د. حسين محمد جمعة
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
Diagnosis and management of the solitary pulmonarynodule
Case reportBMJ 13 December 2011
A 67 year old woman presented with a worsening cough and atwo month history of a small amount of blood in her saliva. She had no history of weight loss, pleuritic pain, or constitutional symptoms. In addition, she had shortness of breath secondary
to chronic obstructive pulmonary disease, and she was on supplemental oxygen at home.
Her medical history included myocardial infarction, moderate to severe peripheral vascular
disease, and type 2 diabetes. She continued to smoke one pack of cigarettes a day and had a cumulative 130 pack year history of smoking.Chest radiography showed a 2.7 cm single pulmonary nodule in the right middle lobe adjacent to the mediastinum. The lesion was confirmed to be non-small cell lung carcinoma by acomputed tomography guided lung biopsy. As part of the staging process, a positron emission tomography-computed tomography (PET-CT) scan was done, which confirmed a malignant right middle lobe lesion, stage IA (T1b), with no nodal or pleural involvement.
Pulmonary function testing showed that an operative resection would not be suitable. Treatment options were combined
chemoradiotherapy and percutaneous ablation. Percutaneous radiofrequency ablation was performed, and the post-procedural
PET-CT scan at one year showed no clinically relevant residual disease.
1 What is the most common clinical
presentation of lung cancer?Short answer
Cough.
Long answer
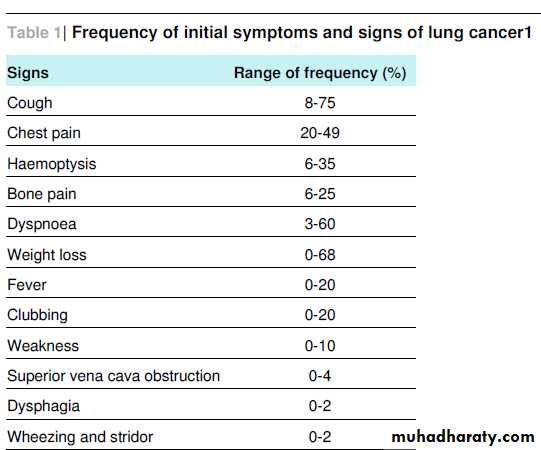
Lung cancer is the second most commonly diagnosed cancer in the United Kingdom. Because of the cancer’s insidious presentation, symptoms are not usually evident until the disease is advanced. At presentation 90% of patients are symptomatic.The most common presenting symptom is cough (8-75%), then weight loss, dyspnoea, chest pain, and haemoptysis (6-35%) (see table 1⇓).
Symptoms can be local (such as cough), distant
as a result of metastatic deposits (such as pain from a bone metastasis), or systemic (such as weight loss). Haemoptysis is rarely severe and usually consists of blood streaking of the sputum. Although findings on chest radiography are usually abnormal in patients with haemoptysis from lung cancer, a small proportion of patients’ chest radiographs will be normal or willnot show a localising abnormality.
What are the indications for biopsy of a lung mass?
Short answerBiopsy is indicated in the presence of a peripheral lesion with no evidence of advanced metastatic disease. The patient must be medically suitable for the procedure.
Long answer
If a solitary pulmonary nodule is suspicious on radiological assessment—if it shows
spiculation,
absence of calcification,or substantial change in interval size—a tissue sample can direct further management.
Methods of obtaining tissue include
bronchoscopy,
transthoracic needle aspiration,
video assisted thoracoscopy, and diagnostic thoracotomy. The method chosen
depends on the position of the lesion within the lungs—whether peripheral or central (within 3 cm of the mediastinum or great vessels).
The increased risk of complications from more invasive
techniques must be weighed against the probability of finding benign lesions.
Transthoracic needle aspiration or core biopsy involves insertion of an aspiration needle or core biopsy needle percutaneously to remove fluid or tissue from the lung, which is then examined for cancer.
Computed tomography or ultrasound can be used to
guide the insertion of the needle. This well established technique has a high sensitivity and specificity for diagnosis of lung cancer, with a low complication rate.
A systematic review assessing mortality and morbidity in 4527 patients undergoing percutaneous biopsy found that a chest drain was needed in 10% of patients, haemoptysis occurred in 4% of patients, pneumothorax occurred in 31%, and 0.04% of patients died.
In patients with peripheral lung lesions, percutaneous biopsy provided a more accurate way of diagnosing lung cancer thanbronchoscopy and mediastinoscopy, although
bronchoscopy remains the best option for central lesions. However, the management of solitary pulmonary nodules is complex and is constantly developing with input from respiratory
physicians,radiologists, thoracic surgeons, and oncologists.
3 What is the value of PET-CT in investigating
a lung nodule?Short answer
Improved staging and treatment planning, particularly in patients with non-small cell lung carcinoma.
Long answer
The use of PET or PET-CT has become routine in the
investigation and staging of lung cancers, largely because of its superiority over other imaging modalities. In the UK, guidelines
have been published by both the National Institute for Health and Clinical Excellence and the Scottish Intercollegiate Guidelines Network on the use of PET in lung cancer.
The salient points of these guidelines are:
• Patients suitable for surgery on computed tomographycriteria should have a PET-CT scan to look for nodal
disease and distant metastases
• Patients with N2/3 disease, of uncertain pathological
relevance, who are otherwise suitable for surgery, should
also undergo PET-CT
• If PET-CT is positive, histological or cytological
confirmation of N2/3 disease should be sought
• If there is definite metastatic disease or a high probability
that the N2/N3 disease is metastatic then histology or
cytology confirmation is not needed
• Biopsy is not needed when PET-CT for N2/N3 disease is
negative, even with enlarged nodes on CT.
PET-CT improves the preoperative staging of non-small cell lung carcinoma and can potentially reduce the number of futile thoracotomies and the total number of thoracotomies.
In 2002,a randomised intention to treat study of 188 patients with non-small cell lung carcinoma showed that, compared with conventional staging, staging with PET-CT resulted in a relative reduction in the risk of futile thoracotomy of 51% and an absolute risk reduction of 20%. Current PET-CT scanners have a spatial resolution of the order of 4-6 mm, so they can potentially miss lesions below 1 cm in size.
What are the current management
guidelines for non-resectable non-small cell
lung carcinoma?
Short answer
• Radiotherapy alone,
• combined chemoradiotherapy,
• Percutaneous ablation, or
• chemotherapy, depending on the stage and
performance status.
Long answer
About 80% of patients with lung cancer have non-small cell lung carcinoma, and most are not suitable for surgical treatment,either because of the stage of the cancer or other limiting
comorbidities. However, 30-35% of patients with non-small cell lung carcinoma present with disease sufficiently localised for attempted curative surgical resection.
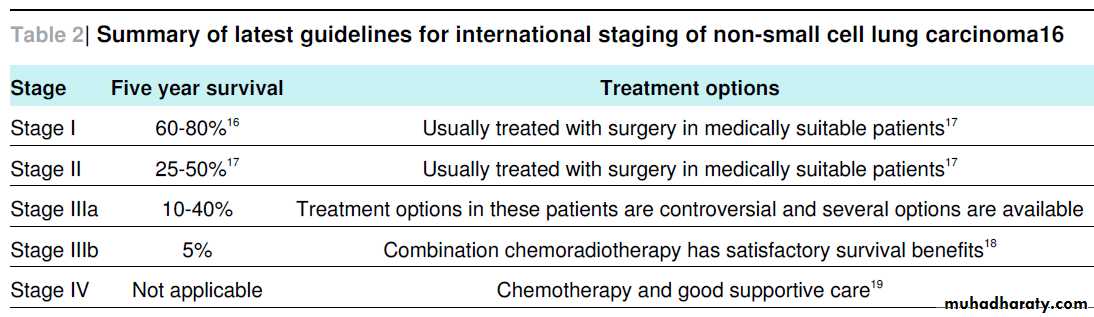
The latest version of the international staging classification for non-small cell lung carcinoma (version 7; 2009) can be used for the most current guidelines for treatment options and survivalrates (table 2⇓).
In clinical practice,
lobar resection continues to be the gold standard in stages I and II of the disease but is often not feasible because the patient has reduced lung capacity (as in our case);other factors to consider are patient preference, poor performance status, or anaesthetic risk.
Patients in any staging group who fall into one of these categories can be considered for other treatment options—such as chemotherapy
(including adjuvant chemotherapy), molecular therapy,conventional radiotherapy, stereotactic radiotherapy, ablation (including radiofrequency, cryotherapy, and microwave ablation), or combinations of these modalities—depending on local expertise and availability.
Radiofrequency ablation uses a percutaneously placed emitting alternating current, which generates friction and high temperatures and results in coagulative necrosis within the target lesion . Radiofrequency ablation has been used in patients
with inoperable cancer who have peripheral tumours that are less than 3.5 cm in size, and occasionally in
apalliative setting.
The procedure is often used to spare normal functional lung tissue in the setting of reduced lung capacity.
The RAPTURE study
of 106 patients with lesions under 3.5 cm who were not suitable for combined chemoradiotherapy or resection but whounderwent radiofrequency ablation reported two year disease-free survival in 75% of patients.
More recently, a prospective trial of 65 patients with unresectable non-small cell lung carcinoma reported that percutaneous cryotherapy and
radiofrequency achieved complete ablation in lesions 3 cm and smaller in 86% and 76% of patients, respectively. Results are still pending on ongoing studies of radiofrequency ablation
versus conventional combined chemoradiotherapy, including aphase II trial that is investigating radiofrequency ablation in stage Ia of non-small cell lung carcinoma.