د. حسين محمد جمعه
اختصاصي الامراض الباطنةالبورد العربي
كلية طب الموصل
2012
Panorama 4In Medicine
What Is Obesity?
Obesity is an excess proportion of total body fat. occurs when a person consumes more calories than he or she burns, eating too much and exercising too little. But there are other factors that also play a role.A person is considered obese when his or her weight is 20% or more above normal weight. A person is considered overweight if his or her BMI is between 25 and 29.9; a person is considered obese if his or her BMI is over 30.
"Morbid obesity”50%-100% over normal weight, more than 100 pounds over normal weight, a BMI of 40 or higher, or is sufficiently overweight to severely interfere with health or normal function.
"apple shape" -- a so-called, "potbelly" or "spare tire" you carry more fat in and around your abdominal organs. Fat deposited primarily around your middle increases your risk of many of the serious conditions . Greater than 95% of those who lose weight regain the weight within five years. The goal of treatment should be to achieve and maintain a "healthier weight", not necessarily an ideal weight.
Even a modest weight loss of 5% to 10% of initial weight and the long-term maintenance of that weight loss can bring significant health benefits by lowering blood pressure and lowering the risks of diabetes and heart disease.
Chances of long-term successful weight loss are enhanced if the doctor works with a team of professionals including dietitians, psychologists, and exercise professionals.
Fat cells are more insulin resistant than muscle cells; therefore,one important cause of insulin resistance is obesity. One genetic cause of obesity is leptin deficiency. Leptin is a hormone produced in fat cells, and also in the placenta. Leptin controls weight by signaling the brain to eat less when body fat stores are too high. The role of leptin replacement as a treatment for obesity is currently being explored.
A diet high in simple carbohydrates. The role of carbohydrates in weight gain is not clear. Carbohydrates increase blood glucose levels, which in turn stimulate insulin release by the pancreas, and insulin promotes the growth of fat tissue and can cause weight gain.
Frequency of eating. The relationship between frequency of eating (how often you eat) and weight is somewhat controversial. There are many reports of overweight people eating less often than people with normal weight. Scientists have observed that people who eat small meals four or five times daily, have lower cholesterol levels and lower and/or more stable blood sugar levels than people who eat less frequently (two or three large meals daily). One possible explanation is that small frequent meals produce stable insulin levels, whereas large meals cause large spikes of insulin after meals.
Medications.
certain antidepressants ,anti-convulsants such as carbamazepine ,valproate, insulin, sulfonylureas and thiazolidinediones), certain hormones such as oral contraceptives and most corticosteroids such as Prednisone. Weight gain may also be seen with some high blood pressure medications and antihistamines.BMI is a useful general guideline and is a good estimator of body fat for most adults 19 and 70 years of age. However, it may not be an accurate measurement of body fat for body builders, certain athletes, and pregnant women. Women typically collect fat in their hips and buttocks, giving their figures a "pear" shape. Men, on the other hand, usually collect fat around the belly, giving them more of an "apple" shape. (This is not a hard and fast rule; some men are pear-shaped and some women become apple-shaped, particularly after menopause). To find out a person's waist-to-hip ratio:
Measure the waist at its narrowest point, and then measure the hips at the widest point.
Divide the waist measurement by the hip measurement.
For example, a woman with a 35-inch waist and 46-inch hips would have a waist-to-hip ratio of 0.76 (35 divided by 46 = 0.76)Women with waist-to-hip ratios of more than 0.8 and men with waist-to-hip ratios of more than 1.0 are "apples."
Stratification by age
Current NICE recommendations represent an evolution of the view that blood pressure is best lowered with β blockers or ACE inhibitors in patients under 55 years (in whom an activated renin-angiotensin system may be an important mechanism) and diuretics or calcium channel blockers in older patients (because sodium retention, with suppression of the renin-angiotensin system, may be more important).Renin declines with age
In the TIMI IIIb study the use of recombinant tissue plasminogen activator (r-tPA) in patients with non-Q wave myocardial infarction or unstable angina was associated with increased death or later myocardial infarction and with a nearly statistically significant increase in intracranial haemorrhage.
Approximately 10% of medically treated patients presenting with unstable angina will suffer either myocardial infarction or death within 4-6 weeks of admission
Metformin treatment has been associated with a lactic acidosis following coronary angiography. In elective procedures metformin should be stopped 48 hours before radiocontrast exposure. Metformin should not be restarted for 48 hours after radiocontrast and until the creatinine has been ascertained to be normal.
Type 2 diabetes mellitus (T2DM) is a common
disease affecting ,3–5% of people living in the
western world. Cardiovascular disease (CVD)
((coronary heart disease (CHD), stroke and peripheral
vascular disease)) is the most important cause
of mortality and morbidity among patients with
T2DM. Compared with a non-diabetic individual,
a person with T2DM has a two- to fourfold
increased risk of dying from a myocardial infarction
(MI) or astroke and a 10- to 15-fold
increased risk of a lower extremity amputation.
T2DM presenting after an acute MI should have intensive glucose control by whichever means as long as glucose control is efficient.
A convenient way would be to start patients presenting with an acute MI and blood glucose >11.0 mmol/l on a 24 h insulin–glucose infusion followed by either insulin treatment, oral hypoglycaemic agents or dietary advice depending on blood glucose values.
A 1% reduction in HbA1c reduces CHD risk by approximately 16%.
A reasonable goal to aim for would be fasting blood glucose of 5–7 mmol/l.
A target for postprandial glucose remains contentious. The American Diabetes Association (ADA) recommends a value <10.0 mmol/l after subjects have achieved theirpre-meal glucose target, while the American
Association of Clinical Endocrinologists (AACE)
recommends a postprandial target <7.8 mmol/l. The European Association for the Study of Diabetes (EASD/IDF) has set a postprandial target of ≤7.5 mmol/l. Both the AACE and Joint British Society (JBS 2) guidelines recommend HbA1c ≤6.5%.
BPH, a histologic diagnosis, is a condition that occurs with aging; the prevalence increases from 25% among men 40 to 49 years of age to more than 80% among men 70 to 79 years of age.
Benign Prostatic Hyperplasia and Lower Urinary Tract Symptoms
Clinical Pearls
What are the lower urinary tract symptoms associated with BPH?The symptoms are classified as obstructive voiding or bladder storage symptoms.
Obstructive voiding symptoms include urinary hesitancy, delay in initiating micturition, intermittency, involuntary interruption of voiding, weak urinary stream, straining to void, a sensation of incomplete emptying, and terminal dribbling.
Storage symptoms include urinary frequency, nocturia, urgency, incontinence, and bladder pain or dysuria.
What are the risk factors for developing BPH?
In addition to increased age, additional risk factors include black (vs. white) race, obesity, diabetes, high levels of alcohol consumption, and physical inactivity; mechanisms underlying these associations remain poorly understood. Physiological markers associated with an increased risk of benign prostatic hyperplasia include levels of endogenous testosterone and dihydrotestosterone as well as increased levels of dehydroepiandrosterone and estradiol, insulin-like growth factors, and inflammatory markers (e.g., C-reactive protein).Physiological markers associated with an increased risk of benign prostatic hyperplasia include levels of endogenous testosterone and dihydrotestosterone as well as increased levels of dehydroepiandrosterone and estradiol, insulin-like growth factors, and inflammatory markers (e.g., C-reactive protein).
Morning Report Questions
Q. What office evaluation should be performed when a diagnosis of BPH is being considered?A. Evaluation includes a complete history to rule out alternative causes of lower urinary tract symptoms, including consideration of excess fluid and caffeine intake and the use of diuretics or medications with antihistaminic effects that may weaken bladder detrusor function. A digital examination of the prostate should be performed and a PSA measurement obtained. A urinalysis should be ordered to screen for urinary tract infection and to look for hematuria, which might indicate urolithiasis or cancer of the kidney, bladder, or prostate.
Urinary tract infections should be treated. Evaluation should also include the use of the American Urological Association Symptom Index, a quantitative measure of the severity of lower urinary tract symptoms. If the patient reports a sense of incomplete bladder emptying or has a palpable bladder on abdominal examination, a post-voiding residual urine measurement should be obtained to rule out “silent” urinary retention (normal residual urine volume, <100 ml).
Q. How does one approach the treatment of BPH?
A. A reasonable approach would be to initiate an alpha-blocker (doxazosin), and then to increase the dose based on symptom response. If symptoms are still bothersome, a 5α-reductase inhibitor can be added as long as the PSA level is higher than 1.5 ng per milliliter (indicating prostatic enlargement).Another option, particularly if the patient also has erectile dysfunction for which he desires treatment, would be to prescribe a phosphodiesterase-5 inhibitor (currently only tadalafil is approved for these symptoms), since this agent could address both problems. In a randomized, placebo-controlled trial comparing doxazosin, a 5α-reductase inhibitor (finasteride), and the combination of the two, type 1 5α-reductase inhibitors (with or without alpha-blocker therapy), but not alpha-blocker therapy alone, significantly reduced rates of secondary outcomes of urinary retention and the need for invasive therapy for BPH.
When evaluating patients with chest pain the most important immediate cause of ST elevation to consider is ST elevation myocardial infarction (STEMI). The ST segments are typically convex and are often associated with reciprocal changes elsewhere. Concave ST elevation is a normal finding in many people, especially young men. Pericarditis can cause diffuse non-specific ST segment abnormalities but classically causes widespread saddle shaped elevation and may be association with depression of the PR interval.
Early repolarisation describes
elevation of the J point (the intersect between the QRS complex and the ST segment) and may be either notched or slurred. Early repolarisation is common and considered a normal variant, although it is more common in people who have survived acardiac arrest.
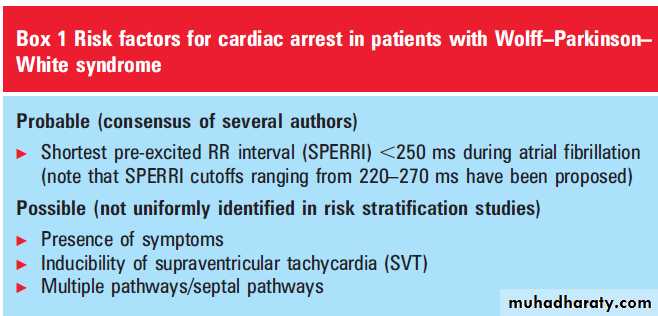
Left bundle branch block, left ventricular hypertrophy (fixed), and coronary spasm (transient) may also be associated with ST elevation. Finally Brugada syndrome is an inherited condition characterised by J point ST elevation and is associated with a risk of syncope and sudden death
Table 1. Targets for controlling diabetes and cardiovascular risk factors in people with diabetes.
Risk factor
OptimalBorderline
PoorValues are mmol/l unless otherwise specified
Plasma glucose
Fasting4.4-6.1
6.2-7.8
>7.8
Postprandial
4.4-8.0
8.1-10.0>10.0
Total cholesterol
<4.0
4.0-5.5>6.5
High density lipoprotein cholesterol
>1.1
0.9-1.1<0.9
Fasting triglycerides
<1.7
1.7-2.2>2.2
Body mass index (kg/m2)
Men
20-25
26-27>27
Women
19-24
25-26>26
Blood pressure (mm Hg)
<130/80*
130/80-140/80>140/80
Smoking
Non-smoker
Pipe/cigarettes*Stricter targets are needed in younger people and in people with early nephropathy who have a good life expectancy.
• Treatment targets
• Table 1 sets out recommended targets for controlling glucose, blood pressure, and lipids.
A 2011 Cochrane Review of 20 trials assessed the benefit of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in patients with type 2 diabetes. This demonstrated:
No significant difference between intensive and conventional glycaemic control (HbA1c 6.5% v 7.3%) for all cause mortality (RR 1.01, 95% CI 0.90 to 1.13) or cardiovascular mortality (RR 1.06, 95% CI 0.90 to 1.26) .Targeting intensive glycaemic control reduced the risk of amputation (RR 0.64, 95% CI 0.43 to 0.95; P = 0.03), the risk of retinopathy (RR 0.79, 95% CI 0.68 to 0.92; P = 0.002; 10,986 participants, 8 trials) and nephropathy (RR 0.78, 95% CI 0.61 to 0.99; P = 0.04).
The Joint British Societies (JBS) Guideline recommends that all patients who have had type 2 diabetes for more than 10 years and all patients with type 2 diabetes who are older than 40 years, have a sufficient level of cardiovascular risk to benefit from statin therapy, unless they have specific contraindications to its use.
• Aspirin
• Current JBS guidelines recommended low dose aspirin (75 mg) is prescribed for patients who have had type 2 diabetes for more than 10 years and all patients with type 2 diabetes who are older than 50 years.• However, a meta-analysis of the primary prevention of cardiovascular events in people with diabetes in 2009 demonstrates any CV benefit is offset by an increased risk of cerebral and gastrointestinal bleeding.
Metformin is contraindicated in patients with:
• Renal impairment (where the eGFR is <30 ml/min)• Liver failure
• Alcoholism
• Diabetic ketoacidosis
• Major surgery
• Sepsis.
For patients undergoing radiological intravascular contrast investigations metformin should be suspended prior to the test and restarted after 48 hours, provided renal function has returned to baseline.
Table 1. WHO thresholds for the 75 g oral glucose tolerance test
Fasting blood sugar
Two hours blood sugar after glucose tolerance testNormal
<6.1 mmol/l
<7.1 mmol/l
Gestational diabetes
≥6.1 mmol/l
>7.8 mmol/l
Diabetes mellitus
≥7.0 mmol/l
≥11.1 mmol/l
• Diagnostic criteria for diabetes in pregnancy
• Gestational diabetes is diabetes first detected during pregnancy. Clearly, some people may have previously undiagnosed diabetes, but this cannot be assumed or confirmed until postnatal testing is undertaken. Unless the patient presents with symptoms, it is usually diagnosed using a 75 g oral glucose tolerance test. The World Health Organization (WHO) thresholds for this test are given in Table 1.
National guidelines on gestational diabetes advise performing an oral glucose tolerance test screening if any of the following risk factors are present:
• BMI over 30
• Previous macrosomic baby weighing over 4.5 kg
• Previous gestational diabetes
• First degree relative with diabetes
• South Asian, black Caribbean, or Middle Eastern origin
National guidelines support the use of metformin and glibenclamide in pregnancy to treat gestational diabetes following a systematic review of all trial data.3 Metformin crosses the placenta, while glibenclamide does not. Data from observational studies suggest metformin and glibenclamide do not have any teratogenic effects, but there are no large randomised control trials of their use in early pregnancy.
Glibenclamide can be used from 11 weeks’ gestation, Metformin is now approved in national guidelines for treating women with gestational diabetes.
Insulin is generally well accepted by women if needed to achieve glycaemic control.
National guidelines advocate the use of short acting insulin analogues (insulin aspart, or insulin lispro, or both).These tend to be better than human insulin because they are associated with fewer hypoglycaemic episodes. Immediately after delivery, women with gestational diabetes should stop all hypoglycaemic medications. You should offer a blood glucose check
Organogenesis occurs during the first 12 weeks of gestation and hyperglycaemia is teratogenic, so you should aim to achieve good glycaemic control before conception. There is a threefold increase in cardiac and neural tube defects in diabetic pregnancies. These organs form before the sixth week of gestation, which is before most women realise that they are pregnant.
Metformin has long been used in early pregnancy as it is used to promote fertility in women with polycystic ovary syndrome. Several studies have shown that metformin exposure in the first trimester is not associated with an increase risk of major congenital malformations.
An HbA1c level over 10% has been shown to be associated with a 35% risk of congenital malformations and an increased miscarriage rate.
You should advise women to avoid pregnancy until their glycosylated haemoglobin levels have fallen. You should offer women monthly HbA1c measurements before conception to monitor their control.
This target will not always be safely achievable, particularly without unacceptable levels of hypoglycaemia. Also, it may be difficult to maintain an HbA1c level of <6.1% until pregnancy is achieved. Clinicians should support women in their attempts to achieve tight control, but compromise HbA1c values may need to be agreed. Before the NICE guidelines, the accepted level many clinicians used was <7%.
You should ensure that patients start folic acid at a high dose (5 mg not 400 µg daily) ideally at least three months before conception, and continued until the end of the first trimester.
During labour the patient should aim to keep blood glucose between 4 mmol/l and 7 mmol/l. There is an increased risk of a neonate born to a diabetic mother becoming hypoglycaemic within the first 24 hours after birth. Maternal hyperglycaemia causes fetal hyperinsulinaemia. After delivery this excess production of insulin in the neonate can lead to hypoglycaemia. This can be reduced by tight glycaemic control during labour and feeding the baby within the first half hour after birth.
National guidelines now support the use of metformin during breast feeding because less than 0.3% passes into the breast milk, and conclude from this that it is safe to use.
The BNF endorses its use in breast feeding.
Both metformin and glibenclamide are compatible with breast feeding, which you should encourage.
Women should feed their babies, ideally, within 30 minutes of giving birth and then at frequent intervals. The neonate should not have a blood glucose level taken until two to four hours after delivery unless it is showing signs of hypoglycaemia. Admission to neonatal intensive care may be necessary for intravenous dextrose and monitoring if the baby has difficulty feeding or signs or hypoglycaemia with abnormal signs. These include:
Jitteriness ,Irritability ,Seizures ,Poor tone.
Other indications for transfer to neonatal intensive care include respiratory distress, jaundice, cardiac decompensation, or gestation of less than 34 weeks.
Patients with haemophilia are classified into three severity groups: severe, moderate, and mild. Patients with severe haemophilia have no measurable factor VIII or factor IX (<0.01IU/mL or <1%) and may bleed spontaneously without preceding
trauma. In patients with moderate and mild haemophilia, the plasma factor VIII or factor IX concentration is 0.02-0.05 IU/mL (or 2-5%) or 0.06-0.40 IU/mL (or 6-40%), respectively.
Excessive bleeding usually occurs after minor trauma, dental procedures, or surgery.
How should surgery be managed?
To prevent haemorrhage during surgical or dental procedures it is important to establish a perioperative management plan in advance of the procedure. Factor VIII or factor IX concentrations should be raised to 0.80-1.00 IU/mL immediately before surgeryand kept above 0.50 IU/mL for five to 14 days after the operation, depending on the type and site of surgery. Guidelines for perioperative care, based on a thorough review of the current literature, are available.
The sex of the fetus can be identified by Y chromosome PCR in maternal blood at around 10 weeks’ gestation or by ultrasound scan at 18-20 weeks’ gestation.
Future of haemophilia treatment
Several new developments in haemophilia care have emerged in the past few years. Long acting factor VIII and factor IX concentrates that enable less frequent prophylactic dosing are currently being tested in clinical trials. These proteins have been engineered by site directed glycopegylation or the fusion of albumin or IgG to the clotting factors. Several research groups have made great progress with gene therapy in the past few years.Noncardiac pulmonary edemaNot all pulmonary edema is the result of heart disease. Fluid may also leak from the capillaries in your lungs' air sacs because the capillaries themselves become more permeable or leaky, even without the buildup of back pressure from your heart. In that case, the condition is known as noncardiac pulmonary edema because your heart isn't the cause of the problem. Some factors that can cause noncardiac pulmonary edema are:
Lung infections. When pulmonary edema results from lung infections, such as pneumonia, the edema occurs only in the part of your lung that's swollen.
Exposure to certain toxins. These include toxins you inhale — such as chlorine or ammonia — as well as those that may circulate within your own body, for example, if you inhale some of your stomach contents when you vomit.
Kidney disease. When your kidneys can't remove waste effectively, excess fluid can build up, causing overload pulmonary edema.
Smoke inhalation. Smoke from a fire contains chemicals that damage the membrane between the air sacs and the capillaries, allowing fluid to enter your lungs.
Adverse drug reaction. Many drugs — ranging from illegal drugs such as heroin and cocaine to aspirin and chemotherapy drugs — are known to cause noncardiac pulmonary edema.
Acute respiratory distress syndrome (ARDS).
This serious disorder occurs when your lungs suddenly fill with fluid and inflammatory white blood cells. Many conditions can cause ARDS, including severe injuries (trauma), systemic infection (sepsis), pneumonia and shock.High altitudes. Mountain climbers and people who live in or travel to high-altitude locations run the risk of developing high-altitude pulmonary edema (HAPE). This condition — which typically occurs at elevations above 8,000 feet (about 2,400 meters) — can also affect hikers or skiers who start exercising at higher altitudes without first becoming acclimated. But even people who have hiked or skied at high altitudes in the past aren't immune.
Although the exact cause isn't completely understood, HAPE seems to develop as a result of increased pressure from constriction of the pulmonary capillaries. Without appropriate care, HAPE can be fatal.
Near drowning. Inhaling water causes noncardiac pulmonary edema that is reversible with immediate attention.
Many conditions are associated with pulmonary edema that appears to be due to diffuse damage and
increased permeability of alveolar-capillary membrane.
These conditions include
infectious (bacterial,viral, parasitic) septicemia,
trauma and disseminatedintravascular coagulation.
Also, shock lung in association with non-thoracic trauma, acute hemorrhagic pancreatitis, inhalation of toxic gases (smoke, ozone,
cadmion, phosgene, chlorine, nitrogen dioxide),
foreign substances (snake venom, alloxan,alpha-naphthyl thiourea)
endogenous vasoactive substances (histamine, kinins).
Burn, aspiration of gastric contents, inhalation of foreign body, acute radiation pneumonitis and drowning.
Pharmaceutical
Narcotic overdose
Chemotherapy
Salicylate intoxication
Calcium antagonist overdose
Hydrochlorothiazide
Contrast fluids
High-altitutde
Neurogenic
Pulmonary embolism
Eclampsia
Post cardioversion
Post anaesthesia
Post cardiopulmonary bypass
Special forms of non-cardiogenic pulmonary edema.
A recent consensus statement on terminology produced by the vascular medicine section of the
Royal Society of Medicine recommended abandoning the terms Raynaud’s syndrome and Raynaud’s disease because of the lack of consensus on their use
(Raynaud’s phenomenon: new insights, new treatments.
Conference organised by the Vascular Medicine Section of the Royal Society of Medicine. 2011 May).
In this review we refer to
primary and secondary Raynaud’s phenomenon. Patients with secondary Raynaud’s phenomenon are more likely to have severe disease, which, if left untreated, can progress to ulceration or gangrene of extremities.
What are the symptoms?
Patients with Raynaud’s phenomenon classically report intermittent triphasic changes in the colour of the extremities (fingers, toes, nose, cheeks, and ears)—usually triggered by cold exposure or emotional stress—from white (owing to vasoconstriction), to blue (tissue hypoxia), to red on rewarming
(reperfusion) (figs 1⇓ and 2⇓).
What causes Raynaud’s phenomenon?
The pathophysiology of Raynaud’s phenomenon is poorly understood and is thought to differ between primary and secondary disease.A recent review discussed pathogenesis.
Abnormalities of the blood vessel wall are thought to be functional in primary Raynaud’s phenomenon and structural in secondary disease.
Ask about drugs that may predispose patients to the phenomenon or aggravate it: β blockers, vinyl chloride, chemotherapy, ergot derivatives, amphetamines,
cocaine, oestrogen (unopposed oestrogen replacement therapy, oral contraceptives), clonidine, and sympathomimetics.
Also ask about current smoking because smoking aggravates the condition.
Cold stimulation test, which measures the response of the digits to cooling and rewarming.
Digits usually rewarm in less than 15 minutes, but in Raynaud’s phenomenon this phase is longer than 20 minutes.
Refer patients with suspected secondary disease for
capillaroscopy if possible because ophthalmoscopy (20×magnification, dermatoscope 10× magnification) can miss capillary changes. The gold standard method is videocapillaroscopy (200× magnification, or a biomicroscope).A patient with primary Raynaud’s phenomenon will have regular disposition of capillary loops along the nail bed. In contrast, patients with secondary disease will have architectural disorganisation, giant capillaries, haemorrhages, loss of capillaries, angiogenesis, and avascular areas (“scleroderma pattern,” seen in 95% cases of systemic sclerosis).
How is Raynaud’s phenomenon treated?
The first step in managing Raynaud’s phenomenon in primary care is lifestyle modification. Such advice can be given to patients while awaiting investigations and referral to secondary care if an underlying cause is suspected.Most people with primary Raynaud’s phenomenon respond well to lifestyle measures and need no further treatment.
Patients with secondary Raynaud’s phenomenon require treatment of the underlying disorder, which entails referral to secondary care.
Distinguishing primary and secondary Raynaud’s phenomenon
Primary disease
Younger age (<30, but can be any age)
Female
Genetic component (30% have an affected first degree relative
No symptoms/signs of underlying disease
No tissue necrosis or gangrene
Normal nail fold capillaries
Normal erythrocyte sedimentation rate
Negative antineutrophil antibodies
In an intravascular ultrasound study of the natural history of CAD, the plaque characteristics most predictive of subsequent coronary events were plaque burden, thin fibrous cap, and small luminal area (<4 mm2), not coronary calcium.
Therefore, the areas of coronary calcium visualized by
CT are not necessarily the same lesions that cause subsequent coronary events.
It should also be remembered that a CAC score of 0 does not mean that CAD is absent,particularly in younger patients who may have soft fatty atheromas.
A recent meta-analysis of data from more than 90 000 participants from 14 randomised trials of statins concluded that
statin therapy can safely reduce the five year incidence of major coronary events, coronary revascularisation, and stroke by 20% per mmol reduction in LDL cholesterol level.
Average cholesterol reduction strategy
The average reduction from baseline in total cholesterol level for the different statins was between 18% and 25%. Daily doses of statin required to achieve the middle of this range, a 22% reduction in total cholesterol level, are approximately:Fluvastatin 40 mg
Pravastatin 20 mg
Lovastatin 20 mg
Simvastatin 10 mg
Atorvastatin 5 mg
Rosuvastatin 2.5 mg.
The advantages of this strategy are reduced statin doses and costs and a possible reduced risk of dose related toxicity. The disadvantage is frequent blood tests.
GUIDELINES
The European Society of Cardiology (ESC) and theAmerican College of Cardiology/American Heart
Association (ACC/AHA) guidelines for intervention
in asymptomatic patients are summarised in table 2
and figures 3 and 4. Aortic valve replacement is
considered only in selected patients who have severe AS, as defined by Vmax ≥4 m/s peak aortic jet velocity, mean gradient≥40-50 mm Hg, and/or aortic valve area ≤1.0 cm2 or 0.6 cm2/m2 body surface area. Although Vmax and mean gradient are flow
dependent indices, they should be checked for
consistency with valve area, which is more subject
to errors of measurements and inaccuracy.
Aortic valve replacement is considered in moderate AS only in patients who need surgery on another valve, coronary arteries or ascending aorta.
Elderly Aortic valve replacement is generally not considered in asymptomatic elderly patients with AS because of the increase in the operative risk with age
At present, the use of transcatheter aortic valve
implantation (TAVI) is targeted towards symptomaticpatients who are at high risk for conventional
valvular surgery. In the future, it is possible
that TAVI will expand the indications of interventions
for AS to low risk patients, including asymptomatic patients. Such extension of indications
could be considered only when the long term
durability of devices has been demonstrated, and
when TAVI is proven to be feasible with a very low
risk in asymptomatic patients.
Elevated natriuretic peptides
B-type natriuretic peptide (BNP) and its inactive
amino-terminal portion (NT-proBNP) result from
the breakdown of proBNP and have vasodilator and diuretic effects.
Interestingly, these hormones are antagonists of the renin -angiotensin and adrenergic systems, and are released in response to myocardial wall stress.
LDL LOWERING
LDL lowering treatments Statins are competitive inhibitors of HMG-CoA reductase, the key rate limiting enzyme involved in cholesterol synthesis. They decrease primarily LDL cholesterol concentrations by upregulatingLDL receptor activity and decreasing entry of LDL into the circulation.
also favourably decrease fibrinogen concentrations and viscosity, increase activation of endothelial nitric oxide synthase, decrease C-reactive protein (CRP) independent of LDL lowering effects, modestly decrease triglycerides, and modestly increase HDL.
Tissue penetration may be less with the
hydrophilic pravastatin and rosuvastatin.All other statins are lipophilic.
Risk factors for statin toxicity include older age, females, small frail frame, multisystem organ disease, multiple medications, steroid use, excessive alcohol intake, and drinking >1litre of grapefruit juice a day. Drugs that inhibit cytochrome P-450 3A4 or 2C9 can increase serum statin concentrations, increasing risk of toxicity.
If patients develop symptoms indicative of myositis, CPK should be checked. Drug treatment should be discontinued if CPK elevation is >10X upper limits of normal. It is not clear what to do for lesser CPK
elevations and it is reasonable to decrease dosage to see if symptoms abate. If symptoms continue then cessation of drug is appropriate.
If CPK is not elevated from baseline but symptoms continue, aldolase may be a more specific test to identify muscle damage.
LOW HDL
Low HDL is often associated with combined hyperlipidaemia and metabolic syndrome but can occur in isolation. Regular aerobic exercise, weight loss (especially in abdominally obese individuals), moderate alcohol consumption, and smoking
cessation all have modest effects on improving HDL. Statins increase HDL by 10% on average.
Niacin increases HDL up to 20–35%.
Niacin increases HDL by inhibiting hepatic uptake of
apolipoprotein A-1 and increases plasma preb HDL cholesterol concentrations..
The metabolic syndrome
includesabdominal obesity and two of the following abnormalities:
high triglycerides (≥ 150 mg/dl (1.69 mmol/l) or on
triglyceride treatment), low HDL ≤40 mg/dl (1.02 mmol/l) for men and ≤ 50 mg/dl (1.28 mmol/l) for women or on HDL treatment), elevated blood pressure (≥ 130/85 mm Hg or on antihypertensive treatment), and elevated fasting blood glucose
≥ 100 mg/dl (5.5 mmol/l) (includes diabetes).
Patients with end stage heart failure fall into stage D of the ABCD classification of
the American College of Cardiology (ACC)/American Heart Association (AHA), and class III–IV of theNew York Heart Association (NYHA) functional classification; they are characterised by advanced
structural heart disease and pronounced symptoms of heart failure at rest or upon minimal physical
exertion, despite maximal medical treatment according to current guidelines.
While repeated or prolonged treatment with positive inotropic agents such as b-adrenergic agonists (dobutamine) and phosphodiesterase inhibitors (milrinone, enoximone) increases mortality and is not recommended for the treatment of chronic
heart failure, intermittent intravenous inotropic treatment may be used in cases of severe cardiac decompensation with pulmonary congestion and peripheral hypoperfusion, or as abridge to heart transplantation. However, treatment-related
Diabetes mellitus is the seventh leading cause of death in the United States.
In addition, it is a leading cause
of morbidity and leads to microvascular (retinopathy, nephropathy, and neuropathy) and macrovascular (coronary artery, cerebrovascular, and peripheral vascular disease) complications.
Patients with Eisenmenger syndrome are in the highest risk group and need special consideration because they present with cyanosis due to right-to-left shunt, which may increase with systemic vasodilation during pregnancy.
Cyanosis poses a particular risk to the fetus.
Live birth is unlikely with maternal
oxygen saturation <85%.
Intervention during pregnancy
Catheter intervention during pregnancy is reservedfor patients who develop serious problems and are at very high risk. Typically balloon valvulotomy
may be an option in patients with severe aortic
or mitral stenosis who develop heart failure during
pregnancy.
Because of the radiation exposure,the best time for intervention is after the fourth month.
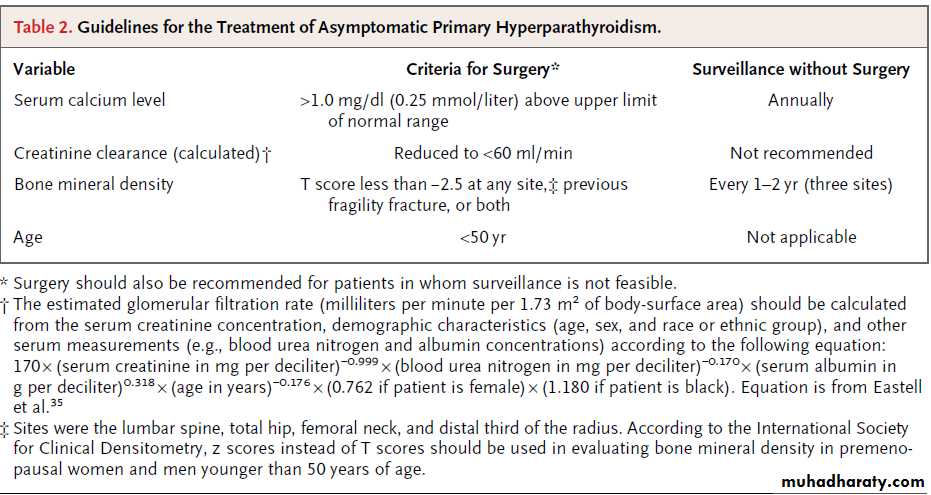
Evaluation
The finding of hypercalcemia on routine biochemicaltesting or in the evaluation of postmenopausal
women with osteoporosis is typically the initial clue to the diagnosis of primary hyperparathyroidism.
The total serum calcium level,which combines both the free and albumin-bound components of circulating calcium, should be adjusted for the level of albumin as follows: corrected or adjusted total calcium = (measured total
calcium in mg per deciliter) + [0.8 × (4.0 − patient’s
serum albumin concentration in g per deciliter)].
Measurement of ionized calcium may be useful
in selected cases, such as in patients with
• hyperalbuminemia,
• thrombocytosis,
• Waldenström’s macroglobulinemia, and
• myeloma; these patients
may have elevated levels of total serum calcium,
but normal levels of ionized serum calcium
(artifactual hypercalcemia).
DEFINITION
Although the wording varies in different publications,resistant hypertension is conventionally
defined as the failure to lower systolic and diastolic
(office) blood pressure to goal in patients who
are adhering to lifestyle measures and to the
optimal doses of an appropriate regimen of three
antihypertensive drugs from different classes, one
of which is a diuretic.
Prognosis
Within one year of having a first myocardial infarction, it has been reported that 25% of men and 38% of women will die.
Within six years of having a first myocardial infarction, 18% of men and 35% of women will have another myocardial infarction, 22% of men and 46% of women will have heart failure, and 7% of men and 6% of women will have sudden death.
Patients on simvastatin should avoid grapefruit juice
This is because grapefruit juice has been shown to increase the concentration of some CYP3A4 substrates such as simvastatin; even modest quantities of grapefruit juice can lead to a large increase in the concentration of simvastatin, thereby increasing the risk of rhabdomyolysisPatients on warfarin should avoid cranberry juice
Cranberry juice can cause the international normalised ratio to rise through an unknown pharmacodynamic interaction and so may cause bleeding in patients on warfarin.
When should warfarin be started?
There is no evidence from clinical trials to guide the timing of starting anticoagulation, but it seems reasonable to start it as soon as it is safe to do so. In patients with transient ischaemic attacks and atrial fibrillation, warfarin might be started once a computed tomography image of the brain has excluded haemorrhage.For patients with a minor stroke, warfarin may be started once they have been clinically stable for 48 to 72 hours.
For those with a more major stroke, the substantial risk of haemorrhagic transformation peaks within the first week, and warfarin may be started after two weeks.
Whether or not fixed doses of oral thrombin inhibitors can be substituted for warfarin is currently being studied.
The key is to predict which patients are at highest risk of early recurrence. One model (the ABCD2 system) uses:
A - age (≥60 years) (1 point)
B - blood pressure at presentation (systolic ≥140 mm Hg or diastolic ≥90 mm Hg) (1 point)
C - clinical presentation
Unilateral weakness (2 points)
Speech impairment without weakness (1 point)
Neither speech impairment or weakness (0 points)
D - duration of symptoms
≥60 minutes (2 points)
10-59 minutes (1 point)
<10 minutes (0 points)
D - presence of diabetes (1 point).
When added together, the total ABCD2 score ranges from 0 (low risk) to a maximum score of 7 points (high risk).
Stroke prophylaxis:AF
The risk of thromboemboli can be reduced with antiplatelet and warfarin therapy. You should treat high risk patients with anticoagulant therapy according to the CHADS2 scoring system. In this system patients are allocated a score based upon the presence of the following risk factors:
• Congestive cardiac failure
• Age over 75 years
• Hypertension
• Diabetes
• Stroke
The history of stroke is allocated two points and each of the other risk factors is allocated a single point. Patients are considered high risk for stroke and should be treated with anticoagulant therapy if they have a score of two points or more. Patients with a single point can be offered aspirin for stroke prophylaxis.
Learning bite
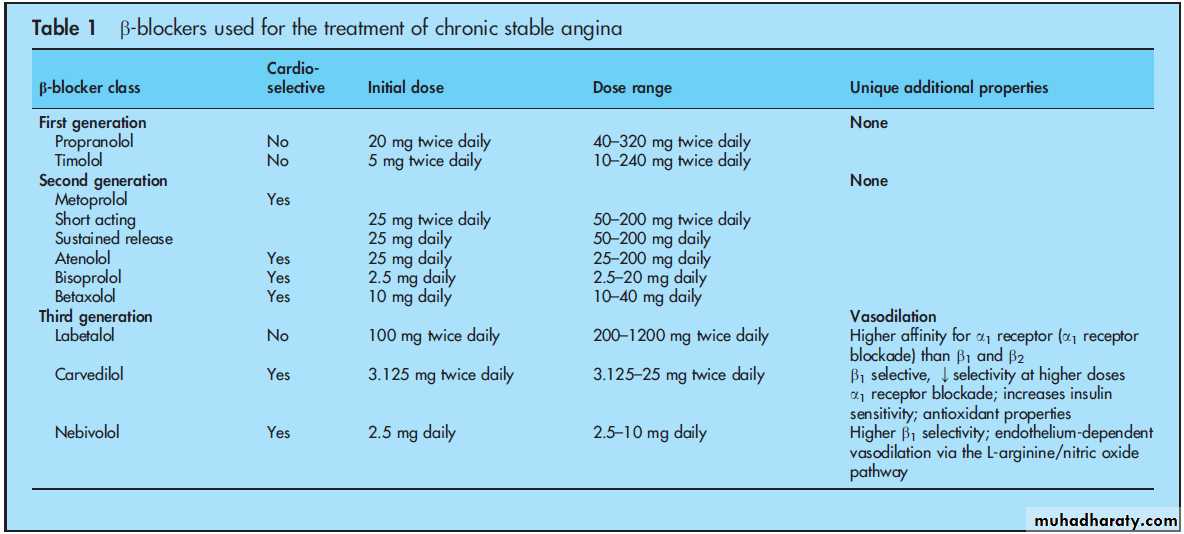
Although beta blockers have been shown to reduce symptoms and development of myocardial ischaemia in stable patients, they have not been shown to reduce mortality in these patients unless they have myocardial infarction or heart failure associated with a reduction in left ventricular systolic function.The use of steroids over as little as three weeks can cause adrenal suppression.
Adrenal suppression can last for as long as a year after a patient has stopped taking steroids (or even longer in rare cases).Signs of AV dissociation, such as a
variable intensity of the first heart sound and intermittent cannon waves in the jugular venous pressure, which may suggest a diagnosis of ventricular tachycardia.Table 3: Features that make a broad complex tachycardia likely to be ventricular tachycardia
History
Advanced age
A history of myocardial infarction, coronary artery disease, structural heart disease, or left ventricular dysfunction each mean that a diagnosis of ventricular tachycardia is likely
Examination
Evidence of AV dissociation, as shown by cannon waves in the jugular venous pulse
ECG features
QRS width >140 ms
Evidence of AV dissociation: independent P waves marching through the ventricular rhythm
Evidence of fusion or capture beats
QRS concordance in leads V1 to V6 (complexes all positive or all negative in polarity)
Axis shift of more than 40 degrees from sinus rhythm frontal axis
Other features
No termination or slowing of tachycardia with adenosine (other than right ventricular outflow tract ventricular tachycardia)
The following types of beats are also diagnostic of ventricular tachycardia:
Capture beats - intermittent narrow complex beats conducted from the atria to the ventricles via the AV nodeFusion beats - QRS complexes composed of both normally conducted beats and the abnormal complexes of ventricular tachycardia. Fusion beats have morphology features of both normal complexes and ventricular tachycardia complexes.
If there remains any doubt about the diagnosis, it is safest to assume the rhythm is ventricular tachycardia until proved otherwise. Haemodynamic stability does not exclude ventricular tachycardia.
Adenosine may be useful in differentiating ventricular tachycardia from supraventricular tachycardia if the patient is haemodynamically stable.
A response to oral amiodarone therapy may not be seen until three weeks after starting the drug.
Verapamil should be avoided if ventricular tachycardia is a possibility because it may cause profound hypotension. It should also be avoided in the treatment of supraventricular tachycardia in the setting of hypotension.
Torsades de pointes VT precipitated by a prolonged QT interval.
The best management would be temporary pacing at a rate that shortens the QT interval, along with correction of serum potassium and magnesium levels.