Investigating asthma symptoms in primary care
BMJ 25 April 2012د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
Even when dyspnoea is accompanied by a history of wheeze, use of spirometry and related tests is needed before making a diagnosis of asthma.
A 36 year old man presents with a six to nine month history of exercise related dyspnoea and chest tightness, especially during
football training. It does not restrict him badly and does not occur every time he exercises. It usually resolves after about 15 minutes of rest, and he can resume exercising.
A friend offered him salbutamol for relief, and it definitely improved his symptoms. He has a history of childhood wheeze with upper respiratory tract infection but never required regular inhalers and seemed to be “cured” by about age 10. There is no family history of asthma. He had hay fever as a teenager, and doesn’t think he has any allergies now. He smoked 10–15 cigarettes aday from age 18 years until age 33. Clinical examination is unremarkable, and his body mass index is in the normal range at 23.4.
What are the likely diagnoses?
Asthma is a common condition, occurring in 10–12% of adults in most Western countries and 15–20% of children depending on definition. Most children with intermittent or infrequent viral-associated or episodic asthma improve through the preschool and early school years.
Those who are atopic and have airway hyper-responsiveness are much more likely to have
persistent asthma, which may be quiescent through adolescence but has the potential to recur in adult life. It is essential to demonstrate the physiological features of asthma and to assess its severity, rather than assume that recurrent breathlessness is due to asthma. Treatment without a definite diagnosis risksunnecessary side effects and costs and may fail to identify and address the real issue.
This history may sound “classic” for asthma, but it is crucial to appraise exercise related symptoms carefully as several other important causes of exertional dyspnoea should be considered.• Anxiety and hyperventilation may be accompanied by lightheadedness, tingling extremities, and air hunger.
• Lack of fitness may be associated with prominent leg fatigue and tiredness, absence of wheeze or cough, rapid settling of symptoms with cessation of exercise but no definite benefit from bronchodilator, plus lack of other spontaneous symptoms to suggest asthma.
• Exercise induced bronchoconstriction is reported in 70-80% of people with untreated asthma. It typically causes chest tightness, wheeze or cough, and dyspnoea, with airflow obstruction that peaks 5–10 minutes after maximal exercise.
This responds promptly to a short acting β agonist or
resolves spontaneously at rest over 30–60 minutes.
• Vocal cord dysfunction is characterised by dyspnoea often accompanied by inspiratory stridor (often mistaken as awheeze), lack of response to short acting β agonists, normal spirometry results, and a normal response to bronchial provocation testing.
Stridor and dyspnoea may not be related to exercise, and may be associated with difficulty in phonation (of sudden onset and offset), and sometimes with a spectrum of psychosocial disorders.
Exercise induced laryngeal dysfunction is a type of vocal cord dysfunction where partial closure of the vocal cords occurs during intense exercise. Exercise induced laryngeal dysfunction is more common in highly trained female athletes, in some clinical series affecting 5–10% of subjects referred for respiratory testing during exercise.
Although symptoms and lung function abnormalities of this partial cord closure may vary, it can cause stridor and flattening of the inspiratory flow-volume curve on the spirometric trace Careful questioning is important, especially to elicit the characteristic features of stridor and hoarseness, and a poor
response to bronchodilators and preventive treatments for asthma.
Chronic obstructive pulmonary disease (COPD)
may be difficult to distinguish from asthma, especially in current or former smokersCOPD and asthma can coexist, in which case the term “mixed airways disease” or “overlap syndrome” is often used.
Longstanding asthma may evolve in adult life into a
syndrome of fixed airflow limitation with poor response to short acting β agonists. This is more prevalent with age but may be as high as 30% of all people with asthma over the age of 50.• More rarely in young adults, cardiac causes such as shunts,outflow obstruction, early coronary artery disease, and cardiomyopathy cause exertional dyspnoea. A clinical history should include questions about chest pain,lightheadedness, syncope, and palpitations Electrocardiography and echocardiography should be performed whenever there is a cardiac murmur, abnormal cardiac silhouette, or hilar vasculature on chest x ray, or
hypertension or hypotension.
If asthma is suspected, ask about triggers such as common inhaled allergens, exercise, and colds, and take an occupational history to identify triggers or potential sensitisers at work, such as timber dusts, spray paints, or baker’s flour.
What is the next investigation?
The British Guideline on the Management of Asthma now provides guidance to enable practitioners to establish the probability of asthma, by listing the clinical features that increase or reduce the probability of asthma. After a thorough historyand examination, an individual can usually be classed into one of three groups—high, intermediate, or low probability of asthma. This approach acknowledges that a firm diagnosis of asthma may take time and the observation of a pattern of symptoms and findings before a confident diagnosis is established.
As long term treatment may be required, the British Guideline on the Management of Asthma, based on a systematic review of the evidence, recommends obtaining objective support for the diagnosis of asthma, even in relatively clear cut cases.
Spirometry is the preferred option, and as the patient in this case is a former smoker, it may also screen for chronic obstructive pulmonary disease (see box 1 for indications for spirometry).
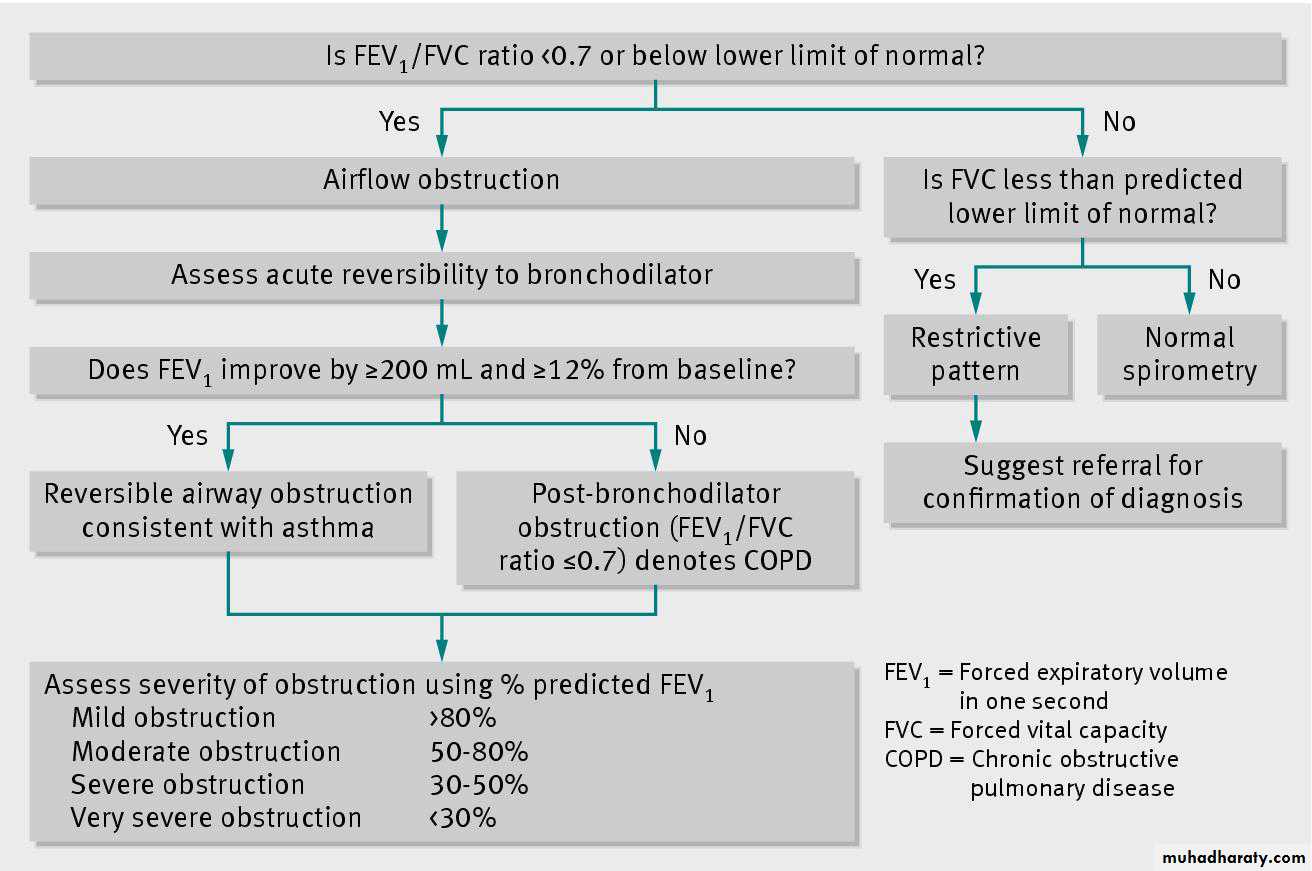
Patterns of physiological abnormalities such as restrictive or obstructive lung disease are recognisable with spirometry, but further investigations are required for confirmation of the disease process. Abnormal spirometry findings can occur in up to 24% of otherwise healthy patients due to the limitations of current reference equations, but a low FEV1/FVC ratio (even with anormal FEV1) is predictive of morbidity and mortality (see box
2 for definitions of terms).
Many compact and reliable spirometers are now available for use in general practice, with a wide choice of reference values in their inbuilt software (box 2). There are readily identifiable pitfalls, but practice and familiarity of the operator with the test will help minimise these (box 3). If spirometry is unavailable, British guidelines recommend peak flow monitoring of asthma at home to demonstrate variable lung function.
However this has more limitations compared to spirometry as a diagnostic test, since it is highly effort dependent and relatively insensitive. Patients must be trained
to put maximum effort into each blow, as poor technique with a peak flow meter may result in misleading readings. Usually two to three weeks of monitoring is all that is required to assess variability and response to bronchodilator. Diurnal variability of >15% is suggestive of asthma. A peak flow chart may assist in writing an asthma management plan, but these can be written just as effectively based on symptoms alone.
Case scenario: spirometry results and
interpretationFigure 1⇓ shows the spirometry results in this case, and fig 2⇓ provides a guide for interpretation. Spirometry reveals apre-bronchodilator FEV1/FVC ratio that is obstructive at 0.69,and substantial reversibility after administration of 400 μg salbutamol with a 19% improvement in baseline FEV1.
This reversibility is consistent with a diagnosis of asthma (a change from baseline of ≥12% and ≥200 mL represents significant reversibility). Although the absolute pre-bronchodilator FEV1 and FVC values are >80% of predicted values (which is
sometimes loosely considered to be normal), they must not be assumed to be normal until the best lung function is determined by post-bronchodilator testing.
What other tests should you do?
In this case, there is no pressing need for further tests to make a confident diagnosis of asthma. However, many young adults with this history will have normal or near normal spirometry between symptomatic periods and will require further testing,often through referral to a lung function laboratory. If spirometry is normal consider referral for bronchial provocation testingwith an indirect agent such as mannitol or hypertonic saline or with direct agents such as histamine and methacholine. Indirect tests have 75–90% sensitivity for current asthma.
Direct testing For personal with histamine or methacholine also indicates the presence of airway hyper-responsiveness, which, with a consistent history, will assist in confirming the diagnosis. Finally, specific tests
such as a eucapneic hyperventilation challenge, which mimics exercise through hyperventilation and is performed in specialist laboratories, can be particularly helpful when a conventional bicycle or treadmill exercise test does not provoke exercise induced bronchoconstriction, as is often the case in athletes and
relatively fit adults. A ≥15% fall in FEV1 with conventional exercise test or eucapneic hyperventilation challenge has 100% specificity for exercise induced bronchoconstriction.
Skin prick testing, measurement of total IgE concentration, or radioallergosorbent test (RAST) is helpful to identify atopic subjects and specific allergen sensitivity, and may help aclinician determine best advice regarding allergen avoidance.
It is important to review a chest x ray if there is uncertainty about an asthma diagnosis.
Newer tests of inflammatory phenotype (such as sputum neutrophilic or eosinophilic cell profiles) are currently being assessed for their role in diagnosis and management of asthma, particularly to assess and treat difficult asthma, but are not ready
for implementation in primary care. Specialist referral may enable dose titration of inhaled corticosteroids, based on the results of an exhaled nitric oxide test or sputum induction. These tests facilitate a targeted approach to avoid overtreatment with inhaled corticosteroids.
Case outcome
Spirometry in this case confirmed a clinical diagnosis of asthma.The patient’s level of asthma control was suboptimal based on current guidelines (easily provoked exercise related symptoms and abnormal spirometry at rest), and low dose inhaled corticosteroids were started, along with salbutamol to be taken as needed.
Correct inhaler technique was taught and reinforced
at subsequent visits. His symptoms improved with inhaled corticosteroids alone, and his spirometry normalised, showing only a 3% post-bronchodilator change in FEV1 after eight weeks of treatment. He needed a short acting β agonist very infrequently for relief of exercise related symptoms, but the need to maintain inhaled corticosteroids, return for ongoing review, and always carry a short acting β agonist was reinforced.Learning points
• Never assume recurrence of dyspnoea is due to asthma without lung function testing, even when a history of wheeze is present• Spirometry with bronchodilator testing is the investigation of choice to diagnose asthma in adults and children >10 years old
• Consider referral for bronchial provocation testing with a direct agent (such as methacholine) or indirect agent (such as mannitol or hypertonic saline) according to clinical features (such as a suggestive history but normal spirometry) and local resources.
• Longstanding asthma may evolve in adult life into a syndrome of fixed airflow limitation with poor response to short acting β agonists,
so diagnostic reversibility is not always present
• If asthma treatment is poorly effective and spirometry is normal or near normal, pursue other diagnoses and consider referral to arespiratory specialist.
Box 1: Indications for spirometry
• Assistance in the diagnosis of lung disease in patients presenting with respiratory symptoms
• Quantitative assessment of severity of airways disease
• Monitoring of therapeutic interventions and disease progression
• Preoperative assessment of risk before anaesthesia or thoracic surgery
• Screening of patients >35 years old who have ever smoked
• Screening of people before starting occupations or activities at risk (such as fire fighting, scuba diving)
Box 2: Definitions
FEV1—Forced expiratory volume in the first secondFVC—Forced vital capacity, the maximal amount of air that can be forcefully exhaled
FEV1/FVC ratio—Gives a clinically useful index of airflow limitation
The presence of ventilatory abnormality can be inferred if any combination of these is below expected values or if the flow-volume curve
shape is abnormal
% predicted—Spirometry parameters are evaluated by appropriate reference values determined from the patient’s sex, age, height, and ethnicity
Box 3: Guide to performing spirometry
• The patient is seated (for safety) with upright posture• Explain and demonstrate the manoeuvre
• Instruct the patient to inhale as deeply as possible until full (“Breathe in all the way”)
• Immediately after, instruct the patient to seal their lips tightly around the mouthpiece and exhale as rapidly as possible until no more air is able to be expelled (“Blast out” and “Keep going”)
• Always use vigorous demonstration and encouragement.
• Repeat until a minimum of three acceptable manoeuvres (see box 4) are obtained
• From these, check for repeatability (that is, the two largest FVC and FEV1 values are within 150 mL of each other), otherwise continue testing.
• The manoeuvre with the largest FEV1+FVC sum is reported for interpretation17
• To assess reversibility, repeat spirometry 15 minutes after administration of bronchodilator (such as four separate 100 μg doses of ashort acting β2 agonist (salbutamol) administered by metered dose inhaler with a spacer).Box 4 Important factors that affect acceptability of spirometry results
• Efforts must be free from cough, glottal closure, tongue occlusion, or mouth leak• Ensure maximal inhalation and exhalation (exhalation should be ≥6 seconds (≥3 seconds in children aged <10 years) or until <25 mL is exhaled in 1 second)
• Eliminate hesitation at the start of expiration (back extrapolation volume must be <150 mL or <5% of FVC)
• The device must be regularly cleaned and calibrated to the manufacturer’s specifications.