FDA approves first drug to prevent HIV infection
BMJ 17 July 2012)د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
The US Food and Drug Administration this week approved for
the first time a drug for use in the prevention of HIV infection.The drug, Truvada, is one of the most commonly used
components of an anti-HIV “cocktail” regimen in the United
States and Europe.
Truvada is two drugs combined in a single pill, tenofovir
disoproxil fumarate and emtricitabine. Its preventive use is
commonly referred to as PrEP (pre-exposure prophylaxis).
Studies in different groups at high risk of infection have shown
its efficacy.
It was approved “to reduce the risk of HIV infection in
uninfected individuals who are at high risk of HIV infection
and who may engage in sexual activity with HIV-infected
partners,” said Debra Birnkrant in a telephone press conference
with reporters. She is director of the Office of Antimicrobial
Products at the FDA’s Center for Drug Evaluation and Research.
Although the incidence of HIV in the US has held steady for
about a decade, at about 50 000 new infections a year, it has
increased in some groups, notably young men from ethnic
minority groups who have sex with men, she said. “
These data show that treatment and new prevention methods are needed in order to have a major impact on the HIV epidemic in this country.”
She added, “Truvada for PrEP represents another effective, evidence based approach that can be added to other prevention methods to help reduce the spread of HIV . . . [when] used daily
as part of a comprehensive HIV prevention strategy that includes other prevention measures.”
After concerns discussed at an advisory committee meeting in May, the FDA has added a “black box warning” to the label requiring that “a negative HIV test must be documented before
prescribing the drug and throughout use of PrEP.”
The FDA’s risk evaluation and mediation strategy requires counsellor education and training for those who prescribe PrEP.
Patients will be given educational materials and urged to sign “a contract” to be placed in their file stating that they understand the need for strict adherence to the daily regimen and for quarterly testing for HIV.
Some people fear that PrEP might lead to “disinhibition” and hence greater risk of infection because of riskier sex and less condom use. Birnkrant said that the placebo controlled studies
did not support that fear.
Furthermore, she said, there is reason
to believe that adherence might increase in real world use because people know that they are being prescribed a drug whose effectiveness has been proved.
The drug has been widely used for a decade and is generally well tolerated. There are some long term problems of bone and kidney toxicity that are “for the most part manageable, can be monitored,” and are reversed on discontinuation of treatment, said Birnkrant.
Support for PrEP has been widespread but not universal among
those working in HIV prevention and treatment. One vocalopponent has been the AIDS Healthcare Foundation, a large
provider of HIV care that is based in Los Angeles but that has
clinics in several states and internationally.
“Widespread use of PrEP has all the makings of a public health
disaster: increased HIV infections, drug resistant strains of HIV,
and tens of thousands of damaged kidneys,” said the
foundation’s president, Michael Weinstein, in March, when it
filed a “citizens’ petition” with the FDA to delay or deny
approval of the drug for prevention.
Gilead Sciences, which makes the drug, has said that it will
work with public health officials and community groups to makesure that the drug is available to those who need it most. This
is likely to include price discounts.
There are no estimates of how widespread use of PrEP might
become. Leading health insurance companies have stated that
they will cover the cost of the drug for a PrEP indication once
it is approved.
No Link Between Birth Defects and Antiretroviral Use in Pregnancy
NEW YORK (Reuters Health) Jul 19 - Antiretroviral use in pregnancy does not seem to increase the risk of birth defects, a new U.S. study finds.
Lead author Dr. Robert S. Brown Jr from the New York Presbyterian Hospital told Reuters Health by email, "It is reassuring" that pregnant women can take tenofovir or lamivudine and "there does not appear to be any increase in the birth defects."
"The data provide guidance for patients and practitioners who either need or want to begin these drugs in pregnancy as to their predicted safety," he said.
Antiretrovirals are not licensed for use in chronic hepatitis B in pregnancy, and their safety is not fully established, but Dr. Brown and his coauthors point out that the drugs are still sometimes used to reduce viral load and mother-child transmission.
"The purpose of this study is not to advocate off-label use of antiviral therapies in pregnancy," they said.
Using data on 13,711 women registered with the Antiretroviral Pregnancy Registry (APR) from 1989-2011, the researchers analyzed birth defect rates among users of various antiretrovirals. Major structural defects, chromosomal defects diagnosed by age six, and aborted fetuses were all counted as birth defects.The authors say the APR is the largest worldwide registry of birth defects related to exposures to antiviral drugs.The prevalence of birth defects was similar among the antiretroviral users and population-based controls (2.8% vs. 2.7% respectively), the researchers reported online June 26th in the Journal of Hepatology.
Birth defect rates were also similar with antiretroviral exposure in the first trimester and later trimesters (3% vs. 2.7%).
Rates with lamivudine, tenofovir and all antiretrovirals combined were similar as well: 3.1%, 2.4% and 3%, respectively, during first trimester and 2.7%, 2% and 2.8% during later trimesters.
The authors say they specifically looked for an increased risk of cardiovascular and renal defects with lamivudine and did not find it.
"The fact that initial exposure to these medications in the first, versus remaining, trimesters was associated with similar birth defect rates supports a lack of teratogenicity,"
Dr. Brown and his colleagues wrote.
"Safety is a complex term and (it is) obviously better to not need to take any medications during pregnancy," Dr. Brown said. "But this (study) suggests that any adverse effects on the fetus are rare enough that they cannot be detected in this relatively large data set."Preexposure Prophylaxis for HIV Prevention
NEJM July 18, 2012c ase vignet tes
The first patient, a 46-year-old sexually active
man who has sex with men, presents for routine
primary care. He lives in New York City and reports
that he is in a long-term, stable, open relationship
with a male partner and that he has had
multiple recent sexual encounters with acquaintances.
A recent HIV test was negative. He has seasonal allergies, for which he occasionally takes antihistamines, and chronic lower back
pain, for which he takes nonsteroidal antiinflammatory
drugs on a regular basis. Otherwise he takes no medications and has no known allergies to medications. He had syphilis 10 years earlier for which he was successfully treated. His physical examination is notable only for the fact that he is uncircumcised.
You review HIV prevention strategies in detail with him, including the potential benefits of circumcision and of the use of condoms. He has been reading information on the Internet, including information about preexposure prophylaxis (PrEP), and asks whether he should be receiving this therapy.
The second patient, an 18-year-old heterosexual
woman in South Africa who has recently becomesexually active, presents for voluntary HIV testing.
She does not know the HIV status of her male
partners. She reports no medical problems, is taking
no medications, and has no known allergies
to medications. She reports that her older sister
recently received a diagnosis of HIV infection.
Her physical examination is unremarkable.
Testing for sexually transmitted infections is performed.
A pregnancy test is negative. She would like to
initiate birth control and elects to start taking
oral contraceptive pills. She returns to the clinic
the following week and is informed that all the
tests for sexually transmitted infections, including
the HIV test, were negative. She thinks that
she had received the hepatitis B vaccination series.
She is negative for hepatitis B surface antigen. She
is given extensive HIV counseling, and the various
HIV prevention strategies are reviewed in detail.
Which one of the following approaches would
you find appropriate for these patients? Baseyour choice on the published literature, your own
experience, recent guidelines, and other sources
of information, as appropriate.
1. Recommend initiating PrEP.
2. Do not recommend initiating PrEP.
To aid in your decision making, each of these
approaches is defended in the following short
essays by experts in the prevention of HIV infection.
Recommend Initiating PrEP
Salim S. Abdool Karim, M.B., Ch.B., Ph.D.
The decision-making process for recommending
PrEP begins with an assessment of the risk of
HIV, followed by a determination of the combination
of HIV-prevention strategies that provides
the maximum protection. In the United States,
men who have sex with men comprise approximately
2% of the population but account for
more than 60% of new HIV infections.
Treatment option 1
A history of sexually transmitted diseases and multiple
partners places the man in the first vignette athigh risk. Despite education and condom-promotion
programs, young women are the highest risk group in Africa, where the prevalence of
HIV among women 20 years of age is as high as
26.7%.1 The fact that the young woman in the
second vignette has had multiple partners places
her at high risk in the generalized HIV epidemic
in South Africa, where 12% of the population
(approximately 5.6 million people) are HIV-infected.
Her risk is higher if any partner is 5 or more
years older than she is.
The effective options for HIV prevention that
are available for the persons in both vignettes include the use of condoms, “sero-sorting” (choosing only partners who are HIV-negative), treatment for prevention (ensuring that all HIV-positive partners are taking antiretroviral treatment),
and, finally, PrEP. Although medical circumcision
of men is an established HIV-prevention option
for heterosexual men, it has not yet been
proven to be effective in protecting women or
men who have sex with men
Although an HIVprevention strategy that is based on knowing every partner’s HIV status is desirable, this is rarely possible. Even partners who recently tested HIV-negative have a tangible risk, in highincidence groups, of having an undiagnosed
“window-period” infection or of having acquired
HIV after the test was performed.
Among HIVpositive partners who say they are receiving treatment, the risk of their transmitting the virus to others depends on their having actually
initiated treatment, their adherence to treatment,
and consequent viral suppression. In the case of
young African women, who are seldom able to
insist on the use of condoms or to establish the
HIV status or treatment status of their partners,
placing their risk of infection totally in the
hands of their male partners is risky and fundamentally undermines efforts to empower women to control their own risk.
Hence, PrEP, which empowers receptive partners
to control their HIV risk, is an essential
component of an effective combination prevention
strategy for the persons in both vignettes.
In the absence of renal disease, daily treatment
with tenofovir disoproxil fumarate (TDF) coformulated
with emtricitabine (FTC), a therapy for
which there are extensive safety data, should be
prescribed, since it was shown to be effective in
reducing HIV acquisition among men who have
sex with men in the Preexposure Prophylaxis
Initiative (iPrEX) trial4 and among heterosexual
partners in the Partners PrEP5 and TDF26 trials.
In these studies, drug resistance, which is aconcern with the use of any antiretroviral agent,was an uncommon occurrence and was largelyrestricted to persons who initiated PrEP during an undiagnosed window-period infection. Nucleic acid testing (which tests for the presence of virus before antibodies can be detected) at the time of the initiation of PrEP, a costly option,
could reduce the risk of resistance.
For resistance that may still be present at the initiation of future treatment, effective therapeutic options
other than TDF–FTC are available. It is important
that PrEP be accompanied by counseling on
the continued and increased use of condoms and
on adherence to therapy, in order to avoid the
lack of effectiveness that was observed in the Preexposure Prophylaxis Trial for HIV Prevention
among African Women (FEM-PrEP).
Widespread implementation of PrEP is, however,
not without challenges that will require additional
financial resources and health services
capacity. Nevertheless, PrEP is an essential new
HIV-prevention strategy that can and should be
implemented in combination with the use of condoms, HIV testing, and promotion of treatments
for HIV infection. PrEP prevents HIV infection,
thereby reducing the need for treatment of AIDS
in the future, is cost-effective,8 and empowers
vulnerable populations to directly control their
risk of HIV infection.
Do Not Recommend Initiating
PrEPGlenda E. Gray, M.B., B.Ch., and
Neil Martinson, M.B., B.Ch., M.P.H.
There are an estimated 5.6 million HIV-infected
people in South Africa, and countrywide surveillance
of pregnant women shows that 14.0% of
pregnant girls and women 15 to 19 years of age
and 26.7% of pregnant women 20 to 24 years of
age were HIV-infected in 20109 — statistics that
suggest that the woman in the second vignette is
at high risk for HIV infection.
treatment option 2
PrEP with daily TDF–FTC4 has been shown to
reduce the risk of HIV acquisition in two specific
populations — men who have sex with men
and serodiscordant couples in Africa. However,
the data are inconclusive, since other trials have
shown no effect in women. PrEP was not shown
to be effective in the FEM-PrEP study,7 in which
daily TDF–FTC was administered in women, nor
in the TDF group of the Vaginal and Oral Interventions
to Control the Epidemic (VOICE) study,10
which was discontinued early for futility.
Although adherence to daily medication has been shown
to influence the effectiveness of PrEP, the inconsistentresults among similar PrEP studies suggest that additional factors influence the effectiveness of PrEP in preventing the acquisition of HIV.
The efficacy data reported from the Partners PrEP study are difficult to extrapolate to the general population, since there may be unique features associated with HIV transmission in the context of a long-term, stable, serodiscordant partnership.
The data on the efficacy of PrEP in the TDF2 study, which was conducted in Botswana, are tantalizing, but there are substantial challenges to understanding these data, especially the effect of the low rate of retention of participants
(which resulted in early termination of the study),
the poor adherence to the study medication, and
an apparent benefit only early after the initiation
of PrEP.
At first glance, the reported 62.2% reduction in HIV acquisition is compelling; however, of nine participants who were HIV-infected despite the receipt of TDF–FTC, seven were women, and in a subanalysis that was restricted
to women, there was no significant protection with TDF–FTC as compared with placebo. Moreover, this and other studies raise concerns about the interaction of TDF–FTC with oral contraceptives, the selection of viral resistance in persons
with undetected HIV-infection at baseline and in
those who undergo seroconversion while receiving
PrEP, and the proper monitoring over time
of the safety of PrEP, including the effect on renal
function and bone mineral density.
Given the high risk of inducing HIV resistance at the initiation of PrEP, HIV nucleic acid testing (not just HIV
antibody testing) should be considered as part of
the assessment before the initiation of PrEP. This
testing is costly and not widely available. The
implications of all these issues in the context of
the increased clinical use of PrEP are substantial
and have yet to be pragmatically sorted out.
Our management of the cases described in both vignettes would therefore include HIV testing
and counseling, including encouragement
that the partners be tested for HIV. We would
encourage the woman in the second vignette to
approach her partners (who are assumed to be
heterosexual, HIV-negative, and uncircumcised)
to be circumcised. We would provide an adequate
supply of male and female condoms and
highlight the importance of adherence to oral
contraceptives.
Given the available data, recommending initiation
of PrEP is premature in either circumstance.
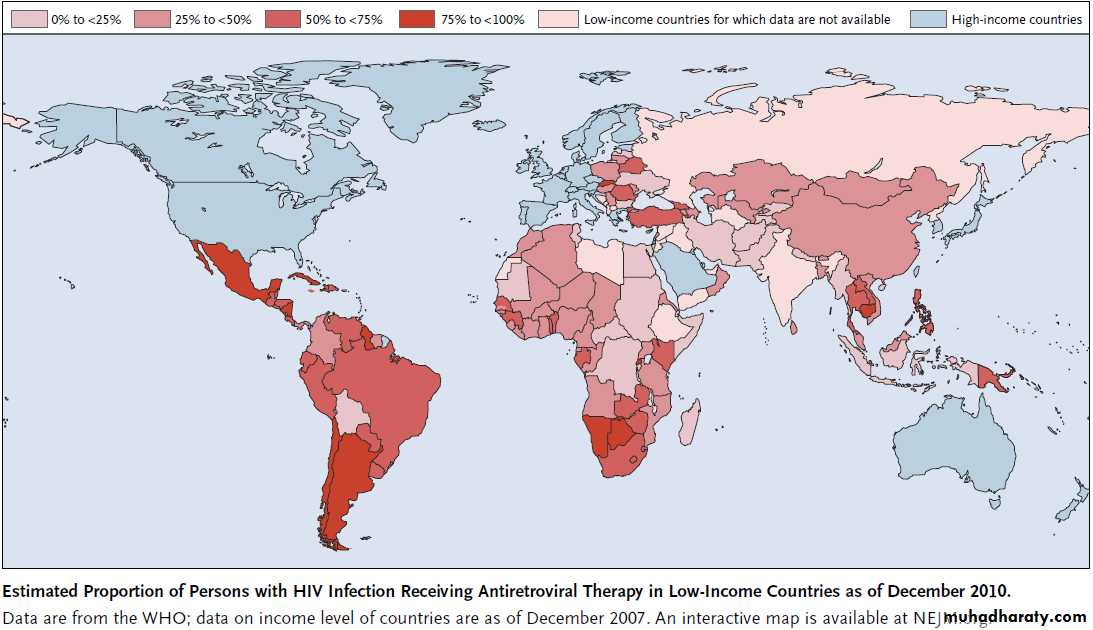
For example, in South Africa, approximately 1.8
million people have initiated antiretroviral therapy,
representing 55% of the people who require
this therapy. First-line therapy now includes TDF,
at a cost of $11 billion (in U.S. dollars).
The implementation of antiretroviral therapy in South
Africa has been further stressed by the increasein the threshold for initiating treatment to a CD4
count of 350 cells per cubic millimeter. In addition,
the frequent lack of availability of antiretroviral
drugs suggests that existing antiretroviral
treatment programs are already overwhelmed.
Until robust concordant trial data are available
to guide the complexity of practice here, we
should not grasp at straws. Giving effective antiretroviral
treatment to HIV-infected persons earlier
and enhancing the use of proven strategies
should be the current mainstays for preventing
HIV transmission.
In neonates whose mothers did not receive ART during pregnancy, prophylaxis with a
two- or three-drug ART regimen is superior to zidovudine alone for the prevention of
intrapartum HIV transmission; the two-drug regimen has less toxicity than the threedrug
regimen. (Funded by the Eunice Kennedy Shriver National Institute of Child Health
and Human Development [NICHD] and others; ClinicalTrials.gov number, NCT00099359.)
NEJM June 20, 2012.
The Beginning of the End of AIDS?
NEJM July 18, 2012.We are at a moment of extraordinary optimism
in the response to the human immunodeficiencyvirus (HIV). A series of scientific breakthroughs,
including several trials showing the partial efficacy of oral and topical chemoprophylaxis and the first evidence of efficacy for an HIV vaccine candidate,
have the potential to markedly expand the available preventive tools.
There is evidence of the first cure of an HIV-infected person. And most important, the finding that early initiation of antiretroviral therapy can both improve
individual patient outcomes and reduce the risk of HIV transmission to sexual partners by 96%4 has led many to assert what had so long seemed impossible:
that control of the HIV pandemic may be achievable.
What will it take to achieve what U.S. Secretary of State Hillary Rodham Clinton called, in a2011 address, an “AIDS-free generation”?
Expanded access to and coverage of high-quality prevention and treatment services tailored
to affected populations are critical to keeping people living with HIV healthy and to dramatically
reducing the number of new HIV infections.
This goal requires an ambitious implementation science agenda that improves efficiency and effectiveness and incorporates strategies for overcoming the stigma and discrimination
that continue to limit the uptake and utilization of services.
Research efforts on HIV vaccines will also probably be key, and thefield has been reinvigorated, after
a series of unsuccessful trials, by the findings of the RV144 trial involving Thai adults, which showed that the vaccine provided modest protection against HIV acquisition in selected populations.
Research focused on curing HIV disease is yielding fascinating insights into how HIV persists in the
face of current therapy, and such research must be earnestly pursued. A combination approach to
prevention that includes HIV treatment can generate tremendous gains in the short term by curtailing
new HIV infections, but ending the AIDS epidemic will
probably require a vaccine, a cure, or both.
The scientific opportunities and optimism at this moment in HIV research are not matched, however, by the available resources.
Global resources have been declining, not growing, in this period of scientific success. This lack of funding is the major point of divergence between optimism and pessimism.
Every country, including ours, must develop more effective ways to reach key affected populations
and to apply the tools that we know work, if we are to make significant advances.
Is there a roadmap to an AIDSfree generation? The core elements of a strategy are arguably now
in hand: first, the strategic use of existing resources, including resources for accelerated research
on prevention, HIV vaccines, and a cure; second, marked increases in HIV testing, counseling, and
linkages to and retention in services and care;
third, the eradication of mother-to-child transmission of HIV and preservation of maternal health, a goal very much within the realm of possibility with existing knowledge; and finally, expanded access to prevention services and antiretroviral treatment to reach everyone in need — which will require an end to the stigma, discrimination,
legal sanctions, and human rights abuses against people at risk for or living with HIV infection.
Markedly expanding high-quality treatment programs, taking newprevention tools to scale, and
maximizing the potential of antiretroviral therapies for prevention will be difficult and costly, but failure to capitalize on the scientific advances of this critical period could be devastating. A future of ongoing transmission of HIV,ever-increasing numbers of people receiving or needing therapy, and further strains on overburdened health systems will not be sustainable.
As the international HIV community gathers in Washington, D.C., for the 19th International AIDS Conference, the meeting’s theme, “Turning the Tide Together,” captures the essence of this defining moment. The response to HIV, perhaps better than efforts against any other epidemic, encapsulates
what can be accomplished when scientists, policymakers, the private sector, and the community mobilize toward a common goal. Propelling us to the point where we can talk about the end of AIDS is nothing short of remarkable.Yet the most important part of the story is about to be written.