• Panorama 3
• In Medicineد. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
Grade
Level of ConsciousnessPersonality and Intellect
Neurologic Signs
Electroencephalogram (EEG) Abnormalities
0
Normal
Normal
None
None
Subclinical
Normal
Normal
Abnormalities only on psychometric testing
None
1
Day/night sleep reversal, restlessness
Forgetfulness, mild confusion, agitation, irritability
Tremor, apraxia, incoordination, impaired handwriting
Triphasic waves
(5 Hz)
2
Lethargy, slowed responses
Disorientation to time, loss of inhibition, inappropriate behavior
Asterixis, dysarthria, ataxia, hypoactive reflexes
Triphasic waves
(5 Hz)
3
Somnolence, confusion
Disorientation to place, aggressive behavior
Asterixis, muscular rigidity, Babinski signs, hyperactive reflexes
Triphasic waves
(5 Hz)
4
Coma
None
Decerebration
Delta/slow wave activity
Grading of Hepatic Encephalopathy
Characteristics associated with a good response to interferon among patients with chronic hepatitis B virus infection
• Alanine aminotransferase more than twice the upper limit of normal
• Hepatitis B virus DNA <106 IU/ml
• Age <50 years
• Hepatitis B virus genotype A or B
• Female
• Non-vertical transmission
PregnancyThe universal prevention of transmission of hepatitis B virus from mother to child during the perinatal period remains an achievable goal. Testing of mothers for hepatitis B surface antigen allows those with a positive result to get hepatitis B immune globulin and early vaccination for their children, a strategy that has been proved to reduce transmission by 95-99%.
The advent of low toxicity antiviral treatment might help in this regard too, with emerging evidence that addition of antivirals in the third trimester, particularly for those with high viral loads, might further reduce infant infection.
Risk of reactivation of hepatitis with immunosuppressionIndividuals positive for hepatitis B surface antigen are at risk of a flare-up in disease if given immunosuppressants or cytotoxic chemotherapy. In addition to routine screening for hepatitis B surface antigen, it is now recommended that exposure to hepatitis B virus should also be assessed using anti-HBcore antibody as even patients who are negative for the surface antigen are at risk of reactivation and should be given prophylactic treatment. Guidelines recommend that patients positive for hepatitis B surface antigen should receive antiviral therapy for the duration of the immunosuppressive period and for 12 months thereafter.
Guidelines recommend that patients positive for hepatitis B surface antigen should receive antiviral therapy for the duration of the immunosuppressive period and for 12 months thereafter.
Myth of γ glutamyltransferase
Cobbold and colleagues state that γ-glutamyltransferase should be measured in all patients with raised serum alanine aminotransferase because if raised it would indicate alcohol related liver disease.Because of its ubiquitous distribution within the liver, γ glutamyltransferase is raised in all types of liver disease. In the absence of serious liver disease, the myth that a raised γ glutamyltransferase is sensitive and specific for alcohol excess persists. In these circumstances, for example, γ glutamyltransferase is raised in only 52% of alcoholic patients, but it is also raised in 50% of patients with non-alcoholic fatty liver disease.
Guidelines recommend that it is measured only to identify the likely origin of an isolated raised alkaline phosphatase, because if raised it indicates a hepatic rather than bony origin.
We therefore suggest that measuring γ glutamyltransferase when investigating raised serum transaminases is unnecessary and potentially misleading.
• Raised serum alanine aminotransferase values usually indicate hepatocellular damage. Aminotransferase values of less than five times the upper limit of normal are often considered mild, while those more than five times the upper limit of normal are severe, representing more extensive hepatocellular injury.
BMJ 30 July 2010
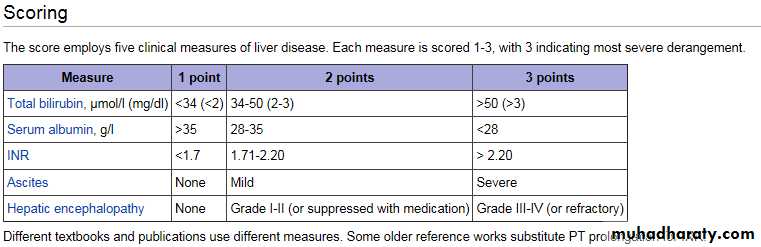
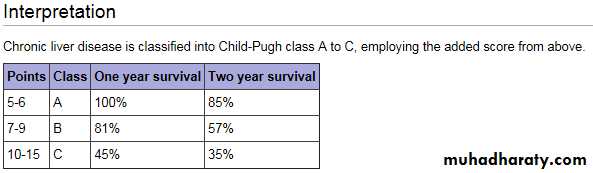
Mildly raised values do not exclude severe chronic liver disease; indeed evidence exists that substantial liver damage may be present even with relatively mild biochemical derangements.1 Therefore we recommend that even mild derangements of aminotransferase values that persist on retesting over a three month period should be investigated further.If clinical features suggest a more pressing need for investigation (such as jaundice or raised bilirubin, deranged clotting, or hepatic decompensation) investigation should be expedited.The Child-Pugh score (sometimes the Child-Turcotte-Pugh score) is used to assess the prognosis of chronic liver disease, mainly cirrhosis. Although it was originally used to predict mortality during surgery, it is now used to determine the prognosis, as well as the required strength of treatment and the necessity of liver transplantation.
Allopurinol inhibits xanthine oxidase prevents the conversion of hypoxanthine and xanthine into uric acid but
does not remove existing uric acid. Although allopurinol prevents the formation of uric acid, existing uric acid must still be excreted.
In contrast, rasburicase
removes uric acid by enzymatically degrading it into allantoin, a highly soluble product that has no known adverse effects on health.Tumor lysis syndrome
The level of uric acid may take 2 days or more to decrease, a delay that allows urate nephropathy to develop .Moreover, despite treatment with allopurinol, xanthine may accumulate,resulting in xanthine nephropathy.
Since the serum xanthine level is not routinely
measured, its effect on the development of acute
kidney injury is uncertain. By preventing xanthine
accumulation and by directly breaking down uric
acid, rasburicase is more effective than allopurinol
for the prevention and treatment of the tumor
lysis syndrome.
Urinary alkalinization increases uric acid solubility but decreases calcium phosphate solubility.
Because it is more difficult to correct hyperphosphatemia than hyperuricemia, urinary alkalinization should be avoided in patients with
the tumor lysis syndrome, especially when rasburicase is available.
The primary management of most cases of BPH is medical therapy. Alpha-blockers can reduce symptoms within days, whereas 5-alpha-reductase inhibitors can take 6 to 12 months to relieve urinary symptoms.
Of these 2 classes of medications, only 5-alpha-reductase inhibitors reduce the risk for urinary retention and the need for prostate surgery. A recent trial suggested a synergistic effect when alpha-blockers were used with 5-alpha-reductase inhibitors in the treatment of BPH.
The tyrosine kinase inhibitor (TKI) imatinib, which targets the enzyme that results from the BCR-ABL mutation and is associated with an overall survival rate of about 89% at 5 years, revolutionized the treatment of chronic myeloid leukemia (CML) during the past decade.[1,2] Since then, newer-generation TKIs, including nilotinib and dasatinib, have been developed for the treatment of CML.[3,4
Community and Expert Perspectives: 2010 Update on Chronic Myeloid Leukemia
MedscapeCME Oncology © 2010
LIVER ENZYME INDUCERS
PhenytoinCarbamazepine
Barbiturates
Rifampicin
Alcohol
Sulphonylureas
LIVER ENZYME INHIBITORS
Omeprazole
Amiodarone
Allopurinol
Ketoconazole
Disulfram
Erythromycin
Valproate
Isoniazid
Ciprofloxacin
Cimetidine
Ethanol
Sulphonamides Inhibitors of cytochrome CYP3A, including:
Diltiazem
Verapamil
Ketoconazole and other azole antifungals
Macrolide antibiotics
Ritonavir (Norvir)
Grapefruit products or grapefruit juice
• Drugs which can cause gynaecomastia :
• digoxin ,oestrogens, spironolactone
• cimetidine ,verapamil ,nifedipine , ketoconazole
• metronidazole.
• Drugs causing galactorrhoea are:
• Oral contraceptive pills
• Phenothiazines
• Metoclopramide
• Bromocriptine
• Drugs producing hypercalcemia
• lithium, alkaline antacids• DES,
• Thiazides
• estrogens
• progesterone
The major effect of grapefruit juice appears to reduce “first-pass” metabolism by reducing CYP3A4 activity. Because grapefruit juice does not generally affect the systemic clearance of affected drugs, it appears that grapefruit juice selectively reduces intestinal CYP3A4 activity ((prevents their absorption )) while having little effect on liver CYP3A4.
Thus Grapefruit juice has no effect on drug disposition after intravenous administration and does not alter liver CYP3A4 activity.
drugs that can induce parkinsonism :
• Old antipsychotics (for example haloperidol)• New antipsychotics (for example olanzapine)
• Anti-nausea agents (for example prochlorperazine)
• Antihistamines (for example cinnarizine).
OBSTRUCTIVE
Asthma
Chronic obstructive lung disease
(chronic bronchitis, emphysema)
Bronchiectasis
Cystic fibrosis
Bronchiolitis
RESTRICTIVE—PARENCHYMA
Sarcoidosis
Idiopathic pulmonary fibrosis
Pneumoconiosis
Drug- or radiation-induced
interstitial lung disease
RESTRICTIVE—EXTRAPARENCHYMAL
Neuromuscular
Diaphragmatic weakness/paralysis
Myasthenia gravis
Guillain-Barre´ syndrome
Muscular dystrophies
Cervical spine injury
Chest wall
Kyphoscoliosis
Obesity
Ankylosing spondylitis
Common Respiratory Diseases by Diagnostic Categories
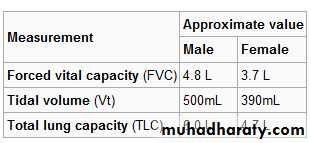
• Two major patterns of abnormal ventilatory function are restrictive and obstructive
• In obstructive pattern:
• Hallmark is decrease in expiratory flow rate, i.e., FEV1.
• Ratio FEV1/FVC is reduced.
• TLC is normal or increased.
• RV is elevated due to trapping of air during expiration.
• In restrictive disease:
• Hallmark is decrease in TLC.
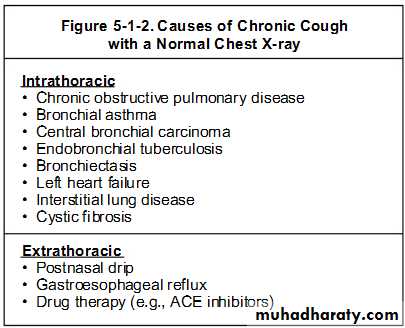
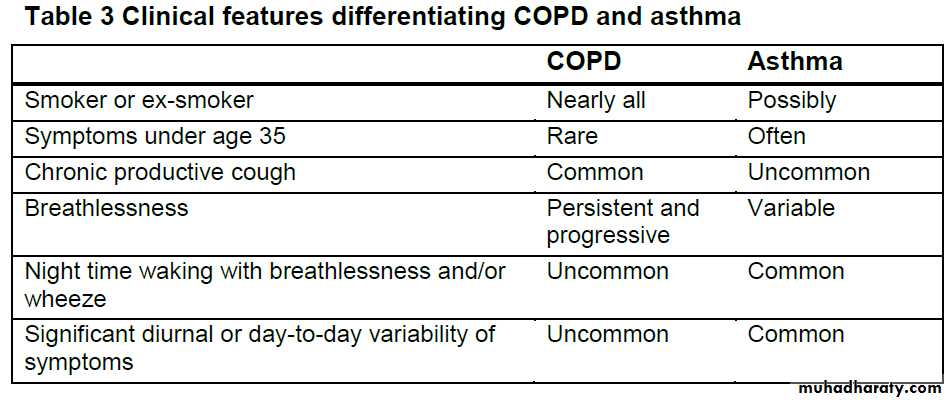
The diagnosis (COPD)is confirmed by spirometry.
The presence of a postbronchodilator• FEV1< 80% of the predicted value in combination
• with an FEV1/FVC < 70% confirms the presence of airflow limitation that is not fully reversible.
Whooping cough, which is caused by the Gram negative bacterium Bordetella pertussis. ELISA using serum is the most commonly available laboratory test used to confirm the diagnosis. Pertussis can be diagnosed in the acute phase by testing nasal secretions using PCR, although most cases present after many weeks (that is, in the chronic phase), by which time the bacteria have been cleared. B pertussis can be hard to grow in vitro, and a positive culture from nasal secretions is often not achieved,neither infection nor immunisation results in lifelong immunity .
B pertussis infection can be associated with a highly elevated lymphocyte count, so a blood count can assist in making the diagnosis, particularly in infants.
Once the diagnosis of pertussis is confirmed in a child, management is supportive. Antibiotics do not alter the course of the infection once paroxysms are established. Eradication with a macrolide antibiotic is indicated to reduce transmission, but this is only thought to be effective where symptoms have been present for less than three weeks.
Acute complications are mostly limited to infants, in whom the infection can be life threatening, and include weight loss, apnoeas, pneumonia, and circulatory failure.The most common chronic complication is bronchiectasis.
Traditionally, a 10 day course of erythromycin was prescribed to eradicate infection; however, a seven day course of clarithromycin or a three to five day course of azithromycin are not inferior in terms of eradication and are associated with a third fewer cases of side effects.
Because inflammation is the main pathologic mechanism, anti- inflammatory agents (specifically inhaled corticosteroids) are first-line therapy in asthma. To prevent and counteract reversible episodes of bronchospasm, beta-2 adrenergic inhalers directly dilate the bronchioles.
In contrast, bronchoconstriction in COPD is progressive, largely cholinergic mediated, and only partially reversible,bronchoconstriction is a major pathologic mechanism in COPD, bronchodilators (specifically anticholinergic inhalers) are first-line therapy.
Efficiency of mouth to patient insufflation
Normal atmospheric air contains approximately 21% oxygen when created in. After gaseous exchange has taken place in the lungs, with waste products (notably carbon dioxide) moved from the bloodstream to the lungs, the air being exhaled by humans normally contains around 17% oxygen.This means that the human body utilises only around 19% of the oxygen inhaled, leaving over 80% of the oxygen in the exhalatory breath.
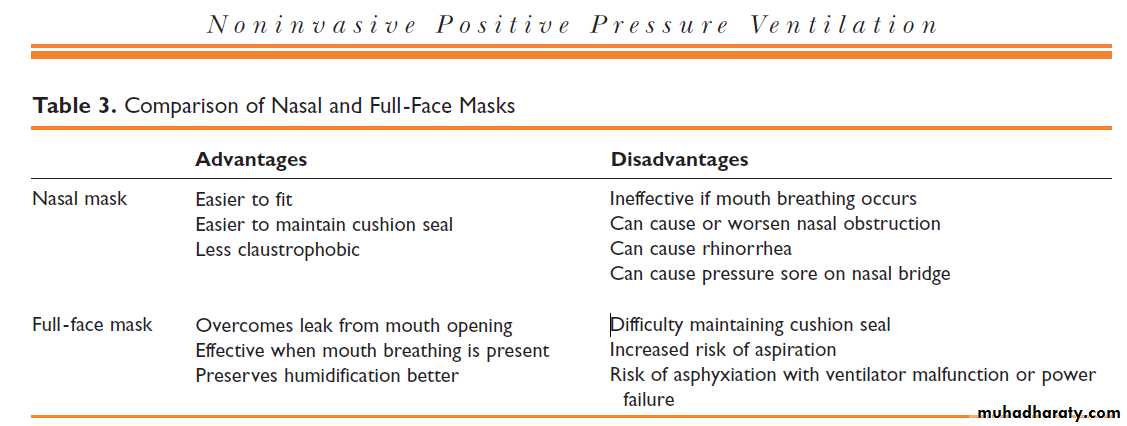
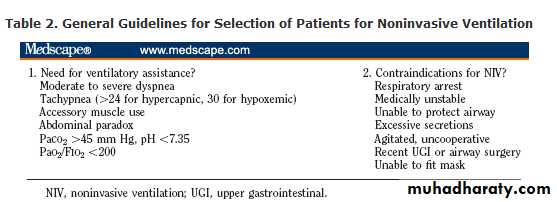
Positive pressure ventilation
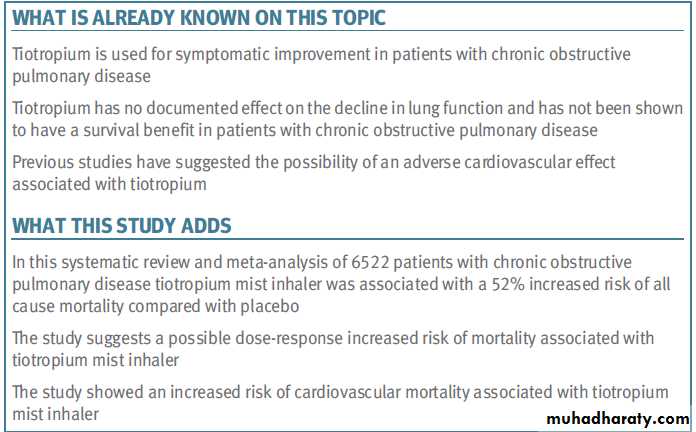
any of numerous types of mechanical ventilation in which gas is delivered into the airways and lungs under positive pressure, producing positive airway pressure during inspiration. It may be done via either an endotracheal tube or a nasal maskInhaled Long-Acting Muscarinic Antagonists (LAMAs) for COPD
Inhaled muscarinic antagonists work by inhibiting muscarinic receptors on the bronchial airways, which lead to muscle relaxation, bronchodilation and improved lung function. Until recently, only one inhaled muscarinic antagonist (ipratropium) has been available in the United States, both as a single agent and in combination with the short-acting beta2 agonist albuterol. This product is short acting and requires dosing four or more times per day.An inhaled LAMA (tiotropium, Spiriva®) suitable for once-a-day dosing has been available in Europe since 2002 and was launched in the United States in May 2004. Tiotropium produces a prolonged blockade of muscarinic M3 receptors. Although blocking the M3 receptor is important for bronchodilation, there is emerging evidence that other receptor sub-types may play a role in mediating bronchodilation.
Current literature suggests that
smoking cessation,long-term oxygen therapy in hypoxaemic patients,
non-invasive ventilation,and
lung volume reduction surgery in selected patients improve survival.
COPD
Theophylline is a nonspecific phosphodiesterase inhibitor and has bronchodilator effects at higher doses, where there is a higher risk of toxicity.
Specific phosphodiesterase E4 inhibitors such as cilomilast and roflumilast are currently undergoing clinical trials.
They may have anti-inflammatory and bronchodilator properties but preliminary results show a modest bronchodilator effect and some benefits on quality of life.
The combination of LABAs and ICS was superior in all endpoints studied compared with ICS alone. It is therefore suggested that in patients with COPD, ICS should not be used alone but rather in combination with a LABA.
In stable COPD there is no role for chronic
use of systemic corticosteroids. Long-term use of systemic corticosteroids is definitely associated with toxic effects such as hyperglycaemia, myopathy, hypertension and osteoporosis,all of which are more pronounced in the elderly.
Forced Vital Capacity (FVC)
FVC is the volume of air that can forcibly be blown out as hard as possible, for as long as possible, preferrably at least 6 seconds. after full inspiration, measured in liters.Forced Expiratory Volume in 1 second (FEV1)
Average values for FEV1 in healthy people depend mainly on sex and age. Values of between 80% and 120% of the average value is considered normal.
The dose of theophylline prescribed should be reduced at the time of an exacerbation
if macrolide or fluroquinolone antibiotics orother drugs known to interact) are prescribed.
Oxygen
Long-term oxygen therapy (LTOT) Clinicians should be aware that inappropriate oxygen therapy in people with COPD may cause respiratory depression. LTOT is indicated in patients with COPD who have a PaO2 <7.3 kPa when stable or a PaO2 >7.3 and less than 8 kPa when stable and one of: secondary polycythaemia, nocturnal hypoxaemia (oxygen saturation of arterial blood [SaO2] <90% for more than 30% of the time), peripheral oedema or pulmonary hypertension
Treatment of cor pulmonale
Patients presenting with cor pulmonale should be assessed for the need for long-term oxygen therapy. Oedema associated with cor pulmonale can usually be controlled symptomatically with diuretic therapy.The following are not recommended for the treatment of cor pulmonale:
• angiotensin-converting enzyme inhibitors
• calcium channel blockers
• alpha-blockers
• digoxin (unless there is atrial fibrillation).
Vaccination and anti-viral therapy
Pneumococcal vaccination and an annual influenza vaccinationshould be offered to all patients with COPD
Lung surgery
Patients who are breathless, and have a single large bulla on a CT scan and an FEV1 less than 50% predicted should be referred for
consideration of bullectomy.
Respiratory stimulants
It is recommended that doxapram is used only when non-invasive ventilation is either unavailable or considered inappropriate.Both Spiriva (Tiotropium) and Ipratropium (Atrovent) are anticholinergic agents that are used for maintenance treatment of bronchospasm associated with COPD. Spiriva has an additional indication for reducing COPD exacerbations based on the outcomes of the large UPLIFT clinical trial. Both medications are not indicated for acute treatment of a bronchospasm and should never be used as rescue medications. The major difference between the two drugs is that Spiriva is a long acting medication and Ipratropium is a short acting drug. Spiriva is used once daily, while Ipratropium may be used every 4 to 6 hours.
Ipratropium bromide and tiotropium bromide are structural analogues of atropine which have minimal systemic absorption following inhalation because of their quaternary ammonium structure. These anticholinergic drugs are useful bronchodilators in chronic obstructive pulmonary disease. They are rarely indicated in asthma. Bronchodilators provide symptomatic relief and improve health-related quality of life in patients with chronic obstructive pulmonary disease, but they do not influence the decline in lung function. The only measure currently known to halt this decline is stopping cigarette smoking.
The main clinical indication for ipratropium bromide is the symptomatic relief of breathlessness in patients with COPD. It is rarely required for the treatment of patients with asthma because proper treatment of asthmatic patients with inhaled corticosteroids and long-acting beta agonists provides good control for the majority of patients. The extent of bronchodilatation with ipratropium in patients with COPD is similar to that achieved with inhaled beta agonists. The choice between ipratropium and beta agonists for a patient with COPD is determined by the patient's tolerance of the drug, rather than its efficacy. There are no long-term studies of tiotropium in asthma so it is not indicated for patients with asthma.
Chronic obstructive pulmonary disease is ranked the fourth leading cause of death worldwide
BMJ 2011;342
A diagnosis of cor pulmonale should be considered if patients have:
• peripheral oedema
• a raised venous pressure
• a systolic parasternal heave
• a loud pulmonary second heart sound.
The following individuals should not receive the varicella vaccine:
Individuals with anaphylactic allergy to gelatin or neomycinIndividuals with untreated active tuberculosis
Individuals with weakened immunity such as HIV infection, or taking medications such as corticosteroids that weaken immunity, or have diseases that weaken immunity
Pregnant women
Individuals who have received immune globulin or blood product in prior 5 months .
The varicella vaccine is highly effective in preventing chickenpox.
It is not certain whether the varicella vaccine prevents shingles.
Infants born to HBsAg-positive mothers should receive hepatitis immune globulin (HBIG) in addition to hepatitis B vaccine at birth. Hepatitis B vaccinations are safe for pregnant and nursing mothers. The hepatitis B vaccines are 95% effective. Five percent of vaccinated individuals will fail to develop the necessary antibodies for immunity after the three doses.
Patients with weakened immunity (such as HIV infection), elderly patients, and patients undergoing kidney hemodialysis are more likely to fail to respond to the vaccinations.
• MMR is made from live viruses that have been modified from the viruses that cause disease. Even though there is no evidence of vaccine-induced birth defects, pregnant women should not receive MMR vaccine.
• Women should also avoid pregnancy for 28 days after receiving MMR or any rubella-containing vaccine
• The following individuals should not receive MMR:
• Patients with allergy to eggs or neomycin
• Pregnant women
• Patients with weakened immunity
• Patients with untreated active tuberculosis
Q. Current guidelines suggest that thrombolytic therapy be withheld from which patients with acute ischemic stroke?
A. If a focal area of low density (or “hypodensity”) is seen on computed tomography of the brain that involves more than 1/3 of the middle cerebral artery territory, most treatment protocols recommend withholding thrombolytic therapy, because this finding (which suggests irreversible injury) is predictive of subsequent hemorrhagic transformation of the infarct in some studies. Platelet count should be ≥100,000, prothrombin time <15 seconds (or INR <1.7) and glucose >50 mg/dl before rt-PA is administered within 3 hours of onset of stroke,. Current guidelines recommend treatment of hypertension to achieve a systolic pressure ≤185 mm Hgsystolic and diastolic values ≤110 mm Hg prior to administering intravenous rt-PA.
What endocrine tumors cause flushing?
Neuroendocrine tumors, including pheochromocytoma, vasoactive intestinal peptide–producing tumors, medullary thyroid carcinoma, and carcinoid tumors, may all secrete substances that cause flushing, hypotension or hypertension, diarrhea, and respiratory symptoms in various combinations.Q. What is the mechanism of glucocorticoid-induced bone disease?
A. Glucocorticoid excess directly reduces osteoclast production, but the lifespan of osteoclasts is prolonged, in contrast to the increase in osteoblast apoptosis. Therefore, with long-term therapy, the number of osteoclasts is usually maintained in the normal range, whereas the number of osteoblasts plummets and bone formation is substantially reduced.The use of the D-dimer assay is of limited value in patients with a high clinical probability of pulmonary embolism.
The specificity of an increased D-dimer level is reduced in patients with cancer, pregnant women, and hospitalized and elderly patients. Most hospitalized patients should not undergo D-dimer testing when pulmonary embolism is suspected.
• When do nausea and vomiting in pregnancy most typically resolve?
• The onset of the nausea is within four weeks of the last menstrual period in most patients. The problem typically peaks at approximately 9 weeks of gestation.
Sixty percent of cases resolve by the end of the first trimester, and 91% by 20 weeks gestation.
Oral vitamin B6 and doxylamine first-line therapy , a 70% reduction in nausea and vomiting
• What are some protective factors against nausea and vomiting in pregnancy?
• Nausea and vomiting are less common in older women, multiparous women, and smokers, an observation that has been attributed to their smaller placental volumes .• How does branch retinal-vein occlusion present?
• Patients with retinal-vein occlusion typically present with sudden, unilateral, painless loss of vision. The degree of vision loss depends on the extent of retinal involvement and on macular-perfusion status. Some patients with branch retinal-vein occlusion report only a peripheral visual-field defect.• Is measurement of natriuretic peptides useful when heart failure is suspected?
• Measurement of the plasma concentration of natriuretic peptides is recommended, since natriuretic peptides are secreted into the circulation increased amounts by the failing heart, and a normal concentration virtually rules out a diagnosis of heart failure (although this observation may not hold true in the case of obese persons).• Which patients with heart failure benefit from an implantable cardioverter–defibrillator?
• An implantable cardioverter–defibrillator is indicated for secondary prevention, in the case of any patient who survives an unprovoked episode of ventricular fibrillation or sustained ventricular tachycardia and for primary prevention, in the case of patients in NYHA functional class II or III who have an ejection fraction that is persistently 35% or less despite optimal medical therapy and who are expected to survive for at least 1 year with a reasonable quality of life and functional status.
Direct sunlight kills tubercle bacilli in 5 minutes . Infectious particles of respiratory secretions usually less than 5 µm in diameter and containing tubercle bacilli). Asingle cough can produce 3000 droplet nuclei.
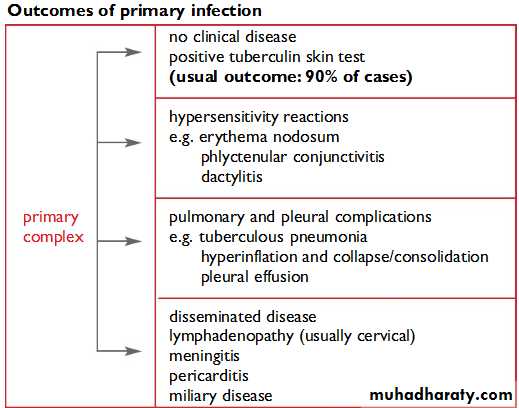
The vast majority (90%) of people without HIV infection who are infected with M. Tuberculosis do not develop TB. Natural history of untreated TB
Without treatment, by the end of 5 years
50% of PTB patients will be dead,
25% will be healthy (self-cured by a strong immune defence) and
25% will remain ill with chronic infectious TB
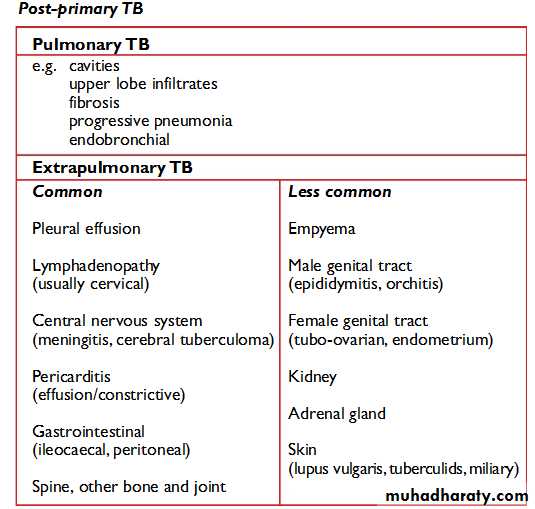
Post-primary TB
occurs after a latent period of months or years following primary infection. It may occur either by reactivation of the dormant tubercle bacilli acquired from a primary infection or by reinfection.The immune response of the patient results in a pathological lesion that is characteristically localized,often with extensive tissue destruction and cavitation.
The characteristic features of post-primary PTB are the following:
• extensive lung destruction with cavitation;• positive sputum smear;
• upper lobe involvement;
• usually no intrathoracic lymphadenopathy. Patients with these lesions are the main transmitters of infection in the commmunity.
Post-primary infection with pulmonary disease usually occurs in adults and leads to microscopy-positive sputum smears.
Conditions that may suppress the tuberculin skin test
• HIV infection• Malnutrition
• severe bacterial infections, including TB itself
• viral infections, e.g. measles, chickenpox, glandular fever
• Cancer
• immunosuppressive drugs, e.g. steroids
• incorrect injection of PPD
The different drugs in the regimen have different modes of action. INH are bacteriocidal against replicating bacteria. EMB is bacteriostatic at low doses, but is used in TB treatment at higher, bactericidal doses. RMP is bacteriocidal and has a sterilizing effect. PZA is only weakly bactericidal, but is very effective against bacteria located in acidic environments, inside macrophages, or in areas of acute inflammation.
The WHO also recommend
a six-month continuation phase of HR• if the patient is still culture positive after 2 months of treatment (approximately 15% of patients with fully sensitive TB) and
• for those patients who have extensive bilateral cavitation at the start of treatment.
The WHO extended the DOTS programme in 1998 to include the treatment of MDR-TB (called "DOTS-Plus"). Implementation of DOTS-Plus requires the capacity to perform drug-susceptibility testing (not routinely available even in developed countries) and the availability of second-line agents, in addition to all the requirements for DOTS. DOTS-Plus is therefore much more resource-expensive than DOTS, and requires much greater commitment from countries wishing to implement it. Resource limitations mean that the implementation of DOTS-Plus may lead inadvertently to the diversion of resources from existing DOTS programmes and a consequent decrease in the overall standard of care.
Up to 25% of patients with TB of the lymph nodes (TB lymphadenitis) will get worse on treatment before they get better and this usually happens in the first few months of treatment. A few weeks after starting treatment, lymph nodes often start to enlarge, and previously solid lymph nodes may become fluctuant. This should not be interpreted as failure of therapy and is a common reason for patients (and their physicians) to panic unnecessarily. With patience, two to three months into treatment the lymph nodes start to shrink again and re-aspiration or re-biopsy of the lymph nodes is unnecessary. In these situations, all that is required is re-assurance. Steroids may be useful in resolving the swelling, especially if it is painful, but they are unnecessary. Additional antibiotics are unnecessary and the treatment regimen does not need to be lengthened.
Tuberculosis of the central nervous system
Tuberculosis may affect the central nervous system (meninges, brain or spinal cord) in which case it is called TB meningitis, TB cerebritis, and TB myelitis respectively; the standard treatment is 12 months of drugs (2HREZ/10HR) and steroid are mandatory.Diagnosis is difficult as CSF culture is positive in less than half of cases, and therefore a large proportion of cases are treated on the basis of clinical suspicion alone. PCR of CSF does not significantly improve the microbiology yield; culture remains the most sensitive method and a minimum of 5 ml (preferably 20 ml) of CSF should be sent for analysis.
The CSF of patients with treated TB meningitis is commonly abnormal even at 12 months,the rate of resolution of the abnormality bears no correlation with clinical progress or outcome,and is not an indication for extending or repeating treatment; repeated sampling of CSF by lumbar puncture to monitor treatment progress should therefore not be done. INH (CSF penetration 100%),RMP (10–20%),EMB (25–50% inflamed meninges only),PZA (100%)
STM (20% inflamed meninges only). The use of steroids is routine in TB meningitis. The absorption of RMP is reduced if taken with fat, but is unaffected by carbohydrate, protein,[24] or antacids.[25]
What are the indications for treatment with steroids?
• TB meningitis (decreased consciousness, neurological defects, or spinal block).*• TB pericarditis (with effusion or constriction).*
• TB pleural effusion (when large with severe symptoms).*
• Hypoadrenalism (TB of adrenal glands).*
• TB laryngitis (with life-threatening airway obstruction).*
• Severe hypersensitivity reactions to anti-TB drugs.*
• Renal tract TB (to prevent ureteric scarring).*
• Massive lymph node enlargement with pressure effects.
Steroids
The usefulness of corticosteroids (e.g., prednisolone or dexamethasone) in the treatment of TB is proven for TB meningitis and TB pericarditis. The dose for TB meningitis is dexamethasone 8 to 12 mg daily tapered off over six weeks .The dose for pericarditis is prednisolone 60 mg daily tapered off over four to eight weeks.
Steroids may be of temporary benefit in pleurisy, extremely advanced TB, and TB in children:
Pleurisy: prednisolone 20 to 40 mg daily tapered off over 4 to 8 weeks
Extremely advanced TB: 40 to 60 mg daily tapered off over 4 to 8 weeks
TB in children: 2 to 5 mg/kg/day for one week, 1 mg/kg/day the next week, then tapered off over 5 weeks
Steroids may be of benefit in peritonitis, miliary disease, tubercular osteomyelitis, TB osteomyelitis, laryngeal TB, lymphadenitis and genitourinary disease, but the evidence is scant and the routine use of steroids cannot be recommended. Steroid treatment in these patients should be considered on a case by case basis by the attending physician.
Thalidomide may be of benefit in TB meningitis and has been used in cases where patients have failed to respond to steroid treatment.
It is possible to test urine for isoniazid and rifampicin levels in order to check for compliance. The interpretation of urine analysis is based on the fact that isoniazid has a longer half-life than rifampicin:
urine positive for isoniazid and rifampicin patient probably fully compliant
urine positive for isoniazid only patient has taken his medication in the last few days preceding the clinic appointment, but had not yet taken a dose that day.
urine positive for rifampicin only patient has omitted to take his medication the preceding few days, but did take it just before coming to clinic.
urine negative for both isoniazid and rifampicin patient has not taken either medicine for a number of days
The relative incidence of major adverse effects has been carefully described:
INH 0.49 per hundred patient monthsRMP 0.43
EMB 0.07
PZA 1.48
All drugs 2.47
The offending drugs are given in decreasing order of frequency:
Thrombocytopenia: RMP
Neuropathy: INH
Vertigo: STM
Hepatitis: PZA, RMP, INH
Rash: PZA, RMP, EMB
Thrombocytopenia is only caused by RMP and no test dosing need be done.
The most frequent cause of neuropathy is INH. The peripheral neuropathy of INH is always a pure sensory neuropathy. Once a peripheral neuropathy has occurred, INH must be stopped and pyridoxine should be given at a dose of 50 mg thrice daily. Simply adding high dose pyridoxine to the regimen once neuropathy has occurred will not stop the neuropathy from progressing. Patients at risk of peripheral neuropathy from other causes (diabetes mellitus, alcoholism, renal failure, malnutrition, pregnancy, etc.) should be given pyridoxine 10 mg daily at the start of treatment. The drug most frequently implicated as causing a drug fever is RMP
Drug-induced hepatitis
The single biggest problem with TB treatment is drug-induced hepatitis, which has a mortality rate of around 5%. Three drugs can induce hepatitis: PZA, INH and RMP (in decreasing order of frequency). It is not possible to distinguish between these three causes based purely on signs and symptoms. Test dosing must be carried out to determine which drug is responsible.Liver function tests (LFTs) should be checked at the start of treatment, but, if normal, need not be checked again; the patient need only be warned of the symptoms of hepatitis. Some clinicians insist on regular monitoring of LFT's while on treatment, and in this instance, tests need only be done two weeks after starting treatment and then every two months thereafter, unless any problems are detected.
If clinically significant hepatitis occurs while on TB treatment, then all the drugs should be stopped until the liver transaminases return to normal.
If the patient is so ill that TB treatment cannot be stopped, then STM and EMB should be given until the liver transaminases return to normal (these two drugs are not associated with hepatitis).
Fulminant hepatitis can occur in the course of TB treatment, but is fortunately rare; emergency liver transplantation may be necessary and deaths do occur.
TB involving the brain or spinal cord (meningitis, encephalitis, etc.) is currently treated with 2HREZ/10HR (12 months of treatment in total), but there is no evidence to say that this is superior to 2HREZ/4HR, it is merely that no-one has been brave enough to do the clinic trial that answers the question if the short course is equivalent.
INH may be associated with an increased risk of seizures. Pyridoxine 10 mg daily should be given to all epileptics taking INH. There is no evidence that INH causes seizures in patients who are not epileptic.
Drug-resistant tuberculosis (MDR- and XDR-TB)
DefinitionsMulti-drug resistant tuberculosis (MDR-TB) is defined as TB that is resistant at least to INH and RMP. It has a mortality rate of up to 80%. Isolates that are multiply resistant to any other combination of anti-TB drugs but not to INH and RMP are not classed as MDR."Extensively drug-resistant tuberculosis" (XDR-TB) is defined as MDR-TB that is resistant to quinolones and also to any one of kanamycin, capreomycin, or amikacin.The old case definition of XDR-TB is MDR-TB that is also resistant to three or more of the six classes of second-line drugs.This definition should no longer be used, but is included here because many older publications refer to it.
Trial of TB treatment
In areas where TB is highly endemic, it is not unusual to encounter patient with a fever, but in whom no source of infection is found. The physician may then, after extensive investigation has excluded all other diseases, resort to a trial of TB treatment.The regimen used is HEZ for a minimum of three weeks; RMP and STM are omitted from the regimen because they are broad spectrum antibiotics, whereas the other three first-line drugs treat only mycobacterial infection. Resolution of the fever after three weeks of treatment is good evidence for occult TB and the patient should then be changed to conventional TB treatment (2HREZ/4HR). If the fever does not resolve after three weeks of treatment then it is reasonable to conclude that the patient has another cause for his fever.If the patient has severe liver damage, an alternative regimen is streptomycin plus isoniazid plus ethambutol in the initial phase followed by isoniazid and ethambutol in the continuation phase with atotal duration of 12 months.* Recommended regimens are 2SRHE/6HE or 2SHE/10HE.
Calcium phosphate, calcium carbonate, and magnesium ammonium phosphate (struvite) develop in alkaline urine. Struvite/calcium carbonate apatite stones also are referred to as "infection stones" because of
their strong association with infection caused by organisms that produce urease ,promotes the generation of ammonia and hydroxide from urea
• Uric acid, cystine, and calcium oxalate stones
• Precipitate in acidic urine.
• streptomycin, neomycin, and kanamycin are effective if
• The urine is alkaline. alkaline urine helps prevent
• formation of sulfonamide crystals.
• High-Potassium Foods a high potassium intake can cut the risk of kidney stones in half. Potassium helps the kidneys retain calcium, rather than sending it out into the urine. Potassium supplements are not generally necessary. Rather, a diet including regular servings of fruits, vegetables, and beans supplies plenty of potassium.
• Sugar accelerates calcium losses through the kidney. Sodium increases the passage of calcium .
• Calcium plenty in diet (forms an insoluble salt with dietary oxalate, lowering oxalate absorption and excretion). Avoid supplements away from meals , The supplement should not contain added vitamin D ,increases calcium absorption, leaving less calcium in the intestinal tract to bind to oxalate.
• sodas contain phosphorus, which leads to kidney stones.
• High fluid intake so that the urine specific gravity remains at ≤ 1.005 throughout the day and night.
• Normal urine is sterile.
• E. coli causes roughly 90% of urinary infections, and this bacterium does NOT contain the enzyme urease.• glycosaminoglycans
• pyrophosphate and
• citrate
• Most often, the urine pH is not altered at all by the infection.the normal urine pH is very variable, but usually in the range of 6.0 -- almost always less than 7.
• Only bacteria that contain the enzyme "urease" will cause an obvious elevation in urine pH. This enzyme will split urea into ammonia plus CO2. The ammonia then combines with water, forming ammonium ions plus hydroxyl ions, thus raising the pH. So infections with "urease positive" bacteria can raise the pH of the urine to something higher than 7 -- as high as 8.0.
• Having said this, you need to know that E. coli causes roughly 90% of urinary infections, and this bacterium does NOT contain the enzyme urease. Therefore in over 90% of urinary infections, you will NOT see elevation of urine pH.
• The urine pH in almost all infections is normal, therefor.Classically, if you DO see a high urine pH, you are supposed to look for proteus infection, which can result in the formation of struvite stones.
The association between animal proteins and stones probably relates both to the amount of protein they contain and to their content of the sulfur-containing amino acids. In particular, the sulfur in cystine and methionine is converted to sulfate, which tends to acidify the blood.
As a part of the process of neutralizing this acid, bone is dissolved, and bone calcium ends up in the urine.
Meats and eggs contain two to five times more of these sulfur-containing amino acids than are found in grains and beans.
Surprisingly, oxalate-rich foods, such as chocolate, nuts, tea, and spinach, are not associated with a higher risk of renal stones, nor is vitamin C, even though it can be converted to oxalate. A large study of men taking vitamin C supplements found that they had no more kidney stones than men who do not take them.
Staghorn refers to the presence of a branched kidney stone occupying the renal pelvis and at least one calyceal system.
Such calculi usually manifest as infection and hematuria rather than as acute pain,are most frequently composed of
struvite and/or calcium carbonate apatite.
cystine or uric acid, either in pure form or mixed with other components, can also grow in a "staghorn“.
but calcium oxalate or phosphate stones only rarely grow in this configuration.
Currently, the drug of choice replacing thiazides in treating idiopathic hypercalciuria is potassium citrate. excreted in the urine, it inhibits the crystallization of stone forming calcium salts by binding the calcium ion, thus decreasing its urinary saturation, One of the problems seen in some patients treated with potassium citrate, may result in an alkaline urinary milieu which promotes calcium phosphate stone formation,so urine must be monitored with dipsticks to maintain a pH level of 7-7.5 for stone prevention. A pH level of 6.5 is usually considered optimal. ???A pH level over 7.0 should be discouraged, as it prompts calcium phosphate precipitation.
A helical CT scan without contrast material is currently believed to be the best initial radiographic examination for acute renal colic. If positive, KUB radiography is recommended to assist in follow-up and planning.
• Extracorporeal shockwave lithotripsy ESWL
• Most urinary tract calculi that require treatment are currently managed with this ESWL, which is the least invasive of the surgical methods of stone removal. ESWL is limited somewhat by the size and location of the calculus.
• A stone larger than 1.5 cm in diameter or one located in the lower section of the kidney is treated less successfully. Fragmentation still occurs, but the large volume of fragments or their location in a dependent section of the kidney precludes complete passage. In addition, results may not be optimal in large patients, especially if the skin-to-stone distance exceeds 10 cm.
• Calcium, cystine, and struvite stones are all
• radiopaque, whereas pure uric acid, indinavir-induced• are relatively radiolucent on plain radiography.
• Staghorn Calculi: struvite , calcium carbonate apatite
• cystine or uric acid, either in pure form or mixed with
• other components, can grow in a "staghorn“.
• (but calcium oxalate or phosphate stones only rarely grow in this configuration. )
Urea-splitting organisms (urease-producing bacteria) include Proteus, Pseudomonas, Klebsiella, Staphylococcus, and Mycoplasma.
The solubility of calcium oxalate is not influenced by changes in urine pH.
The problem in diagnosis of UTI is that of contamination arising from voided specimens passing through the non-sterile distal urethra. For this reason, clinicians use the criteria of 105 bacteria/ml of “clean catch” urine to diagnose UTI. At this level (105 bacteria/ml), < 1% of the represent contaminants. At counts of 1000-10,000/ml, there is a 50/50 chance the result represents contamination. Such a count may represent true infection, but to be sure a second culture showing the same organism might be more convincing.
The second criteria for diagnosing UTI is the presence of pyuria (> 5 WBC/HPF) on the urinalysis.
Nutrition and Renal Disease
According to K/DOQI guidelinesNational Kidney Foundation's Kidney Dialysis Outcome Quality Initiative (K/DOQI)
in CKD patients stage 1-4, sodium is restricted to 2000 mg/d, calcium is restricted to 1200 mg/d, and potassium and phosphorus intakes should be correlated with laboratory values. Fluid intake can be unrestricted assuming normal urine output. Careful monitoring of laboratory values is necessary.
In stage 5, potassium, phosphorus, and fluid, as well as sodium and calcium, are restricted, depending upon the type of dialysis the patient is undergoing.
Patients on dialysis (stage 5) are known to lose certain water-soluble vitamins. However, patients in renal failure have decreased excretion of vitamin A, and vitamin A toxicity has been reported in some cases. Therefore, patients on dialysis should receive a multivitamin supplement that avoids excessive vitamin A.
• Current K/DOQI guidelines suggest a protein intake of 0.6-0.75 grams of protein per kilogram of body weight per day (g/kg/d) for patients in stages 1-4 of CKD.
• In stage 5, when patients are receiving dialysis, increased protein intake is suggested (approx. 1.2 g/kg/d).
• most (but not all) literature suggests that decreasing protein intake in CKD stages 1-4 can delay progression into stage 5.
• Finally, the amount of calories consumed in addition to the protein reduction is critical.
• Enough calories need to be consumed by CKD patients in stages 1-4 to spare protein from being used as a fuel. This prevents loss of lean muscle mass and protein-calorie malnutrition. Because of the cardiovascular risk discussed above, these extra calories should not come from foods that increase risk for cardiovascular disease.
• 35 kcals per kilogram of body weight per day for patients younger than 60 years for all 5 stages. An example of foods to add to the diet to increase calorie intake is given below .
Diet for Nephrotic Syndrome
A well-planned diet can replace lost protein and ensure efficient utilization of ingested proteins through provision of adequate calories. Dietary changes can also help control hypertension, edema, and hyperlipidemia, and slow the progression of renal disease.Protein: High-protein diets are not recommended as they may encourage damage to the nephrons, leading to a progression of renal insufficiency. Since albumin losses in nephrotic patients are due to increased catabolism, rather than a reduction in protein synthesis, low-protein diets, which decrease catabolism, may be more beneficial.
The optimal amount of dietary protein necessary to prevent protein catabolism and progression of renal disease has not been established. A common recommendation is 0.6 grams of protein per kilogram of ideal body weight, adjusted depending on the glomerular filtration rate and nutritional status, plus gram-for-gram replacement of urinary protein losses.
• Energy: Calorie intake should be adequate to achieve and maintain ideal body weight and maintain protein stores. Foods rich in complex carbohydrates should provide the majority of calories.
• Supplements: Patients with nephrotic syndrome are often low in B vitamins and zinc, and can benefit from supplements. In addition, since a significant portion of serum calcium is protein-bound, it tends to be low when serum proteins are reduced. No modification is routinely needed for potassium, but potassium losses due to secondary hyperaldosteronism may require replacement.
Indications for Dialysis -In Chronic Renal Failure
Uremic PericarditisUremic Encephalopathy or Neuropathy
Pulmonary edema (unresponsive to diuretics)
Severe Hypertension
Severe hyperkalemia
Intractable acidosis
Severe Bleeding diathesis
Persistent gastrointestinal symptoms
S.Creatinine more than 12 mg/dl, BUN more than 100 mg/dl
• Specific indications for peritoneal dialysis
• Patients with cardiovascular or hemodynamic instability
• Hemodialysis patients with vascular access failure or can not be created (e.g. diabetic patients(
• High risk of anticoagulation
• Patients in the older age group (over 65) and small children
• Severe hemodialysis-related symptoms or disequilibrium
• Social reason
• Indications for Dialysis other than chronic renal failure
• Acute renal failure• Poisons and Drug intoxication
• Hypercalcaemia
• Hyperuricemia
• Hypothermia
• Metabolic alkalosis.
• Absolute
• Peritoneal fibrosis• Pleuroperitoneal leak
• Relative Major
• Chronic Ostomies
• Severe hypercatabolic state
• Fresh aortic prosthesis
• Recent Abdominal surgery
• Recent Thoracic surgery
• Extensive Abdominal adhesions
• Quadriplegia
• Blindness
• Physical handicaps
• Mental Retardation
• Polycystic Kidney disease
• Diverticulosis
• Obesity
• Peripheral vascular disease
• Hyperlipidemia
• Social
Complications during Hemodialysis
a. Medical Complications
Common Complications during Hemodialysis
1- Hypotension (20-30% of dialyses)
2- Muscle Cramps (5-20% of dialyses)
3- Nausea and Vomiting (5-15%of dialyses)
4- Headache (5% of dialyses)
5- Chest Pain (2-5% of dialyses)
6- Back Pain (2-5%of dialyses)
7- Itching (5% of dialyses)
8- Fever and chills (<1%of dialyses)
b. Mechanical Complications
1.Rupture dialyzer
2.Clotted dialyzer
3. Air embolism
4.High conductivity
5.Low conductivity
6.Low water pressure
7.High venous pressure
8.Abnormal arterial pressure
9.Electrical failure
10.Needle-site bleeding
11.Hemolysis
• Serious complications during hemodialysis
• 1-Disequilibrium syndrome
• 2-First use syndrome
• 3-Arrhythmia
• 4-Cardiac tamponade
• 5-Intracranial bleeding
• 6-Seizures
• 7-Hemolysis
• 8-Air embolism
• An elevated BUN in the setting of a relatively normal creatinine may reflect
• A physiological response to a relative decrease of blood flow to the kidney (as seen in heart failure or dehydration) without indicating any true injury to the kidney.• Excessive formation of urea seen in bleeding in the upper gastrointestinal tract. The nitrogenous compounds from the blood are resorbed as they pass through the rest of the GI tract and then broken down to urea by the liver
• Enhanced metabolism of proteins will also increase urea production, as may be seen with high protein diets, steroid use, burns, or fevers .
• A low BUN usually has little significance, but its causes include
• liver problems
• malnutrition
• excessive alcohol consumption.
• Overhydration from intravenous fluids.
• pregnancy
Microalbuminuria
AER of 20–200 μg/min , (30 to 300 mg/L or day)
or an albumin:creatinine ratio > 2 mg/mmol
in at least two of three consecutive collections,in elderly patients will be subject to error due to urinary tract infection, prostatic disease and heart failure, all of which may cause raised AER unrelated to diabetic nephropathy. For this reason, it is our practice not to screen beyond the age of 70 years.
• Bence-Jones proteins
• Waldenstrom's macroglobulinemia• Chronic lymphocytic leukemia
• Amyloidosis
• Malignancies (e.g., lymphoma, other cancers)
• Multiple myeloma
Myoglobinuria
HemoglobinuriaPorphyrinuria
Porphobilinuria
Food-induced urine coloring (some foods, eg, beets, rhubarb, sometimes food coloring, may make urine appear red)
Drug-induced urine coloring ,phenazopyridine but sometimes cascara, diphenylhydantoin, methyldopa phenacetin, phenindione, phenolphthalein, phenothiazines, and senna .
Red urine
• Foamy urine and swelling (edema) are two signs of proteinuria
• foamy urine may also be caused by bilirubin in the urine
• retrograde ejaculation,
• pneumaturia (air bubbles in the urine) due to a fistula,
• or drugs such as pyridium
• Cyclosporine can be nephrotoxic and can cause hirsutism, hypertension, and gingival hypertrophy.
The metabolic acidosis caused by RTA is normal anion gap acidosis.
It is calculated by subtracting the serum concentrations of chloride and bicarbonate (anions) from the concentrations of sodium plus potassium (cations):= ( [Na+] +[K+] ) - ( [Cl-]+[HCO3-] ) .
However, for daily practice, the potassium is frequently ignored because potassium concentrations, being very low, usually have little effect on the calculated gap. This leaves the following equation:
= ( [Na+] ) - ( [Cl-]+[HCO3-] ) .
The average anion gap for healthy adults is 8-12 mEq/L. The drop in HCO3-is compensated by an increase in Cl- and hence is also known as hyperchloremic acidosis.
Proximal type 2 RTA renal loss of HCO3- failure to recover sufficient bicarbonate ions from the filtrate in the proximal tubule
Distal type 1 RTARenal failure ,hypoaldosteronism,Ingestions ammonium chloride .Acetazolamide.hyperalimentation . insufficient secretion of hydrogen ions into the distal tubule.
High anion gap In these conditions, bicarbonate concentrations decrease, in response to the need to buffer the increased presence of acids (as a result of the underlying condition). The bicarbonate is replaced by the unmeasured anion resulting in a high anion gap.
Lactic acidosis
Ketoacidosis
Toxins: Ethylene glycolLactic acid Methanol Propylene Glycol PhenforminAspirin CyanideIron isoniazid
Low anion gap largely associated with hypoalbuminaemia . Nephrotic, cirrhosis.
Cloudy urine can be caused by pus ,blood ,sperm, bacteria, yeast, crystals, stones, mucus, or a parasite infection, such as trichomoniasis,protein, high doses of B vitamins or vitamin C which are water soluble, dehydration, drinking large amounts of milk can cause urine cloudiness due to the presence of phosphates in the milk.
RBCs < 3/HPF may be normal (< 5/HPF is sometimes normal, eg, after exercise). On microscopic analysis, glomerular RBCs are dysmorphic, with spicules, folding, and blebs; nonglomerular RBCs retain their normal shape.
WBCs < 5/HPF may be normal;
Pyuria defined as > 5 WBCs /HPF in a sample of centrifuged urine.
Allopurinol treatment was associated with slower progression of renal disease.
allopurinol treatment was associated with a 71% reduction in cardiovascular risk."Allopurinol decreases C-reactive protein and slows down the progression of renal disease in patients with chronic kidney disease.
Most species of bacteria that colonize in the urine cause nitrates, which are derived from dietary metabolites, to be converted to nitrites. In healthy people, both the urinary nitrite test and the leukocyte esterase (LE) tests are negative.
A negative nitrite test does not necessarily mean that the urine is free of all bacteria, particularly if there are clinical symptoms, because some bacteria do not produce nitrites.
Urinary Nitrites and Leukocyte Esterase
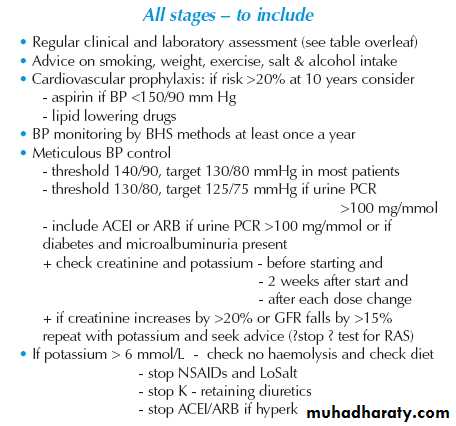
The renoprotective benefits of ACE inhibitors or ARBs are not seen in patients with chronic kidney disease who do not have diabetes or proteinuria. Since cardiovascular disease is the most common cause of complications and death among patients with chronic kidney disease, particularly when they also have diabetes, ACE inhibitors or ARBs should be considered for the treatment of hypertension in these patients. The propensity for hyperkalemia increases with declining glomerular filtration rate, and therefore these agents should be used with caution in patients with advanced chronic kidney disease, with or without proteinuria.
However, doses sufficient to lower blood pressure to target levels may not reduce proteinuria optimally, and residual proteinuria is a risk factor for progression. Evidence suggests that more effective blockade of the renin–angiotensin system, rather than simply more effective blood-pressure control, confers maximal renoprotection. Some, but not all, studies show that doses of ACE inhibitors or ARBs above the maximum recommended doses achieve a greater reduction in proteinuria than do conventional doses in patients with chronic kidney disease — both those with diabetes and those without diabetes.
A slow deterioration in renal function is not a contraindication to the use of ACE inhibitors in patients with renal insufficiency, but a rapid progressive rise in serum creatinine following initiation of ACE inhibitors should trigger immediate discontinuation of the agent and further evaluation of the patient for advanced renovascular disease.