The Pathogenesis of Rheumatoid Arthritis
N Engl J Med 2011;365:2205-19.د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
Rheumatoid arthritis is a common autoimmune disease that is associated with progressive disability, systemic complications, early death, and socioeconomic costs.
The cause of rheumatoid arthritis is unknown, and the prognosis is guarded. However, advances in understanding the pathogenesis of the disease have fostered the development of new therapeutics, with improved outcomes.
The current treatment strategy, which reflects this progress, is to initiate aggressive therapy soon after diagnosis and to escalate the therapy, guided
by an assessment of disease activity, in pursuit of clinical remission.
However, several unmet needs remain. Current conventional and biologic disease modifying therapies sometimes fail or produce only partial responses. Reliable predictive biomarkers of prognosis, therapeutic response, and toxicity are lacking.
Sustained remission is rarely achieved and requires ongoing pharmacologic therapy.
The mortality rate is higher among patients with rheumatoid arthritis than among healthy persons, and cardiovascular and other systemic complications remain amajor challenge.
Molecular remission and the capacity to reestablish immunologic tolerance remain elusive. Elucidation of the pathogenic mechanisms that initiate and perpetuate rheumatoid arthritis offers the promise of progress in each of these domains. Rheumatoid arthritis is predominantly classified on the basis of the clinical phenotype.
We believe it is important to make the transition to a new molecular taxonomy that defines discrete disease subgroups with distinct prognostic and therapeutic significance.
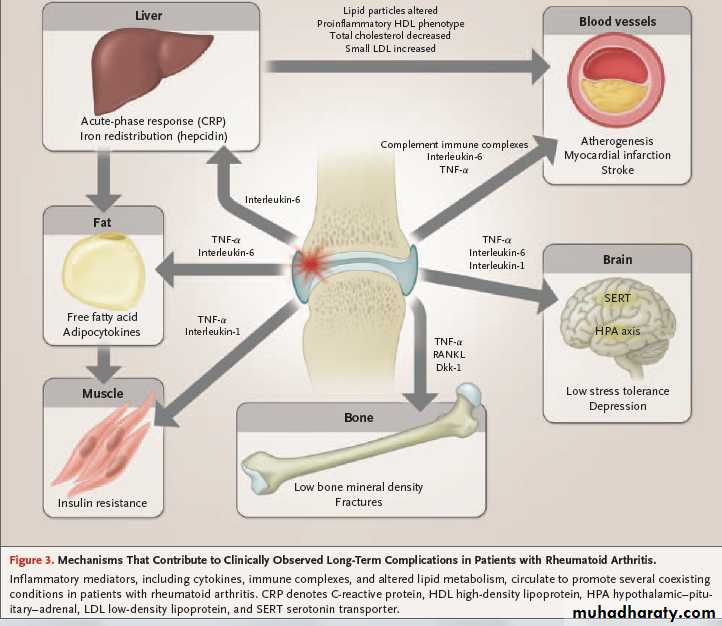
Rheumatoid arthritis is characterized by synovial inflammation and hyperplasia (“swelling”), autoantibody production (rheumatoid factor and anti–citrullinated protein antibody [ACPA]), cartilage and bone destruction (“deformity”), and systemic features, including cardiovascular, pulmonary, psychological, and skeletal disorders. These clinical features pose critical mechanistic questions: What genetic environmental interactions must occur to facilitate autoimmunity a priori, and why does this beget articular localization?
Why does synovial inflammation perpetuate?
What drives local destruction leading to joint dysfunction?
Why does rheumatoid arthritis cause systemic illness?
We herein summarize key pathogenetic advances informing these issues.
The pathogenetic advances described herein have
paralleled the introduction of new, effective therapiesand remarkable improvement in clinical
outcomes. Severe disease manifestations, such as
vasculitis, nodule formation, scleritis, and amyloidosis,
that are associated with persistent, uncontrolled
inflammation have become rare.
A rich pipeline of biologic and small-molecule agents, and of potential clinical biomarkers, exists that will add to our therapeutic armamentarium. In
time, this should render remission achievable in increasing numbers of patients.
However, much remains to be resolved. We need to understand the factors that lead to loss of tolerance and that cause localization of inflammation
in the joint. We need to find ways to promote immunologic resolution or homeostasis and repair of damaged joints.
We must elucidate the mechanisms driving the various systemic disorders that contribute substantially to reductions in the quality and length of life. Ultimately, we must strive to develop curative and preventive
therapeutics that will transform the notion of
rheumatoid arthritis as a chronic disease.