Effect of Two Intensive Statin Regimenson Progression of Coronary Disease
NEJM November 15, 2011د. حسين محمد جمعة
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
Background
Statins reduce adverse cardiovascular outcomes and slow the progression of coronaryatherosclerosis in proportion to their ability to reduce (LDL)cholesterol. However, few studies have either assessed the ability of intensive statin
treatments to achieve disease regression or compared alternative approaches to maximal statin administration.
Methods
We performed serial intravascular ultrasonography in 1039 patients with coronary disease, at baseline and after 104 weeks of treatment with either atorvastatin, 80 mg daily, or rosuvastatin, 40 mg daily, to compare the effect of these two intensive statin regimens on the progression of coronary atherosclerosis, as well as to assess their safety and side-effect profiles.Results
After 104 weeks of therapy, the rosuvastatin group had lower levels of LDL cholesterol than the atorvastatin group (62.6 vs. 70.2 mg per deciliter [1.62 vs. 1.82 mmol per liter], P<0.001), and higher levels of high-density lipoprotein (HDL) cholesterol (50.4 vs. 48.6 mg per deciliter [1.30 vs. 1.26 mmol per liter], P = 0.01). The primary efficacy end point, percent atheroma volume (PAV), decreased by 0.99% (95% confidence interval [CI], −1.19 to −0.63) with atorvastatin and by 1.22% (95% CI, −1.52 to −0.90) with rosuvastatin (P = 0.17).The effect on the secondary efficacy end point, normalized total atheroma volume (TAV), was more favorable with rosuvastatin than with atorvastatin: −6.39 mm3 (95% CI, −7.52 to −5.12), as compared with −4.42 mm3 (95% CI, −5.98 to −3.26) (P = 0.01). Both agents induced regression in the majority of patients: 63.2% with atorvastatin and 68.5% with rosuvastatin for PAV (P = 0.07) and 64.7% and 71.3%, respectively, for TAV (P = 0.02). Both agents had acceptable side-effect profiles, with a low incidence of laboratory abnormalities and cardiovascular events.
Conclusions
Maximal doses of rosuvastatin and atorvastatin resulted in significant regression of coronary atherosclerosis. Despite the lower level of LDL cholesterol and the higher level of HDL cholesterol achieved with rosuvastatin, a similar degree of regression of PAV was observed in the two treatment groups. (Funded by AstraZeneca Pharmaceuticals;ClinicalTrials.gov number, NCT000620542.)imaging trials have shown that intensive statin regimens slow the progression of coronary atherosclerosis and may even result in disease regression in some patients.
Accordingly, guidelines for cardiovascular
disease prevention have increasingly emphasized
that lowering LDL cholesterol levels with
statins is the primary goal of lipid-modulating
therapy.
Atorvastatin and rosuvastatin are the most
effective statins for lowering LDL cholesterol levels,yielding average reductions that approach 50% foratorvastatin and exceed 50% for rosuvastatin. Direct comparisons have shown greater reductions in LDL cholesterol levels and greater increases in HDL cholesterol levels with rosuvastatin
The use of intravascular ultrasonography in clinical trials permits examination of the effects of antiatherosclerotic therapies on the course of coronary artery disease.
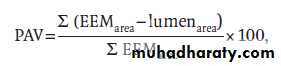
percent atheroma volume (PAV), was calculated as follows:
where EEMarea is the cross-sectional area of the
external elastic membrane, and lumenarea is thecross-sectional area of the lumen. For PAV, the
summation of the EEM area minus the lumen
area is performed first. This value is then divided
by the summation of the EEM area, which is finally multiplied by 100. The change in PAV was
calculated as the PAV at 104 weeks minus the PAV at baseline.
As compared with the atorvastatin regimen, the rosuvastatin regimen resulted in lower LDL cholesterol levels (a difference of −7.5 mg per deciliter [−0.19 mmol per liter]) and slightly higher HDL `cholesterol levels (a difference of 1.8 mg per deciliter [0.05 mmol per liter]). These differences did not result in a significant incremental effect on disease regression, as assessed according to the primary intravascular ultrasonographic end point
(PAV). These results may have been influenced by smaller-than-anticipated differences between the two groups with respect to HDL cholesterol levels.
Rosuvastatin did show a significant benefit with
respect to disease regression as assessed according to TAV, a secondary intravascular ultrasonographic end point, but the difference between the two regimens was relatively modest. These data show that the two regimens are similar in their ability to limit progression or induce regression of coronary disease, although a small difference in efficacy cannot be ruled out on the basis of the significant differences observed for the change in TAV.Our study shows that in appropriately selected patients, either regimen can be used to reduce the atheroma burden for the purpose of secondary prevention.
Overall, regression of atherosclerosis was observed
in approximately two thirds of the study patients during 104 weeks of statin therapy. For the primary end point (PAV), a numerically higher percentage of rosuvastatin-treated patients had regression (68.5%, vs. 63.2% with atorvastatin),with a trend toward significance (P = 0.07). The frequency and extent of regression in both groups were unprecedented, as compared with the results of prior intravascular ultrasonographic studies.Previous studies have suggested an association
between progression rates and cardiovascular outcomes, but the precise nature of the relationship remains a subject of ongoing research. Theoretically,regression involves reductions of the lipid,
inflammatory, and necrotic components of plaque,
each of which has been implicated in plaque rupture.Yet intravascular ultrasonography remains
asurrogate end point, and a reduction in plaque
volume should not be interpreted as equivalent to
a clinical benefit in terms of preventing cardiovascular events.
Furthermore, the clinical significance of regression or of observed differences in the secondary end point remains to be established.
Despite these limitations, we consider the current
evidence showing that the growth of atherosclerotic plaques can be reversed to be promising and deserving of further study in clinical trials.
The incidence of adverse effects accompanying
the benefits observed in this trial was low. Increases in liver enzyme levels were more common in the atorvastatin group, with alanine aminotransferase levels that were more than 3 times the upper limit of the normal range in 14 patients, as compared with 5 patients in the rosuvastatin group (2.0% vs. 0.7%).Creatine kinase levels were more than 10 times the upper limit of the normal range in 4 atorvastatin-treated patients and in 1 rosuvastatin-treated patient, but in neither treatment group were there two consecutive increases in creatine kinase levels that were more than 5 times the upper limit of the normal range. Rhabdomyolysis was not observed in any patient.
Proteinuria was more common in the rosuvastatin group than in the atorvastatin group (3.8% vs. 1.7%). Although the effect of statins on the incidence of diabetes has received considerable attention recently, neither treatment group had an increase in glycated hemoglobin levels.
Taken as a whole, our findings indicate that intensive statin treatment led to disease regression with few adverse events.
Although the study was not powered to detect
between-group differences in major adverse clinical events, these outcomes were adjudicated at acentral site. The overall incidence of myocardial infarction was 1.6% during 24 months of followup, and the incidence did not differ significantly between the treatment groups.The rate of stroke was 0.4% and the rate of cardiovascular death was 0.3%, with no significant between-group differences in these rates. Only 0.5% of patients underwent coronary-artery bypass grafting, but 5.4% of patients underwent percutaneous coronary intervention,in most cases for restenosis involving lesions initially treated at the time of enrollment.
These event rates are extremely low for a population
with angiographically documented coronary disease and affirm that very intensive lipid-lowering with statins is associated with favorable clinical outcomes in a patient population at high risk.
Although subgroup analyses do not furnish
definitive evidence of benefit or harm, they mayprovide hypothesis-generating insights. Statistical evidence of heterogeneity showing benefit with Rosuvastatin,the most useful measure of subgroup differences, was observed among women and among patients with higher baseline levels of LDL cholesterol.
The greater benefit noted among patients with higher HDL cholesterol levels may reflect improved functional activity of HDL. The better response of patients with higher LDL cholesterol levels seems biologically plausible, since these patients may have greater benefits from a more effective LDL cholesterol–lowering regimen. Future analyses may yield useful insights into which of the effects of statin therapy — reductions in LDL cholesterol levels, increases in HDL cholesterol levels, nonlipid antiinflammatory effects, or a combination of effects — is associated with plaque regression.
Our findings have implications for the development
of novel antiatherosclerotic therapies. TheLDL cholesterol levels seen in this study are lower
than those endorsed by current guidelines, providing
a biologic foundation for future trials that
target very low LDL cholesterol levels. The levels
of LDL and HDL cholesterol observed in the current
study cannot be achieved with statins alone
in all patients with atherosclerotic coronary disease;
however, LDL cholesterol–lowering therapies
currently under development may result in these
lipid levels in more patients.
Furthermore, about one third of patients in our study had disease progression despite maximally intensive statin therapy.
This finding suggests a potentially important
role for novel agents designed to reduce LDL cholesterol
levels, increase HDL cholesterol levels, or
modify disease activity by means of other pathways.
Indeed, a substantial residual risk of clinical
events remains in most secondary-prevention populations despite the use of the most effective current medical therapies, affirming the need for new
antiatherosclerotic agents.
This study has important limitations. It was not
ethically possible to measure disease progression
in placebo-treated patients. The trial involved patients undergoing clinically indicated coronary
angiography. It remains uncertain whether our
findings apply to primary prevention in asymptomatic patients.
In trials that use intravascular ultrasonographic assessment of regression–progression,some patients elect not to undergo follow-up cardiac catheterization and therefore cannot be considered in the calculation of intravascular ultrasonographic end points.
In the current trial, 25% of patients did not have intravascular ultrasonographic imaging that could be evaluated at follow-up, which was a smaller percentage than that reported in most contemporary trials. Patients who did not complete the trial may have had rates of progression that were different from those among patients who completed the trial. This study used intravascular ultrasonography to examine disease progression, but some newer analytic methods may permit the characterization of plaque constituents. Alternative therapies might have differing effects on plaque composition.
Statins have been among the most extensively
studied classes of pharmacologic therapies.The findings have elucidated how these agents work
and have expanded their potential clinical usefulness.
Although the current comparative study does not show a significant difference between the
treatment groups with regard to the primary endpoint, it does show that high-dose, intensive
statin therapy can be administered safely and can
promote regression of atherosclerotic plaque to a
greater extent than has previously been reported.
These findings represent a useful step forward in
the effort to prevent the devastating clinical sequelae
of atherosclerotic cardiovascular disease.