation.
Learning points
The likely cause of travellers’ diarrhoea depends on the duration of symptoms .Bacteria, in particular enterotoxic Escherichia coli, are the most common pathogens found in travellers with acute symptoms (less than two weeks’ duration)
Stool microscopy for ova, cysts, and parasites and culture (ideally three specimens) form the key investigation in apatient who has just returned from travelling and has diarrhoea, although a causative agent is often not found.If symptoms persist, investigate for less common pathogens, such as parasites, and for non-infective causes.
BMJ 2011;342:
Nasogastric feeding tubes are commonly used for people such as stroke patients with dysphagia or those on ventilators. They are generally used in the short to medium term (up to six weeks), rather than for longer term feeding, which occurs via gastrostomy tubes, jejunostomies, or gastrostomy buttons.Checking placement of nasogastric feeding tubes in
adults (interpretation of x ray images): summary of a
safety report from the National Patient Safety Agency
BMJ 2011;342:
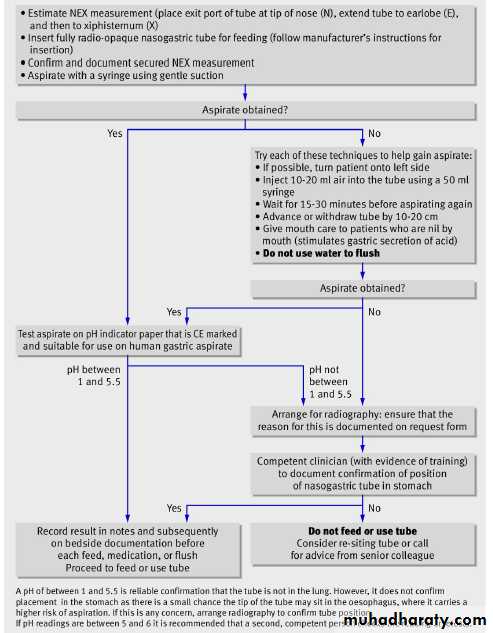
Most are inserted safely, but patients can be harmed if the tube is mistakenly inserted into the lungs or later becomes displaced from the stomach. If such errors are not detected before feeding, patients can develop serious complications, such as intrapulmonary feeding and aspiration pneumonia, which can be fatal. The position of tubes should therefore always be checked before feeding is started.
The National Patient Safety Agency (NPSA) issued guidance in 2005 for safe placement and position checking of nasogastric tubes. The guidance highlighted the unreliability of certain
tests—such as the “whoosh” test (listening for bubbling sounds after air entry) and testing for acidity with litmus paper—and instead recommended testing with pH indicator paper as the first line check.
It recommended checking x ray images as the
second line test, although not for routine use. Since 2005, staff in England and Wales have reported 21 deaths and 79 cases of harm resulting from feeding into the lungs through misplaced nasogastric tubes. The single greatest cause of harm resulted from misinterpretation of x ray images, which accounted for 45 serious incidents, including 12 deaths.The NPSA therefore issued a further safety alert in March 2011 focusing on safe interpretation of x ray images. The guidance covers adults and
children (not neonates), but this short article, based on the March
safety alert, summarises advice for adults only.
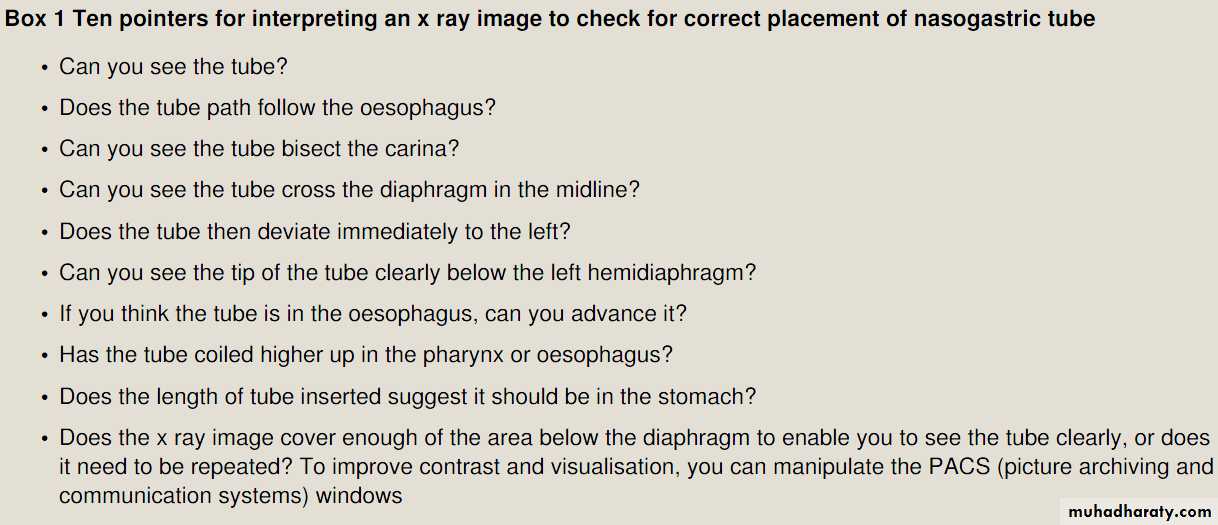
Individual clinicians should ask themselves:
Is nasogastric feeding appropriate for this patient? Do not use this method of feeding if the patient has a high risk of aspiration or any deviation in normal anatomy, such as pharyngeal pouch, strictures, or facial trauma. In these cases, seek advice as fluoroscopic guidance can often beused.
Because of the risks of intubation, the decision to feed after assessment of the patient must be agreed by two competent professionals and recorded.
Does this need to be done now? Risks are greater at night time, when there is reduced access to a full range of staff and equipment.
Am I competent to do this?
Ensure you have had training in safe insertion and checking, including interpretation of x ray images, and that you are supervised until competent. If you do not feel confident to do this procedure, ask for help.
How can I check that the correct amount of tube has been inserted? Use NEX measurement (place exit port of the tube at the tip of the nose (N), stretching it to the earlobe (E) and then down to xiphisternum (X)) and confirm and record the external tube length before each feed to check
that it has not moved.
Do I know how to test for correct placement (figure)? Do not flush tubes or insert any liquid until you can confirm by testing with pH indicator paper (first line) or correct placement by radiography (second line).
What is a safe pH level? Obtain a nasogastric aspirate: if the pH level is between 1 and 5.5, it is safe to start feeding.To be sure, check with a competent colleague if the reading falls between 5 and 6, because of possible misinterpretations at this level. Always record the result and the decision to start feeding.
When should I arrange radiography? If no aspirate can be
obtained or the pH level is higher than 5.5, requestradiography and specify the purpose on the request form
so that the radiographer knows that the tip of the
nasogastric tube should be visible (that is, the film will be
centred lower than for normal chest radiography).
What should I look for in the x ray image? You need to
check that the tube is in the stomach (see box 1 and
guidance from the NPSA4). Ask a radiologist if you are
unsure about this.
After radiography, have I clearly recorded my decisions and next steps for the patient (box 2)? If the tip of the tubeis well into the stomach (see NPSA guidance4), it is safeto feed. If the tube looks misplaced or the position is not clear, it is not safe to feed. If there is any chance that the tube is in the respiratory tract, take it out.
You cannot rely on absence of respiratory distress as a sign of correct tube placement.
What about repeat checks? As tubes can be dislodged, tube
placements should be checked at least once daily and beforeadministering each feed or medication. Note that some
patients, such as those taking proton pump inhibitors, will
have persistently high gastric pH and so daily radiography
would be impractical. Provided that the initial placement
was appropriately confirmed and no other signs of
dislodgement (such as retching or coughing) are present,
repeat radiography would not usually be needed as long as
the external length of tube remains unchanged. For further
details see the NPSA’s supporting information4 and the
2003 guidelines commissioned by the British Society of
Gastroenterology
Sorbitol, or glucitol as it is sometimes called, is a slow-metabolizing sugar alcohol derived from fruits, corn and seaweed. It's a sugar substitute found in foods such as frozen desserts, sugar-free chewing gum and dietetic candies. Sorbitol is also used as a thickener and moisturizer in beauty products.
Sorbitol is only about 60% as sweet as sugar. Since it's very slow to be metabolized by the body, sorbitol does not cause insulin levels to increase as much as sugar. Sorbitol also doesn't lead to tooth decay and is used in many sugar-free cough syrups. It is a popular addition to gel toothpastes as it helps add transparency.
What is Sorbitol,
Sorbitol is added to soaps, especially transparent glycerin bar soaps. It has moisturizing qualities and may be found in lotions and moisturizing soaps. Sorbitol has been used in cosmetic products for close to a century and is a Generally Recognized as Safe (GRAS) product by the United States Food and Drug Administration (FDA).
Sorbitol can have a laxative effect and is not recommended for consumption by children and those with sensitive digestion symptoms or a gastro-intestinal condition such as Irritable Bowel Syndrome (IBS). Sorbitol can cause diarrhea, bloating and gas unless it's consumed in small quantities. It may also cause abdominal pain in some cases.
Sorbitol's chemical formula is C6H1406. It may be used in cigarette production as a moisturizing substance as well as a sweetener in some diet drinks. Sorbitol is also used, along with sucrose, to preserve the freshness of surimi proteins used in producing imitation crab.
Sorbitol used in the food and cosmetics industry today comes mostly from corn. The People's Republic of China is a large producer of sorbitol. Different grades of sorbitol include food grade for food and beverage products, cosmetic grade for cosmetic and personal health products and Vitamin C grade used to produce Vitamin C tablets.
Sorbitol is a sugar alcohol (C6H1406), which is otherwise known as glucitol. In its natural form, it is found in certain fruits, corn, seaweed, prunes, plums, apricots, etc. It is a white odorless powder that is sweet in taste. Sorbitol is found to be around 60% as sweet as sugar. As it is very low in calories, when compared to sugar, sorbitol is used as a sugar substitute in a wide range of products, including diabetic products to diet drinks, sugar free candies, gums, chocolates, etc. Studies show that sorbitol is metabolized by the human body in a very slow manner and this reduces the chances of increased insulin levels, as in case of sugar consumption.
Sorbitol is also said to have laxative properties, as it draws water into the colon, thereby stimulating bowel movements. Do you have any idea about what is sorbitol solution? It is nothing other than the sorbitol medical preparation that is available in drug stores as a laxative and is used to treat constipation. This compound is also said to have moisturizing properties and so is used in various cosmetics too. It is also used as a thickener in some cosmetics. In gel toothpastes, sorbitol is used for enhancing the transparency. It is also used in some types of cigarettes.
Apart from being a sweetener, sorbitol provides energy too. Today, most of the sorbitol used in food and cosmetic industry is derived from corn. It can also be made synthetically. Now, you know more about what is sorbitol and what is sorbitol used for.
Even though sorbitol is said to be safe, excess consumption of food products with sorbitol may sometimes lead to abdominal pain, cramping, bloating, severe diarrhea, etc. In some rare cases, black and tarry stools may occur as a side effect of sorbitol. In such cases, you must consult your doctor immediately. It has been reported that regular use of sugar-free gum with sorbitol (around 20 grams per day) leads to weight loss too. Use of sorbitol solution is sometimes said to cause anal irritation, dizziness, irritability and rectal bleeding (uncommon).
Sorbitol Dangers
In some rare cases, consumption of sorbitol is said to hinder absorption of vitamin B12 in the intestine and also cause electrolyte imbalances. Sorbitol side effects include excess thirst, dry mouth, edema, dehydration, trouble breathing, seizures, etc. It is said that some people develop allergic reactions to sorbitol. Even occurrence of chest pain and certain cardiac and pulmonary disorders are included as sorbitol dangers.
In short, sorbitol is used in a wide range of food products, cosmetics, medical preparations, etc. As far as consumption of sorbitol is concerned, moderate use is always recommended, so as to avoid the possible side effects. It is better for kids to avoid products with sorbitol. Even those with certain medical conditions of the gastrointestinal tract like irritable bowel syndrome, must avoid use of sorbitol. In people with certain gastrointestinal problems, use of a small amount of sorbitol may be enough to cause pain and bloating.
It is said that sorbitol, being non-digestible, accumulates in the bowel, thereby casing side effects. Even sorbitol intolerance is said to develop in some people. Sorbitol is usually not recommended for pregnant and nursing women. Medical use of this compound must be according to your doctor’s instructions only. If you experience any side effects or allergic reactions after using sorbitol, contact your doctor immediately. Now that you know what is sorbitol, you may control the use of sorbitol products.
The size of gastroesophageal varices is one of the most important factors leading to hemorrhage related to portal hypertension. An endoscopic evaluation of the size of gastroesophageal varices before and after different operations for portal hypertension was performed in 73 patients with schistosomiasis, as part of a randomized trial: proximal splenorenal shunt (PSS n=24), distal splenorenal shunt (DSS n=24), and esophagogastric devascularization with splenectomy (EGDS n=25). The endoscopic evaluation was performed before and up to 10 years after the operations.
Variceal size was graded according to Palmer's classification: grade 1 up to 3 mm, grade 2 from 3 to 6 mm, grade 3 greater than 6 mm, and were analyzed in four anatomical locations: inferior, middle or superior third of the esophagus, and proximal stomach. The total number of points in the pre-operative grading minus the number of points in the post-operative grading gave a differential grading, allowing statistical comparison among the surgical groups.
Good results, in terms of disappearance or decrease of variceal size, were observed more frequently after PSS than after DSS or EGDS — 95.8%, 83.3%, and 72%, respectively. When differential grading was analyzed, a statistically significant difference was observed between PSS and EGDS, but not between proximal and distal splenorenal shunts. In conclusion, shunt surgeries were more efficient than devascularization in diminishing variceal size.
Classification of esophageal varices
GradeEndoscopic appearance
I.
Dilated venes (< 5mm) still at the level of the surrounding tissue
II.
Dilated, straight venes (> 5 mm) protruding into the esophageal lumen but not obstructing it
III.
Large, tense and winding venes already obstructing the esophageal lumen considerably
IV.
near complete obstruction of the esophageal lumen with impending danger of hemorrhage (cherry red spots)
Ursodiol
Ursodiol is one of the naturally occurring bile salts. Bile salts are made in the liver and flow down the bile ducts to the intestine where they are needed to help digest the fats in the food we eat. There are a number of bile salts, some of which are toxic when retained in the liver. Ursodiol has low liver toxicity. When taken as a medication, it replaces some of the more toxic liver bile salts. Therefore, if bile is retained in the liver for some reason, there is less liver damage.The two main types of liver damage caused by bile salts being retained in the liver are
primary biliary cirrhosis and
primary sclerosing cholangitis.
Ursodiol is approved by the FDA for the following:
• Dissolving cholesterol gallstones• Preventing gallstone formation during rapid weight loss
• Treatment of primary biliary cirrhosis
It is also used by physicians in the treatment of primary sclerosing cholangitis and other chronic disorders of the liver.
Since one of the side effects is diarrhea, it occasionally is even used to treat difficult constipation.
Interaction with this drug may occur with the following:
• antacids that contain aluminum (Alucaps, Rolaids)• cholesterol lowering medications (Lopid, Mevacor, Questran)
• estrogens (Premarin)
• birth control pills
Ursodiol is ranked B. Always consult your physician before taking any drug during or when planning pregnancy. The safety of using ursodiol beyond 24 months is not established. However, since it is a naturally occurring bile salt, it is likely safe to use it long-term. It is gastroenterologists' experience that patients can safely stay on this drug for long periods.
Minor:
diarrheanausea
vomiting
gas
metallic taste
constipation
rash
headache
muscle aches
How about side effects?
Major:
severe itching
severe muscle or joint pain
persistent cough
Gastroenterologists have been using ursodiol for years to treat primary biliary cirrhosis and primary sclerosing cholangitis because the drug lowers the abnormally elevated blood liver enzymes. It is assumed that this, in turn, results in less liver damage. Since the drug has a very good safety profile, physicians have been comfortable using it long-term. Data is coming into the medical literature that, indeed, there is significant benefit. People with these liver problems do seem to live longer and do not come to a liver transplant as soon as those who do not use it.
Dissolving gallstones is almost never done anymore because laparoscopic gallbladder removal has become so easy. Dissolving gallstones takes a long time and, in many people, they may return when the drug is stopped. Still, for some who just don't want surgery or where surgery is considered too dangerous, it can be used.
Lactose Intolerance Management Guidelines
Many lactose-intolerant individuals can tolerate up to 24 g lactose daily (the amount in 2 cups of milk) if it is ingested throughout the day, according to a National Institutes of Health (NIH) Consensus Development Conference Statement on Lactose Intolerance and Health.Chronic Constipation: A Possible New Therapeutic Agent
lubiprostone, a chloride channel activator, was recently shown to be effective in the treatment of chronic constipation. Nevertheless, a large proportion of patients do not experience complete relief with this drug or other currently available approaches.AccessMedicine from McGraw-Hill © 2010 03/24/2010
Linaclotide, a new agent, is a minimally absorbed, 14-amino-acid peptide that increases intestinal fluid secretion and transit via the intestinal guanylate cyclase C (GCC) receptor. Activation of this receptor results in increased fluid secretion as well as an increase in transit. In addition, animal studies show that the drug leads to decreased sensitivity to visceral distention.
Recently, Lembo and colleagues (2010) reported the results of a placebo-controlled study evaluating the efficacy of a 4-week treatment with linaclotide in chronic constipation. In this multicenter study, patients were randomized to treatment with placebo or drug at various doses once daily. Patients with irritable bowel syndrome criteria were excluded. The primary endpoint was a change in the mean weekly spontaneous bowel movement frequency. Additional endpoints included improved stool consistency, abdominal discomfort and bloating, and overall evaluation of the relief of constipation.
In a dose-dependent manner, linaclotide significantly increased the frequency of spontaneous bowel movements as well as all the other endpoints that were the objective of the study. Overall, relief of constipation was consistently higher with linaclotide than with placebo. The drug was well tolerated; not surprisingly, the most commonly reported adverse event was diarrhea, which was usually transient and mild.
Linaclotide significantly improves bowel habits and abdominal symptoms in patients with chronic constipation. The drug has a rapid onset of action, and doses of 150 or 300 mg seem to provide the best relief. In an accompanying editorial, Drs. Bharucha and Waldman noted that “linaclotide and other GCC targeted agents expand the spectrum of molecularly based therapeutic options available to treat chronic constipation disorders.”
AccessMedicine from McGraw-Hill © 2010 03/24/2010
Common Tongue Conditions in Primary Care Reviewed
The most frequently encountered tongue problems are geographic tongue; fissured tongue; and hairy tongue, which is caused by hypertrophy of the filiform papillae resulting in white, tan, or black tongue discoloration. These conditions do not require treatment. Fissured tongue is associated with deep grooves and may give rise to bad odor and discoloration if the grooves become inflamed or if food gets trapped.03/16/2010 MedscapeCME
Geographic tongue, which may occur with fissured tongue, is characterized by bare patches on the dorsal aspect of the tongue surrounded by a serpiginous, raised, slightly discolored border. When geographic tongue gives rise to tongue sensitivity, topical steroid gels or antihistamine rinses can be helpful.
Median rhomboid glossitis is characterized by a smooth, shiny, erythematous, and sharply circumscribed plaque- like lesion on the dorsal midline of the tongue. It is usually asymptomatic but may cause tongue burning or itching. This condition usually reflects an underlying candidal infection and responds to topical therapy with antifungal agents such as nystatin, fluconazole, or clotrimazole, administered as a suspension or oral troche.
Nutritional deficiency of iron, folic acid, vitamin B12, riboflavin, or niacin may result in atrophic glossitis, also known as smooth tongue because of the smooth, glossy appearance with a red or pink background. This condition typically responds to correction of the underlying deficiency.
Patients with underlying immunodeficiency may have oral hairy leukoplakia, or white, hairy-appearing lesions on the lateral border of the tongue, caused by the Epstein-Barr virus. Recommended treatment is oral antiviral agents.
When a tongue growth is detected, biopsy is usually needed to distinguish benign conditions from premalignant leukoplakia or squamous cell carcinoma. In squamous cell carcinoma, there is typically a thickened white or red patch or plaque on the lateral part of the tongue, which may develop nodularity or ulceration. Tobacco use, alcohol use, and older age are risk factors for squamous cell carcinoma, which can be treated with surgical excision and radiation.
Geographic tongue appears as migratory smooth areas with raised serpiginous borders: It is associated with fissured tongue.It is usually asymptomatic.
Treatment is not required, but topical steroid gels and antihistamine mouth rinses can decrease sensitivity to hot or spicy foods.
Fissured tongue appears as deepening of normal fissures, which usually occurs with aging: Associations include Down's syndrome, acromegaly, psoriasis, Sjogren's syndrome.
Treatment is not required, but gentle brushing of the tongue can reduce symptomatic inflammation.
Hairy tongue appears as a white or tan-to-black color and hair-like elongated strands on the dorsal aspect of the tongue:
Associations include antibiotics, smoking, and poor oral hygiene.Hairy tongue is usually asymptomatic but can cause halitosis or abnormal taste.
Treatment is not required, but gentle brushing or scraping of the tongue can be useful.
Oral hairy leukoplakia appears as white, hair-like lesions on 1 or both lateral margins:Associations include immunosuppression and Epstein-Barr infection.Treatment is oral antiviral agents.
Lichen planus appears as a reticular, white, lacy pattern on the buccal mucosa of the tongue or as shallow ulcerations: Treatment is antifungal if candidal coinfection occurs, topical steroids for ulcerations, biopsy if unclear diagnosis, and no treatment if it is reticular.
Median rhomboid glossitis appears as a shiny, smooth, erythematous, sharply circumscribed, rhomboid-shaped plaque in the dorsal midline of the tongue:
It is often linked with candidal infection.
It is usually asymptomatic but can cause burning or itching.
Treatment is topical antifungal medications.
Atrophic glossitis appears smooth and glossy with a pink or red background:
Common causes are iron, folic acid, vitamin B12, riboflavin, and niacin deficiencies; underlying disease; or medications.
Treatment is directed at the underlying cause.
Linea alba appears as a thin white line on the buccal mucosa of the tongue or bilateral edges as a result of trauma from chewing:
Treatment is not required.
Tongue growths usually require biopsy or excision:
Granular cell tumors appear as small, smooth, solitary, firm, painless lesions.
Traumatic fibroma appears as a focal, thickened, dome-shaped, pink, smooth area along the bite line.
Leukoplakia is a white patch or plaque commonly linked with tobacco use.
Erythroplakia is a red patch or plaque.
Erythroleukoplakia is a speckled red-and-white lesion.
Squamous cell carcinoma appears as slight thickening over red or white base on the lateral surface that can become nodular or ulcerated.
Lingual thyroid nodule appears as smooth nodular lesion in the midline of the posterior dorsal surface, which can be linked with difficulty swallowing and hypothyroidism.
Lymphoepithelial cysts appear as yellow nodules on the ventral surface, tonsillar area, or floor of the mouth.
Squamous papilloma appears as single pedunculated lesion with finger-like projections.
Burning tongue symptoms are sudden sensation of scalded tongue with normal or denuded appearance:
Spontaneous resolution can occur after years.
Treatment of symptoms includes alpha-lipoic acid, clonazepam, and cognitive behavior therapy.
Ankyloglossia or short lingual frenulum in an infant with breast-feeding difficulty can be treated with frenulectomy.
Macroglossia can be linked with Down's syndrome, hypothyroidism, tuberculosis, sarcoidosis, amyloidosis, multiple myeloma, neurofibromatosis, infection, and angioedema or allergic reaction.
Tongue lesions of unknown cause can be evaluated by an oral and maxillofacial surgeon, head and neck surgeon, or dentist with oral pathology experience.
Management of tongue abnormalities includes antifungal medications for median rhomboid glossitis; topical steroids for ulcerative lichen planus; correction of nutritional deficiency for atrophic glossitis; antivirals for oral hairy leukoplakia; biopsy for tongue growths; and alpha lipoic acid, clonazepam, and cognitive behavior therapy for burning mouth syndrome.
03/16/2010 MedscapeCME
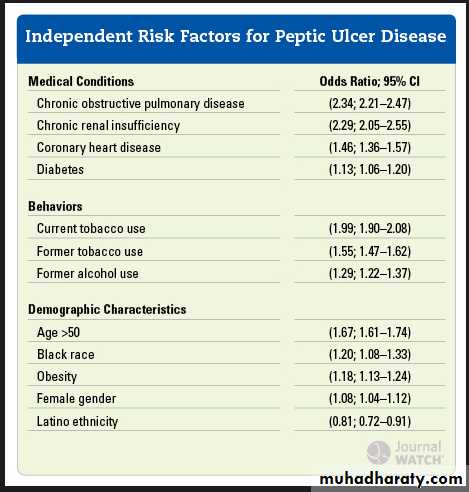
Diagnosis and Management of H pylori Infection
"Infection with H. pylori is a cofactor in the development of three important upper gastrointestinal diseases: duodenal or gastric ulcers (reported to develop in 1 to 10% of infected patients), gastric cancer (in 0.1 to 3%), and gastric mucosa-associated lymphoid-tissue (MALT) lymphoma (in <0.01%)," writes Kenneth E. L. McColl, MD, from the Division of Cardiovascular and Medical Sciences, University of Glasgow, Gardiner Institute, Glasgow, United Kingdom. "The risk of these disease outcomes in infected patients varies widely among populations.The great majority of patients with H. pylori infection will not have any clinically significant complications."
Routine testing for H pylori infection is not recommended because the vast majority of patients with this infection do not have any associated clinical disease.
Methods of Testing
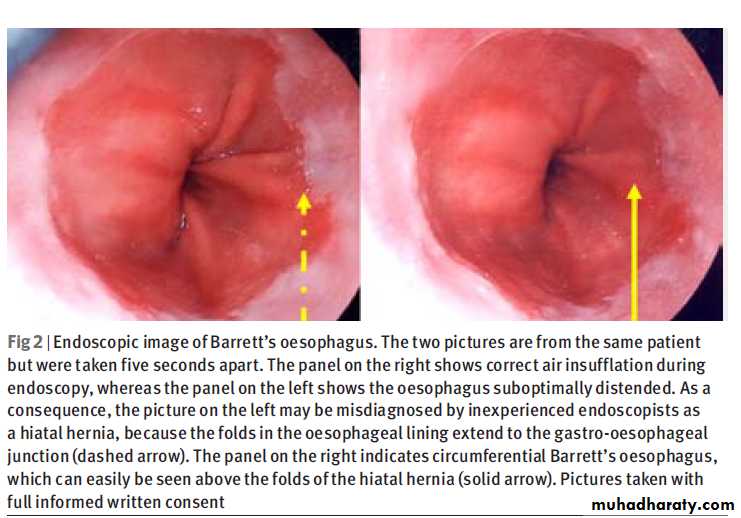
Routine testing for H pylori infection is not recommended because the vast majority of patients with this infection do not have any associated clinical disease. However, confirmed gastric or duodenal ulcers and gastric MALT lymphoma are definite indications for detecting and treating H pylori infection. After surgical removal of early gastric cancers, it may also be reasonable to test for and eradicate H pylori infection.For younger patients with upper gastrointestinal tract symptoms but without alarm symptoms such as weight loss, persistent vomiting, or gastrointestinal tract bleeding, it is reasonable to use a noninvasive test-and-treat strategy for H pylori infection. Options for noninvasive testing include the urea breath test, fecal antigen test, and serologic test. Of these options, the least accurate is the serologic test. Patients with positive test results should undergo eradication therapy.
For patients with alarm symptoms, or for older patients with new-onset dyspepsia, endoscopy is recommended. Depending on the specific set of guidelines used, older patients are defined as those 45 years or older or 55 years or older. Because nonsteroidal anti-inflammatory drugs can cause ulcers in the absence of H pylori infection, endoscopy is warranted for patients with dyspepsia associated with use of these drugs.
Treatments
Unless there is a high local rate of resistance to clarithromycin, appropriate first-line treatment is triple therapy using a proton-pump inhibitor plus clarithromycin and amoxicillin, each given twice per day for 7 to 14 days.Patients with a penicillin allergy should receive metronidazole instead of amoxicillin.
When the prevalence of clarithromycin-resistant H pylori infection exceeds 20%, an alternative initial treatment regimen is quadruple therapy with a proton-pump inhibitor, tetracycline, metronidazole, and a bismuth salt for 10 to 14 days. However, bismuth salts are not available in the United States and in some other countries.
Another option is 10-day sequential therapy with a proton-pump inhibitor plus amoxicillin for 5 days, followed by a proton-pump inhibitor plus clarithromycin and tinidazole for 5 more days. However, the efficacy of this regimen needs to be confirmed before it is widely used.
"Data are lacking to inform the optimal management of recurrent or persistent dyspepsia after noninvasive testing and treatment of H. pylori infection," Dr. McColl writes. "Options include symptomatic acid-inhibitory therapy, endoscopy to check for underlying ulcer or another cause of symptoms, and repeat of the H. pylori test-and-treat strategy; other potential reasons for the symptoms should also be reconsidered."
After Eradication Therapy: What Next?
When symptoms recur or persist after eradication therapy without first testing for H pylori, the most likely explanation is that the symptoms are unrelated to H pylori infection, rather than treatment failure. Unless persistent H pylori infection is confirmed, further eradication therapy should not be considered.Eradication of H pylori infection should be confirmed in patients who have had an H pylori–associated ulcer or gastric MALT lymphoma or who have undergone resection for early gastric cancer.
Tests for eradication may include a urea breath test or fecal antigen test performed at least 4 weeks after treatment is completed, so that false-negative results from suppression of H pylori are avoided. For patients requiring endoscopy, eradication can also be confirmed by testing during this procedure.
When treatment fails to eradicate H pylori infection, therapeutic options include empiric acid-inhibitory therapy, endoscopy to detect underlying ulcer or another cause of symptoms, and subsequent use of the noninvasive test-and-treat strategy. Clinicians should also consider another cause for the symptoms, such as biliary tract, pancreatic, musculoskeletal, or cardiac disease or psychosocial stress.
Poor compliance with initial treatment may also be implicated and mandates adherence to the second treatment regimen.
Treatment failure may be caused by H pylori resistance to clarithromycin or metronidazole, or both. Bismuth-based quadruple therapy is often used as second-line therapy if initial treatment did not include a bismuth salt. In patients previously treated with a proton-pump inhibitor, amoxicillin, and clarithromycin, a proton-pump inhibitor used in combination with metronidazole and either amoxicillin or tetracycline is recommended.
"Data from randomized trials are lacking to guide the care of patients whose symptoms persist after completion of H. pylori eradication therapy for uninvestigated dyspepsia," Dr. McColl concludes. "The effect of eradication of H. pylori infection on the risk of gastric cancer is unclear but is currently under study."
N Engl J Med. 2010;362
Approximately 50% of the human population has H pylori infection. It is a cofactor in the development of duodenal or gastric ulcers (1% - 10% of those infected), gastric cancer (0.1% - 3%), and gastric MALT lymphoma (< 0.01%). Eradication of H pylori provides a cure in 80% of those with duodenal ulcers attributed to the infection. The risk for gastric cancer is highest with inflammation of both antral and fundic mucosa, but it is unclear if eradication reduces the risk for gastric cancer.
H pylori infection is lower among patients with gastroesophageal reflux disease and esophageal adenocarcinoma because of associated atrophic gastritis, which reduces acid secretion.
Routine testing for H pylori infection is not indicated, but screening of those with a first-degree family history of gastric cancer or MALT lymphoma is recommended by European guidelines.
Those with uncomplicated dyspepsia without alarm signs should undergo testing by nonendoscopic method; eradication therapy is recommended for positive results.
In those with a positive result on an H pylori breath test, the number needed to treat for benefit at 1 year is 7.
However, the test-and-treat strategy is unlikely to be cost effective in populations with a prevalence of H pylori infection below 20%.
Among nonendoscopic tests, serologic testing for immunoglobulin G antibodies is least accurate, with a sensitivity of 85% and a specificity of 79%.
The urea breath test has a sensitivity and specificity of 95%.
Fecal antigen tests require fecal collection, which may be unpleasant to patients. Sensitivity and specificity are also 95%.
For both the breath test and the fecal antigen test, patients should stop taking proton-pump inhibitors 2 weeks before testing and avoid antimicrobial treatment for 4 weeks before testing because these medications may suppress infection.
Endoscopic tests include urea-based tests, which are inexpensive and accurate, but proton-pump inhibitors and antimicrobials should also be stopped before testing.
Clinical Implications
The urea breath test and the fecal antigen test have similar accuracy for the nonendoscopic diagnosis of H pylori infection.Triple therapy is the initial choice of treatment of H pylori infection followed by quadruple or sequential therapy.
McColl K. N Engl J Med 2010;362:1597-1604
Guidelines for Evaluation and Management of Helicobacter pylori InfectionDiarrhoea that persists for more than four weeks is considered to be chronic .
Microscopic colitis is thought to account for 10% of cases of chronic diarrhoea. It classically causes watery diarrhoea in the absence of blood or mucus in the stool.Diagnosis is histological through multiple colonic biopsies.
To date, budesonide is the only treatment that significantly improves symptoms.
BMJ 6 January 2010;340
Patients over 65 were five times more likely to develop microscopic colitis (relative risk 5.6, 95%confidence interval 4.0 to 7.7) than those under 65, and the incidence is higher in women. The condition has two different forms—collagenous colitis and lymphocytic colitis. Microscopic colitis can be used to describe both entities, however, because although they are histologically different they present and are treated in similar ways.9 The most common presentation is chronic watery porridge-like diarrhoea, often several times a day, which lasts a few days then spontaneously resolves before another relapse. There is no associated blood or mucus, but other symptoms include abdominal cramps, nausea, and weight loss.
considerable overlap exists between microscopic colitis and diarrhoea predominant irritable bowel syndrome, and it has been suggested that people with this syndrome should be investigated to exclude microscopic colitis.13 Any clinician must be cautious in diagnosing de novo irritable bowel syndrome in elderly people. The diagnosis of microscopic colitis is based on multiple colonic biopsies through colonoscopy. Macroscopically, the bowel mucosa appears normal.
Histologically, epithelial cells are slightly flattened and the number of globlet cells is slightly decreased. Thickening of the basal lamina is also seen in collagenous colitis, whereas increased numbers of intraepithelial mononuclear inflammatory cells are seen in lymphocytic colitis. A mixed picture is also not uncommon. Biochemical tests and faecal sampling do not aid diagnosis.
The aetiology of microscopic colitis is unknown. Some evidence points to the involvement of immune hypersensitivity or autoimmunity, and the prevalence of autoimmune disorders—such as arthritis, hyperthyroidism, diabetes, scleroderma, and coeliac disease—is increased in patients with microscopic colitis.9 However, unlike ulcerative colitis and Crohn’s disease, the condition does not seem to predispose to the development of malignancy.
Certain drugs have been associated with a higher incidence of microscopic colitis, mostly non-steroidal anti-inflammatory drugs. Although no direct causative link has been shown, such drugs are generally avoided in patients with microscopic colitis.15 Several case reports have also linked lansoprazole with microscopic colitis.16 17 The time delay between initiation of lansoprazole and diarrhoea varied from five days to nine months. Switching to omeprazole reduced the incidence both clinically and histologically within four to 10 days.17 Reports are also emerging of a higher incidence of microscopic colitis in patients on other drugs, such as selective serotonin reuptake inhibitors, statins, and β blockers; however, further studies on larger samples of patients are needed to confirm the strength of these associations.
How is it treated?Until recently, management options for microscopic colitis had largely been anecdotal and varied from case to case. However, a recent systematic review has helped establish which treatments are effective.19 Only treatment with the glucocorticoid, budesonide, which has fewer systemic side effects than prednisolone, has been proved to be effective. Budesonide capsules have been designed to dissolve in a pH dependent manner so that they act locally in the ileum and colon. Less than 10% of the dose is available to the systemic circulation after liver metabolism.
In a recent randomised controlled double blinded trial, 42 patients with lymphocytic colitis were assigned treatment with 9 mg/day oral budesonide for six weeks or placebo. In the treatment arm, 18 patients were in clinical remission compared with 10 given placebo (P<0.01). Histological remission was seen in 15 patients given budesonide compared with 7 given placebo (P<0.03).21 Mesalazine, methotrexate, prednisolone, and probiotics have not been shown to be of significant benefit, although most trials have been small.
Current estimates suggest that 60-80% of patients relapse after budesonide is stopped, and trials have looked at treatment for six weeks only, so further research is needed on the long term effects of budesonide.
Microscopic colitis is a cause of chronic diarrhoea that is growing in prevalence. Until recently little was known about its presentation, diagnosis, and aetiology. It is not thought to be associated with an increased risk of inflammatory bowel disease or colonic malignancy, although patients do have an increased incidence of autoimmune conditions.
It is important at an early stage to exclude any "red flags" that might suggest a more serious pathology.
These include weight loss, passage of blood per rectum, positive clinical findings such as an abdominal mass, and signs of anaemia. In our patient, a change in bowel habit certainly raised suspicion.
• Causes of chronic diarrhoea
• Functional• Irritable bowel syndrome
• Anxiety
• Spurious diarrhoea
• Organic
• Pathological causes within the gut
• Colon:
• Colon carcinoma
• Inflammatory bowel disease (ulcerative colitis or Crohn’s diseas
• Microscopic colitis
• Diverticular disease
• Ischaemic colitis
• Villous adenoma
Small intestine:
Small bowel carcinoma
Coeliac disease
Pancreas:
Chronic pancreatitis
Pancreatic carcinoma
Cystic fibrosis
Gastric:
Gastrectomy
Vagotomy
• Pathological causes outside the gut
• Drugs:• Antibiotics
• Laxatives
• Proton pump inhibitors
• Thiazides
• Alcohol
• Infection
• Endocrine causes:
• Diabetes
• Hyperthyroidism
• Hypoparathyroidism
• Addison’s disease
• Carcinoid syndrome
BMJ 2010;340
Clostridium difficile — Beyond Antibiotics
Standard therapy with oral metronidazole or vancomycin has not changed since the 1970s. Although antibiotics are effective at inhibiting C. difficile and treating symptoms, the use of such drugs does not allow for the reestablishment of normal bowel flora. As a result, 15 to 30% of patients will have recurrent C. difficile infection after the cessation of treatment.1 Many patients will have multiplerecurrences. For older, frailer patients, such recurrences may lead to additional complications, as well as perpetuating the spread of C. difficile in health care settings. In the community, there are many sufferers of recurrent C. difficile infection who have frequent episodes of diarrhea, which has a significant effect on social and occupational functioning.
NEJM January 21, 2010
Various approaches to the management of recurrent C. difficile infection have been tried with variable success. Such measures include repeated courses of metronidazole or vancomycin, tapered and pulsed courses of vancomycin, combinations of antibiotics, toxin binders, probiotics, and immunotherapy. Probiotic therapy ranges from the aesthetically very acceptable but probably ineffective use of probiotic drinks and supplements to the less aesthetically acceptable but probably effective fecal transplantation.2 Intravenous pooled human immunoglobulin products have been used off-label and on an ad hoc basis for passive immunotherapy. However, pharmacokinetic and efficacy data for these products are not available.1 Activeimmunization with a C. difficile toxoid vaccine is currently being tested in a phase 2, randomized, secondary prevention trial
Lowy et al.3 present the results of a multicenter, randomized, double-blind, placebo-controlled trial of two novel neutralizing fully human monoclonal antibodies against C. difficile toxins A (CDA1) and B (CDB1) for the secondary prevention of C. difficile infection. Among 484 eligible patients who were screened at 30 centers in the United States and Canada, 200 were enrolled in the study. These patients were given standard therapy for C. difficile infection and were randomly assigned to receive a single intravenous infusion of either CDA1+CDB1 or saline placebo. Patients were followed for 84 days. The primary outcome measure was recurrent C. difficile infection.
The trial results are impressive. In the intention-to-treat analysis, recurrent infection developed in 7 of 101 patients (7%) in the antibody group, as compared with 25 of 99 patients (25%) in the placebo group, a relative reduction of 72%. Patients with multiple recurrences were particularly likely to benefit, with a relative reduction of 82% in the recurrence rate, as compared with the placebo group. CDA1+CDB1 had no effect on the duration or severity of initial episodes of infection. The monoclonal antibodies were not immunogenic and had an adverse-event profile similar to that of placebo.
The trial results are consistent with previous studies showing that inadequate circulating antibody levels against C. difficile toxins predispose patients to symptomatic and recurrent infection and with observational data suggesting a benefit associated with passive and active immunization for secondary prevention.1,4,5 The mechanism by which systemic antibody responses help to minimize toxin-mediated disease in the colon is not wellunderstood.
Antitoxin antibodies may be exuded through inflamed colonic mucosa. An alternative mechanism for active transport of antitoxin is provided by the IgG Fc receptor FcRN, which is expressed by adult epithelial cells and facilitates the transport of systemic IgG into the intestinal lumen.6 Pharmacokinetic data from the study by Lowy et al. indicate that antitoxin monoclonal antibodies have circulating half-lives of 22 days (for CDB1) to 26 days (for CDA1). This is a critical time for protection, since the majority of recurrences in the placebo group occurred within the first 30 days.
The investigators used a combination of monoclonal antibodies against both toxins A and B, since previous studies in animals and humans have shown that this combination optimally protected against recurrence.7,8 The importance of neutralizing the effects of toxin B as well as toxin A was emphasized in the recent study by Lyras et al.,9 which showed that toxin B was an essential virulence factor in C. difficile infection. The emergence ofclinically relevant C. difficile strains that are negative for toxin A and positive for toxin B further highlights the importance of therapeutic interventions targeted against both toxins.
This novel nonantibiotic approach to secondary prevention is likely to offer hope to physicians and patients battling C. difficile infection. Parenteral administration of monoclonal antibodies will be useful for hospitalized patients who may be unable to take oral medications but may be less convenient for outpatients. The mean age of the patients in the study was 64 years (range, 20 to 101).3 This factor is relevant, since an age of more than 65 years is associated with an increased risk of recurrence by a factor of six, and older patients are likely to benefit most from secondary prevention.10
The lack of efficacy for monoclonal antibodies in attenuating the severity of initial episodes may be related to the definition of severe infection used by study investigators: the occurrence of at least five unformed stools for at least 2 consecutive days. More conventional markers of disease severity (e.g., serum leukocyte counts, creatinine levels, admission to an intensive care unit, and colectomy rates) were not recorded.
We are entering a new era of novel passive and active immunotherapy for the management of C. difficile infection.
Passive immunization with monoclonal antibodies may reduce the rate of recurrence in groups of patients who are likely to have a reduced response to active immunization at a critical time in their illness. Studies are needed to determine whether monoclonal antibodies are useful as adjunctive therapy in patients with severe or fulminant C. difficile infection or whether there is a role for prophylactic passive immunization of patients at high risk for infections associated with health care settings.
It is unlikely that monoclonal antibodies will be used for primary treatment, but they may allow a reduction in the number of days of standard antibiotic therapy for C. difficile infection. These novel approaches to breaking the cycle of C. difficile infection, along with continued attention to appropriate antibiotic use and infection prevention and control, offer hope in the battle against this increasingly prevalent and difficult-to-manage disease.
NEJM January 21, 2010
Diagnosis and management of Barrett’s oesophagusBMJ | 18 SEPTEMBER 2010 | VOLUME 341
Barrett’s oesophagus affects 2% of the adult population in the West, which makes it one of the most common premalignant lesions after colorectal polyps. Conversion to oesophageal adenocarcinoma is the most important complication of the condition, with a lifetime risk of 5% in men and 3% in women.
What is Barrett’s oesophagus and who gets it?
Barrett’s oesophagus is a change in the lining of the oesophagus from normal stratified (multilayered) squamous mucosa to single layered, inflamed, premalignant, mucin secreting mucosa with variable degrees of goblet cell differentiation, termed intestinal metaplasia.It develops in 5% of people with gastro-oesophageal reflux disease, which affects as many as 30% of adults in the Western world.
Evidence from one case series suggests that at least 60% of patients with Barrett’s oesophagus develop the disease as a result of chronic reflux, although other forms of mucosal inflammation in the lower oesophagus (such as from damage by chemotherapy, non-steroidal anti-inflammatory drugs, and viral infections) could be linked to the condition.
What is the natural history of the condition?
The majority of cases of Barrett’s oesophagus stay constant, neither progressing to oesophageal adenocarcinoma nor regressing. Complete resolution of Barrett’s oesophagus is rare, although it is not uncommon to see modest shrinkage of the segment length in patients treated with acid suppression.The risk of progression from Barrett’s oesophagus to oesophageal adenocarcinoma is small in absolute terms (~5% lifetime risk in men and ~3% in women) according to data from case series.
Conditions associated with the development of Barrett’s oesophagus
• Chronic oesophageal reflux (>60% of cases)• Congenital retardation syndromes (1%)
• Non-steroidal anti-inflammatory drugs (1%)
• Chemotherapy (<1%)
• Viral oesophagitis (<1%)
How does Barrett’s oesophagus progress to adenocarcinoma of the oesophagus?
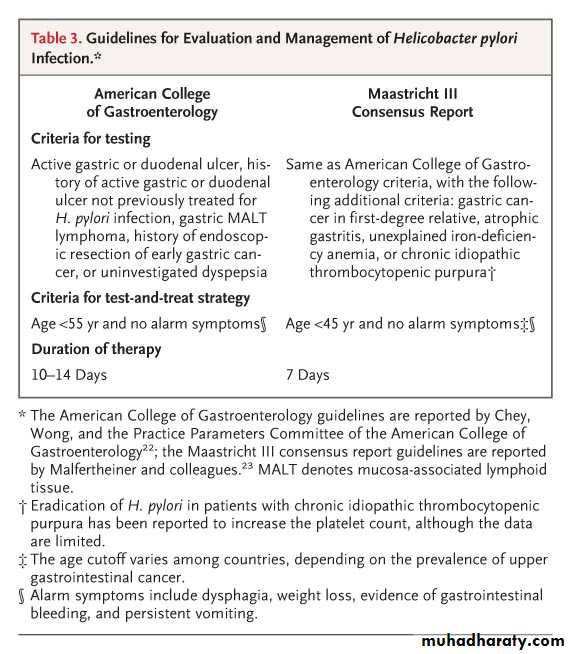
Figure 1 illustrates the stages of progression of Barrett’s oesophagus, from oesophagitis through metaplasia and dysplasia to adenocarcinoma.
The steps of progression to cancer all involve genetic (damage to the DNA in cells) and epigenetic (reversible alterations to cell function) changes. For example, the development of metaplasia is associated with alterations in genes controlling stem cells, and progression to dysplasia is reflected by loss of heterozygosity or methylation of the adenomatous polyposis coli (APC) gene.
Further progression entails loss of expression or mutations in P16 and P53, which decrease their function.12 13 However, none of these biological alterations can yet replace conventional histology for diagnosis and staging, because their exact relationship with clinical progression has not been robustly tested in large randomised clinical trials.
What influences the risk of developing adenocarcinoma?
The major factors associated with progression to cancer are: male gender; white ethnicity; length of Barrett’s segment in centimetres, as seen during endoscopy (higher risk for length greater than 8 cm); diet poor in vegetables and fruit and high in fats; cigarette smoking; and obesity.Case-control studies have shown that symptoms of gastro-oesophageal reflux disease are associated with a significant increase in the risk of developing cancer (odds ratio 40±15), but also that as many as 40% of those with adenocarcinoma do not report a history of reflux symptoms.
How is Barrett’s oesophagus diagnosed?
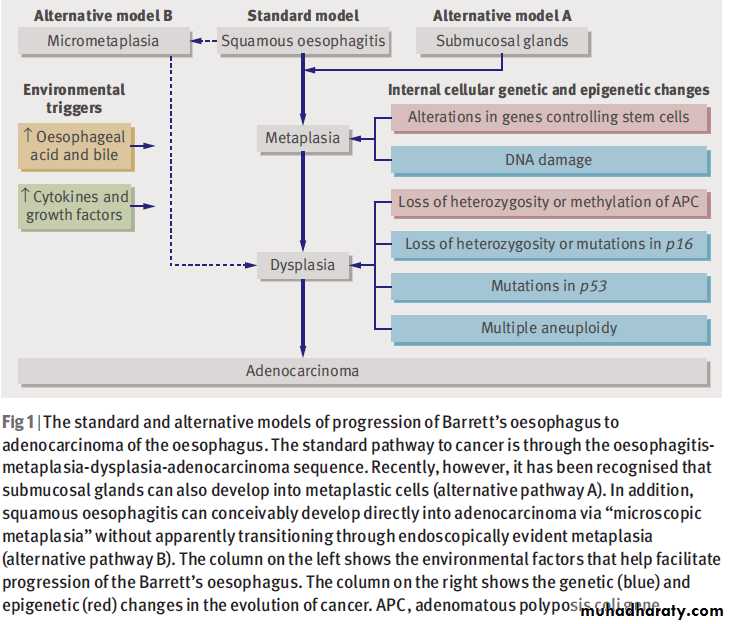
Current guidelines on the management of dyspepsia from the (NICE) advise that patients with symptoms of reflux for more than 5-10 years should be referred for screening endoscopy to check for Barrett’s oesophagus or its complications. On endoscopy, if the distal oesophagus looks pink or crimson in colour and is clearly distinguishable from the appearance of a hiatal hernia (fig 2) using accepted criteria such as the Prague endoscopic criteria, then mucosal biopsies should be examined histopathologically.Biopsy samples are graded as
“diagnostic of Barrett’s oesophagus,” “corroborative of Barrett’s oesophagus,” “consistent with Barrett’s oesophagus,” or “Barrett’s oesophagus not present.”The first three classifications should qualify the patient for entry into an endoscopic surveillance programme.
Protocols for surveillance programmes vary but usually consist of endoscopies every two years with random circumferential biopsies. If dysplasia is found, more frequent intervals of endoscopy a few months apart coupled with more intensive endoscopic pinch biopsies will usually occur. Those who are no longer fit for any intervention may be discharged. However, age alone should not be the sole criterion for removing patients from surveillance.
Does surveillance prevent the development of adenocarcinoma?
Several medium sized case series have found that patients with Barrett’s oesophagus enrolled in surveillance programmes have cancer detected at an earlier (and hence more curable) stage than patients not in a surveillance programme who present with symptoms of oesophageal cancer, but other evidence suggests that patients with cancer related to Barrett’s oesophagus do not benefit from surveillance endoscopy.In addition, several audits have shown that many specialists do not adhere to international guidelines. The Barrett’s Oesophagus Surveillance Study (BOSS) of 2500 patients aims to strengthen the evidence base by identifying both the objective value of endoscopic surveillance in preventing oesophageal cancer, and the best protocol (regular two year upper gastrointestinal endoscopic surveillance programme versus endoscopy at time of need).
The cost effectiveness of surveillance is still highly uncertain in the absence of real cost estimates from randomised controlled trials such as BOSS. Costs have been estimated to be about £40 000 (€50 000; $60 000) per cancer diagnosed for less than one quality adjusted life year (QALY) gained.
Surveillance related prevention of oesophageal adenocarcinoma might not dramatically increase the longevity of patients because Barrett’s oesophagus has also been associated with an increased risk of other potentially fatal conditions. For example, Barrett’s oesophagus might be associated with obesity and gastropulmonary aspiration, which increase the risk of ischaemic heart disease and bronchopneumonia, respectively.
The cost effectiveness is arguably better in the US because the country has a lower incidence of oesophageal adenocarcinoma than in the UK and endoscopic surveillance is undertaken less often (three yearly in the USA compared with two yearly in the UK). In addition, endoscopic surveillance is more cost effective when undertaken only in patients with proven intestinal metaplasia on biopsy, because such patients are three times more likely to develop cancer than those without proven intestinal metaplasia.
What treatments can prevent progression of Barrett’s oesophagus to adenocarcinoma?
Case series have suggested that as many as 10% of patients with Barrett’s oesophagus develop high grade dysplasia in their lifetime. Cohort studies have shown that such patients have an increased risk of progression to adenocarcinoma compared with those who have non-dysplastic Barrett’s oesophagus (30-55% in 8 years).Data from several case-control series indicate that management of multifocal areas of high grade dysplasia can be technically difficult and may require multiple interventions. Experts agree that because of their increased risk of cancer, such patients warrant intervention with either several sessions of endoscopic ablation therapy or, in exceptional cases, oesophagectomy. Arguably these patients represent a bigger burden to healthcare providers than those with cancer.
Proton pump inhibitors
A recent large randomised controlled trial found that early effective therapy for gastro-oesophageal reflux disease with proton pump inhibitors both manages symptoms effectively and heals oesophageal ulceration. These findings support the use of acid suppressant drugs such as proton pump inhibitors not only to heal and maintain healing of oesophagitis but also for “chemoprevention” in patients with Barrett’s oesophagus.Case-control studies and randomised controlled trials have shown that proton pump inhibitor therapy is well tolerated and safe in patients with Barrett’s oesophagus, despite initial fears that they may promote elongation of Barrett’s oesophagus through hypergastrinaemia.
However, case reports have speculated about a possible link between use of proton pump inhibitors and intestinal infections—especially Clostridium difficile—deficiencies of nutrients like folate and vitamin B12, and osteoporosis. Proton pump inhibitors also reduce the effectiveness of clopidogrel, and co-administration of the two drugs should be avoided if possible.
Some practitioners have attempted to reduce costs and potential for side effects by treating patients who have gastro-oesophageal reflux disease with on demand proton pump inhibitor therapy. However, this approach might be the worst of all options because intermittent treatment could increase the risk of Barrett’s oesophagus and adenocarcinoma. Partial treatment might prevent the oesophagitis from healing completely and might also conceivably allow the metaplastic Barrett’s cells at the ulcer base, which can tolerate a low pH, to colonise the residual ulcerated oesophageal mucosa.
Detecting significant differences between interventions for relatively rare outcomes in Barrett’s oesophagus such as adenocarcinoma would need a controlled study with a very large number of subjects. Future developments in linking routine clinical data with research in the community could potentially facilitate this type of large scale study.
A large randomised trial in secondary care—the Aspirin Esomeprazole Chemoprevention Trial (AspECT)—is currently evaluating the long term value of low dose (20 mg) esomeprazole (a proton pump inhibitor) compared with high dose (80 mg) esomeprazole, either with or without aspirin (aspirin may help to prevent cancers of the gastrointestinal tract). So far 2513 patients have been recruited into the trial, and an interim analysis in one large centre has found a low rate of major side effects, suggesting that any interaction between esomeprazole and aspirin is acceptable.
TIPS FOR NON-SPECIALISTS
Who should be referred for routine endoscopy?Patients with reflux for more than five years and who are aged over 50 years
What are the alarm symptoms for immediate referral for endoscopy?
Dysphagia.Weight loss.Vomiting blood.Anaemia
What other comorbid diseases should be screened for?
Ischemic heart disease.Hypercholesterolaemia
What is the best treatment approach for patients diagnosed with Barrett’s oesophagus?
90% can be managed by acid suppression therapy,
5% may benefit from Nissen fundoplication
5% may develop adenocarcinoma after at least 15 years
What dose of proton pump inhibitors should be used?
Use the lowest effective dose that suppresses symptoms so that heartburn occurs less than once a week
When should patients be reviewed?
Primary care physician—Dose of proton pump inhibitors should be reviewed annually, and healthy living messages—such as maintaining a low fat diet, exercising, and maintaining a BMI of less than 30—
Secondary care physician—Patients should be reviewed endoscopically every two years in the UK and every three years elsewhere (because of higher incidence of cancer in the UK)
Nissen fundoplication
Randomised controlled trials have shown that surgical repair of the oesophageal sphincter by buttressing the stomach onto the oesophagus (fundoplication) offers good symptom control in patients with severe reflux disease and Barrett’s oesophagus. In addition, this approach might be cheaper than proton pump inhibitors when drug use over many years is anticipated.Other randomised trials have confirmed that surgery controls reflux more completely than does medical therapy.
Furthermore, fundoplication may prevent all constituents of the refluxate, including contents of the duodenum such as bile, from entering the oesophagus, which may not occur with proton pump inhibitor therapy according to evidence from case series.
Newer endoscopic therapies
Endoscopic mucosal resection for the eradication of early cancers (by definition confined to the mucosal lining) is highly effective—five year survival is 98% in patients with early adenocarcinoma confined to the mucosa and high grade dysplasia. The type of epithelium that re-grows is in part determined by the depth of injury that occurs as a consequence of treatment. In order to ensure squamous cell regeneration as opposed to recurrence of Barrett’s oesophagus, some of the superficial squamous lined ducts of the oesophageal mucus glands must survive.Photodynamic therapy comprises systemic administration of photosensitising agents that are retained selectively in malignant tissue. When exposed to appropriate wavelength laser light, a cytotoxic reaction occurs that causes cellular destruction. The strongest evidence for the effectiveness of photodynamic therapy comes from the five year follow-up of a randomised, multicentre, multinational, pathology blinded trial that evaluated the usefulness of the technique to eradicate dysplasia.
Photodynamic therapy was significantly more effective at eradicating high grade dysplasia than omeprazole only (odds ratio 2±0.7) and reduced the likelihood of developing cancer by half, with a significantly longer time to progression in the photodynamic therapy group compared with the omeprazole group. It may be necessary to repeat ablation at intervals, and patients treated this way should remain in lifelong surveillance.
A further randomised trial compared thermal ablation and argon plasma coagulation with surveillance in 40 patients who had undergone surgical reflux control. Significant reversal of Barrett’s oesophagus occurred in patients treated by argon plasma coagulation ablation (63% v 15% in patients under surveillance (odds ratio 4.1±1.2)). Most recently, a randomised trial showed that radiofrequency ablation is effective in ablating both non-dysplastic and dysplastic Barrett’s oesophagus, with complete eradication in 90.5% and 81.0% of cases, respectively.
The immediate side effects of ablation are minor retrosternal discomfort in 30% of patients, but full functional activity is possible in almost all patients. Stricture, bleeding, and perforation occur in 10%, 1%, and less than 1% of patients, respectively.
Recently published NICE guidelines from the UK recommend that clinicians consider offering endoscopic ablative therapy as an alternative to oesophagectomy for people with high grade dysplasia and intramucosal cancer, according to individual patient preferences and their suitability for the procedure.
NICE guidelines consider endoscopic therapy—especially endoscopic resection and radiofrequency ablation—to be particularly suitable for patients who are considered unsuitable for surgery and those who do not wish to undergo oesophagectomy
What does the future hold?
There is not yet consensus on the value of either tissue or blood biomarkers to stratify patients with Barrett’s oesophagus in terms of risk of developing cancer. Researchers hope that data from genome-wide association studies may further understanding of the inherited basis of Barrett’s oesophagus and its progression, which might allow risk stratification for individual patients based on ethnicity, gender, and mucosal phenotype and may facilitate individually tailored treatment.Several genetic consortiums are being set up to replicate these genetic data once published and validate them for clinical use. Perhaps the largest in Europe is the Esophageal Adenocarcinoma Genetic LinkagE (EAGLE) consortium, which incorporates both the Chemoprevention Of Premalignant Intestinal Neoplasia (ChOPIN) trial and the Inherited Predisposition of Oesophageal Diseases (IPOD) study.
A large specialist and patient international consensus on the management of high grade dysplasia (BArretts’s Dysplasia and CAncer Taskforce (BAD CAT)) is due in 2011.
BMJ | 18 SEPTEMBER 2010 | VOLUME 341
Transjugular Intrahepatic Porto Systemic Shunts• Functions similar to surgical shunts
• No surgery, done transjugular
• Re-bleed rate 20% in first year
• Major drawback is hepatic encephrlopathy
• Shunt stenosis common
• Very expensive
• Best used as salvage procedure
Rotavirus Vaccine — A Powerful Tool to Combat Deaths from Diarrhea
Rotavirus infection, the leading cause of severe childhood diarrhea in both developed and developing countries, results in over half a million deaths each year.1 Currently, two rotavirus vaccines (Rotarix [GlaxoSmithKline Biologicals] and RotaTeq [Merck]) are licensed in many countries and used routinely in several. Until recently, available efficacy data were from developed and developing countries with relatively low mortality rates among children younger than 5 years of age,the first dose between 6 and 15 weeks of age, and the third dose no later than 32 weeks of age.
Motion sickness or kinetosis, also known as Travel Sickness, is a condition in which a disagreement exists between visually perceived movement and the vestibular system's sense of movement. Depending on the cause it can also be referred to as seasickness, car sickness, simulation sickness, airsickness, or space sickness.
Dizziness, fatigue, and nausea are the most common symptoms of motion sickness.[Sopite syndrome in which a person feels fatigue or tiredness is also associated with motion sickness. Nausea in Greek means seasickness (naus means ship).
Motion sickness can be divided into three categories:
• motion sickness caused by motion that is felt but not seen motion is sensed by the vestibular system and hence the motion is felt, but no motion or little motion is detected by the visual system.
• motion sickness caused by motion that is seen but not felt detected by the visual system and hence the motion is felt, but no motion or little motion is sensed by the vestibular system.
• motion sickness caused when both systems detect motion but they do not correspond.
Dizziness due to spinning
When one spins and stops suddenly, fluid in the inner ear continues to rotate causing a sense of continued spinning while one's visual system no longer detects motionTreatment
Many cures and preventatives for motion sickness have been proposed.Natural
One common suggestion is to simply look out of the window of the moving vehicle and to gaze toward the horizon in the direction of travel. This helps to re-orient the inner sense of balance by providing a visual reaffirmation of motion.
In the night, or in a ship without windows, it is helpful to simply close one's eyes, or if possible, take a nap. This resolves the input conflict between the eyes and the inner ear. Napping also helps prevent psychogenic effects (i.e. the effect of sickness being magnified by thinking about it).
A simple method for relieving common and mild car sickness is chewing. Chewing gum has an uncanny effectiveness for reducing car sickness in those affected. Chewing gum, however, is not the only thing one may chew to relieve mild effects of car sickness, snacking on lollies or just chewing in general seems to reduce adverse effects of the conflict between vision and balance.
Fresh, cool air can also relieve motion sickness slightly, although it is likely this is related to avoiding foul odors which can worsen nausea.
Chemical
Over-the-counter and prescription medications are readily available, such as Dramamine (dimenhydrinate),Stugeron (cinnarizine), and Bonine/Antivert (meclizine).Scopolamine is effective and is sometimes used in the form of transdermal patches (1.5 mg) or as a newer tablet form (0.4 mg). The selection of a transdermal patch or scopolamine tablet is determined by a doctor after consideration of the patient's age, weight, and length of time treatment is required.
Interestingly, many pharmacological treatments which are effective for nausea and vomiting in some medical conditions may not be effective for motion sickness. For example, metoclopramide and prochlorperazine, although widely used for nausea, are ineffective for motion-sickness prevention and treatment. This is due to the physiology of the CNS vomiting centre and its inputs from the chemoreceptor trigger zone versus the inner ear. Sedating anti-histamine medications such as promethazine work quite well for motion sickness, although they can cause significant drowsiness.
Ginger root is commonly thought to be an effective anti-emetic. One trial review indicated that sucking on crystallized ginger or sipping ginger tea can help to relieve the nausea,[17] while an earlier study indicated that it had only a placebo effect.[18] Tests conducted on the television show Mythbusters support the theory that ginger is an effective treatment for the nausea caused by motion sickness.[19]
Ginger is reported to calm the pyloric valve located at the base of the stomach.[17] This relaxation of the valve allows the stomach to operate normally whereby the contents will enter the small intestine instead of being retained within the stomach. It is this undesirable effect of retention in the stomach that eventually results in vomiting. Stugeron is not available in the U.S. either over-the-counter or by prescription. It has been implicated in triggering palsy and has been banned by the FDA.
Electronic
As astronauts frequently have motion sickness, NASA has done extensive research on the causes and treatments for motion sickness. One very promising looking treatment is for the person suffering from motion sickness to wear LCD shutter glasses that create a stroboscopic vision of 4 Hz with a dwell of 10 milliseconds.[2Motion sickness is the unpleasant sensation of nausea and dizziness that some people experience when riding in a moving vehicle. Motion sickness can be brought on by travelling in cars, boats, submarines, aeroplanes, trains, by riding amusement rides that spin, and even when using a swing at a playground. Astronauts in zero-gravity space can also suffer from a form of motion sickness, called ‘space adaptation syndrome’.
Children between the ages of four and 12 years are particularly prone to motion sickness. Symptoms can range from mild to serious. Frequent vomiting can lead to dehydration and low blood pressure, so it is important to seek prompt medical attention if you are severely affected. Motion sickness is also known as travel sickness. Other popular terms depend on the mode of transport: for example, airsickness, carsickness or seasickness.
Symptoms of motion sickness can include:
Generally feeling unwellExcessive production of saliva
Headache
Nausea
Dizziness
Hyperventilating
Heavy sweating
Weakness
Losing colour in the face or turning red
Vomiting.
Conflicting informationSuppose you are a passenger in a car, reading a map while being driven along a winding road. Your inner ear tells your brain (via the vestibular nerve) that your body is moving but, according to your eyes which are focused on the stationary map, your body is still. At sea, the eye views the static horizon or the unmoving interior of the boat while the body feels the rolling of the waves.
The clash of sensory information is passed along to a portion of the brain known as the area postrema, which lies close to the brain area responsible for vomiting. It appears that motion sickness can only occur if the vestibular system is intact, because people with damaged vestibular nerves don’t experience motion sickness.
One theory suggests that the vomiting response is caused by the brain’s futile attempt to rid the body of a perceived poison.
(Laboratory animals whose labyrinths are surgically removed are less likely to vomit when they have eaten poison.)
There are different things you can try to prevent motion sickness or at least reduce its effects including: Watch the scenery going by, so that your eyes confirm the sensation of motion picked up by your inner ear. This may mean, for example, being out on deck at sea. However, don’t fix your gaze on individually moving objects, such as each rolling wave - just scan generally.
Position yourself where you will experience the least motion: for example, over the wings in an aeroplane or in the dead centre of a ship.
If possible, drive the vehicle. Passengers in moving cars are more likely to experience motion sickness than drivers.
The larger the vehicle, the less susceptible it is to motion so, if possible, try to travel on a ship rather than a small boat, for instance.
Keep your head still. Moving your head around will ‘swirl’ the fluid in your canals and add to the sensory confusion.
Some people find that closing their eyes is the best way to eliminate sensory confusion.
Lying down on your back allows the fluid in the ear canals to pool, rather than swirl around.Cut back on, or eliminate, alcoholic drinks and don’t have any alcohol for 24 hours before travelling.
Make sure you have plenty of fresh air. Fumes or smoke can exacerbate symptoms.
On brief journeys, try not to eat or drink anything.
On long journeys, eat and drink sparingly and often.Anxiety worsens symptoms. Use relaxation techniques such as abdominal breathing or an absorbing book or hobby to counteract the effect of worrying. If your anxiety is severe, you could consider professional counselling.
Medications either calm the nerves of the inner ear or soothe the brain’s vomiting centre. However, most motion sickness pills are only effective if they are taken before you feel sick. In many cases, motion sickness pills can induce drowsiness as a side effect. You may need to experiment with the different drugs available to find which one works best for you. Ask your doctor or chemist for further information.
Research suggests that ginger can help to ease the symptoms of motion sickness. You could chew on raw ginger or make a quick tea by adding minced ginger to boiling water.
High-Fiber Foods
Dietary FiberDietary fiber is only found in plants, and functions like a skeleton to help maintain their shape and structure. Humans eat plants but we cannot digest the fiber so it passes through the small intestine into the colon. The fiber helps to keep the colon healthy. Some disorders like diverticulitis, constipation and irregularity may be connected with not getting enough fiber in the diet.
Types of Dietary Fiber
Insoluble fiber is the type of dietary fiber found in high-fiber foods like whole grains, nuts, wheat bran and vegetables. Insoluble fiber does not dissolve in water so it helps to move material through the colon faster by increasing the bulk of the stool. This can be very helpful to people who suffer from constipation or irregularity. Diets high in insoluble fiber may also decrease the risk of diabetes.Soluble fiber is also found in many high-fiber foods like oats, citrus fruits as oranges and apples ,Vegetables such as carrots ,barley, psyllium, flax seeds and beans. Soluble fiber absorbs water, which helps to soften stools making them easier to eliminate from the body. Some soluble fibers, like beta glucan found in oats, bind to bile acids in the intestinal tract. Bile acids contain cholesterol and normally your body reabsorbs some of those bile acids, but when their bound to beta-glucan, they are eliminated through the stool. This reduces the amount of bile reabsorbed into your blood, and in turn helps to lower cholesterol levels. high-fiber foods are usually high in vitamins and minerals as well.
Complex carbohydrates are chains of three or more single sugar molecules linked together. Long chains of sugar molecules called starches serve as a storage form of energy in plants and when you eat those plants, your body breaks down the carbohydrates for your own energy needs.
Another form of complex carbohydrate called cellulose forms the structural components that give plants their shape, and is a main component of dietary fiber.
Foods with the most complex carbohydrates include legumes, starchy vegetables like potatoes and corn, rice and grain products Other vegetables such as green beans, broccoli and spinach contain less starch, but they have more fiber.
Complex carbohydrates should supply about half the calories in your diet; however, the best complex carbohydrates come from legumes, vegetables and 100% whole grain bread, cereal and pasta products because they contain fiber and a variety of nutrients that refined flour has lost.
Spinach
Whole BarleyGrapefruit
Turnip Greens
Buckwheat
Apples
Lettuce
Buckwheat bread
Prunes
Water Cress
Oat bran bread
Apricots, Dried
Zucchini
Oatmeal
Pears
Asparagus
Oat bran cereal
Plums
Artichokes
Museli
Strawberries
Okra
Wild rice
Oranges
Cabbage
Brown rice
Yams
Celery
Multi-grain bread
Carrots
Cucumbers
Pinto beans
Potatoes
Dill Pickles
Yogurt, low fat
Soybeans
Radishes
Skim milk
Lentils
Broccoli
Navy beans
Garbanzo beans
Brussels Sprouts
Cauliflower
Kidney beans
Eggplant
Soy milk
Lentils
Onions
Whole meal spelt bread
Split peas
• Some examples of healthy foods containing complex carbohydrates:
Table sugar
Corn syrupFruit juice
Candy
Cake
Bread made with white flour
Pasta made with white flour
Soda pop, such as Coke®, Pepsi®, Mountain Dew®, etc.
Candy
All baked goods made with white flour
Most packaged cereals
• Some examples of foods containing simple carbohydrates:
• Simple carbohydrates are more refined, are usually found in foods with fewer nutrients, and tend to be less satisfying and more fattening.
Simple carbohydrate is a sweetener that is classified as a monosaccharide or a disaccharide. Some common examples of simple carbohydrates are glucose, sucrose and lactose.like sugar and corn syrup, are created in a factory – while
complex carbohydrates in vegetables and whole grains are designed by nature, and help you maintain your health.
Fresh fruit is one of the best sources of carbohydrates that fall into this category. Berries, grapefruit, apples, and pears all provide a quick lift without adding a lot of calories to the body. For this reason, natural sources of simple carbohydrates are often recommended for people who are trying to lose weight.
However, there is another grouping of simple carbohydrates that is not considered helpful with the task of losing weight. These include processed foods. Among these are such foods as fudge, cakes, and any type of candy. The carbohydrate content in processed foods is what usually gives simple carbohydrates their reputation as bad carbs, since the carb content of these types of foods also includes a great deal of calories.
With the popularity of low-carb diets, many people are afraid to eat any carbohydrates, but it is important to distinguish between the health-robbing effects of simple sugars and other carbs, and the health-giving properties of complex carbohydrates.
Complex carbohydrates are high-fiber foods, which improve your digestion. They help stabilize the blood sugar, keep your energy at an even level, and help you feel satisfied longer after your meal.
In contrast, sugar and other simple carbohydrates can alter your mood, lead to cravings and compulsive eating, cause wide swings in your blood-sugar levels, and cause weight gain in most people. In addition, a high consumption of sugar can lead to uncomfortable withdrawal symptoms when you finally decide to improve your diet and forgo the sweets.
The glycemic index, or GI is a measure of the effects of carbohydrates on blood sugar levels. Carbohydrates that break down quickly during digestion and release glucose rapidly into the bloodstream have a high GI; carbohydrates that break down more slowly, releasing glucose more gradually into the bloodstream, have a low GI. The concept was developed by Dr. David J. Jenkins and colleagues[1] in 1980–1981 at the University of Toronto in their research to find out which foods were best for people with diabetes.
Classification
GI rangeExamples
Low GI
55 or less
most fruits and vegetables, legumes/pulses, whole grains, nuts, fructose and products low in carbohydrates
Medium GI
56–69
whole wheat products, basmati rice, sweet potato, sucrose
High GI
70 and above
baked potatoes, watermelon, white bread, most white rices, corn flakes, extruded breakfast cereals, glucose
The 40 Best Age-Erasing Superfoods
The latest science on
the muscle building,
brain-enhancing,
Wrinkle erasing,
heart-strengthening,
bone-protecting,
Immunity boosting,
and inflammation fighting
foods you should be eating every day.
Almonds
Flaxseeds
Tomatoes
Pomegranates
Ginger
ArtichokesWalnuts
Avocado
Spinach
Wild Salmon
Green Tea
Carrots
Whole Grains
Yogurt
BroccoliKiwis
Olive Oil
Leeks
Eggs
Grass-Fed Beef
Figs
Pineapples
Mushrooms
The Search for Effective Treatment of Clostridium difficile InfectionC. difficile infection is particularly
problematic when three factors are aligned:
coexisting conditions, including
advanced age;
disturbed intestinal microbiota as a result of antibiotic therapy or antitumor drugs; and exposure to
vegetative cells or spores of C. difficile.
NEJM february 3, 2011
C. difficile infection has four clinical forms:
short-term colonization, which usually developswhen a patient is in a health care facility;
acute diarrhea, ranging from mild to severe; fulminant diarrhea, which may be associated with pseudomembranous colitis (which in some cases requires colectomy) and leukocytosis and may lead to
death; and
recurrent C. difficile infection, which
typically occurs within 60 days after initial treatment
for the infection.
Current treatments for C. difficile infection are inadequate. Metronidazole is an inexpensive treatment that is considered by
most authorities to be the standard therapy for
nonsevere cases of C. difficile infection, Unfortunately, metronidazole has unacceptable
pharmacokinetic characteristics; it is almost
completely absorbed in the gut, resulting in
very low drug levels in the colon and a high rate
of treatment failure. Severe cases of C. difficile
infection are treated preferentially with oral vancomycin.
Recurrent disease is
seen in 20 to 30% of cases, regardless of whichof these two treatments is used. recurrence appears to be related
to a combination of a failure to reestablish
microbial flora, the presence in the intestines of
spores of C. difficile, and a defective host immune response to the infecting organism and its toxins.
Because of the importance of intestinal flora in
the recovery process, antibiotics that inhibit vegetative cells of C. difficile while preserving colonic flora or aiding in the restoration of flora during treatment are being evaluated preferentially.Fidaxomicin, a new macrocyclic antibiotic that has no cross-resistance with other antibiotics, has in vitro activity against strains of C. difficile and may have less deleterious effects on intestinal microbiota than do other commonly used antibacterial agents.
In this issue of the Journal, Louie et al. report
the results of a phase 3 trial involving 629 patients,in which fidaxomicin was compared with
vancomycin in the treatment of C. difficile infection.
The rates of clinical cure in the two groups
were similar, but C. difficile infection recurred significantly less often with fidaxomicin than with
vancomycin (15% vs. 25% in the modified intention-to-treat population, P = 0.005).
The most promising agents for future development
should be safe, have low levels of systemic
absorption, have low potential for the development of resistance among intestinal and
extraintestinal bacteria, provide high levels of active drug in the colon, and be associated with a
low rate of recurrence of C. difficile infection after treatment. Fidaxomicin fits these criteria better than any other agent evaluated so far.
Therapy for C. difficile infection is generally administered for either 10 or 14 days, Additional study is needed
to determine the optimal duration of treatment for C. difficile infection.
With data showing that the rate of recurrence
of C. difficile infection is increased in patients inwhom anti–C. difficile toxin A IgG antibodies do
not develop, immunologic approaches to the prevention and treatment of recurrences are in development and include the use of immunoglobulins, monoclonal anti–C. difficile toxin antibodies,and active immunization. Perhaps future therapy for C. difficile infection will combine an antibacterial drug with an immunologic approach.
NEJM february 3, 2011
Intensive care units (ICUs) are high-risk settings for the transmission of methicillinresistant
Staphylococcus aureus (MRSA) and vancomycin-resistant enterococcus (VRE).Treatment
with systemic antibiotics that have antianaerobic
activity promotes high-density colonization of VRE
in the gastrointestinal tract, and the use of fluoroquinolone has been associated with increased rates of MRSA colonization or infection. Efforts to reduce the unnecessary use of these agents may complement other interventions.
Intervention to Reduce Transmission
of Resistant Bacteria in Intensive Care
NEJM april 14, 2011
Standard interventions to prevent the transmission
of MRSA and VRE in health care facilities
include hand hygiene, the use of barrier
precautions (gloves and gowns) in the care of
colonized and infected patients, the use of dedicated instruments and equipment for these patients, and the placement of colonized or infected patients in single rooms or multibed rooms
or areas reserved for such patients.
Additional interventions, including active surveillance —screening to identify asymptomatically colonized patients who may serve as undetected reservoirs of MRSA and VRE(nasal swabs for MRSA surveillance cultures and stool or perianal swabs for VRE surveillance cultures) .
topical antimicrobial,Intranasal mupirocin, reduces MRSA colonization in the short term, but its long-term effect is limited and is associated with the development of mupirocinresistance. Daily bathing of patients with chlorhexidine and improved environmental cleaning have, in quasi-experimental studies, shown promise in reducing the incidence of MRSA and VRE colonization among ICU patients.
NEJM april 14, 2011
A large outbreak of diarrhea and the hemolytic–uremic syndrome caused by an unusual serotype of Shiga-toxin–producing Escherichia coli (O104:H4) began in Germany
in May 2011. As of July 22, a large number of cases of diarrhea caused by Shiga-toxin–producing E. coli have been reported — 3167 without the hemolytic–uremic syndrome (16 deaths) and 908 with the hemolytic–uremic syndrome (34 deaths) — indicating
that this strain is notably more virulent than most of the Shiga-toxin–producing E. coli strains.
NEJM July 27, 2011
We used third-generation, single-molecule, real-time DNA sequencing to determine
the complete genome sequence of the German outbreak strain, as well as the genomesequences of seven diarrhea-associated enteroaggregative E. coli serotype O104:H4
strains from Africa and four enteroaggregative E. coli reference strains belonging to other serotypes.
Results
The enteroaggregative E. coli O104:H4 strains are closely related and form a distinct clade among E. coli and enteroaggregative E. coli strains. However, the genome of the German outbreak strain can be distinguished from those of other O104:H4 strains
because it contains a prophage encoding Shiga toxin 2 and a distinct set of additional
virulence and antibiotic-resistance factors.
Conclusions :
studies revealed that the outbreak strain belonged to an enteroaggregative E. coli lineage that had acquired genes for Shiga toxin 2 and for antibiotic resistance.Our findings suggest that horizontal genetic exchange allowed for the emergence of
the highly virulent Shiga-toxin–producing enteroaggregative E. coli O104:H4 strain
that caused the German outbreak. More broadly, these findings highlight the way in which the plasticity of bacterial genomes facilitates the emergence of new pathogens.
NEJM July 27, 2011
Antibiotics for Both Moderate and Severe Cholera
Several antibiotics are effective in the treatment of cholera, including doxycycline, ciprofloxacin,and azithromycin, assuming that the cholera strain is sensitive. The WHO advocates giving antibiotics
to patients with cholera only when their illness is judged to be “severe.” This recommendation
is interpreted to mean that only patients who present with “severe dehydration” (≥10% dehydration) should be given antibiotics.
NEJM January 5, 2011.
With effective antibiotic therapy,the purging rate is lessened by about 50%, the illness is shortened by about 50%, and the duration
of excretion of Vibrio cholerae in the stool is shortened to 1 or2 days. Without effective antibiotic therapy, patients continue toexcrete V. cholerae for 5 or more days and shed for a longer period at home. If antibiotics are used,patients recover more quickly andrequire less rehydration fluid.Nursing care is lessened, and patients are able to leave the treatment
center earlier, as demonstrated in a study that showed
dramatic resolution of diarrhea at 24 hours with azithromycin.
Regarding transmission, ricewater stools contain 1011 to 1012V. cholerae organisms per liter. An
infectious dose is 105 to 108 organisms.
These numbers might explain why 50% of household contacts of a patient who is the
index case in Bangladesh develop diarrhea about 2 days after the index case occurs. Direct data
are not available to determine whether household contacts are protected when the index case is
treated with antibiotics. However,given the liter volumes of diarrhea,antibiotics will decrease
contamination in the household.
We do not, however, recommend antibiotic prophylaxis for household contacts because of the programmatic difficulty in restricting the use of such prophylaxis only to those persons in the immediate family who are at highest risk and because doing so would almost certainly drive antibiotic resistance. Since families of patients with cholera are at high risk for cholera themselves,they need targeted education about safe water and sanitation,appropriate home use of oral rehydration solution, and information
about the availability of treatment facilities in case illness does occur.
A practical reason for hesitancy regarding administering antibiotics to patients with cholera relates to the severe vomiting that usually accompanies infection.Vomiting generally stops within a few hours after patients are rehydrated;thus, the administration of the antibiotic should be delayed until the patient is able to take food and drink without vomiting. Doxycycline can be associated with nausea and should be taken with food and plenty of fluids.
In summary, the use of antibiotics is an urgent issue for all stakeholders, because effective
antibiotic therapy shortens the duration of illness and reduces the shedding of thousands of
infectious doses. Our goal is to promote more effective care for large numbers of patients with
cholera while maximizing limited resources to keep patients who are discharged early from dying,
reduce the number of repeat hospital admissions, and limit at home shedding of V. cholerae. To
achieve these aims, we believe that patients with moderate and severe cholera should be treated
with antibiotics.
NEJM January 5, 2011.
Anti-tissue transglutaminase
Antibodies to tissue transglutaminase (anti-tTG) are found in patients with several conditions, including coeliac disease, juvenile diabetes,inflammatory bowel disease[3], and various forms of arthritis[4].
In Coeliac Disease, ATA are involved in the destruction of the villous extracellular matrix and target the destruction of intestinal villous epithelial cells by killer cells. Deposits of anti-tTG in the intestinal epithelium predict coeliac disease.
Transglutaminase isoform reactivity
Anti-endomysial reactivity
The endomysium is a layer of connective tissue that ensheaths a muscle fiber. The endomysium contains a form of transglutaminase called "tissue transglutaminase" or "tTG" for short, and antibodies that bind to this form of transglutaminase are called anti-endomysial antibodies or EMA for short,[6] therefore targeting those cells for apoptosis. The antiendomysial antibody test is a histological assay for patient serum binding to esophageal tissue from primate. EMA are present in celiac disease. They do not cause any direct symptoms to muscles, but detection of EMA is useful in the diagnosis of the disease.Anti-epidermal transglutaminase
Antibodies to epidermal transglutaminase (eGT, also Keratinocyte transglutaminase) are the autoantibodies believed to cause dermatitis herpetiformis.ATA IgA are more frequently found in CD; however, ATA IgG are found in CD and at higher levels when affected individual had the IgA-less phenotype. The IgA-less phenotype is more common in CD than the normal population; however, one haplotype, DQ2.5 is found in most CD, has genetic linkage to the IgA-less gene location