Panorama 1In Medicine
د. حسين محمد جمعهاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
• intermittent claudication, calf, thigh, or buttock pain that is exacerbated by exercise and relieved by rest.
• impotence, and
• nonhealing ulceration and infection of the extremities.
• Intermittent claudication may be companied by pallor of the extremity and paresthesias.
Abdominal aortic aneurysm typically is asymptomatic prior to the dramatic and often fatal symptoms and signs of
1-rupture, although patients may describe a
2-pulsatile abdominal mass.
3-Atheroembolism
may present with symptoms of digital necrosis,
gastrointestinal bleeding, myocardial infarction,
retinal ischemia,
cerebral infarction, and
renal failure.
Dietary and pharmacological
treatment of hypertension is associated with a decreased incidence of stroke and, to a lesser degree, atherosclerotic cardiovascular disease.There are no clinically appreciable differences in the safety profiles of the statins. However, unlike the other statins,
pravastatin is not metabolized by the cytochrome P450 system. Therefore, it is less likely to cause a problem when given concomitantly with drugs that inhibit the cytochrome P450 system (e.g., macrolide antibiotics, azole antifungals).
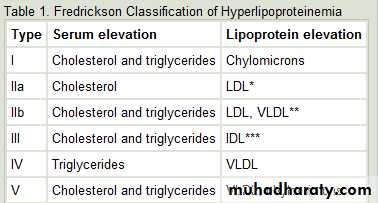
Investigating the solitary pulmonary nodule
The presence of a solitary pulmonary nodule raises the suspicion of cancer and requires carefulfurther investigation to determine whether it is malignant or benign.
BMJ 19 April 2012
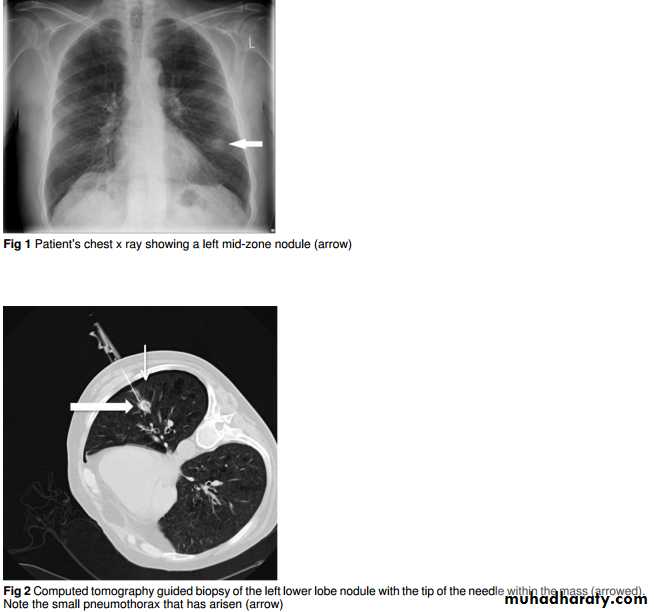
An 81 year old man presented to the emergency department with a one week history of fever, cough, and right sided chest pain. He had had a myocardial infarction in 2004 but was otherwise well. He had a 50 pack-yearsmoking history. Clinical examination was unremarkable. His chest x ray showed a left mid-zone nodule (fig 1⇓). He wastreated for a lower respiratory tract infection and referred to the lung cancer clinic with two week wait for an appointment.
Chest x ray
The chest x ray is often the first investigation where a solitary pulmonary nodule is detected. A solitary pulmonary nodule is a rounded opacity, well or poorly defined, measuring up to 3 cm in diameter. They may represent early lung cancer, andprompt detection and treatment may improve clinical outcome. However, some nodules are benign, and determining which require further investigation may be difficult.
Some common differential diagnoses are listed in box 1.
Chest x rays are readily available and have a low radiation dose.They may help identify features of the nodule that can give an indication of the cause.
Larger nodules, ill defined edges, and those growing over time are more likely to be malignant.However, a chest x ray is less sensitive at identifying these features than computed tomography. In addition most nodules are visible only once they reach 1 cm in size and hence can be easily missed.
Peripheral nodules or those lying close to or
behind other structures may be obscured from view.It has been estimated that 19% of patients with lung cancer diagnosed have solitary pulmonary nodules visible when previous chest x rays are retrospectively reviewed.False positives may occur from misinterpretation of composite shadows, vascular structures,
skin lesions, and rib abnormalities.
Comparison with previous radiographs is important as lesions that are stable over two years are unlikely to be malignant.
Other appearances such as lobar
collapse, non-resolving consolidation, and pleural effusions may be due to underlying lung cancer and require further investigation.
What should be the next investigation?
When a solitary pulmonary nodule is discovered the first step should be to make an assessment of the probability of lung cancer based on factors such as age and smoking history. The patient’s fitness and preferences for treatment also need to be taken into account. This will guide the next investigations and how the patientshould be followed up. Both clinical factors and the radiological features of the nodule affect the probability of malignancy.Computed tomography
Computed tomography of the lower neck, chest, and upper abdomen is performed to allow precise characterisation of the nodule and stage malignant disease. Computed tomography is highly sensitive for nodule detection and may identify nodulesas small as 2 mm in diameter. It allows better characterisation of features that may suggest malignancy or identify benign features such as certain patterns of calcification or fat density
Material seen in hamartomas.
Computed tomography is widely available and well tolerated, although patients have to be able
to lie flat. Its drawbacks include the substantial radiation dose of approximately 7 mSv (compared with 0.02 mSv for a chest x ray). Intravenous contrast is precluded in patients with contrast allergy or pre-existing renal impairment, which reduces the information obtainable from the scan.
Staging of malignant disease is achieved by assessing the size and location of the tumour, nodal involvement, and identifying metastatic disease. However computed tomography can less reliably determine whether mediastinal lymph nodes are involved than positron emission tomography.
Positron emission tomography
may help determine whether anodule is malignant or benign and is indicated when considering a patient for radical treatment.It combines computed tomography with the administration of radiolabelled glucose which is taken up by metabolically active tissues. The sensitivity for detection of malignant nodules is 96% with a specificity of 88%.
Positron emission tomography also has a high sensitivity for detecting metastatic disease and can determine with more certainty whether mediastinal lymph nodes are infiltrated by tumour. This allows more accurate staging and ensures that radical treatment is carried out in appropriate patients.
Its limitations include false positives from uptake of radiolabelled glucose in inflammatory lesions such as pneumonia or granulomas from old tuberculosis or sarcoid. The brain also
appears “hot,” which limits the ability to detect cerebral metastases.
Small lesions below 1 cm may be below resolution and yet could represent an early tumour or metastasis.
Like wise“cold” lesions with little metabolic activity may still be low grade tumours, and if these are not biopsied follow-up computed
tomography is usually recommended. Positron emission tomography is a limited and expensive resource that involves a prolonged scan time and high radiation dose.
Lung biopsy
There are several techniques which can be used to obtain a tissue diagnosis in those with suspected lung cancer. Current guidelines recommend biopsying the area which provides the most staging information and is least risky to the patient.Where less invasive techniques fail then options include surgical resection of nodules and mediastinoscopy to sample lymph nodes.
Bronchoscopy and endobronchial ultrasound
Flexible bronchoscopy allows examination of the central airways and biopsy of central lesions to obtain histology.
It is usually performed by respiratory physicians or thoracic surgeons.
Bronchoscopy and endobronchial ultrasound
Flexible bronchoscopy allows examination of the central airways and biopsy of central lesions to obtain histology.It is usually performed by respiratory physicians or thoracic surgeons.
The diagnostic yield for solitary pulmonary nodules is poor.
although emerging techniques such as radial endobronchial ultrasound and navigational bronchoscopy allow better access
to peripheral lesions, but these are not yet in widespread use.
Although “blind” transbronchial needle aspiration of enlarged subcarinal lymphadenopathy is possible, it is limited in the
staging information it can give.
Endobronchial ultrasound allows real-time imaging and guided transbronchial needle aspiration of multiple mediastinal nodal stations and peribronchial tumours.
A meta-analysis has shown a sensitivity of 88% and specificity of 100% for staging mediastinal disease.
Guidance from the National Institute for Health and Clinical Excellence (NICE) gives recommendations on its use in staging disease and biopsying paratracheal or peribronchial tumours.
Transthoracic needle biopsy
Transthoracic needle biopsy under computed tomographic or ultrasound guidance is often the only available approach in patients witha solitary pulmonary nodule where no metastases have been found. The sensitivity of transthoracic biopsy for detecting malignant lesions is estimated at 86% and specificity
as high as 98.8%.
Complications include pneumothorax: although the rates vary widely depending on whether x ray or computed tomography is used for detection. A recent large study found that only 6.6% of patients required chest tube drainage.
Bleeding was seen in just 1% of cases.
There is also a risk of inadequate sampling,
and the procedure may need to be repeated. Before performing a biopsy, lung function should be measured and clotting should be checked. An FEV1 of >35% of predicted is preferred to avoid respiratory compromise from pneumothorax.
Anticoagulants and antiplatelet agents such as clopidogrel should be stopped, although aspirin may be continued.
Small nodule pathway Computed tomography is the modality of choice for following up smaller indeterminate lesions whether detected on chest x ray or computed tomography. Smaller lesions are difficult to investigate as they are below the resolution of positron emission tomography and difficult to biopsy.
The Fleischner Society guidelines suggest radiological follow-up of nodules at various intervals depending on size and risk factors for malignancy.
Where nodules increase in size further investigation isindicated,with consideration of biopsy or positron emission tomography.
Stable nodules should be followed for up to two years. This approach offers a balance between timely identification of malignancies against the burden of scans, radiation exposure, and complications from procedures.
Outcome
Computed tomography revealed a 17 mm peripheral nodule staged as T1aN0M0. The patient was counselled regarding treatment options and was initially keen to know a diagnosisand consider surgery. The nodule was biopsied percutaneously under computed tomographic guidance, complicated by a small pneumothorax that did not require intervention (fig 2⇓).
The histology showed a squamous cell carcinoma. Positron emission tomography was performed with a view to surgery and demonstrated a metabolically active nodule (fig 3⇓) with low
grade uptake in a 6 mm subcarinal lymph node but no other evidence of metastases. The possibility ofspread to lymph nodes was discussed, and endobronchial ultrasound or mediastinoscopy was offered.
At this point the patient did not want to pursue surgical intervention as he felt the impact of treatment on quality of life in the short term would outweigh its benefits. The final
radiological staging was T1aNxM0.
An alternative approach following the new NICE guidance would be to offer positron emission tomography before consideration of biopsy. If any positive nodes are identified then these can be sampled to obtain both a histological diagnosis and accurate staging in a single test.
The patient remains well and asymptomatic at more than 12 months from diagnosis.
Learning points
Certain chest radiograph appearances, including a solitary pulmonary nodule, raise suspicion of cancer and require prompt referral for further investigation.Both radiological and clinical factors influence the probability of malignancy in a solitary pulmonary nodule.
Computed tomography will help to make the diagnosis, stage the disease, and guide which investigation should be performed to obtain a histological diagnosis.
Positron emission tomography has high sensitivity for detecting malignant disease and, if available, should be offered to all patients suitable for radical therapy to ensure accurate staging.
Small nodules have a lower risk of malignancy and may be observed for change over an interval period
Malignant
• Bronchogenic carcinoma• Single metastasis
• Carcinoid
Benign
• Granuloma (often healed tuberculosis)
• Benign tumours (hamartoma, chondroma)
• Rounded pneumonia or abscess
• Aspergilloma
• Rheumatoid nodule
• Arteriovenous malformations
Common causes of a solitary pulmonary nodule
Factors increasing the probability of malignancy in a solitary pulmonary nodule
Patient factors Likelihood ratio
Haemoptysis 5.08
History of malignancy 4.95
Age >70 years 4.16
Smoker 2.27
Radiological factors (computed tomography)
Spiculated edges 5.54
Size >3 cm 5.23
Size 2.1–3 cm 3.67
Malignant growth rate (doubling time 7–465 days) 3.40
Contrast enhancement 2.32
Approximately 50% of patients who develop heart attacks have warning symptoms such as exertional angina or rest angina prior to their heart attacks, but these symptoms may be mild and discounted
According to the World Health Organization,
62% of all strokes and 49% of coronary heart disease events are attributable to high blood pressure. A reduction of 5 g a day in habitual salt intake is associated with a 23% reduction in the rate of stroke and 17% reduction in the rate of total cardiovascular diseaseHigh salt intake is associated with significantly increased risk of stroke and total cardiovascular disease. The habitual salt intake in most Western countries is close to 10 g a day. A reduction of 5 g (about one teaspoon) of salt would bring consumption close to the WHO recommended level (5 g a day at the population level).
Intravascular ultrasound (IVUS)Intravascular ultrasound (IVUS) is a catheter-based examination that provides images of the thickness and the acoustic density of the vessel wall. It has long been considered the criterion standard for the study of the anatomy of the vessel wall. IVUS can depict the presence of atherosclerotic plaques not visible with contrast coronary angiography and may reveal signs of recent disruption.
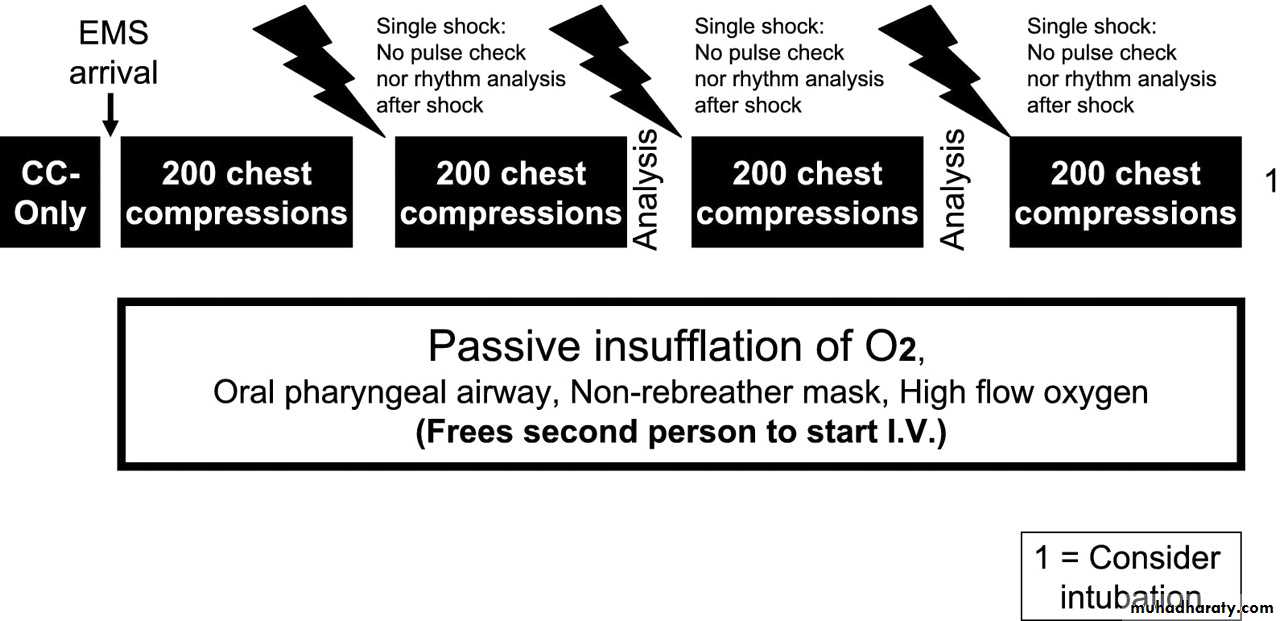
Recent literature has separated ventricular fibrillation arrest into time-sensitive phases.During the first phase (the first 4-5 minutes), the heart is amenable to prompt defibrillation. This is termed the "electrical phase" of cardiac arrest.
During the second phase, the "circulatory phase," the fibrillating myocardium has used up much of its energy stores, and chest compressions are necessary to perfuse or "prime" the heart before defibrillation will likely be successful. This second phase is usually the time in which prehospital care providers arrive.
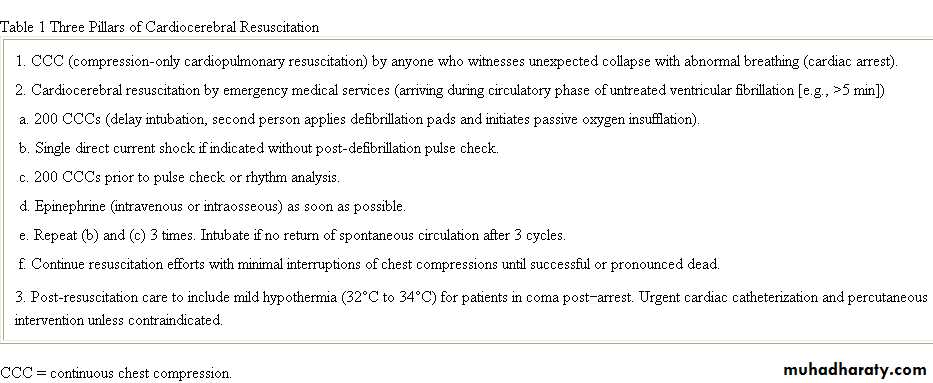
Cardiocerebral Resuscitation: EMS Protocol for Out-of-Hospital Cardiac Arrest Cardiocerebral resuscitation protocol for emergency medical services (EMS) providers once they arrive on the scene. Continuous chest compressions (CCCs) only indicates that a bystander is doing adequate CCCs. If so, the paramedics do not perform the initial 200 CCCs before the first electrocardiograph rhythm analysis with their automated external defibrillator or defibrillator that has the ability to record the electrocardiographic rhythm via the electrode paddles or pads. If there is no bystander doing CCCs or if there is and CCCs are deemed to be inadequate by the EMS personnel, 200 forceful CCCs are carried out with full chest wall release after each compression. The compressions are given at a rate of 100 compressions/min before electrocardiographic analysis. When appropriate, a defibrillator shock (indicated by the lightning symbol) is given. Following the defibrillator shock, the EMS personnel should not check for pulse or electrocardiographic rhythm but rather immediately initiate another 200 CCCs. After these 400 CCCs, they perform an analysis of the electrocardiographic rhythm and ascertain the presence or absence of a pulse. Three such sequences are completed prior to intubation. Intubation as well as bag-valve-mask ventilations are initially prohibited. This is because intubation delays the initiation of CCCs, and both result in excessive ventilations. Rather, the patient is treated with passive insufflation of oxygen by placing an oral pharyngeal airway and a nonrebreather mask and attaching high-flow (10 to 15 l/min) oxygen. Intubation is recommended if the patient does not have a shockable rhythm or after 3 single shocks, each followed by 200 CCCs, and a perfusing rhythm is still not present. If the patient is unconscious or not breathing adequately, intubation is recommended prior to transfer. 1 = consider intubation.
The Third Pillar of CCR Post-Resuscitation Care
Only about 25% of those initially resuscitated survive to leave the hospital. Among those initially resuscitated who do not survive long term, about one-third die from central nervous system damage, another one-third die from myocardial failure, and the final one-third from a variety of causes including infection and multiorgan failure .For comatose patients post-resuscitation, hypothermia and early cardiac catheterization (unless contraindicated), even in the absence of classic electrocardiograph (ECG) signs of infarction or ischemia, are recommended. Because these therapies are not available in all hospitals, the Arizona Bureau of Emergency Medical Services and Trauma is designating "Cardiac Arrest" hospitals, much as "Trauma One" hospitals are designated.
Sunde et al. in Norway formalized their post-resuscitation care and pursued an aggressive approach with such patients. Their approach emphasized providing therapeutic hypothermia to all who remained comatose post-resuscitation and performing early coronary angiography and percutaneous coronary intervention (PCI) in any patients with possible myocardial ischemia as a contributing factor to their cardiac arrests. Using this approach, they found a significant improvement in survival.
The overall survival rate to hospital discharge was 61%, but there was a significant difference between those who were cooled pre-PCI and those who were not. Of those who received both angioplasty and hypothermia, the hospital discharge survival rate was 75%, with 73% of those survivors having good neurologic function. Among those who did not receive hypothermia, 44% were discharged from the hospital and only 16% had normal neurologic function .
CCR is not recommended for individuals with respiratory arrest. These individuals require early ventilations; until alternatives to the current approach are shown to be better, guidelines recommend CPR for individuals with respiratory arrest .
In-hospital cardiac arrest may be different. Hopefully, most in-hospital VF cardiac arrests can be detected and treated during the electrical phase with immediate defibrillation. The National Registry of CPR of in-hospital cardiac arrests has shown that the majority are not VF but are rather non-VF arrests, many of which are noncardiac in etiology .In such cases, ventilation and chest compressions may be important.
CHD(coronary heart dis)includes history of myocardial infarction, unstable angina, coronary artery procedures (angioplasty or bypass surgery), or evidence of clinically significant myocardial ischemia.
CHD risk equivalents include:
clinical manifestations of noncoronary forms of atherosclerotic disease (peripheral arterial disease, abdominal aortic aneurysm, and carotid artery disease [transient ischemic attacks or stroke of carotid origin or >50% obstruction of a carotid artery]), diabetes, and 2+ risk factors with 1-year risk for hard CHD >20%.
The newer, third-generation dihydropyridine CCBs such as lacidipine,manidipine,and lercanidipine are regularly reported to cause less peripheral edema.
Patients with noncardiogenic pulmonary edema have a
• warm periphery,• a bounding pulse,
• absence of S3 gallop and jugular venous distention.
4. Differentiation is often made based on PCWP measurements from invasive hemodynamic monitoring.
PCWP is generally more than 18 mm Hg in HF and is less than 18 mm Hg in noncardiogenic pulmonary edema, but superimposition of chronic pulmonary vascular disease can make this distinction more difficult to discern.
5. With the advent of BNP level testing, reliably differentiating cardiac from noncardiac causes of pulmonary edema is now possible.
In obese respondents (>BMI 30 kg/m2), relative risk of
fatal CVD was fourfold higher and risk of
nonfatal CVD was twofold higher than in normal-weight respondents. Similar associations were observed for WC (>88 cm vs <80 cm in women and >102 cm vs <94 cm in men).
Hypertension 5-fold higher in obese women
The cardio-metabolic risk associated with abdominal obesity is attributed to the presence of visceral adipose tissue (VAT), which promotes insulin resistance, dyslipidaemia, and hypertension.
VAT stores can be measured by computerized axial tomography, magnetic resonance imaging, and dual energy x-ray absorptiometry, but these techniques are not feasible and too expensive for everyday use.
Abdominal obesity as measured by WC and WHR is significantly associated with the risk of incident CVD events. A 1 cm increase in WC is associated with a 2% increase in risk of future CVD and a 0.01 increase in WHR is associated with a 5% increase in risk. These simple measures of abdominal obesity should be incorporated in CVD risk assessments.
The burden of cardiovascular disease (CVD) among patients with diabetes is substantial.
Individuals withdiabetes are at 2- to 4-fold increased risk of cardiovascular events compared with age- and sex-matched individuals without diabetes. In diabetic patients over the age of 65 years, 68% of deaths are from coronary heart disease (CHD) and 16% are from stroke. Anumber of mechanisms for the increased cardiovascular risk
with diabetes have been proposed, including increased tendency toward intracoronary thrombus formation, increased platelet reactivity, and worsened endothelial dysfunction.
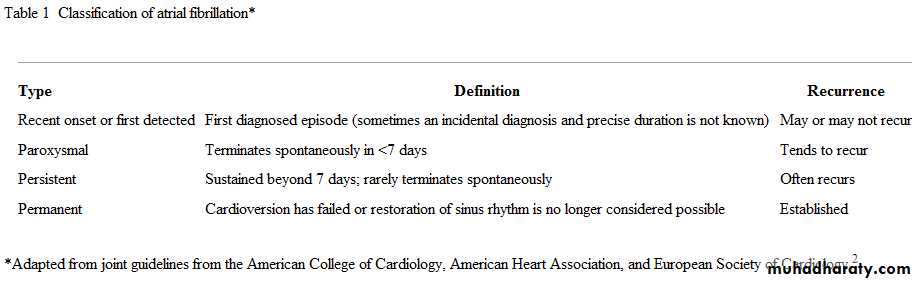
Atrial fibrillation(AF)
paroxysmalif it terminates spontaneously in fewer than 7 days (often in <24 h)
persistent
when it terminates either spontaneously after 7 days or following cardioversion.
Permanent
that persists for more than one year, either because cardioversion has failed or because cardioversion has not been attempted.
Atrial Fibrillation, Diagnosis and Management
Medscape Oct 29, 2009
What are the indications for rate control?
Although one may believe that restoring the normal sinus rhythm would yield a better outcome in patients with atrial fibrillation than the ventricular rate-control strategy, the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study showed that the two methods yield similar results in terms of mortality rate and stroke rate. Therefore, because of the cardiac and noncardiac side effects associated with currently available antiarrhythmic drugs, rate control has become a popular strategy in most patients with atrial fibrillation. This is particularly true in elderly patients and in those who would benefit from rate-control drugs because of other associated diseases (eg, hypertension, other cardiac diseases).How is adequate rate control ensured?
The adequacy of rate control should be assessed after beta-blocker or other rate-control drug therapies have been started.Persisting symptoms are a sign of rate-control inadequacy. Rate control should be assessed both at rest and with exertion.
Heart rate targets include the following:
A resting heart rate of fewer than or equal to 80 bpm
A 24-hour Holter monitor average of fewer than or equal to 100 bpm A heart rate of 110 or fewer bpm during a 6-minute walk In addition to Holter monitoring, an ECG exercise test is also commonly used to evaluate rate control during exertion in active and younger patients.
What are the indications for rhythm control?
The AFFIRM study showed that rate- and rhythm-control strategies yield similar results in terms of mortality rate and stroke rate Therefore, rhythm control is used mainly in younger patients, in patients1.who remain symptomatic with adequate rate-control therapy, and in patients in whom rate-control
2.drugs are contraindicated or in whom these drugs cause adverse effects. Rhythm-control drugs can also be used in combination with rate-control drugs.
Which patients should be referred for rhythm control?
Current guidelines recommend considering rhythm control in patients with(a) lone atrial fibrillation, especially younger patients;
(b) symptomatic atrial fibrillation, such as frequent symptomatic paroxysmal atrial fibrillation or symptoms despite rate control; or
(c) atrial fibrillation secondary to a corrected precipitant.
(d)patients who should but cannot take warfarin might reduce their risk of stroke if sinus rhythm is restored.
According to recent guidelines, prevention of recurrence of atrial fibrillation by ablation is justified only when atrial fibrillation is associated with disabling symptoms, if amiodarone fails.
and its use depends on the type of atrial fibrillation.2
On what basis is a drug chosen for rhythm control?
A.In the absence of associated cardiac disease, sotalol, flecainide, or propafenone is used as the first line of rhythm-control therapy, and amiodarone• is reserved for patients in whom the other drugs do not elicit a response.Long-term amiodarone use carries substantial noncardiac adverse events. However, in patients with
• cardiac disease such as coronary artery disease or systolic or diastolic heart failure, amiodarone becomes the drug of choice because of its decreased proarrhythmic effects compared with other antiarrhythmic drugs. The Canadian Trial of Atrial Fibrillation (CTAF) and Sotalol Amiodarone Atrial Fibrillation Efficacy Trial (SAFE-T) studies showed that amiodarone is also more effective at maintaining sinus rhythm than other drugs.
Administration of class Ic drugs in patients with atrial fibrillation and atrial flutter is associated with the risk of potentially life-threatening conversion of atrial fibrillation to atrial flutter with 1:1 AV conduction. Therefore, pre-administration of a beta-blocker or calcium channel blocker is recommended when class Ic drugs are taken.
Class III agents (sotalol, amiodarone) have some beta-blocking effect and should be used with caution in patients with a history of bradycardia.
What are the indications and recommendations for anticoagulation in patients with atrial fibrillation?
A patient with a CHADS-2 score of 0 (ie, absence of all of the above risk factors) can be safely treated with aspirin. Clopidogrel is an option in patients who are allergic to aspirin.
A patient with a score of 3 or greater should undergo anticoagulation with warfarin (if it is not contraindicated).
The decision in patients with CHADS-2 score of 1 or 2 is individualized and depends on the other risk factors and patient preference.
In most studies, a prior history of stroke or TIA is the strongest independent predictive risk factor for embolization. A history of hypertension, as well as the severity of the hypertension, may also influence the risk of stroke. Female sex and coronary artery disease have been suggested as other factors associated with a higher risk of thromboembolism in atrial fibrillation.
DC cardioversion is the delivery of electrical current that is synchronized to the QRS complexes; it can be delivered in monophasic or biphasic waveforms. The required energy for cardioversion is usually 100-200 J (sometimes higher energy is required) for monophasic waveforms and less for biphasic waveforms. The patient should be sedated. In patients with atrial fibrillation of relatively short duration in whom the left atrium is not significantly large, the success rate of cardioversion exceeds 75% (ie, the size of the left atrium and the duration of atrial fibrillation inversely correlate with the success rate of cardioversion).
DC cardioversion is the delivery of electrical current that is synchronized to the QRS complexes; it can be delivered in monophasic or biphasic waveforms. The required energy for cardioversion is usually 100-200 J (sometimes higher energy is required) for monophasic waveforms and less for biphasic waveforms. The patient should be sedated. In patients with atrial fibrillation of relatively short duration in whom the left atrium is not significantly large, the success rate of cardioversion exceeds 75% (ie, the size of the left atrium and the duration of atrial fibrillation inversely correlate with the success rate of cardioversion).
The ACC strongly recommends anticoagulation (INR between 2 to 3) be administered at least 3 weeks prior to and 4 weeks following cardioversion in patients with atrial fibrillation of 48 hours’ duration or longer or of unknown duration, regardless of the method (DC vs pharmacological).
In this situation, as an alternative to anticoagulation prior to cardioversion, it is reasonable to perform TEE to search for thrombus in the left atrium or left atrial appendage.In patients with no identifiable thrombus, immediate cardioversion with concurrent heparinization and subsequent anticoagulation for 4 weeks is an option. However, patients in whom TEE reveals thrombus should receive anticoagulation for at least 3 weeks prior to and 4 weeks following cardioversion.
Embolization is the most important complication of cardioversion.
Other complications of electrical cardioversion pulmonary edema,hypotension,
myocardial dysfunction,
skin burns, which may be avoided with the use of steroid cream and proper technique.
Electrical cardioversion is also associated with some ST- and T-wave changes on ECG and may elevate levels of serum cardiac biomarkers.
Synchronization prevents serious ventricular arrhythmias.
What is the success rate of catheter ablation in the treatment of atrial fibrillation?
The success rate depending on the type and duration of atrial fibrillation (ie, paroxysmal vs persistent),structural remodeling of the heart, and the technique and expertise of the cardiac electrophysiologist but usually ranges from 60-80% in 1- to 2-years of follow-up
The threshold for catheter ablation has fallen over the years and is likely to continue to fall. Ablation of chronic and persistent atrial fibrillation is more complex and yields lower success rates. Therefore, it is an option only if antiarrhythmic drugs fail in patients with persistent atrial fibrillation who remain severely symptomatic despite adequate ventricular rate control.
What are the complications of pulmonary vein isolation?
Complications associated with RF ablation of atrial fibrillation include cardiacperforation, pericardial effusion, cardiac tamponade, vascular access complications,
pulmonary vein stenosis,
thromboembolism,
atrioesophageal fistula, and
left atrial flutter.
Prognosis of angina
The main adverse outcomes are unstable angina, MI, and sudden death due to arrhythmias. Annual mortality rate is about 1.4% in patients with angina, no history of MI, a normal resting ECG, and normal BP. However, women with CAD tend to have a worse prognosis. Mortality rate is about 7.5% when systolic hypertension is present, 8.4% when the ECG is abnormal, and 12% when both are present.
Type 2 diabetes about doubles the mortality rate for each scenario.
Predicting prognosis in stable angina—results from the Euro heart survey of stable angina: prospective observational study
The rate of death and non-fatal myocardial infarction in the first year was 2.3 per 100 patient years; factors most predictive of adverse outcome were comorbidity, diabetes, shorter duration of symptoms, increasing severity of symptoms, abnormal ventricular function, resting electrocardiogaphic changes, The annual incidence of death in the survey was 1.5%, and the incidence of non-fatal myocardial infarction was 1.4%. In the subgroup with proved coronary disease these rates were 1.8% and 3.2%.
Progestogen only pills and hormone releasing intrauterine devices were not associated with any increased risk of venous thrombosis.
Any disorder that elevates left heart filling pressures, including systolic dysfunction, diastolic dysfunction, and valvular heart disease, can result in elevated pulmonary artery pressures.
Two open-label safety and efficacy trials were conducted with the Rheos® system: the Rheos® Feasibility Trial in the United States, and the CVRx Device Based Therapy in Hypertension Trial (DEBuT-HT) in Europe. Both trials enrolled patients with resistant hypertension, defined as blood pressure ≥ 160 mm Hg SBP and/or ≥ 90 mm Hg DBP despite at least 2 months of full therapy with 3 or more antihypertensive medications, including at least 1 diuretic. In all patients the Rheos® system was surgically implanted and activated 1 month later. Patients showed sustained decreases in blood pressure after 1 year in both studies.
It is generally recommended that
orthostatic blood pressure be measured while the patient is in the standing position every minute during the first 3 minutes after he or she has been lying supine for 5 minutes.2 If the patient cannot stand for this period of time, the lowest systolic blood pressure should be recorded.Orthostatic hypotension is a physical sign defined as a reduction of at least 20 mm Hg in systolic blood pressure or of at least 10 mm Hg in diastolic blood pressure within 3 minutes after standing.3
Coronary Revascularization in Context
(CABG), introduced in 1968, was the only method of coronary revascularization until 1977, when percutaneous balloon angioplasty was first performed. The complications of balloon angioplasty (acute vessel closure in 3 to 5% of patients and restenosis in almost half) prevented its use in patients with severe coronary artery disease. In the 1990s, the introduction of bare-metal stents led to reduced rates of these complications. The improved short-term and long-term procedural success with percutaneous coronary intervention (PCI) allowed for its safe and effective performance in patients with severe coronary artery disease.
NEJM February 18, 2009
By the year 2000, more PCI procedures than CABG procedures were being performed in the United States. In early 2000, drug-eluting stents were approved for use in Europe and North America, after studies showed a markedly reduced incidence of restenosis with drug-eluting stents as compared with bare-metal stents. Subsequently, the use of drug-eluting stents was rapidly adopted; in 2006, a total of 253,000 CABG procedures and 1,131,000 PCI procedures were performed in the United States,1 with drug-eluting stents used in 90% of the PCIs.2
Should We Look for Silent PE in Patients with DVT?
Although one third of patients with lower-extremity deep venous thrombosis exhibited silent pulmonary embolism, routine screening for PE generally does not change management.Autopsy studies have shown that, even in patients with large or fatal pulmonary embolisms (PEs), most cases were unsuspected or undiagnosed ante mortem. This finding begs the question: Should standard screening for PE be performed in patients with deep venous thrombosis (DVT) but without clinical symptoms of PE?
Should We Look for Silent PE in Patients with DVT?
Although one third of patients with lower-extremity deep venous thrombosis exhibited silent pulmonary embolism, routine screening for PE generally does not change management.Autopsy studies have shown that, even in patients with large or fatal pulmonary embolisms (PEs), most cases were unsuspected or undiagnosed ante mortem. This finding begs the question: Should standard screening for PE be performed in patients with deep venous thrombosis (DVT) but without clinical symptoms of PE?
• However, most episodes of pulmonary embolism carry a low mortality risk (about 1%) when properly diagnosed and treated .
• Massive pulmonary embolism represents only 5% of all cases of pulmonary embolism and is fatal in about 40% of patients.
Why is it missed?
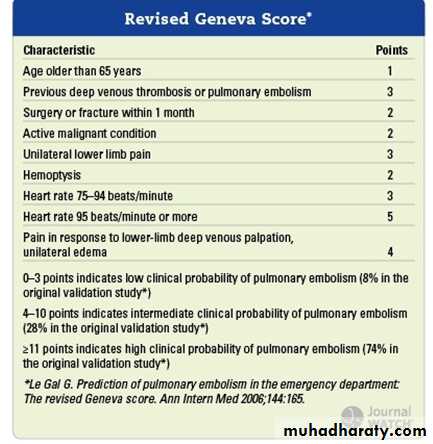
The classic triad of pleuritic chest pain, dyspnoea, and haemoptysis occurs in less than 10% of patients, but the most common symptoms (dyspnoea, chest pain) are non-specific. In 40% of cases, major thromboembolic risk factors are absent. Clinical signs of deep vein thrombosis are observed in only 15% of patients and haemoptysis in only 4.5-11% of cases.1 5 Pulmonary infarction with fever may mimic pneumonia. Chest pain reproducible on palpation also does not rule out pulmonary embolism.BMJ April 2010
Pulmonary embolism
As a class, the plasminogen activators have been shown to restore normal coronary blood flow in 50% to 60% of STEMI patients. The successful use of fibrinolytic agents provides a definite survival benefit that is maintained for years. The most critical variable in achieving successful fibrinolysis is time from symptom onset to drug administration. A fibrinolytic is most effective within the first hour of symptom onset and when the door-to-needle time is 30 minutes or less.
As a class, the plasminogen activators have been shown to restore normal coronary blood flow in 50% to 60% of STEMI patients. PCI can successfully restore coronary blood flow in 90% to 95% of MI patients. Several studies have demonstrated that PCI has an advantage over fibrinolysis with respect to short-term mortality, bleeding rates, and reinfarction rates. However, the short-term mortality advantage is not durable, and PCI and fibrinolysis appear to yield similar survival rates over the long term.
Percutaneous Coronary Intervention
Patients with STEMI or MI with new left bundle branch block should have PCI within 90 minutes of arrival at the hospital if skilled cardiac catheterization services are available.9Patients with NSTEMI and high-risk features such as elevated cardiac enzymes, ST-segment depression, recurrent angina, hemodynamic instability, sustained ventricular tachycardia, diabetes, prior PCI, or bypass
are recommended to undergo early PCI (<48 hours).
PCI consists of diagnostic angiography combined with angioplasty and, usually, stenting.
Surgical Revascularization
Emergent or urgent (CABG) is warranted in the setting of failed PCI in patients with hemodynamic instability and coronary anatomy amenable to surgical grafting.9 also indicated in the setting of mechanical complications of MI, such as ventricular septal defect, free wall rupture, or acute mitral regurgitation.CABG can limit myocardial injury if performed within 2 or 3 hours of symptom onset. Emergency CABG carries a higher risk of perioperative morbidity (bleeding and MI extension) and mortality than elective CABG. Elective CABG improves survival in post-MI patients who have left main artery disease, three-vessel disease, or two-vessel disease not amenable to PCI.
Complications of deep-vein thrombosis, which are less common in the upper extremities than in the lower extremities, include
• Pulmonary embolism (6% for upper extremities, vs. 15 to 32% for lower extremities),
• Recurrence at 12 months (2 to 5% for upper extremitiesvs. 10% for lower extremities), and
• The post-thrombotic syndrome (5% for upper extremities vs. up to 56% for lower extremities).
Randomised controlled trial data show that untreated patients with essential hypertension with normal or raised plasma renin concentration (for example,many younger <55 years patients with essential hypertension, especially those who have successfully reduced their dietary salt intake) respond rather better to A and B drugs,
whereas those with low renin (such as people of African origin and older >55 years patients) respond well to C or D drugs). B drugs are no longer preferred as aroutine initial treatment for adults with hypertension.
How is acute aortic dissection diagnosed?
Clinical
A triad of symptoms—characteristic chest pain (usually abrupt and/or severe), a pulse deficit or blood pressure differential, and an abnormal chest radiograph—increases the likelihood of dissection but is present in only a third of patients. A pulse deficit is the unilateral absence or diminution of a pulse compared with contralateral palpation. To detect this, a full peripheral pulse examination is mandatory (radial, brachial,carotid, and femoral pulses). The blood pressure differential is defined as a difference in systolic blood pressure between both arms of >20 mm Hg.
Although similar to the diastolic rumble of mitral stenosis, the Carey Coombs murmur does not have an opening snap, presystolic accentuation,or a loud first sound, but may follow an S3 gallop. The latter may be superficially confused with an opening snap.
To help reduce restenosis, drug eluting stents that release anti-proliferative agents—such as sirolimus, tacrolimus, paclitaxel, and zotarolimus—were developed and introduced at the beginning of the 21st century.
Rates of revascularisation at one year for drug eluting stents within individual trials were less than 5% compared with 10-25% for bare metal stents. Restenosis is caused by proliferation of cells in the intima, a smooth muscle wall in the coronary vessel (neointimal hyperplasia), which together with clots can occlude the stented artery.
In a meta-analysis of randomised controlled trials, the incidence of definite or probable in-stent thrombosis one to four years after implantation was 0.9% in the sirolimus and paclitaxel eluting stent groups versus 0.4-0.6% in the bare metal stent group,
• Eplerenone should not be started in patients with a serum potassium concentration above 5mmol/L, creatinine clearance below 50mL/min or severely impaired liver function, or in those taking potassium supplements or potassium-sparing diuretics. Eplerenone is primarily metabolised via cytochrome P450 isoenzymeCYP 3A4, and so patients taking "strong" inhibitors of this isoenzyme (e.g. itraconazole, ritonavir, clarithromycin) should not be started on eplerenone. For patients taking mild–moderate inhibitors (e.g. erythromycin, diltiazem, verapamil, fluconazole), the dose of eplerenone should not exceed 25mg daily.
• Prominent U waves can easily be mistaken for T waves, leading to overestimation of the QT interval.This mistake can be avoided by identifying a lead where U waves are not prominent—for example, lead aVL.
• 1. Prophylaxis is now recommended only for patients with these four conditions:
• prosthetic cardiac valve• previous infective endocarditis
• certain types of congenital heart disease
• cardiac transplantation with valvulopathy
• 2. For patients with the conditions listed above, prophylaxis should be given only before:
• dental procedures that involve manipulation of gingival tissue or the periapical region of teeth, or perforation of oral mucosa .incision or biopsy of respiratory tract mucosa,procedures on infected skin or musculoskeletal structures
In view of the limited evidence, the AHA has published a new guideline to prevent infective endocarditis
• 3. Prophylaxis is no longer recommended for gastrointestinal or genitourinary procedures. However, if urine is colonized by enterococcus, eradication before invasive urinary procedures is reasonable.
• 4. A single 2-g dose of amoxicillin, given 30 to 60 minutes before the procedure, remains the regimen of choice .
• Recommendation
• conditions as being at increased risk of developing infective endocarditis:• acquired valvular heart disease with stenosis or regurgitation
• valve replacement
• structural congenital heart disease, including surgically corrected or palliated structural conditions, but excluding isolated atrial septal defect,fully repaired ventricular septal defect or fully repaired patent ductus and closure devices that are judged to be endothelialised
• previous infective endocarditis
• hypertrophic cardiomyopathy.
It now seems clear that magnetic resonance imaging (MRI) is better at detecting acute stroke than conventional computed tomography (CT),
The difference was especially marked in the first few hours after onset of stroke, when critical decisions about management must be made. In this study, 90 patients presented within three hours of an acute ischaemic stroke. MRI detected 41 of the strokes, computed tomography only six.
MRI better than CT for diagnosing acute stroke
• The prevalence of atrial fibrillation rises with age from 1.5% in people in their 60s to more than 10% in those over 90. People with atrial fibrillation have double the mortality and a four to fivefold higher risk of stroke than those without fibrillation. About a quarter of all strokes in elderly people are caused by atrial fibrillation.Strokes caused by atrial fibrillation are often severe and lead to high mortality and a low quality of life. Even if normal rhythm cannot be restored, antiplatelet agents reduce the risk of stroke by around 22% vitamin K antagonists such as warfarin, reduce the risk by 64%.
• 1. contraindications to anticoagulation.
• 2. structural heart disease (e.g. large left atrium >5.5 cm, mitral stenosis) that precludes long-term maintenance of sinus rhythm.• 3. a long duration of AF (usually >12 months).
• 4. a history of multiple failed attempts at cardioversion and/or relapses.
• 5. an ongoing but reversible cause of atrial fibrillation (e.g. thyrotoxicosis).
Normal daily requirements for fluid and electrolytes for a healthy adult
Item Requirement
Water 1.5 ml/kg/hour
Sodium 1–1.5 mmol/kg
Potassium 1 mmol/kg
Chloride 1.5 mmol/kg
Phosphate 0.2–0.5 mmol/kg
Calcium 0.1–0.2 mmol/kg
Magnesium 0.1–0.2 mmol/kg
Energy 145 kJ/kg
Results of a three year study involving 2400 patients treated in 10 hospitals across England show that primary angioplasty is feasible and cost effective. Provided that the procedure is carried out within two hours of a heart attack, death rates are lower than with thrombolysis, the current standard treatment, and hospital stays are shorter, says a report of the study. Roger Boyle, England’s clinical director for heart disease and stroke, said that the 30 day mortality rate for thrombolysis is 7%, but this reduces to 5% for angioplasty if it is given within two hours.
All myocardial infarction patients in England are to be offered angioplasty
• When it comes to heart attacks and strokes, men and women are not created equal. Women develop cardiovascular disease later than men -- usually after menopause, and often well into their 70s. And women are different from men when it comes to the response to aspirin as well, says Nanette Wenger, MD, spokesperson for the American Heart Association. Based on study data:
• For healthy men aspirin seems to prevent heart attacks, but not strokes.
• For healthy women under 65, aspirin prevents strokes, but not heart attacks.
• For healthy women over 65, aspirin appears to prevent heart attacks similarly to men.
Aspirin: Different Benefits for Men and Women
Timely and effective reperfusion with the use of either primary percutaneous coronary intervention (PCI) or thrombolytic therapy remains the most effective treatment strategy for limiting the size of the myocardial infarct, preserving left ventricular ejection fraction, and improving the clinical outcomes in such patients. However, despite optimal reperfusion therapy, morbidity and mortality remain substantial, with about 5 to 6% of patients having a subsequent cardiovascular event by 30 days. The abrupt reperfusion of ischemic myocardium can itself inflict injury on the myocardium — a phenomenon termed myocardial reperfusion injury.
Time to Take Myocardial Reperfusion Injury Seriously
• Cardiac TNs are regulatory proteins in striated muscle and consist of 3 subunits: TN-T, TN-I, and TN-C. Striated muscle is present in skeletal and cardiac muscle. TN-C is also found in smooth muscle so it has the least cardiac specificity. In this viewpoint, the term "TN" will refer to TN-I and TN-T, not TN-C. TN-I is considered the most cardiac-specific because it has not been identified in skeletal muscle.
• and all-cause inpatient mortality. The majority of the non-ACS conditions tend to cause rather low-level TN elevations, and usually they do not tend to cause the typical evolving rise-and-fall pattern of TN levels over 12 to 24 hours that are found in patients with true ACS. Therefore, when there is a question regarding whether a patient with an initially elevated TN level has ACS or not, it would be prudent to monitor changes in the electrocardiograph and serial TN levels to help make the distinction
• A cardiovascular event
• Is defined in the Framingham equation as myocardial infarction, new angina, ischaemic stroke, transient ischaemic attack (TIA), peripheral vascular disease (PVD), congestive heart failure (CHF) and cardiovascular-related death.Dual antiplatelet therapy need not be interrupted for dental or minor surgical procedures.
Where therapy must be discontinued prematurely to minimise the operative bleeding risk during major surgery, trial data suggest that this should be done at least five days before surgery. Aspirin should be continued perioperatively if possible and clopidogrel restarted at the earliest opportunity after surgery.
A cardiologist must be involved in any decision to discontinue antiplatelet therapy prematurely in patients with a recently implanted coronary stent.
In patients at high risk of perioperative stent thrombosis in whom an interruption in dual antiplatelet therapy is unavoidable, "bridging" therapy with heparin, direct thrombin, or short acting intravenous glycoprotein IIb/IIIa inhibitors until oral antiplatelet agents can be safely restarted should be considered, although the success of this approach is unclear. For such patients, it might be safest to perform surgery in centres with rapid access to emergency percutaneous coronary intervention.
November 2008 BMJ
• The typical image of a patient with heart failure is of a breathless person with a large flabby heart, which contracts poorly with a reduced left ventricular ejection fraction. However, many patients, mainly elderly women, have symptoms of heart failure but their hearts are not enlarged. Echocardiography shows a relatively normal left ventricular ejection fraction but usually with some left ventricular hypertrophy. Because systolic function was thought to be normal or near normal, the term "diastolic heart failure" was coined for this group of patients. However, we now know that systolic function is not entirely normal, and the problem is not only caused by diastolic dysfunction; hence the term "heart failure with a normal ejection fraction" is more appropriate.• Recent European Society of Cardiology guidelines
• suggested a diagnostic algorithm for heart failure with a normal ejection fraction. In essence, if a breathless patient has left ventricular hypertrophy, left atrial enlargement, and evidence of a raised left atrial pressure either by B-type natiuretic peptide (which is especially useful in primary care) or newer echocardiographic indices then the diagnosis of heart failure with a normal ejection fraction is highly likely.• Medically speaking, "ventricular remodeling" implies a decline in function (even though the word "remodeling" usually implies improvement).
• The term reverse remodeling in cardiology implies an improvement in ventricular mechanics and function after a remote injury.
• Concentric hypertrophy is due to pressure overload, while eccentric hypertrophy is due to volume overload
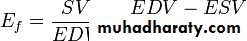
By definition, the volume of blood within a ventricle immediately before a contraction is known as the end-diastolic volume. Similarly, the volume of blood left in a ventricle at the end of contraction is end-systolic volume. The difference between end-diastolic and end-systolic volumes is the stroke volume, the volume of blood ejected with each beat. Ejection fraction (Ef) is the fraction of the end-diastolic volume that is ejected with each beat; that is, it is stroke volume (SV) divided by end-diastolic volume (EDV):
In a healthy 70-kg (154-lb) man, the SV is approximately 70 ml and the left ventricular EDV is 120 ml, giving an ejection fraction of 70/120, or 0.58 (58%).
• Systolic dysfunction was defined as an LVEF <40% or qualitative documentation of systolic dysfunction, while
• preserved systolic function meant LVEF >40% or qualitative documentation of preserved systolic function.
Aspirin (acetylsalicylic acid or ASA ) is acetylated, while others such as
Disalcid (salsalate) and (Trilisate) choline magnesium trisalicylate are nonacetylated.Nonacetylated Salicylates
Nonacetylated salicylate compounds such as choline magnesium trisalicylate (Trilisate) 500 to 750 mg two or three times daily are effective therapies for many patients, and we have had success using this group of drugs. These medications have fewer adverse GI effects than regular aspirin compounds or NSAIDs and provide a less expensive alternative to the COX-2 inhibitors. Salicylate levels can also be measured relatively easily in serum, similar to other pharmaceutical compounds, although this is not routine practice.• A previous recommendation suggested that patients with known cardiovascular disease receive the following treatment algorithm for musculoskeletal pain: acetaminophen or aspirin → nonacetylated salicylates → nonselective NSAIDs → COX-2 inhibitors.
• In the current study, the use of NSAIDs increased the risks for overall mortality, hospitalization because of heart failure, and hospitalization because of MI in patients with existing heart failure.
The clinically overt DHF and SHF appear to be 2 separate syndromes with
distinctive morphologic and functional changes althoughsigns, symptoms, and prognosis are very similar.
In DHF, the left ventricle is not dilated and the ejection fraction is preserved.
In contrast in SHF, it is dilated and the ejection fraction is reduced.
The neurohormonal abnormalities in DHF and SHF appearto be similar.
The stimuli and the signals that ultimately produce these 2 different phenotypes of chronic heart failure remain, presently, largely unknown.
Definition of Heart Failure
Heart failure is a complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood.The cardinal manifestations of HF are dyspnea and fatigue, and signs (edema,rales)
which may limit exercise tolerance, and fluid retention, which may lead to pulmonary congestion and peripheral edema. Both abnormalities can impair the functional capacity and quality of life of affected individuals, but they do not necessarily dominate the clinical picture at the same time.
Some patients have exercise intolerance but little evidence of fluid retention, whereas others complain primarily of edema and report few symptoms of dyspnea or fatigue.
Because not all patients have volume overload at the time of initial or subsequent evaluation, the term “heart failure” is preferred over the older term “congestive heart failure.”
In most patients,abnormalities of systolic and diastolic dysfunction coexist,regardless of EF.
Several recent assays have been developed for natriuretic peptides (BNP and NT-proBNP). Several of the natriuretic peptides are synthesized by and released from the heart.
Elevated plasma BNP levels have been associated with
• reduced LVEF .
• LV hypertrophy, elevated LV filling pressures,
• acute MI and ischemia,
• pulmonary embolism and chronic obstructive pulmonary disease.
BNP levels tend to be less elevated in HF with preserved EF than in HF with low EF
When interpreting an elevated BNP level, it is useful to remember that values may be elevated due to factors other than heart failure.
Higher levels are often seen in obese patients and those with renal disease, in the absence of heart failure.
BNP is also one of the reasons why people will feel the need to urinate after getting into the bathtub or pool. The increased pressure on the body drives more fluid back into systemic circulation which in turn leads to a slight increase in preload. The left ventricle, and to a small degree the left atrium, secrete BNP in response. The natriuretic effect of BNP leads to an increase in urine production.
The physiologic actions of BNP are similar to ANP and include decrease in systemic vascular resistance and central venous pressure as well as an increase in natriuresis.
Thus, the net effect of BNP and ANP is a decrease in blood volume and a decrease in cardiac output.
In long standing biventricular chronic heart failure, chest radiographs may only show cardiomegaly without alveolar edema or pleural effusions due to adaptive lung mechanism with increased arterial vasoconstriction and lymphatic drainage.
The clustering of cardiovascular risk factors in individual patients, termed the metabolic syndrome or syndrome X, includes any 3 of the following criteria:
• Abdominal diposity,
• Hypertriglyceridemia,
• low high-density lipoprotein,
• hypertension,
• fasting hyperglycemia.
The use of calcium channel blockers with negative inotropic effects is not recommended in asymptomatic patients with EF less than 40% after MI
Several studies have suggested that prolonged therapy with hydralazine and nifedipine in patients with severe aortic regurgitation and preserved LV function might act to minimize structural changes in the ventricle and thereby possibly delay the need for surgical intervention; however, these drugs are often poorly tolerated in this setting, and no trial has shown that these vasodilators can reduce the risk of HF or death .There are no long-term studies of vasodilator therapy in patients with severe asymptomatic mitral regurgitation.
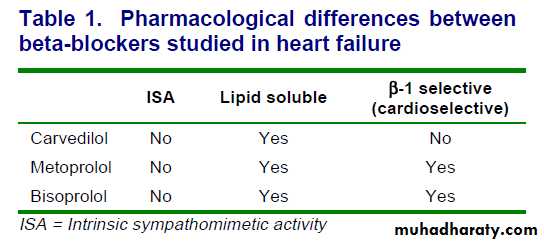
Use of 1 of the 3 beta blockers proven to reduce mortality (i.e.,
bisoprolol, carvedilol, and sustained release metoprolol succinate)is recommended for all stable patients with current or prior symptoms of HF and reduced LVEF, unless contraindicated .(Evidence: A)
Nonsteroidal anti-inflammatory drugs can cause sodium retention and peripheral vasoconstriction and can attenuate the efficacy and enhance the toxicity of diuretics and ACEIs .
Development of newer agents has focused on obtaining a higher degree of vascular selectivity.
Felodipine is a highly vascular selective calcium entry blocker, with a vascular selectivity ratio greater than 100, as shown experimentally.
Isradipine and nicardipine are also vascularly selective calcium entry blockers. Hemodynamic studies in patients with hypertension, coronary artery disease, congestive heart failure, or in patients receiving beta-adrenergic blockade, show that felodipine can produce profound arteriolar dilatation without the negative effects of left ventricular systolic performance. Furthermore, felodipine alone or when added to a beta-adrenergic blocker does not interfere with cardiac conduction.
Preliminary studies in patients with heart failure indicate that felodipine and amlopidine may improve hemodynamics, reduce neurohormonal activation, and increase exercise tolerance, but final conclusions must await the randomized clinical trials now underway
DRUGS RECOMMENDED FOR ROUTINE USE
Most patients with HF should be routinely managed with acombination of 3 types of drugs: a diuretic, an ACEI or an ARB, and a beta blocker .The value of these drugs has been established by the results of numerous large-scale clinical trials, and the evidence supporting a central role for their use is compelling and persuasive. Patients with evidence
of fluid retention should take a diuretic until aeuvolemic state is achieved, and diuretic therapy should be continued to prevent the recurrence of fluid retention.
Even if the patient has responded favorably to the diuretic, treatment with both an ACEI and a beta blocker should be initiated and maintained in patients who can tolerate them because they have been shown to favorably influence the long-term prognosis of HF.
Therapy with digoxin as a fourth agent may be initiated at any time to reduce symptoms,prevent hospitalization, control rhythm, and enhance exercise tolerance.
DIURETICS.
Diuretics interfere with the sodium retention of HF by inhibiting the reabsorption of sodium or chloride at specific sites in the renal tubules. Bumetanide,furosemide, and torsemide act at the loop of Henle (thus,they are called loop diuretics),whereas thiazides, metolazone, and potassium-sparing agents (e.g., spironolactone) act in the distal portion of the tubule .These 2 classes of diuretics differ in their pharmacological actions.
The loop diuretics increase sodium excretion up to 20% to 25% of the filtered load of sodium, enhance free water clearance, and maintain their efficacy unless renal function is severely impaired. In contrast, the thiazide diuretics increase the fractional excretion of sodium to only 5% to 10% of the filtered load, tend to decrease free water clearance, and lose their effectiveness in patients with impaired renal function (creatinine clearance less than 40 mL per min).
1. Patients should not be given an ACEI if
they have experiencedlife-threatening adverse reactions angioedema Or
anuric renal failure) during previous exposure to the drug or if they are pregnant.
2. caution if they have very low systemic blood pressures (systolic blood pressure less than 80 mm Hg), creatinine (greater than 3 mg perdL), bilateral renal artery stenosis, or elevated levels of serum potassium (greater than 5.5 mEq per liter).
3. should not be initiated in
hypotensive patients who are at immediate risk of cardiogenic shock.
Because fluid
retention can blunt the therapeutic effects and fluid depletion can potentiate the adverse effects of ACE ,healthcare providers should ensure that patients are being given appropriate doses of diuretics before and during treatment with these drugs.
Retrospective analyses of large-scale clinical trials have
suggested that aspirin might interfere with the benefits of ACE inhibition in patients with HF by inhibiting kinin Mediated prostaglandin synthesis. In short-term hemodynamic and maximal-exercise studies, aspirin can attenuate the hemodynamic actions of ACEIs in patients with HF ,an effect not seen with nonaspirin antiplatelet agents (e.g., clopidogrel)Sympathetic activation
can increase ventricular volumes and pressure by causing peripheral vasoconstriction and byimpairing sodium excretion by the kidneys
Norepinephrine can also induce cardiac hypertrophy,
provoke arrhythmias by increasing the automaticity
of cardiac cell, development of hypokalemia,
increase heart rate and potentiate the actions of other neurohormonal systems. Finally, by stimulating growth and oxidative stress in terminally differentiated cells, norepinephrine can trigger programmed cell death or apoptosis .These deleterious effects are mediated through actions on alpha-1–,beta-1–, and beta-2–adrenergic receptors .
long-term treatment with beta blockers can
lessen the symptoms of HF,improve the clinical status of patients,and overall sense of well-beingIn addition,like ACEIs, beta blockers can reduce the risk of death and the combined risk of death or hospitalization.
These benefits of beta blockers were seen in
patients with or without coronary artery disease and in
patients with or without diabetes mellitus, as well as in
women and black patients. The favorable effects of beta
blockers were also observed in patients already taking
ACEIs, which suggests that combined blockade of the 2
neurohormonal systems can produce additive effects.
Physicians may minimize the risk of hypotension by administering the beta blocker and ACEI at different times during the day.
PRACTICAL USE OF DIGITALIS IN HF (Heart failure).
Physicians may consider adding digoxin in patients withpersistent symptoms of HF during therapy with diuretics,
an ACEI (or ARB), and a beta blocker .Digoxin may also be added to the initial regimen in patients with severe symptoms who have not yet responded symptomatically during treatment with diuretics, an ACEI, and beta blockers. Alternatively, treatment with digoxin may be delayed until the patient’s response to ACEIs and beta blockers has been defined and be used only in patients who remain symptomatic despite therapy with the neurohormonal antagonists.
There is no reason to use loading doses of digoxin to initiate therapy in patients with HF.
Digoxin should be used with caution or not used at all in post-MI patients, particularly if they have ongoing ischemia
Current indications for cardiac transplantation focus on the identification of patients with
1.severe functional impairment or dependence on intravenous inotropic agents.
Less common indications include recurrent
2. life-threatening ventricular arrhythmias or angina that is refractory to all currently available treatments .HF itself is associated with
resistance to the actions of insulin ,and the resulting hyperinsulinemia may promote both cardiac and vascular hypertrophy and thus may hasten the progression of HF.Anticoagulation with warfarin is most justified in patients with HF who have experienced a previous embolic event or who have paroxysmal or persistent atrial fibrillation .
Despite recent advances in the management of patients with heart failure, morbidity and mortality rates remain high, with an
estimated 5-year mortality rate of 50%.
Most patients require more than one agent for optimal blood pressure control.
Guidelines recommend starting two drugs for blood pressures 20 mmHg or more above the desired goal.
Treatment of HTN with α-adrenergic blockade is generally restricted to patients with urinary tract obstruction or benign prostatic hyperplasia, since these drugs may increase the incidence of HF.
Carvedilol, sustained-release metoprolol and bisoprolol have been shown to improve overall and event-free survival of patients with mild-to-advanced HF and, thus, are approved for treating HF in the USA.
Carvedilol is distinguished by its blocking of β2- and α1-adrenergic receptors, in addition to β1-receptors, and by its antioxidant properties.
The administration of β-receptor blockers with intrinsic sympathomimetic activity, such as pindolol and acebutolol, should be avoided.
Less-ideal Agents
Some drugs are not recommended for HF patients. Calcium channel blockade does not improve symptoms and can worsen CHF and the risk of death in these patients. Amlodipine and felodipine neither improve nor worsen the survival of HF patients and, generally, would not be chosen before other drugs of known survival benefit. However, the American College of Cardiology (ACC), American Heart Association (AHA) and Heart Failure Society accept using amlodipine in HF patients with HTN because it may be safe and well tolerated.Conflicting data exist in the use of β-blockers for patients with HTN without HF and in patients with HFNEF.
Extensive data support the use of β-blockers in patients with HFREF, especially carvedilol and metoprolol.
DHF cannot usually be distinguished from SHF by patient history, physical exam, x-ray, and EKG alone. Diagnosis requires an estimate of LV size and EF. These measurements can be made using echo, MUGA, or cath. Really, DHF diagnosis is a matter of ruling out other possible causes in patients seeming to have heart failure but who have normal heart size and EF.Since echo does have limits for spotting DHF and cath is invasive, one trial studied whether the BNP blood test could help spot diastolic heart failure. It turns out that a quick BNP test can help a doctor diagnose DHF.
Several agents currently under investigation include
NebivololA third-generation, highly selective β1-receptor blocker that
also promotes endothelial nitric oxide production.HF patients with HTN tolerate this drug well. In patients with symptomatic HF and reduced systolic function, its hemodynamic effects are similar to carvedilol. A large trial showed that nebivolol reduced the composite end point of mortality and hospitalization in HF patients.
• Besides excluding
• SHF, it is also important to rule out mitral valve stenosis and chronic lung disease, both of which can imitate heart failure with a normal EF.
Digitalis may be given as tablets or capsules
Therapeutic index is very low so, low safety marginWide distribution to various tissues because of lipid solubility
{Advantage—reaches the target site very quickly, Disadvantage—goes to other tissues}
Digoxin mainly eliminated by the kidney (may be given to patients with liver diseases)
Digitoxin is mainly eliminated by hepatic metabolism (may be given to patients with renal failure)decreased impulse discharge/generation from the SA node and decrease impulse propagation through the AV node.
In general, cardiac glycosides slow conduction and increase the refractory period in specialized cardiac conducting tissue by stimulating vagal tone.
Digitalis has parasympathetic properties, which include hypersensitization of carotid sinus baroreceptors and stimulation of central vagal nuclei.
Digitalis
• Digitoxin
• Digoxin• Less polar and more lipid soluble
• More polar and less lipid soluble
• Easily crosses BBB
• Does not cross BBB
• Produces CNS symptom
• Does not produce CNS symptom
• ½ life is 5 days
• ½ life is 1½ days
• Heart : plasma ratio is 7:1
• Heart : plasma ratio is 30:1
• Mostly metabolized in the liver, so it’s excretion is independent of renal function
• More than 80% excreted unchanged via urine, rest is removed by non-renal routes like biliary excretion and hepatic metabolism
• Digitalization requires (4x5) 20 days
• Digitalization requires (4x1½) 20 days
• Differences between Digitoxin and Digoxin
Contraindication of Digoxin
1. Wolff Parkinson white (WPW)
2. In diastolic failure
3. Heart block
4. Previous history of stroke’s Adams syndrome
5. Obstructive cardiac myopathy
Treating heart failure in patients with an EF of 30% requires that beta-blocker dose be raised carefully, starting with tiny doses and raising it slowly over several months. In the DHF patient, that very slow rise in dose is not usually necessary.
Another example is calcium channel blockers. These drugs should not be used in systolic heart failure patients at all, but they may help DHF patients. As another example, diuretic use needs to be much more cautious in the DHF patient since drying them out too much can easily cause too-low blood pressure.
A fall in systolic blood pressure of at least 20 mm Hg or in diastolic blood pressure of at least 10 mm Hg within 3 minutes after standing, or a head-up tilt on a tilt table is a classic manifestation of sympathetic vasoconstrictor (autonomic) failure is diagnostic of orthostatic hypotension.
• The standard treatment for OH is a drug called midodrine, which helps to alleviate symptoms. However, standard doses of midodrine also raise blood pressure when people lie down. Now, researchers led by Phillip Low, M.D., of the Mayo Clinic in Rochester, Minnesota, have shown that another drug called pyridostigmine can alleviate many of the symptoms of OH, either alone or in combination with a low dose of midodrine.
• Midodrine and pyridostigmine both work by causing blood vessels to constrict. Midodrine causes this constriction continuously while it is in the bloodstream. On the other hand, pyridostigmine is thought to work by slowing breakdown of the nerve-signaling chemical acetylcholine, which is used by a cluster of nerve cells called the autonomic ganglion. The autonomic ganglion transmits signals from the central nervous system to the peripheral nervous system.
A recent meta-analysis of data from more than 90 000 participants from 14 randomised trials of statins concluded that
statin therapy can safely reduce the five year incidence of major coronary events, coronary revascularisation, and stroke by 20% per mmol reduction in LDL cholesterol level.
Q. What are the guidelines for antiplatelet therapy in secondary stroke prevention?
A. Current guidelines indicate that aspirin alone, clopidogrel, and aspirin plus dipyridamole are all acceptable first-line options in secondary stroke prevention.Randomized trials have shown no benefit, and increased hemorrhagic risks, with the combined use of clopidogrel and aspirin as compared with clopidogrel alone or aspirin alone for long-term secondary prevention after stroke.
N Engl J Med 2012