د. حسين محمد جمعة
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2011
DIAGNOSIS AND TREATMENT OFSYNCOPE
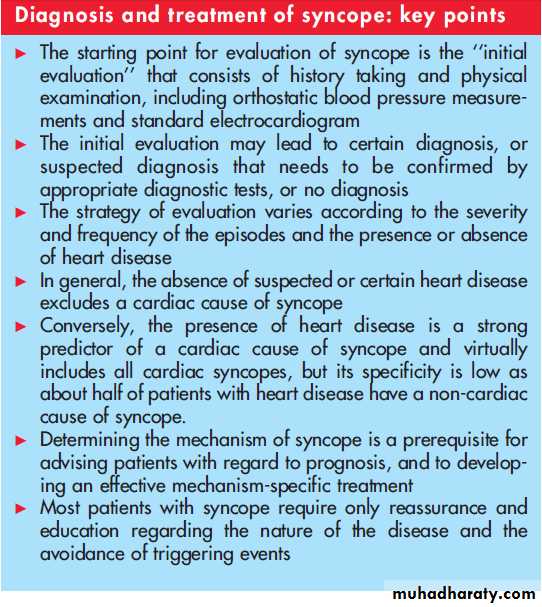
Heart 2007In the evaluation of patients with syncope, the critical first step is a detailed medical history.
Adiagnostic strategy based on initial evaluation is warranted.
The importance of the initial evaluation goes well beyond its capability to make a diagnosis as it determines the most appropriate subsequent diagnostic pathways and risk evaluation.
According to the Guidelines on Syncope of the European Society of Cardiology (ESC) the ‘‘initial
evaluation’’ of a patient presenting with syncope consists of taking a careful history, and a physical
examination, including orthostatic blood pressure measurements and standard (ECG).
Three key questions should be addressed during the initial evaluation:
Is loss of consciousness attributable to syncope or not?
Differentiating true syncope from ‘‘nonsyncopal’’
conditions associated with real or apparent transient loss of consciousness is generally the first diagnostic challenge and influences the subsequent diagnostic strategy.
Are there features in the history that suggest the diagnosis? Accurate history taking alone is a key
stage and often leads to the diagnosis or may suggest the strategy of evaluation.
Is heart disease present or absent?
The absence of signs of suspected or overt heart disease virtually excludes a cardiac cause of syncope with the exception of syncope accompanied by
palpitations which could be due to paroxysmal tachycardia (especially paroxysmal supraventricular
tachycardia).
Conversely, the presence of heart disease at the initial evaluation is a strong predictor of a cardiac cause of syncope, but its specificity is low as about half of patients with heart disease have a non-cardiac cause of syncope.
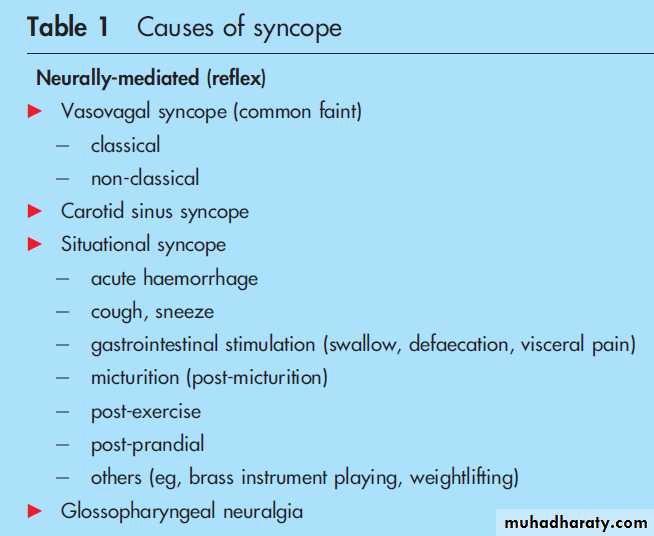
Table 1 provides the clinical classification of the principal known causes of syncope proposed by the
Task Force on Syncope of the ESC. The subdivision of syncope is based on pathophysiology as
follows:
1. ‘‘Neurally-mediated (reflex) syncope’’ refers to
areflex response that, when triggered, gives rise to
vasodilatation and/or bradycardia; however the contribution of each of these two factors to
systemic hypotension and cerebral hypoperfusion may differ considerably. The triggering events
might vary considerably in individual patients.
The ‘‘classical vasovagal syncope’’ is mediated by
emotional or orthostatic stress and can be diagnosed by history taking.
‘‘Carotid sinus syncope’’ is defined as syncope which, by history, seems to occur in close relationship to accidental mechanical manipulation of the carotid sinuses, and which can be reproduced by carotid sinus massage.
‘‘Situational syncope’’ refers to those forms of neurally-mediated syncope associated with specific
scenarios (for example, micturition, coughing, defaecating, etc).
Neurally-mediated (reflex) syncope
Often, however, neurally mediated
reflex syncopes have ‘‘non-classical’’ presentations. These forms are diagnosed by minorclinical criteria, exclusion of other causes for syncope (absence of structural heart disease) and
positive response to tilt testing or carotid sinus massage. Examples of non-classical vasovagal
syncope include episodes without clear triggering events or premonitory symptoms.
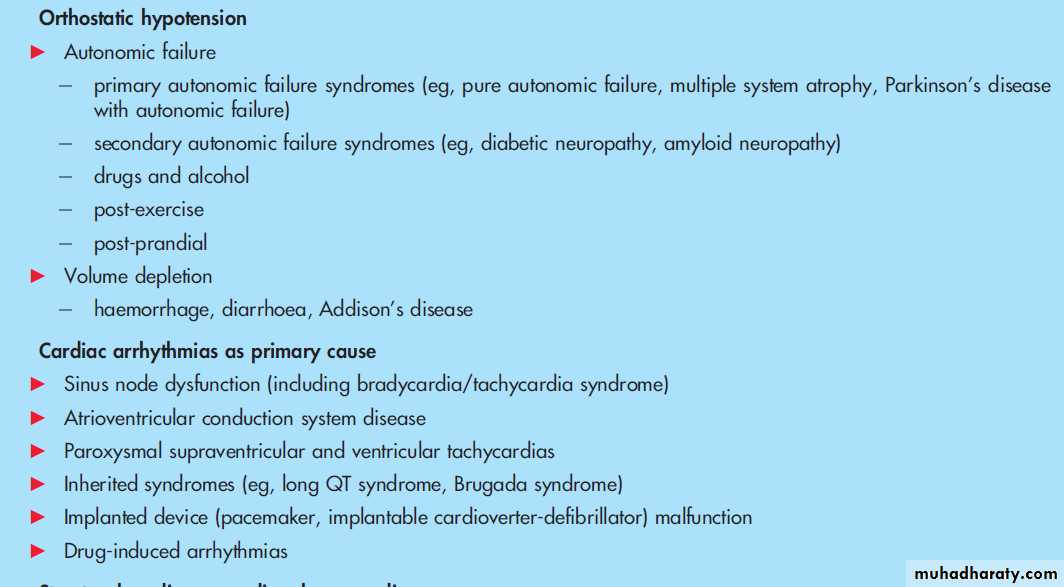
2.‘‘Orthostatic hypotension’’ refers to syncope in which the upright position (most often the
movement from sitting or lying to an upright position) causes arterial hypotension.
This occurs when the autonomic nervous system is incapacitated and fails to respond to the challenges
imposed by upright position.
A second major cause is ‘‘volume depletion’’ in which the autonomic nervous system is itself not deranged, but is unable to maintain blood pressure due to decreased
circulating volume.
Note that vasovagal syncope can also be provoked by standing (for example, soldiers fainting on parade), but these events are grouped under ‘‘neurally-mediated (reflex) syncope’’.
3.Cardiac arrhythmias’’ can cause a decrease in cardiac output, which usually occurs irrespective of
circulatory demands.
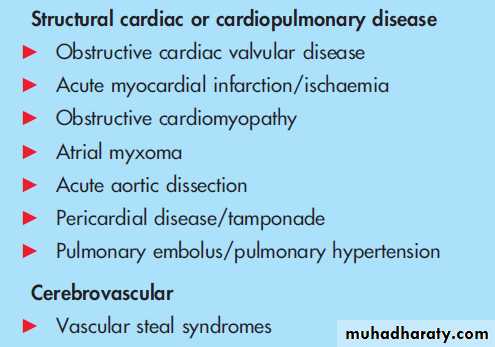
4.‘‘Structural heart disease’’ can cause syncope when circulatory demands outweigh the impaired
ability of the heart to increase its output.
5.‘‘Steal’’ syndromes are rare, but can cause syncope when blood supply is diverted from the brain to another organ (the most common example is the so-called ‘‘subclavian steal syndrome’’).
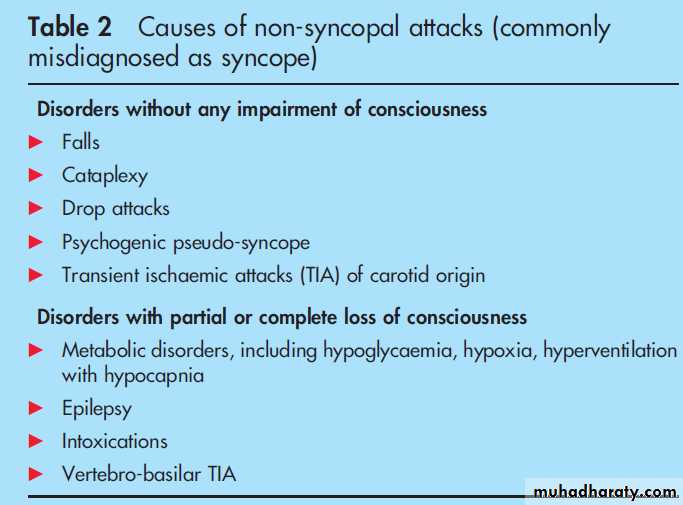
Table 2 lists the most common conditions misdiagnosed as causes of syncope. Such a differentiation is crucial because the clinician is usually confronted with patients in whom sudden loss of consciousness has been provoked by causes not associated with decreased cerebral blood flow such as seizure
and/or conversion reaction.
Several disorders may resemble syncope in two different ways. In some, consciousness is truly
lost, but the mechanism is not related to cerebral hypoperfusion:
epilepsy, metabolic disorders (including hypoxia and
hypoglycaemia) and intoxications. In several other disorders, consciousness is only apparently lost; this is the case in ‘‘psychogenic pseudo-syncope’’, cataplexy and drop attacks.
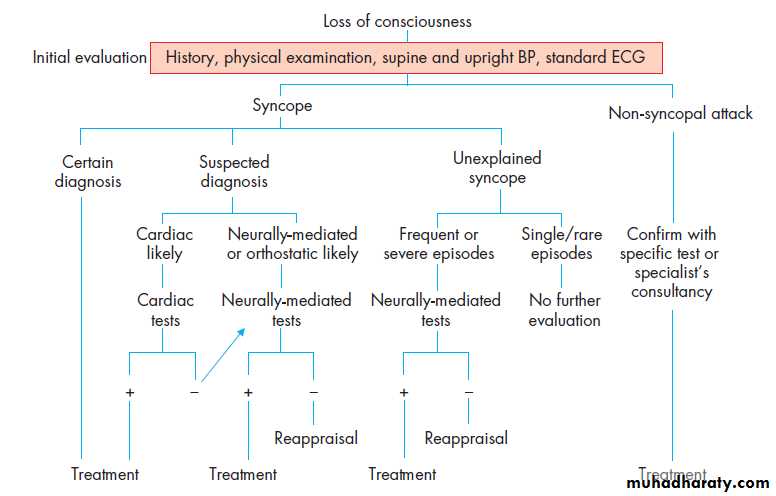
The initial evaluation may lead to certain or suspected
diagnosis or no diagnosis (here termed as unexplained syncope) (fig 1).
CERTAIN DIAGNOSIS
Initial evaluation may lead to a certain diagnosis based on symptoms, physical signs, or ECG findings. Under suchcircumstances, no further evaluation may be needed and
treatment, if any, can be planned. The results of the initial evaluation are most often diagnostic of the cause of syncope in the following situations:
Classical vasovagal syncope is diagnosed if precipitating events such as fear, severe pain, emotional distress, instrumentation or prolonged standing are associated with typical prodromal symptoms.
Situational syncope is diagnosed if syncope occurs during or immediately after urination, defaecation, cough or swallowing.
Orthostatic syncope is diagnosed when there is documentation of orthostatic hypotension (defined as a decrease in systolic blood pressure >20 mm Hg or a decrease of systolic blood pressure to ,90 mm Hg) associated with syncope or presyncope.
Cardiac ischaemia-related syncope is diagnosed when symptoms are present with ECG evidence of acute ischaemia with or without myocardial infarction. However, in this case further determination of the specific ischaemia-induced aetiology may be necessary (for example, neurally-mediated hypotension,tachyarrhythmia, ischaemia-induced atrioventricular block, etc).
Arrhythmia-related syncope is diagnosed by ECG when there is:
– sinus bradycardia <40 beats/min or repetitive sinoatrial blocks or sinus pauses >3 s in the absence of medications.known to have negative chronotropic effect
– second degree Mobitz II or third degree atrioventricular block
– alternating left and right bundle branch block
– rapid paroxysmal supraventricular tachycardia or ventricular tachycardia
– pacemaker malfunction with cardiac pauses
However, it is important to bear in mind that syncope is often multifactorial. The latter is especially true in older individuals.
Thus, careful consideration should be given to multiple potential interacting factors (for example, diuretics in older patients already susceptible to orthostatic hypotension, myocardial ischaemia in the setting of moderate aortic stenosis, etc).
SUSPECTED DIAGNOSIS
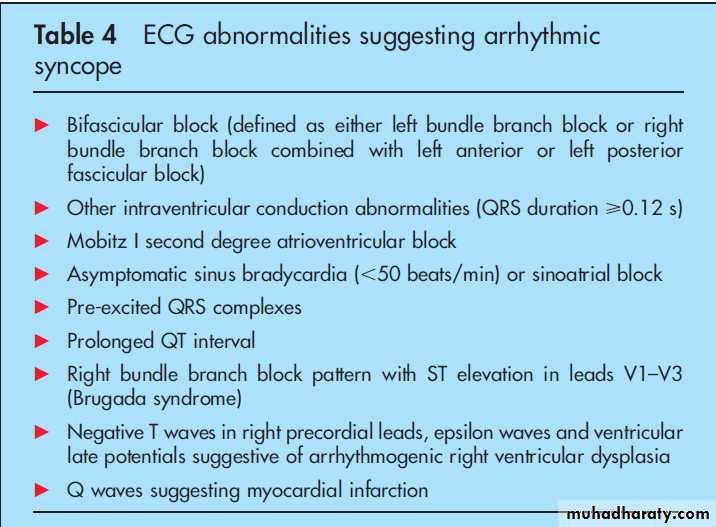
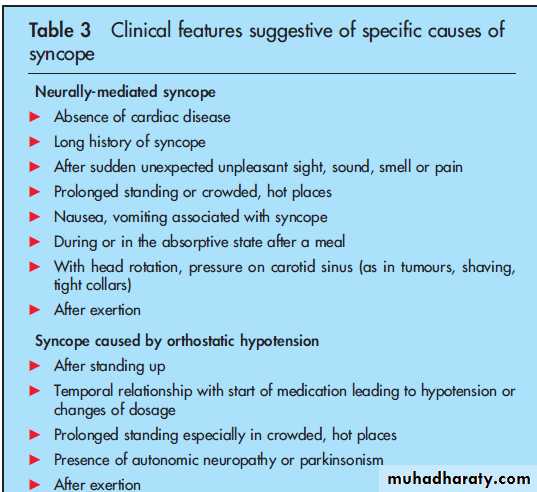
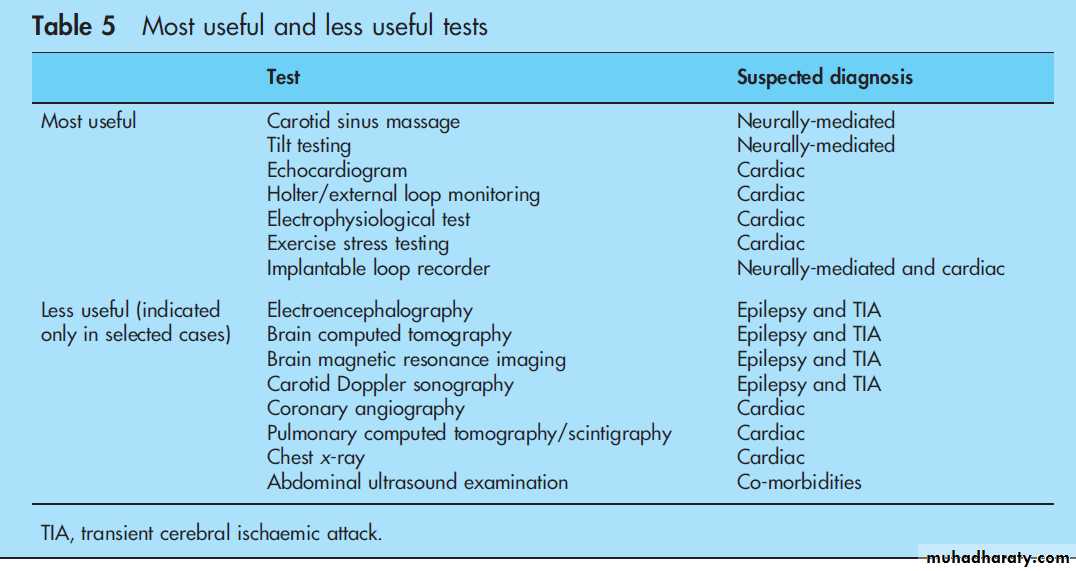
Commonly, the initial evaluation leads to a suspected diagnosis, when one or more of the features listed in tables 3 and 4 are present, which needs to be confirmed by tests (table 5).The presence of suspected or certain heart disease is
associated with a higher risk of arrhythmias and mortality at one year. In these patients, cardiac evaluation
(echocardiography, stress testing, electrophysiological study and prolonged ECG monitoring including loop recorder) is recommended.
If cardiac evaluation does not show evidence of arrhythmia as a cause of syncope, evaluation for neurally-mediated syndromes is recommended only in those with recurrent or severe syncope. It includes tilt testing, carotid sinus massage, and ECG monitoring, and often further requires implantation of an implantable loop recorder (ILR).
The majority of patients with single or rare episodes in this setting have a high likelihood of neurally-mediated syncope and tests for confirmation are usually not necessary.
Neurologic disease may cause transient loss of consciousness (for example, certain seizures), but is almost never the cause of syncope. Thus, neurologic testing may be needed to distinguish seizures from syncope in some patients, but these should not be
considered as essential elements in the evaluation of the basis of true syncope.
The possible contribution of electroencephalography
(EEG), computed tomography and magnetic resonance imaging of the brain is to disclose abnormalities caused by epilepsy; there are no specific EEG findings for any loss of consciousness other than epilepsy.Accordingly, several studies conclusively showed that EEG monitoring was of little use in unselected patients with syncope.
Thus, EEG is not recommended for patients in whom syncope is the most likely cause for a transient loss of consciousness.
Carotid TIAs are not accompanied by loss of consciousness.
Therefore, carotid Doppler ultrasonography is not required in patients with syncope.
If the diagnosis is confirmed, treatment may be initiated; if not, a reappraisal process may be useful.
UNKNOWN DIAGNOSIS
The cause of syncope may remain unexplained after the initial evaluation. The strategy varies according to the severity and frequency of the episodes (fig 1). For patients with unexplained syncope the most likely diagnosis is neurally-mediated for which the appropriate tests are described above. The majority ofpatients with single or rare episodes in this category probably have neurally-mediated syncope and tests for confirmation are usually not necessary.
REAPPRAISAL
Once the evaluation is completed and the cause of syncope is undetermined, reappraisal of the work-up is needed since subtle findings or new historical information may change the strategy.
Reappraisal may consist of obtaining additional details of history and re-examining the patient, placement of an ILR if not previously undertaken, as well as review of the entire workup.
If new clues to possible cardiac or neurological disease are yielded, further cardiac and neurological assessment are recommended. In these circumstances, consultation with appropriate specialists may be useful. Psychiatric assessment is recommended in patients with frequent recurrent syncope
who have many other somatic complaints and initial evaluation raises concerns about stress, anxiety and possible other psychiatric disorders.
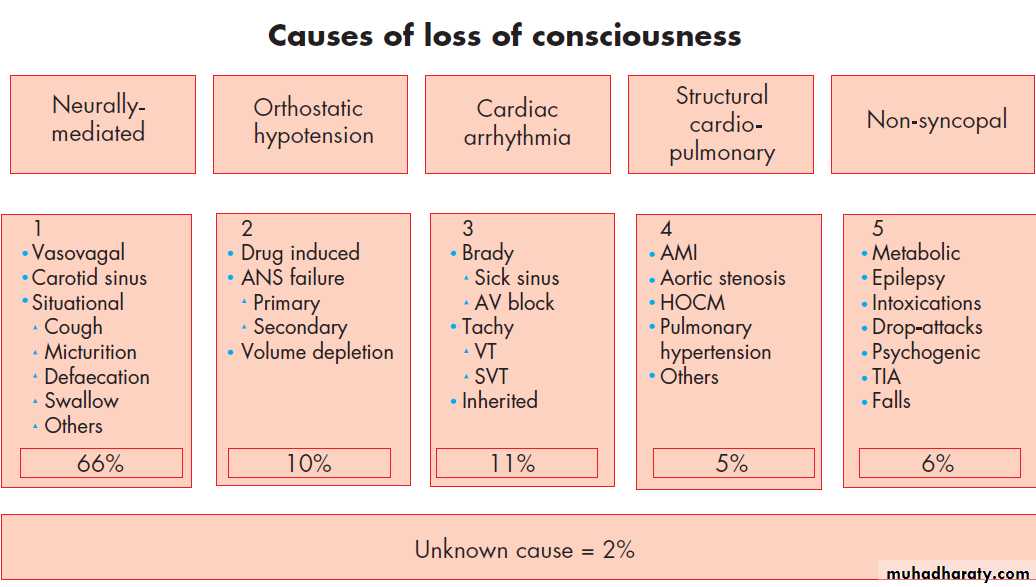
DIAGNOSTIC YIELD AND PREVALENCE OF CAUSES OF SYNCOPE
The EGSYS study was a prospective systematic evaluation—based on strict adherence to the Guidelines on Syncope of the ESC—of consecutive patients referred for syncope to the emergency departments of several general hospitals.The EGSYS study was aimed at assessing the management of syncope as recently defined by ESC guidelines.
The results of this study probably assess the current standard for the management of syncope.
A definite diagnosis was established
in 98% (unexplained in 2%): neurally-mediated syncope accounted for 66% of diagnoses, orthostatic hypotension 10%, primary arrhythmias 11%, structural cardiac or cardiopulmonary disease 5%, and non-syncopal attacks 6% (fig 2).
The initial evaluation established a diagnosis in 50% of cases. Hospitalisation for the management of syncope was appropriate in 25% and was required for other reasons in a further 13% of cases.
The median in-hospital stay was 5.5 days (interquartile range 3–9 days).
Apart from the initial evaluation, a mean (SD)of 1.9 (1.1) appropriate tests per patient were performed in 193 patients and led to a final diagnosis in 182 of these (94%).
This study showed that a guideline-based standardised method of syncope management improved the overall diagnostic yield and reduced hospital admissions, resource consumption and overall costs compared to previous population-based studies.
TREATMENT
Need for mechanism-guided specific treatment
A major issue in the use of diagnostic tests is that syncope is atransient symptom and not a disease. Typically patients are asymptomatic at the time of evaluation and the opportunity to capture
a spontaneous event during diagnostic testing is rare.
This type of reasoning leads, of necessity, to uncertainty in establishing a cause.
Establishing the basis for syncope (that is, determining the ‘‘diagnosis’’) is a prerequisite for advising
patients with regard to prognosis, and to developing an
effective treatment strategy.
However, arriving at the diagnosis can be difficult, and is often marked by the undertaking of costly and often useless diagnostic procedures.
The ultimate goal of diagnostic testing is to establish a sufficiently strong correlation between syncope and detected abnormalities to permit both an assessment of prognosis and initiation of an appropriate treatment plan. Knowledge of what occurs during a
spontaneous syncopal episode is ideally the gold standard for syncope evaluation.
For this reason it is likely that ILRs will become increasingly important in the assessment of the
syncope patient, and their use will increasingly be appropriate instead of, or before, many current conventional investigations.
This early ILR approach implies the need for a careful initial risk stratification in order to exclude from such a strategy patients with potential life threatening conditions.
Neurally-mediated (reflex) syncope. Patients who seek medical advice after having experienced a
vasovagal faint require reassurance and education regarding the nature of the disease and the avoidance of triggering events.
In general, education and reassurance are sufficient for most patients. Modification or discontinuation of hypotensive drug treatment for concomitant conditions and avoidance of triggering situations are other first line measures for the prevention of syncope recurrences.
Treatment is not necessary for patients who have sustained a single syncope and are not having syncope in a high risk setting.
Additional treatment may be necessary in high risk or high frequency settings when:
1.syncope is very frequent—alters the quality of Life
2. syncope is recurrent and unpredictable (absence of premonitory symptoms) and exposes patients to ‘‘high risk’’ of trauma
3. syncope occurs during the prosecution of a ‘‘high risk’’activity (for example, driving, machine operation, flying,competitive athletics, etc).
Non-pharmacological ‘‘physical’’ treatments are emerging as a new front line treatment of vasovagal syncope. In highly motivated patients with recurrent vasovagal symptoms, the prescription of progressively prolonged periods of enforced upright posture (so-called ‘‘tilt-training’’) may reduce syncope
recurrence. However, this treatment is hampered by the low compliance of the patients in continuing the training programme for a long period.
Two recent clinical trials have shown that isometric counterpressure manoeuvres of the legs
(leg crossing), or of the arms (hand grip and arm tensing), are able to induce a significant blood pressure increase during the phase of impending vasovagal syncope, which allow the patient
to avoid or delay losing consciousness in most cases.
Many drugs have been used in the treatment of vasovagal syncope (b-blockers, disopyramide, scopolamine, clonidine, theophylline, fludrocortisone, ephedrine, etilefrine, midodrine, clonidine, serotonin reuptake inhibitors, etc).
In general, while the results have been satisfactory in uncontrolled trials or short-term controlled trials, long-term placebo-controlled prospective trials have failed to show any benefit of the active drug over placebo.
B-adrenergic blocking drugs have failed to be
effective in five of six long-term follow-up controlled studies. Vasoconstrictor drugs are potentially more effective in orthostatic hypotension caused by autonomic dysfunction than in neurally-mediated syncope.Etilefrine proved to be ineffective.
To date there are insufficient data to support the use of any other pharmacological treatment for vasovagal syncope.
The role of cardiac pacing for vasovagal syncope is not yet established. In unselected tilt-positive patients, pacing for vasovagal syncope has produced controversial results.
Pooling together the results of five randomised controlled trials syncope recurred in 21% of the paced patients and in 44% of un-paced patients.
Specifically, the efficacy of pacemaker therapy was questioned after two recent controlled trials failed
to prove superiority of cardiac pacing over placebo of unselected patients with positive tilt testing.
It seems that pacing therapy might be effective in some but not in all patients.
This is not surprising if we consider that pacing is probably efficacious for asystolic reflex but has no role in combatting hypotension which is frequently the dominant reflex in neurally-mediated syncope.
A recent study using the ILR as reference standard showed that only about half of the patients
had an asystolic pause recorded at the time of spontaneous syncope.
A new strategy of delaying treatment until ILR documentation of the mechanism of syncope with cardiac pacing, limited to those patients who had asystole at the time of syncope, proved to be very effective by reducing syncopal recurrence rate of 90% to an absolute value of 5% at one year.
It must be underlined that the decision to implant a pacemaker needs to be kept in the clinical context of a benign condition which frequently affects young patients.
Thus, cardiac pacing should be limited as a last resort choice to a very selected small proportion of patients affected by severe vasovagal syncope.
Cardiac pacing appears to be beneficial in the carotid sinus syndrome and, although only one relatively small randomised controlled trial has been undertaken, pacing is acknowledged to
be the treatment of choice when bradycardia has been documented.
Single chamber atrial pacing is not appropriate for vasovagal syncope, and dual-chamber pacing is generally preferred over single chamber ventricular pacing.
Orthostatic hypotension
Drug-induced autonomic failure is probably the most frequent cause of orthostatic hypotension.The principal treatment strategy is elimination of the offending agents, mainly diuretics and vasodilators. Alcohol is also commonly associated with
orthostatic intolerance.
Additional treatment principles, used alone or in combination,are appropriate for consideration on an individual patient basis:
1. chronic expansion of intravascular volume by encouraging ahigher than normal salt intake and fluid intake of 2–2.5 litres per day.
2. fludrocortisone in low dose (0.1–0.2 mg per day)
3. raising the head of the bed on blocks to permit gravitational exposure during sleep
4. reduce vascular volume into which gravitation induced pooling occurs by use of abdominal binders and/or waist height support stockings or garments
5. introduce physical counter manoeuvres such as leg crossing, gripping or squatting
6. use of drugs which increase peripheral resistance (midodrine 5–15 mg three times daily).Cardiac arrhythmias as primary cause Syncope caused by cardiac arrhythmias must receive treatment
appropriate to the cause in all patients in whom it is lifethreatening and when there is a high risk of injury.
Treatment may be warranted when:
• the culprit arrhythmia has not been demonstrated conclusively, but a diagnosis of life-threatening arrhythmia is presumed from surrogate data
• the culprit arrhythmia has been identified but is not life threatening or presenting a high risk of injury.
Cardiac pacing, implantable cardioverter-defibrillators, and catheter ablation are the usual treatments of syncope caused by cardiac arrhythmias, depending on the mechanism of syncope.
Structural cardiac or cardiopulmonary disease
Treatment is best directed at amelioration of the specific structural lesion or its consequences.
Figure 1 Flow diagram outlining an approach to the evaluation of loss of consciousness based on the initial evaluation, proposed by the Task Force on
Syncope of the European Society of Cardiology1 2. Differentiating true syncope from other ‘‘non-syncopal’’ conditions associated with real or apparent transient loss of consciousness is generally the first diagnostic step and influences the subsequent diagnostic strategy. For the classification of syncope refer to table 1 and for the classification of non-syncopal attack refer to table 2. The conditions in which the results of the initial evaluation are diagnostic of the cause of syncope and no further evaluation is required are listed as recommendations in the section ‘‘The diagnostic strategy based on the initial evaluation’’. The features which suggest a cardiac or a neurally-mediated cause of syncope are listed in tables 3 and 4. Among cardiac investigations, echocardiography, prolonged electrocardiographic monitoring, stress test, electrophysiological study and implantable loop recorder are most useful. Among neurally-mediated investigations, tilt test, carotid sinus massage and implantable loop recorder are most useful. When a cardiac diagnosis cannot be confirmed, neurally-mediated tests are usually performed. Once the evaluation, as outlined, is completed and no cause of syncope is determined, reappraisal of the work-up may be needed. BP, blood pressure; ECG, electrocardiogram.
Evidence level
Differential diagnosis/symptom prevalence study1a
Systematic review of prospective cohort studies
1b
Prospective cohort study with good follow up
1c
All or none case series
2a
Systematic review of 2b and better studies
2b
Retrospective cohort study, or poor follow up
2c
Ecological studies
3a
Systematic review of 3b and better studies
3b
Non-consecutive cohort study, or very limited population
4
Case series or superseded reference standards
5
Expert opinion without explicit critical appraisal, or based on physiology, bench research, or "first principles"
• Syncope
A history of syncope precipitated by exercise raises the possibility of hypertrophic cardiomyopathy, Brugada’s syndrome, or pre-excitation disorders such as congenital long QT syndrome and arrhythmogenic right ventricular dysplasia, which can be precipitated by a sympathetic surge.
A brief or absent pre-syncopal period may be associated with syncope of a cardiac nature, especially an arrhythmia. Here, an average length of pre-syncopal symptoms of three seconds has been reported.2
Syncope associated with neurocardiogenic (vasovagal) syncope has been reported to last an average of two and a half minutes.2 3 Vasovagal syncope is more likely to be associated with palpitations, blurred vision, and feelings of nausea, warmth, and light headedness prior to the syncope episode, and patients are more likely to have had previous syncopal episodes.
Lucidity post event is the most important feature in the history that may point to an anoxic seizure rather than neurogenic seizure activity. Whilst confusion may be present immediately after true syncope, this should not last for more than several minutes.3
Sudden onset syncope without pre-warning symptoms may be indicative of syncope of cardiac origin and must be taken seriously. (Evidence Level 1b)
The cardiovascular system should be specifically examined looking for a postural drop (a fall of 20 mm Hg or more, or a fall to <90 mm Hg after standing for at least three minutes), a displaced apex, valve lesions, the presence of cardiac failure, carotid bruits, and a ventricular pause of greater than three seconds precipitated by carotid sinus massage.
A postural drop should always be looked for in patients presenting with syncope. A drop of 20 mm Hg or more is significant and may need to be treated. (Evidence Level 5) It is important to identify features in the history that may point to neurogenic seizure activity, the most important of which is the presence of a post-ictal phase. Whilst confusion may be present immediately after true syncope, this should not last for more than several minutes.3
It is important to identify features in the history that may point to neurogenic seizure activity, the most important of which is the presence of a post-ictal phase. Whilst confusion may be present immediately after true syncope, this should not last for more than several minutes. It is important to identify features in the history that may point to neurogenic seizure activity, the most important of which is the presence of a post-ictal phase. Whilst confusion may be present immediately after true syncope, this should not last for more than several minutes.
It is important to identify features in the history that may point to neurogenic seizure activity, the most important of which is the presence of a post-ictal phase. Whilst confusion may be present immediately after true syncope, this should not last for more than several minutes. It is important to identify features in the history that may point to neurogenic seizure activity, the most important of which is the presence of a post-ictal phase. Whilst confusion may be present immediately after true syncope, this should not last for more than several minutes.3
Other discriminators such as tonic-clonic activity, incontinence, and tongue biting may help, however, do not in isolation rule out true syncope if a period of cerebral anoxia has occurred.
Seizure activity that is thought to be neurogenic should not be classified as syncope.
Syncope has been defined as a transient loss of consciousness followed by spontaneous recovery.3 Most patients do not remember their syncopal episode. Some patients can recall the event as it may terminate just prior to the loss of consciousness ("pre-syncope").
The presence of pre-syncopal symptoms such as nausea, diaphoresis, dizziness, and a feeling of warmth may suggest vasovagal syncope.
Precipitant factors, ie micturition and coughing, may suggest situational syncope, and a positional aspect, ie syncope precipitated by rising from a sitting position, may suggest orthostatic syncope. Other important symptoms prior to the syncopal event include chest pain, sudden onset of headache or dyspnoea, palpitations, back pain, or focal neurological deficits. The presence of any of these may suggest an alternative serious cause.
A witness history should be sought and a drug history taken to identify the use of antihypertensive or other cardiac medication, and drugs that cause bradycardia, hypotension, or
prolong the QT interval (ie erythromycin, quinine, and major tranquillisers). Nitrate use immediately prior to the syncopal episode is associated with GTN syncope. A menstrual history should also be taken in women of childbearing age as syncope is not an uncommon presentation of ectopic pregnancy. In addition neurocardiogenic syncope is relatively common in early pregnancy.
Some patients presenting with syncope may be under the influence of alcohol or recreational drugs making a thorough history difficult. Whilst these substances may lead to collapse, syncope is unlikely to occur as a direct consequence of either alcohol or recreational drugs. These patients should be assessed at the time of presentation with a thorough examination and ECG, however, subsequent assessment of risk and additional investigations may need to wait until the patient is more compliant.
Finally, a family history of cardiac disease or sudden unexplained family death or history of syncope precipitated by exercise raise the possibility of hypertrophic cardiomyopathy, Brugada's syndrome, or pre-excitation disorders such as congenital long QT syndrome and arrhythmogenic right ventricular dysplasia, which can be precipitated by a sympathetic surge.
Key learning point 2
A prolonged post-ictal phase is the best discriminator between a true syncopal event with an anoxic seizure and a likely neurological seizure. (Evidence Level 5)Key learning point 6
The OESIL score defined four additive risk factors associated with increasing one year mortality. (Level 1b)The most recent and largest derivation and validation study on syncope risk stratification to date was performed by Quinn et al. They derived a clinical decision rule (the San Francisco Syncope Rule) using five risk factors:
Abnormal ECG
Anaemia (haematocrit <30%)
A complaint of shortness of breath
Systolic hypotension (<90 mm Hg)
A history of congestive cardiac failure.
This is the only study that has looked at short term adverse outcomes relevant to emergency practice, however two of the risk markers chosen in the rule would usually necessitate immediate hospital admission: systolic blood pressure less than 90 mm Hg and a haematocrit of less than 30%.
The researchers also derived their rule using seven day outcome but attempted to validate it using one month outcome.8 Subsequent attempts to externally validate it have failed.
Key learning point 7
The San Francisco Syncope Rule was the first large study to attempt to derive characteristics associated with adverse short term syncope outcome. It has not externally validated well. (Evidence Level 1b)All guidelines discuss history, examination, and investigation of syncopal patients, however, only the American College of Emergency Physicians (ACEP) guidelines have focused directly on Emergency Department investigations and management.9 These suggest admission for patients with:
A history of congestive heart failure or ventricular arrhythmias .Associated chest pain or other symptoms compatible with acute coronary syndrome
Evidence of significant congestive heart failure or valvular heart disease on physical examination
ECG findings of ischaemia, arrhythmias, prolonged QT interval, or bundle branch block.
The ACEP guidelines also suggest that admission should be considered for patients with syncope who:
Are older than 60 years.
Have a history of coronary artery or congenital heart disease.
Have a family history of unexpected sudden death
Are younger patients presenting with exertional syncope without an obvious benign aetiology.
All guidelines discuss history, examination, and investigation of syncopal patients, however, only the American College of Emergency Physicians (ACEP) guidelines have focused directly on Emergency Department investigations and management.9
These suggest admission for patients with:
A history of congestive heart failure or ventricular arrhythmias.Associated chest pain or other symptoms compatible with acute coronary syndrome.
Evidence of significant congestive. heart failure or valvular heart disease on physical examination
ECG findings of ischaemia, arrhythmias, prolonged QT interval, or bundle branch block.
The ACEP guidelines also suggest that admission should be considered for patients with syncope who:
Are older than 60 years
Have a history of coronary artery or congenital heart disease.
Have a family history of unexpected sudden death
Are younger patients presenting with exertional syncope without an obvious benign aetiology.
Presently it is unclear whether either the application of guidelines to syncope management, or the practice of admitting patients with syncope to hospital has any impact on patient outcome. No such benefits have ever been demonstrated.
Key learning point 8
The American College of Emergency Physician guidelines are the most relevant guidelines to Emergency Department practice and should form the basis of any syncope guidelines for use in UK EDs (Level 1a).
The commonest ECG abnormality seen in arrhythmogenic right ventricular dysplasia is T wave inversion in leads V1 to V3. This is a non-specific finding, and may be considered a normal variant in right bundle branch block (RBBB), women, and children under 12 years old. The epsilon wave is found in about 50% of those with arrhythmogenic right ventricular dysplasia. This is a terminal notch in the QRS complex due to slowed intraventricular conduction.
Key learning point 9
Whilst an ECG may be normal in most patients with syncope it MUST be performed in every syncopal patient who presents to the Emergency Department. (Evidence Level 1b)The current European Society of Cardiology syncope guidelines17 document the ECG abnormalities that increase the risk of a syncope secondary to arrhythmia as:
Bifascicular block
QRS >0.12 seconds
Mobitz second degree AV block
Sinus bradycardia (<50 bpm), sinoatrial block, sinus pause >3 seconds
Pre-excited QRS complexes
Prolonged QT interval
Signs of Brugada's syndrome (right bundle branch block, ST segment elevation in leads V1 to V3)
Arrhythmogenic right ventricular dysplasia (epsilon wave or localised QRS >110 msecs in V1-V3, or inverted T waves in V2 and V3 without right bundle branch block)
Q waves suggesting myocardial infarction.
It is suggested that patients with these abnormalities should be admitted for monitoring and be investigated for arrhythmic syncope. There is no evidence that any of these findings are associated with an early adverse outcome and no studies have been powered to assess the prognostic value of individual ECG abnormalities.
For patients considered at risk of having an arrhythmic cause for their syncope, longer ECG assessment in the form of 24 hour tape monitoring and loop recording may be considered on either an inpatient or outpatient basis. These investigations have good sensitivity, however, patients suffering arrhythmias may not demonstrate abnormalities during the monitoring period. Whilst arrhythmias demonstrated during routine Emergency Department monitoring are obviously diagnostic, more prolonged monitoring does not form part of Emergency Department investigation.
• Syncope
• Our Emergency Department patient is moved into the resuscitation room and external pacing pads are placed onto his chest in case of further episodes of asystole. He is transferred to the Coronary Care Unit where a temporary pacing wire is placed prior to a formal definitive implantable pacemaker. He is discharged home two days after his initial attendance.The San Francisco Syncope Rule is a clinical decision rule derived using five risk factors: abnormal ECG, anaemia (haematocrit <30%), a complaint of shortness of breath, systolic hypotension (<90 mm Hg), and a history of congestive cardiac failure.