• Panorama 2
• In Medicineد. حسين محمد جمعة
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
When is it mandatory to admit a TB patient to the ward?
Admit your patient if he develops complications such as massive haemoptysis orpneumothorax, if you suspect your patient will be non-compliant to treatment, poor family
support or no proper home.
TB involving vital organs such as the brain, heart, adrenal glands, kidneys, spine etc also needs admission.
You can discharge your patient after 5 days of treatment if he tolerates anti-TB drugs, blood results are normal and you are satisfied with compliance after counseling.
THERE IS NO NEED TO KEEP TB PATIENTS IN THE WARD TILL THEY ARE SMEAR NEGATIVE OR DO DAILY SPUTUM AFB IN THE WARD. IT WILL TAKE AT LEAST ONE MONTH BEFORE SPUTUM AFB BECOMES NEGATIVE.
Advise your patient to wear a surgical mask upon discharge to minimize transmission to his family at
home while he is taking TB treatment.
My patient has TB but she is pregnant, are the TB drugs safe in pregnancy?
Just give EHRZ. Streptomycin is contraindicated in pregnancy.
My patient has TB but has renal failure; what regimen do I give?
Just use HRZ regimen and prolong the duration of treatment. Streptomycin and Ethambutol are
contraindicated in renal failure.
In cases of isolated elevation of alkaline phosphatase, γ‑glutamyl transpeptidase (GGT) should be obtained; levels are elevated in hepatobiliary disease but not if the high alkaline phosphatase level is due to a bone disorder.
• Causes of an absent knee and ankle reflex with extensor plantars ((upper and lower motor neurone lesion)): 1. subacute combined degeneration of the spinal cord 2. motor neurone disease 3. syphilitic tabo-paresis 4. Friedreich's ataxi5. conus medullaris or cauda equina lesion - at the conus medullaris the spinal root entry zones and the pyramidal tracts are in close proximity - they may be damaged by a small lesion such as a neurofibroma 6. multiple sclerosis - involvement of the corticospinal tract leads to hyperreflexia and extensor plantars. Severe sensory involvement may break the reflex arc, and the reflexes disappear 7. pellagra 8. diabetes mellitus + cervical myelopathy
• 9. spinal cord compresion at the 3rd and 4th lumber levels
• Delayed relaxation phase of deep tendon reflexes
• Differential Diagnosis• hypothyroidism
• neurosyphilis
• parkinsonism
• pernicious anemia
• sarcoidosis, myasthenia gravis
• schizophrenia
• diabetes mellitus
• glucose administration
• sprue
• medications (propranolol, procainamide, reserpine, potassium), hypothermia, leg edema, normal puerperium, female sex, age
• Pulsus paradoxus
• decreased right heart functional reserve, e.g. myocardial infarction and tamponade.
• right ventricular inflow or outflow obstruction, e.g. superior vena cava obstruction and pulmonary
• embolism, and decreased blood to the left heart due to lung hyperinflation (e.g. asthma, COPD)
• and anaphylactic shock.
• List of causes
• Cardiac:
• cardiac tamponade
• pericardial effusion
• pulmonary embolism
• cardiogenic shock
• Pulmonary:
• tension pneumothorax
• asthma
• Non-pulmonary and non-cardiac:
• anaphylactic shock
• superior vena cava obstruction
Medications That May Cause Lymphadenopathy
Allopurinol (Zyloprim) Atenolol (Tenormin) Captopril (Capozide) Carbamazepine (Tegretol) Cephalosporins Gold Hydralazine (Apresoline)Penicillin Phenytoin (Dilantin) Primidone (Mysoline) Pyrimethamine (Daraprim) Quinidine Sulfonamides Sulindac (Clinoril)
Adapted with permission
Matting. A group of nodes that feels connected and seems to move as a unit is said to be "matted." Nodes that are matted can be either benign (e.g., tuberculosis, sarcoidosis or lymphogranuloma venereum) or malignant (e.g., metastatic carcinoma or lymphomas).
Supraclavicular lymphadenopathy has the highest risk of malignancy, estimated as 90 percent in patients older than 40 years and 25 percent in those younger than age 40. Having the patient perform a Valsalva's maneuver during palpation of the supraclavicular fossae increases the chance of detecting a node. Lymphadenopathy of the right supraclavicular node is associated with cancer in the mediastinum, lungs or esophagus. The left supraclavicular (Virchow's) node receives lymphatic flow from the thorax and abdomen, and may signal pathology in the testes, ovaries, kidneys,
Although rarely present, a paraumbilical (Sister Joseph's) node may be a sign of an abdominal or pelvic neoplasm. pancreas, prostate, stomach or gallbladder.
Biopsy should be avoided in patients with probable viral illness because lymph node pathology in these patients may sometimes simulate lymphoma and lead to a false-positive diagnosis of malignancy.
• What are a couple's chances of having a child with Down syndrome?In the usual circumstance, the chances depend upon the age of the mother. The odds of having a child with Down syndrome at age 35 are approximately 1 in 350. Under age 25, the odds are about 1 in 1400 and at age 40 the odds are about 1 in 100. (Thompson, et al., 1991)
• The chances of a parent of a child with Trisomy 21 having another child with Down syndrome is approximately 1 in 100.
• If the child has a translocation, the recurrence risk can be as high as 100% or as low as 2%. Parents of children with translocation type of Down syndrome should have chromosome analysis to detect a carrier state.
• Hyperprolactinaemia – drugs that are responsible
• include dopamine antagonists:• Antipsychotics (Haloperidol, Sulpiride)
• Metoclopramide
• Domperidone
• SSRIs
Except in neonates, a tuberculin skin test should always be done before administering BCG. A reactive tuberculin skin test is a contraindication to BCG. Someone with a positive tuberculin reaction is not given BCG, because there is a high risk of severe local inflammation and scarring, not because of the common misconception that tuberculin reactors "are already immune" and therefore do not need BCG.
People found to have reactive tuberculin skin tests should be screened for active tuberculosis.
Roughly, transudates are a result of increased pressure in the portal vein(>8 mmHg, usually around 20 mmHg), e.g. due to cirrhosis, while exudates are actively secreted fluid due to inflammation or malignancy. As a result, exudates are high in protein, high lactate dehydrogenase , have a low PH (<7.30), a low glucose level, and more white cell .
Transudates have low protein (<30g/L), low LDH, high pH, normal glucose, and fewer than 1 white cell per 1000 mm³. Clinically,
the most useful measure is the difference between ascitic and serum albumin concentrations. A difference of less than 1 g/dl (10 g/L) implies an exudate.
Imaging
Cerebral infarction cannot be distinguished with certainty from intracerebral hemorrhage on the basis of symptoms and signs alone. In all patients with suspected ischemic stroke, (CT) or (MRI) of the brain is therefore required.Both CT and MRI have a high sensitivity for acute intracranial hemorrhage, but MRI has a much higher sensitivity than CT for acute ischemic changes, especially in the posterior fossa and in the first hours after an ischemic stroke.
Febrile seizures
defined as seizures associated with fever in the absence of central nervous system infection or acute electrolyte imbalance in a young child. The prevalence of febrile seizures is between 3% and 8% in children up to 7 years of age.• Febrile seizures are the most common seizure disorder .
• They are benign and have a normal cognitive outcome.• Febrile seizures recur in a third of children and are associated with a low risk of epilepsy.
• Risk factors for epilepsy include complex febrile seizure, neurological abnormality, and family history of epilepsy.
• Febrile seizures are prolonged in 9% of cases; these should be treated with buccal or intranasal midazolam
Febrile seizures result from a combination of genetic and environmental factors.
Of children with febrile seizures, 24% have a family history of febrile seizures and 4% have a family history of epilepsy. Although polygenic inheritance is usual, a small number of families exist in whom the inheritance of febrile seizures is autosomal dominant, a temperature of at least 38°C.
Febrile seizures are defined as occurring between 6 months and 6 years of age
Febrile seizures may occur before the fever is apparent and early or late in the course of a febrile illness . An entity of afebrile convulsions in young children with mild gastroenteritis is increasingly recognised .
Febrile seizures are predominantly brief, generalised tonic-clonic seizures, and 4-16% have focal features . In 87% of children, the duration of the febrile seizure is less than 10 minutes
Thirty per cent of children have recurrent febrile seizures during subsequent illnesses.
Risk factors for recurrence
include onset before 18 months, lower temperature close to 38°C, shorter duration of fever (<1 hour) before the seizure, and a family history of febrile seizures
Of children who have all these risk factors, 76% will have a recurrence of febrile seizure compared with 4% without risk factors.
Complex febrile seizures
are defined by at least one of the following features: duration longer than 15 minutes, multiple seizures within 24 hours, and focal features. These features are absent in simple febrile seizures, which make up 75% of attacks.Children with a history of at least one complex feature, a neurological abnormality, and a family history have a 10% risk of developing epilepsy by the age of 7. Prolonged febrile seizures increase the incidence of epilepsy to 21%. For children with all three features of a complex febrile seizure, the risk increases to 49%.
Febrile seizures have an excellent outcome; population studies show normal intellect and behaviour, even for children with complex febrile seizures
Lumbar punctureWhen the clinical history suggests meningitis, a lumbar puncture should be done unless contraindications such as signs of raised intracranial pressure with altered conscious state, focal neurological signs, cardiorespiratory compromise, a bleeding diathesis, or infection in the area the needle will traverse are present. Antibiotics should be started if
a contraindication to lumbar puncture is present.
Meningitis is rare (0.23%) in children presenting with seizures and fever in the developed world. Nevertheless, meningitis presents with seizures in 24% of children.
In the vast majority of children, meningitis can be ruled out on clinical grounds, rendering a lumbar puncture unnecessary. Meningitis is very unlikely in children over the age of 2 years in the absence of a complex febrile seizure, meningeal irritation, or petechiae.
Children under 2 with meningitis without meningism usually show other features such as being unwell for a few days, vomiting, drowsiness, petechiae, decreased feeding, or complex febrile seizures.
ElectroencephalographyNo evidence exists that epileptiform discharges in children with febrile seizures have any diagnostic or prognostic implications, even in the subgroup with complex febrile seizures
Imaging Non-urgent magnetic resonance imaging should be considered in children with recurrent complex febrile seizures who have other neurological findings, including abnormal head circumference, significant developmental delay, and persistent focal neurological abnormality.
Management
Reassurance about the cause and prognosis of this disorder can alleviate the anxiety and let the family return to normal life.Acute treatments such as rectal diazepam (0.5 mg/kg) and buccal (0.4-0.5 mg/kg) or intranasal (0.2 mg/kg) midazolam are effective and can be administered at home for a seizure lasting longer than five minutes. trials have shown that midazolam has superior efficacy to diazepam.
Paracetamol and ibuprofen are often useful in relieving the discomfort of a febrile child. no evidence exists that this decreases recurrence of febrile seizures.
No compelling evidence exists that continuous anticonvulsant drugs reduce the risk of epilepsy developing, and considerable potential side effects exist. Given the benign prognosis of febrile seizures, prophylactic treatment is not indicated.
trials have found that diazepam given during a fever reduces recurrence of febrile seizures
Chronic persistent hiccups is a rare but distressing condition most frequently associated with serious underlying health problems of peripheral (esophagogastric irritational noxae, chest tumors, etc) and central (cerebral ischemia, cerebral expanding lesions especially in the posterior fossa, etc)
Nefopam (3,4,5,6- Tetrahydro-5-methyl-l-phenyl-1H-2.5-benoxazocine) is a centrally acting non-opioid analgesic agent that has anti-shivering properties, structurally related to antihistamine and anti-parkinsonian drugs (orphenadrine) .
Nefopam for chronic persistent hiccups
Treatment of Vasomotor Symptoms
EstrogensMultiple randomized trials have demonstrated that estrogen markedly improves the frequency and severity of hot flushes, generally reducing the frequency by 80 to 95%. All types and routes of administration of estrogen are effective. Relief is usually substantial within 4 weeks after starting standard doses of estrogens (1 mg per day of oral estradiol or its equivalent).
Both estrogen alone and estrogen plus progestin increased the risk of stroke by 40%. Although the two regimens were not compared directly, estrogen with added progestin appeared to be associated with a higher risk of coronary events, pulmonary embolism, and breast cancer than was estrogen alone.
However, treatment with unopposed estrogen in women with a uterus markedly increases the risk of uterine hyperplasia and cancer.
Estrogen should be avoided in women who have a history of or are at high risk for
• cardiovascular disease,• breast cancer,
• uterine cancer, or
• venous thromboembolic events and in those with
• active liver disease.
• Whether lowering diastolic blood pressure is harmful to some patients with isolated systolic hypertension is uncertain. Myocardial perfusion occurs during diastole, and excessive reduction of diastolic pressure could be detrimental in those with coronary artery disease.
• Several studies have suggested that a diastolic pressure below 60 mm Hg, particularly in patients with documented coronary disease, may be associated with an increased risk of myocardial infarction and death (the so-called J-curve phenomenon) .
• The effects of treating hypertension in patients older than 80 years of age are unclear because few intervention studies have been performed in hypertensive patients in this age group .
Cushing's syndrome without excess cortisol
In patients taking inhaled corticosteroids the biochemical detection of a suppressed hypothalamicpituitary-adrenal axis is well documented. Fluticasone propionate is the most potent inhaled glucocorticoid, and adrenocortical insufficiency has been reported in 12% of patients on a high dose of inhaled fluticasone. The incidence of addisonian crises is lowerItraconazole is an orally active antifungal triazole that inhibits cytochrome P450 dependent CYP3A4 and consequently decreases the clearance of synthetic glucocorticoids.
The combination of long term inhaled steroid with oral itraconazole may exacerbate suppression of the hypothalamic-pituitary-adrenal axis
Clinicians and patients have been discouraged from using methotrexate, however, because of the need for routine liver biopsies to detect, albeit rare, clinically and biochemically silent liver fibrosis and cirrhosis.
Recently, measurement of serum procollagen III (every three months during treatment) has been adopted as a surrogate marker of liver toxicity and means that most patients can avoid liver biopsies.
Biological treatments
Block molecular steps important in the pathogenesis of psoriasis.Currently they comprise two main groups:
agents that target the cytokine tumour necrosis factor
(etanercept, infliximab, adalimumab)
agents that target T cells or antigen presenting cells (efalizumab).
parenteral administration (intravenously every eight weeks for infliximab, self administered subcutaneous injections twice weekly, weekly, or every two weeks for the others),
with severe disease these treatments can be life saving. Risks of infection (especially tuberculosis with the antitumour necrosis factor agents) and possible future malignancy remain concerns .
• The most promising new anti-inflammatory agents for use in COPD are phosphodiesterase 4 (PDE4) inhibitors.
These orally active drugs increase cyclic AMP concentrations in inflammatory cells and exhibit a broad spectrum of anti-inflammatory effects
New anti-inflammatory treatments
Although effective in animal models of COPD, PDE4 inhibitors (such as cilomilast and roflumilast) have so far proved disappointing in clinical trials. This is because the dose is limited by adverse effects—particularly nausea and gastrointestinal problems. However, in a large randomised, placebo controlled study of patients with COPD with a mean FEV1 of around 50%, treatment with roflumilast reduced exacerbations and improved lung function over a 24 week period. Diarrhoea was the most common adverse effect largely due to active treatment and occurred in roughly 5% of patients.
More selective inhibitors (PDE4B inhibitors) or inhaled administration of drugs are being investigated as ways to circumvent the problem of adverse effects.
Upper gastrointestinal events (UGIE), symptomatic or complicated ulcers, occur in 1 of every 20 NSAID users and in 1 of 7 older adults using NSAIDs, accounting for 30% of UGIE related hospitalizations and deaths. Inhibition of the COX-1 pathway blocks production of prostaglandins that play an important protective role in the stomach by increasing mucosal blood flow and stimulating the synthesis and secretion of mucus and bicarbonate, as well as promoting epithelial proliferation. Accordingly, the inhibition of these prostaglandins impairs these protective factors, resulting in a gastric environment that is more susceptible to topical attack by endogenous factors, such as acid, pepsin, and bile salts.
• Because COX-2 is the primary intended target for antiinflammatory drug therapy, agents that selectively block COX-2, while having little to no effect on COX-1, should result in effective pain relief with reduced GI toxicity. This concept, called the “COX-2 hypothesis,” has been challenged by data from animal studies, which indicated that both COX-1 and COX-2 must be inhibited for gastric ulceration to occur. Interestingly, while the selective inhibition of either COX-1 or COX-2 alone failed to cause gastric damage, inhibition of both COX isoforms produced gastric ulceration. Thus, the explanation for reduced GI toxicity for COX-2–specific inhibitors may be their lack of dual COX inhibition rather than their COX-1–sparing effects.
• The level of acid suppression provided by traditional doses of H2-receptor antagonists (H2RAs) does not prevent most NSAID-related gastric ulcers. There are little data on their use in conjunction with ASA.
• In the acute setting following successful endoscopic and medical treatment of major GI hemorrhage, it seems prudent, following discussion among the specialties, to briefly discontinue antiplatelet therapy until lack of rebleeding is observed in the intensive care unit setting. The optimal duration for cessation of antiplatelet therapy leading to a balance of GI and cardiovascular outcomes has not been established by clinical trials. The current efficacy of endoscopic therapy for ulcer bleeding combined with intravenous continuous infusion PPI therapy suggests that reintroduction of antiplatelet therapy in such high-cardiovascular-risk patients is reasonable in those who remain free of rebleeding after 3 to 7 days.
• The estimated average excess risk of UGIE related to cardioprophylactic doses of ASA is 5 cases per 1000 ASA users per year. Among elderly patients, the odds ratios (ORs) of bleeding with daily doses of ASA of 75, 150, and 300 mg are 2.3, 3.2, and 3.9, respectively.
• COX
• Expression• Function
• Inhibitors
• COX-1
• constitutively throughout the body
• organ pain, platelet function, stomach protection
• NSAIDs including aspirin
• COX-2
• Inducible and constitutively in brain, kidney
• Inducible: inflammation, pain, feverConstitutive: synaptic plasticity
• COX 2 inhibitors celecoxib (Celobrex )
• COX-3
• Constitutively, high in brain, heart
• pain pathways, not inflammation pathways
• acetaminophen some NSAIDs
• The effect as "quite considerable." For example, for rofecoxib (Vioxx, Merck), the number of patients needed to treat for one year to cause one death was just nine, and the corresponding number for celecoxib (Celebrex, Pfizer) was 14 and diclofenac 11. "These numbers are very low," Gislason said, noting that for antihypertensive drugs, the number needed to treat for one year to save one life is in the range of 50 to 100. "Everyone agrees that it is worth treating hypertension. So the harmful effect of some NSAIDs is much greater than the beneficial effect of antihypertensive treatment."
No clinically significant differences have been demonstrated between traditional NSAIDs and Cox-2 agents (i.e., fluid retention, edema and ↑ blood pressure.) NSAIDs prevent the production of prostaglandins, molecules which dilate the afferent arteriole.
NSAIDs could therefore worsen kidney function by decreasing afferent blood flow to the Bowman's capsule.
Renal Effects
OBSTRUCTIVE
AsthmaChronic obstructive lung disease
(chronic bronchitis, emphysema)
Bronchiectasis
Cystic fibrosis
Bronchiolitis
RESTRICTIVE—PARENCHYMA
Sarcoidosis
Idiopathic pulmonary fibrosis
Pneumoconiosis
Drug- or radiation-induced
interstitial lung disease
RESTRICTIVE—EXTRAPARENCHYMAL
Neuromuscular
Diaphragmatic weakness/paralysis
Myasthenia gravis
Guillain-Barre´ syndrome
Muscular dystrophies
Cervical spine injury
Chest wall
Kyphoscoliosis
Obesity
Ankylosing spondylitis
Common Respiratory Diseases by Diagnostic Categories
• Two major patterns of abnormal ventilatory function are restrictive and obstructive
• In obstructive pattern:
• Hallmark is decrease in expiratory flow rate, i.e., FEV1.
• Ratio FEV1/FVC is reduced.
• TLC is normal or increased.
• RV is elevated due to trapping of air during expiration.
• In restrictive disease:
• Hallmark is decrease in TLC.
Although there was initially concern about cardiovascular risks with all anticholinergics, safety trials demonstrated that there is no increased cardiovascular risk associated with tiotropium.
However, data indicate that ipratropium is associated with a slight risk for excess cardiovascular mortality.
Both Spiriva (Tiotropium) and Ipratropium (Atrovent) are anticholinergic agents that are used for maintenance treatment of bronchospasm associated with COPD (Chronic Obstructive Pulmonary Disease). Spiriva has an additional indication for reducing COPD exacerbations based on the outcomes of the large UPLIFT clinical trial. Both medications are not indicated for acute treatment of a bronchospasm and should never be used as rescue medications. The major difference between the two drugs is that Spiriva is a long acting medication and Ipratropium is a short acting drug. Spiriva is used once daily, while Ipratropium may be used every 4 to 6 hours.
How does MODY present clinically?
Patients with MODY typically display one or more of the following features:• A strong family history of diabetes (of any type),
• Onset of diabetes in the second to fifth decade,
• Insulin independence (although insulin may be needed for optimal control),
• Absence of features of insulin resistance, such as acanthosis nigricans, abnormal fat distribution (lipodystrophy), central obesity, and dyslipidaemia
• , and absence of β cell autoimmunity.
The specific genetic subtype of MODY determines the clinical presentation, prognosis, and treatment response.
Which patients diagnosed with type 1 diabetes should be referred for genetic testing?
Patients with MODY who present at a young age may be
misdiagnosed as having type 1 diabetes and inappropriately treated with insulin.
In type 1 diabetes, autoimmune destruction of the β cells results in complete insulin deficiency within three to five years of diagnosis (the “honeymoon period”), whereas some β cell function is maintained in MODY. Consider MODY in patients with evidence of continued endogenous insulin secretion (for example, persistent C peptide production, low insulin dose (<0.5 units/kg/day), and no tendency to ketoacidosis when insulin is omitted) three to five years after diagnosis with apparent type 1 diabetes.
Evidence of continued endogenous insulin secretion (for example,
• persistent C peptide production,• low insulin dose (<0.5 units/kg/day), and
• no tendency to ketoacidosis when insulin is omitted)
Which patients diagnosed with type 2 diabetes should be referred for genetic testing?
In contrast to type 2 diabetes, patients with MODY have β cell dysfunction that typically occurs in the absence of insulin resistance. Thus, patients with young onset (<45 years) of apparent type 2 diabetes, who do not have features of insulin resistance, may have MODY. Clinical features such as• acanthosis nigricans,
• central obesity,
• hypertension, and
• dyslipidaemia can be used as surrogate markers of insulin resistance in everyday clinical practice.
Aspirin therapy should be instituted for diabetic patients when the 10-year risk for a cardiovascular event exceeds 10%.
This parameter should include men older than 50 years with diabetes and women older than 60 years with diabetes if they have 1 additional cardiovascular risk factor. Such risk factors include hypertension, dyslipidemia, smoking, albuminuria, or a family history of cardiovascular disease.
Definitions of Microalbuminuria and Macroalbuminuria
• Parameter• Normal
• Micro- albuminuria
• Macro- albuminuria
• Urine AER
• (g/min)
• < 20
• 20 - 200
• >200
• Urine AER
• (mg/24h)
• < 30
• 30 - 300
• >300
• Urine albumin/
• Cr# ratio (mg/gm)
• < 30
• 30 - 300
• >300
AER=Albumin excretion rate CR# =creatinine
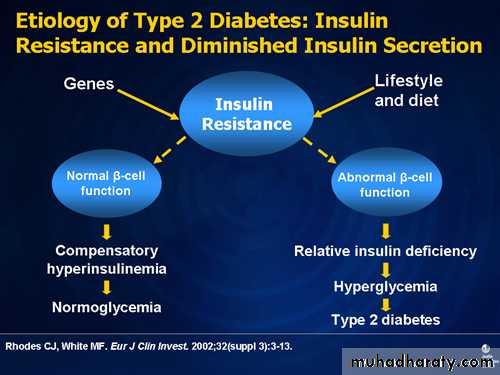
In terms of the pathophysiology of type 2 diabetes, we all understand that the insulin resistance state is very common. Ninety percent of patients who have type 2 diabetes have insulin resistance, whether it is genetically determined or whether environmental factors or a sedentary lifestyle and obesity add to the insulin-resistant state.
If you add to that beta-cell dysfunction, then you have relative insulin deficiency that ultimately leads to hyperglycemia and type 2 diabetes. On the other hand, not every patient who has insulin resistance or is obese has diabetes. There is compensatory hyperinsulinemia, and there is maintenance of normal glycemic states. It is the insulin resistance plus the abnormal beta-cell function that ultimately leads to diabetes.
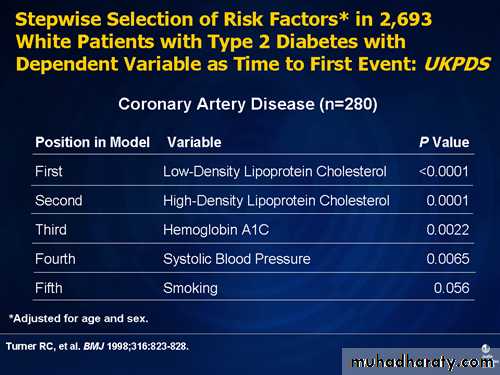
From the United Kingdom Prospective Diabetes Study (UKPDS), we know that if you want to predict who is going to get an MI, LDL-C is still the number one variable. So for the time to the first heart attack, LDL-C predictors are the best. Second was HDL-C. Hemoglobin A1C was third, and systolic blood pressure was fourth. So it is still extremely important, from the perspective of lowering cardiovascular risk, to lower the LDL-C parameters .
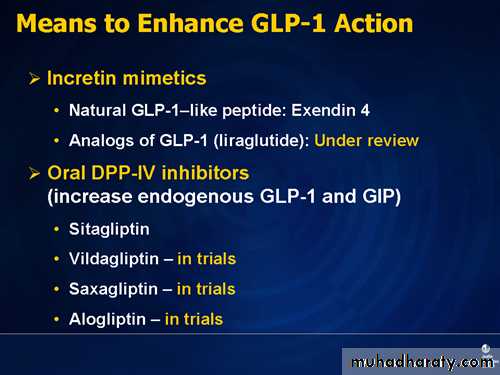
A relatively new approach in type 2 diabetes pharmacotherapy is the result of understanding
incretin physiology. Briefly, after eating a meal, certain gut hormones are released that sensitize the beta cell to secrete more insulin. One of the most important gut hormones is
glucagon-like peptide-1 (GLP-1), which goes into the circulation and stimulates insulin secretion in a glucose-dependent manner.
In addition, this pathway has the added benefit of suppressing glucagon secretion, which has a role in the pathophysiology of diabetes. GLP-1 is also involved in slowing gastric emptying and in working on the central nervous system causing early satiety, leading to some beneficial effects in glycemic control. The problem is that GLP-1 is very rapidly degraded through the very important enzyme, DPP-IV. This leads to rapid inactivation of GLP-1, making its use impractical in patients who have type 2 diabetes.
Coming back to this pathway of GLP-1 degradation through DPP-IV, one of the ways to use this physiologic knowledge is to develop a drug that might block DPP-IV activity, which has been done with the DPP-IV inhibitors. They sustain GLP-1 level in the circulation longer, which then stimulates pancreatic insulin secretion and suppresses glucagon secretion.
Another strategy that one can employ is to develop a GLP-1-like substance synthetically that is not recognized by DPP-IV. That is the approach underlying the GLP-1 analogs that are not degraded through this pathway, and you can then use that substance in the treatment of type 2 diabetes.
The oral dipeptidyl peptidase-4 (DPP-4) inhibitor sitagliptin (Januvia) slows the degradation of endogenous GLP-1.
Incretin mimetics are alternatives to sulfonylureas or thiazolidinediones when diabetes is not controlled by metformin alone.
They also recommend an "angled injection with a pinched skin fold for children, while in adults the technique should be left to patient preference."According to Dr. Schwartz, the angle at which the 5-mm needle is inserted is important, depending on how much subcutaneous fat is available. "If the patient is obese, a 90° insertion with a 5-mm needle will get insulin into the subcutaneous fat. With children or thin adults with very little subcutaneous fat, a 45° insertion may be more appropriate,"
In the treatment of diabetes the term basal rate simply means the low rate of insulin supply needed to cover the basal metabolic functions of daily living
(i.e. breathing, heart rate, and other metabolic processes of the body). That is, what insulin is needed to maintain good blood sugar control without taking into account eating any food .
(food is covered with a “bolus" of insulin).
Usually, one unit of regular or rapid acting insulin per 15 grams of carbs is a good starting point. This may be adjusted according to individual need. A bolus of regular insulin should be injected (or released via the pump) 1/2 hour before the meal.
Rapid-acting insulins should be givenat the start of the meal.
Monitoring PPG is also important because it has been shown to be a significant and independent risk factor for macrovascular events in patients with diabetes. Being able to target the testing may not add extra tests to the total number done per week or month. If patients know that they lose control after every meal, the information will help them to modify their carbohydrate intake. This change will help to lower postmeal hyperglycemia and the A1C level.
In healthy, nondiabetic subjects, 2-h postprandial blood glucose levels are usually <120 and rarely >140 mg/dl. Glucose levels peak at 1h after the start of the meal and then return to preprandial levels within 2–3 h. This rise and fall of postprandial glucose levels is mediated by the first-phase insulin response, in which large amounts of endogenous insulin are released, usually within 10 min, in response to nutrient intake. In individuals with type 2 diabetes, the first-phase insulin response is severely diminished or absent, resulting in persistently elevated postprandial glucose throughout most of the day.
Limitations of A1C as the recommended means of diagnosing diabetes
The A1C assay is the test of choice for the chronic management of diabetes and is now being recommended for its diagnosis; Although the discussion above argues for using the A1C assay for the diagnosis of diabetes in nonpregnant individuals, there are patient conditions that either will require a specific A1C assay method or will preclude A1C testing.
First, some hemoglobin traits, such as HbS, HbC, HbF, and HbE, interfere with some A1C assay methods .
Currently, many assay methods can correct for the presence of the most common hemoglobin traits .and affinity assays that are unaffected by hemoglobin traits may be used .
Second, any condition that changes red cell turnover, such as hemolytic anemia, chronic malaria, major blood loss, or blood transfusions, will lead to spurious results..
Third, A1C levels appear to increase with age ,but the extent of the change, whether it relates to factors other than glucose metabolism, and the effect of the age-related increases on the development of complications are not sufficiently clear to adopt age-specific values in a diagnostic scheme.
Similarly, racial disparities in A1C, based on putative differences in the relationship between glucose levels and A1C, have been suggested ,however, here too, their etiology and significance are unclear, and it is premature to establish race-specific diagnostic values. Finally, there are rare clinical settings, such as rapidly evolving type 1 diabetes, where the A1C level will not have had time to “catch up” with the acute elevations in glucose levels; however, in these very rare cases, diabetes should be diagnosable with typical symptoms and casual glucose levels >200 mg/dl (11.1 mmol/l) despite a nondiagnostic A1C level.
2009 by the American Diabetes Association
• Low-dose aspirin (75–162 mg daily) "is reasonable" for patients with 10-year cardiovascular disease (CVD) risk >10% and no risk factors for bleeding. This group would include most diabetic men older than 50 and women older than 60 who have at least one additional major risk factor (i.e., smoking, hypertension, dyslipidemia, family history of premature CVD, or albuminuria).
• Aspirin "should not be recommended" for diabetic men younger than 50 and women younger than 60 with no other risk factors (10-year CVD risk, <5%).
• Aspirin "might be considered" for those at intermediate risk (10-year CVD risk, 5%–10%); this group would include younger patients with, and older patients without, other risk factors.
Bardoxolone Methyl and Kidney Function
in CKD with Type 2 DiabetesBardoxolone methyl, an oral antioxidant inflammation modulator, has shown efficacy in patients with CKD and type 2 diabetes. Patients receiving bardoxolone methyl had significant increases in the mean (±SD) estimated GFR, as compared with placebo, at 24 weeks (with between-group differences per minute per 1.73 m2 of 8.2±1.5 ml in the 25-mg group, 11.4±1.5 ml in the 75-mg group, and 10.4±1.5 ml in the 150-mg group; P<0.001). The increases were maintained through week 52, with significant differences per minute per 1.73 m2 of 5.8±1.8 ml, 10.5±1.8 ml, and 9.3±1.9 ml, respectively. Muscle spasms, the most frequent adverse event in the bardoxolone methyl groups, were generally mild and dose-related. Hypomagnesemia, mild increases in alanine aminotransferase levels,and gastrointestinal effects were more common among patients receiving bardoxolone methyl.
In conclusion, patients with advanced CKD
and type 2 diabetes who received treatment with bardoxolone methyl had sustained increases inthe estimated GFR throughout the 52-week study
period, a finding that is consistent with an improvement in kidney function. Thus, bardoxolone
methyl appears to be an attractive therapeutic candidate for further study in patients with CKD.
NEJM June 25, 2011
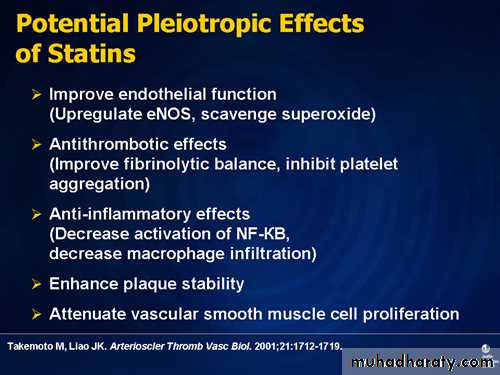
imaging trials have shown that intensive statin regimens with either atorvastatin, 80 mg daily, or rosuvastatin, 40 mg daily slow the progression of coronary atherosclerosis and may even result in disease regression in some patients.
Accordingly, guidelines for cardiovascular
disease prevention have increasingly emphasized
that lowering LDL cholesterol levels with
statins is the primary goal of lipid-modulating
therapy.
Atorvastatin and rosuvastatin are the most
effective statins for lowering LDL cholesterol levels,yielding average reductions that approach 50% foratorvastatin and exceed 50% for rosuvastatin. Direct comparisons have shown greater reductions in LDL cholesterol levels and greater increases in HDL cholesterol levels with rosuvastatin
Testosterone Risks
Recent studies reviewed in Drug Topics show that testosterone replacement therapies may increase the chances of prostate cancer in men. The study's authors believe that many doctors are prescribing replacement therapy without considering long-range risks and without a true diagnoses of hypogonadism which is an actual defect in the male gonads. Other risks of testosterone treatment in men of any age include acne, cardiovascular disease, testicular atrophy, and benign enlargement of the prostate.Testosterone is made by the testicles. A small amount also is made by the adrenal glands. (In women, small amounts of testosterone are made by the ovaries.)
Testosterone production is controlled by gonadotropin-releasing hormone (GnRH),pituitary gland makes luteinizing hormone (LH), which signals the testicles to make testosterone. When there is enough testosterone, the hypothalamus sends a message to the pituitary glad to stop making LH, and the testicles slow down production of testosterone. In an adult male, about
7 mg of testosterone is made each day.
• Clinicians cannot rely exclusively on physical examination to confirm or rule out hypothyroidism. Patients with suspected hypothyroidism require a diagnostic workup that includes thyroid hormone assays.
• The combination of signs that had the highest likelihood ratios (coarse skin, bradycardia and delayed ankle reflex) was associated with modest accuracy .
• The reflex changes corrected with treatment, even before the TSH returned to normal.
Three efficacious treatments are available for hyperthyroidism.
Radioiodine therapy and surgery
are considered definitive therapies, since the primary goal of this approach to treatment is to
destroy hyperfunctioning thyroid tissue. Antithyroid drugs (methimazole, carbimazole, and propylthiouracil) are used in one of two ways.
On occasion before radioiodine administration
And usually before surgery, several weeks of treatment with an antithyroid drug is administered to achieve a euthyroid state. Antithyroid drugs are
also used in Graves’ hyperthyroidism for 1 to 2
years, or longer, with the hope of achieving a remission.
Remission of hyperthyroidism is not
expected when antithyroid drugs are used during
the long-term treatment of toxic adenoma or toxic
multinodular goiter;
in these cases, early definitive
therapy with radioiodine or surgery is indicated.
Classification of esophageal varices
GradeEndoscopic appearance
I.
Dilated venes (< 5mm) still at the level of the surrounding tissue
II.
Dilated, straight venes (> 5 mm) protruding into the esophageal lumen but not obstructing it
III.
Large, tense and winding venes already obstructing the esophageal lumen considerably
IV.
near complete obstruction of the esophageal lumen with impending danger of hemorrhage (cherry red spots)
case reports have speculated about a possible link between use of proton pump inhibitors and intestinal infections—especially Clostridium difficile—deficiencies of nutrients like folate and vitamin B12, and osteoporosis. Proton pump inhibitors also reduce the effectiveness of clopidogrel, and co-administration of the two drugs should be avoided if possible.
Types of Dietary Fiber
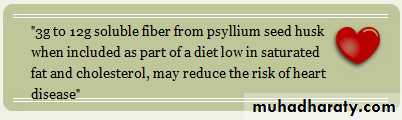
Insoluble fiber is the type of dietary fiber found in high-fiber foods like whole grains, nuts, wheat bran and vegetables. Insoluble fiber does not dissolve in water so it helps to move material through the colon faster by increasing the bulk of the stool. This can be very helpful to people who suffer from constipation or irregularity. Diets high in insoluble fiber may also decrease the risk of diabetes.Soluble fiber is also found in many high-fiber foods like oats, citrus fruits as oranges and apples ,Vegetables such as carrots ,barley, psyllium, flax seeds and beans. Soluble fiber absorbs water, which helps to soften stools making them easier to eliminate from the body. Some soluble fibers, like beta glucan found in oats, bind to bile acids in the intestinal tract. Bile acids contain cholesterol and normally your body reabsorbs some of those bile acids, but when their bound to beta-glucan, they are eliminated through the stool. This reduces the amount of bile reabsorbed into your blood, and in turn helps to lower cholesterol levels. high-fiber foods are usually high in vitamins and minerals as well.
• The requirement of 5 g/dL of reduced (ie, deoxygenated) hemoglobin in the capillaries translates into a reduced hemoglobin content of 3.4 g/dL in arterial blood. For this reason, patients with normal hemoglobin manifest cyanosis at higher SaO2 values than patients with anemia. consider the following examples:
• A patient whose hemoglobin content is 15 g/dL (hematocrit 45%) would not generate 5 g/dL of reduced (ie, deoxygenated) hemoglobin in the capillaries until his/her
• SaO2 level reached 85% (PaO2 50 mm Hg).
• Generation of Cyanosis
• Normal Results
• The following values represent the
• percentage of hemoglobin derivatives based
• on total hemoglobin:
• Carboxyhemoglobin: 3% (but may be as
• high as 15% in smokers)
• Methemoglobin: less than 3%
• Sulfhemoglobin: undetectable
• Cyanosis is commonly caused by either an excess of
• deoxygenated hemoglobin( > 5 g/dL)• methemoglobin (>1.5 g/dL) or
• sulfhemoglobin (>0.5 g/dL), resulting in a grayish bluish coloration of the skin and mucous membranes.
• Because the absolute amount of deoxygenated or abnormal hemoglobin (rather than its percentage) is required for cyanosis to be clinically evident, patients with moderate-to-severe anemia may not appear cyanotic, even with elevated percentages of deoxygenated or abnormal hemoglobins.
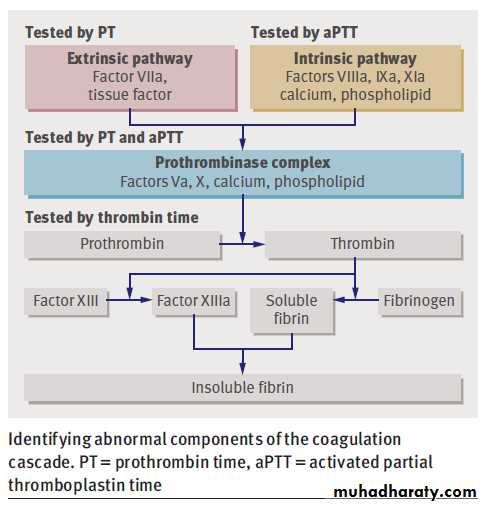
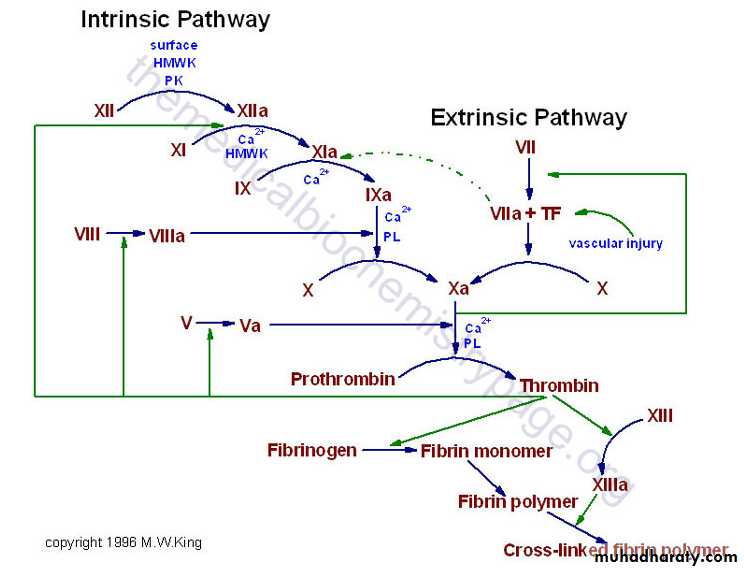
Factor I: fibrinogen
Factor II: prothrombinFactor III: tissue thromboplastin (tissue factor and phospholipid)
Factor IV: ionized calcium
Factor V: occasionally called labile factor or proaccelerin
Factor VI: unassigned
Factor VII: occasionally called stable factor or proconvertin
Factor VIII: antihemophilic factor
Factor IX: plasma thromboplastin component, Christmas factor
Factor X: occasionally called Stuart-Prower factor
Factor XI: occasionally called plasma thromboplastin antecedent
Factor XII: Hageman factor
Factor XIII: fibrin-stabilizing factor
Fibrinolysis pathway
Process of degrading the fibrin clot when it is no longer needed .Also prevents extension of clot beyond site of injury .Initiated by tPA (tissue plasminogen activator) or uPA (urokinase-like plasminogen activator), which convert plasminogen to plasmin in the presence of fibrin by cleaving the Arg561-Val562 peptide bondPlasmin degrades the fibrin clot and intact fibrinogen to soluble fibrin/fibrinogen degradation products (FDP)
Plasmin also inactivates factors Va and VIIIa (as does Protein C and Protein S) tPA is produced by endothelial cells; its activation of plasminogen is major mechanism for lysis of fibrin clots.
Recombinant tPA is used to treat myocardial infarction, stroke and some cases of acute thrombosis.
uPA is produced by urine and plasma; keeps renal tracts free of blood clots; also is important for other cell surfaces and initiating nonfibrinolytic activities of plasmin.
Excessive fibrinolysis is prevented by plasmin inhibitor (antiplasmin, formerly called alpha2-antiplasmin) and plasminogen activator inhibitor 1 (PAI-1, inhibits tPA and uPA). PAI-1 is synthesized by hepatocytes and endothelial cells, is present in platelets and plasma; can bind to fibrin and inhibit plasminogen activators tPA and uPA.
Prothrombin time (PT) screens for abnormalities in the extrinsic and common pathways of coagulation (plasma factors VII, X, V, prothrombin II, and fibrinogenI). The PT is reported as the international normalized ratio (INR), which reflects the ratio of the patient's PT to the laboratory's control value; the INR controls for differences in reagents among different laboratories. Because commercial reagents and instrumentation vary widely, each laboratory determines its own normal range for PT and PTT; a typical normal range for the PT is between 10 and 13 sec.
Prolonged PTT with normal platelets and PT suggests hemophilia A or B. Factor VIII and IX assays are indicated. Inhibitors that prolong the PTT include an autoantibody against factor VIII and antibodies against protein-phospholipid complexes (lupus anticoagulant).
Such inhibitors are suspected when a prolonged PTT does not correct upon 1:1 mixing with normal plasma.
Prolonged PT with normal platelets and PTT suggests factor VII deficiency. Congenital factor VII deficiency is rare; however, the short half-life of factor VII in plasma causes factor VII to decrease to low levels more rapidly than other vitamin K-dependent coagulation factors (eg, in patients given warfarin anticoagulation or in patients with incipient liver disease).
Prolonged PT and PTT with thrombocytopenia suggest DIC.
• Hereditary disorders include erythrocyte membrane and enzymatic defects and hemoglobin abnormalities. Some hereditary disorders include the following:
• G6PD deficiency enzy
• Hereditary spherocytosis memb
• Sickle cell anemia hemo
• Acquired hemolytic conditions can be due to immune disorders, toxic chemicals and drugs, antiviral agents (eg, ribavirin[1 ]) physical damage, and infections. They can include the following:
• Autoimmune hemolytic anemia (AIHA) may result from warm or cold autoantibody types; rarely, mixed types occur. Most warm autoantibodies are (Ig) G and can be detected with the direct Coombs test, which is also known as the direct antiglobulin test (DAT).AIHA may occur after allogeneic hematopoietic stem cell transplantation.
• Microangiopathic anemia is found in patients with (DIC) or (HUS) and (TTP). Fragmented erythrocytes (schistocytes) also occur with defective prosthetic cardiac valves.
Hemolytic anemia
Microangiopathic anemia
is found in with (DIC) or (HUS) and (TTP) patients.Fragmented erythrocytes (schistocytes) also occur with defective prosthetic cardiac valves. Intravascular hemolysis occurs in hemolytic anemia due to
DIC, HUS , TTP, prosthetic valves,
PNH, and G6PD deficiency,
Autoimmune hemolytic anemia warm or cold autoantibody types and hereditary spherocytosis are classified as examples of extravascular hemolysis because the red blood cells are destroyed in the spleen and other reticuloendothelial organs.
A person who is going to have a bone marrow transplant should not receive blood transfusions from close family members before the transplant. When a person receives blood transfusions, their bodies can develop antibodies against the donated blood. If a person develops antibodies against the blood of a close family member, the person would not be able to receive a bone marrow transplant from that family member.
What are the appropriate screening tests for celiac disease?
The tests of choice are antibody measurements in the blood, ideally performed before the patient has removed gluten from the diet. However, patients and physicians must remember that no screening test is perfect, and that the keys to confirming the diagnosis of CELIAC DISEASE remain a small intestinal biopsy combined with the patient’s subsequent clinical response to a gluten-free diet. Thus, a patient (especially a young child) with symptoms of CELIAC DISEASE should have a small bowel biopsy, even if the antibodies are not highly suggestive.The blood tests can be divided into 2 different types of antibodies: those which are “anti-gluten”, and those that “anti-self”. The “anti-gluten” antibodies are the anti-gliadin IgG and IgA.
The “anti-self” antibodies are anti-endomysial IgA and anti-tissue transglutaminase IgA. Each antibody test varies widely in its sensitivity and specificity for predicting whether the disease is present in any individual.
There are also several conditions which may yield false negative antibody results. One of the conditions that may give a false negative result is Immunoglobulin A or IgA deficiency. If a patient has a low total IgA level, the antibodies may be falsely low. This is why I always recommend that a patient have a total IgA level drawn at the same time the antibody testing is done. Young children may not make the some of the “anti-self” antibodies, as it takes a somewhat mature immune system to make them. So in a young child, antiendomysial antibody, or the TTG antibody, can have false negative results. A gluten-free diet will make the antibody tests negative.