Panorama 6In Medicine
د. حسين محمد جمعهاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
AST/ALT ratio in these patients is typically 2:1 or more.
increased GGT levels with normal ALP levels and macrocytosis make alcohol induced liver damage more likely. Urea levels are often low in alcohol related cirrhosis due to reduced hepatic metabolism of protein and reduced protein intake.Alcoholic liver disease
Hazardous drinking is defined as a quantity or pattern of alcohol consumption that places patients at risk for adverse health events, while
harmful drinking is defined as alcohol consumption that results in adverse events (eg, physical or psychological harm).
Heavy drinking is defined as a quantity of alcohol consumption that exceeds an established threshold value.
• hazardous drinking was defined as an average consumption of 21 drinks or more per week for men (or 7drinks per occasion at least 3 times a week), and 14 drinks or more per week for women (or 5 drinks per occasion at least 3 times a week).
Because hazardous and heavy drinking are similarly defined (ie, a quantity or pattern of alcohol consumption that exceeds a specific threshold and may increase risk for adverse health events), we will use 1 term, hazardous drinking, to define this type of drinking disorder.
Harmful drinking is defined as alcohol consumption that results in physical or psychological harm.
Recommended amount of alcohol
The amount of alcohol contained in any alcoholic drink is measured in units. A unit is equivalent 10ml of pure alcohol.
The recommended daily limits for alcohol consumption are:
no more than 3-4 units per day for men
no more than 2-3 units per day for women
If you regularly exceed the recommended daily limits, you are putting your health at risk.
Pregnant women and women trying to conceive should avoid drinking alcohol. If they do choose to drink, they should not drink more than 1-2 units of alcohol once or twice a week and should avoid getting drunk.
How to measure units
Any drink that you buy will contain a measurement of its alcohol by volume (ABV). ABV is a measurement of how much of that drink is made up of pure alcohol.The easiest way to work out how many units of alcohol a drink provides is:
find out what the drink’s ABV is then multiply that by how many millilitres of liquid are in the drink then divide that by 1,000 So for a standard pint of strong lager:
its ABV would be 5% a pint contains 568ml
5 times 568 equals 2,840
divide that by 100, to give a measurement of 2.8 units
Types of alcohol misuse
• hazardous drinking• harmful drinking
• dependent drinking
Hazardous drinking
Hazardous drinking is defined as when a person drinks over the recommended weekly limit (21 units for men and 14 units for women).
It is also possible to drink hazardously by binge drinking, even if you stick within your weekly limit.
Binge drinking is when you drink an excessive amount of alcohol in a short space of time – eight units in a day for men, six units in a day for women.
Abinge drinker is defined as someone who drinks over half the recommended number of units for a week in a single session, eight units in a day for men, six units in a day for women, in a short space of time
Hazardous drinking, especially binge drinking, also carries additional risks such as:
being involved in an accident
becoming involved in an argument or fight
taking part in risky or illegal behaviour when drunk – such as drink driving
Harmful drinking
drinks over the recommended weekly amount and has experienced health problems directly related to alcohol.• depression
• alcohol-related accident
• acute pancreatitis
• high blood pressure ,heart disease
• cirrhosis
• cancer, mouth, liver, bowel and breast.
What Is Binge Drinking?
Binge drinking used to mean drinking heavily over several days. Now, however, the term refers to the heavy consumption of alcohol over a short period of time (just as binge eating means a specific period of uncontrolled overeating).Today the generally accepted definition of binge drinking in the United States is the consumption of five or more drinks in a row by men — or four or more drinks in a row by women — at least once in the previous 2 weeks. Heavy binge drinking includes three or more such episodes in 2 weeks.
Although there is no universal definition of mild, moderate, and severe abnormality of aminotransferase levels, the degree of abnormality can be practically considered to be:
Mild when the enzyme level is less than five times the upper reference value
Severe when AST and ALT levels are greater than 10 to 15 times the upper reference value.
Although not the rule, chronic liver diseases are often characterised by mild abnormality of aminotransferase levels, whereas severe abnormality is usually encountered in patients with acute hepatic injury.
Aminotransferases
Alanine aminotransferase (ALT) is considered more specific for hepatocellular injury because it is predominantly represented in the liver, with low concentrations in other tissues.Aspartate aminotransferase (AST) is also expressed in the heart, skeletal muscle, and red blood cells. AST and ALT are released in the bloodstream after hepatocellular injury (not necessarily hepatocellular death).
Abnormal GGT levels and normal ALP levels together with an AST predominant pattern and macrocytosis is suggestive of alcohol induced liver disease. In patients with alcoholic liver disease, the AST:ALT ratio is typically above 2 or greater.
The levels of alcohol associated with withdrawal vary between men and women. In men they are:
10 units of alcohol or more a day for 10 to 20 years. A unit is equivalent 10ml of pure alcohol.
In women they are:
7.5 units of alcohol or more a day for five to 10 years.Alcohol units
Alcohol consumption should not exceed 28 units for men and 21 units for women in one week.In a single drinking session, alcohol consumption should not exceed four units in men and three units in women.
Alcohol units are calculated by using:
The volume of alcohol in millilitres
The alcohol strength - this is its percentage alcohol by volume (% ABV).
One unit is equivalent to 10 ml of pure alcohol:
One standard glass of wine 175 ml at 12% ABV = 2.1 units
One bottle of wine 750 ml at 12% ABV = 9 units
One pint of beer 568 ml at 3.5% ABV = 2 units
One pint of beer 568 ml at 5% ABV = 2.8 units
One single glass of spirits 25 ml at 40% ABV = 1 unit.
A binge drinker is defined as someone who drinks over half the recommended number of units for a week in a single session
The two most serious complications of alcohol withdrawal are
delirium tremens and Wernicke’s encephalopathyBenzodiazepines are used in the treatment of alcohol withdrawal
withdrawal are at risk of seizures and hallucinations
Injectable anticoagulants
Injectable anticoagulants comprise:• Heparins
• Heparinoids
• Fondaparinux
• Hirudins.
The main mechanism for the anticoagulant activity of standard or unfractionated heparin is binding to antithrombin III, which catalyses the inactivation of factors IIa, Xa, IXa, and XIIa. Thrombin and factor Xa are most sensitive to the effects of heparin.
Low molecular weight heparins exert their effects almost entirely through inhibiting factor Xa.
Before starting, you should test the INR, APTT, platelets, and liver function. If the baseline INR is greater than 1.4, you should screen the patient for coagulopathies.
Heparinoids, such as danaparoid, have similar activity to that of LMWH , but contain no heparin or heparin fragments. Danaparoid is indicated only for treating venous thromboembolism in patients with a history of heparin induced thrombocytopenia.
Fondaparinux is licensed for prophylaxis of VTE in medical patients and in patients undergoing major orthopaedic surgery of the legs. It is also licensed for treating deep vein thrombosis and for pulmonary embolism.
Hirudins are polypeptides that inhibit factor IIa (prothrombin)
therefore be classed as direct thrombin inhibitors.Two products are available in the UK:
• Lepirudin is licensed for anticoagulation of people with heparin induced thrombocytopenia type II• Bivalirudin is licensed for patients undergoing PCI.
Clinical indications
The most common clinical indications for oral anticoagulation are:• Atrial fibrillation
• Treating and preventing venous thromboembolism
• Heart valve prostheses.
Warfarin is the most commonly used oral anticoagulant in the UK. Because oral anticoagulants act by interfering with the activation of clotting factors, it takes several days before the clotting factors already present are degraded and the full effects of a dose are seen.
Moreover, in the early stages of anticoagulation a temporary hypercoagulable state can be induced by the rapid depletion of the natural anticoagulant protein C.
The mean plasma half life of warfarin is 35-40 hours and the duration of effect is two to five days.
The antithrombotic effect of warfarin depends on the clearance of prothrombin, which has a half life of around 50 hours in patients with normal hepatic function.
So the full effects of starting warfarin or of increasing the dose are not seen for five days
Starting treatment: rapid anticoagulation
The goal of rapid anticoagulation is to achieve the target INR as quickly as possible. It takes five to 10 days for the full effects of warfarin to be seen and in the early stages a hypercoagulable state may be induced as a result of the rapid depletion of proteins C and S. For this reason, rapid anticoagulation is achieved using heparin. Heparin and warfarin are started together and heparin should continue until the INR has been in the therapeutic range for two consecutive days. This will usually be at least four or five days after starting. For rapid anticoagulation you must give a loading dose of warfarin starting at the same time as the heparin. Two dosing algorithms have been validated. The algorithms start from the basis that a healthy person would need 20-30 mg of warfarin over three days as a loading dose.
The dose is then reduced to take account of factors that increase sensitivity to the effects of warfarin : Body weight less than 50 kg,Low serum albumin,Age older than 65,Raised baseline INR,Interacting drugs (especially drugs that inhibit the metabolism of warfarin, such as metronidazole and erythromycin),Liver disease,Heart failure.
You should start patients older than 60 on a dose of about 5 mg.
Starting warfarin: slow induction
Introducing anticoagulation in the non-acute environment (for example for thromboprophylaxis in people with atrial fibrillation) should be started slowly because this avoids the risk of overanticoagulation and bleeding, which can occur with rapid anticoagulation. It also avoids the theoretical risk of evoking a paradoxical prothrombotic state.Patients with atrial fibrillation are at increased risk of thromboembolism and stroke,are likely to benefit from warfarin and in these groups slow induction of anticoagulation is suitable. One advantage of this approach is that the potential hypercoagulability seen with rapid anticoagulation does not occur. One way to start treatment is to give 1 mg of warfarin daily and then measure the INR after one week.Half lives of the vitamin K dependent clotting factors
FactorHalf life (hours)
II (prothrombin)
48-72
VII
2-6
IX
18-30
X
32-60
Protein C
6
Protein S
42
The dose of warfarin may need to be reduced in patients:
• With liver dysfunction
• With heart failure
• With hyperthyroidism
• Starting some drugs (for example those that inhibit warfarin metabolism (check details in the British National Formulary)) or discontinuing drugs that increase warfarin metabolism
With pyrexia.
The dose of warfarin may need to be increased in patients:
• With hypothyroidism
• Taking remedies containing vitamin K, for example some herbal remedies and enteral feeds
• Starting some drugs (for example those that increase warfarin metabolism) or stopping drugs that inhibit warfarin metabolism.
For rapid and complete reversal within 10-15 minutes give prothrombin complex concentrates (immediate replacement of vitamin K dependent coagulation factors) plus intravenous vitamin K.
Fresh frozen plasma immediately replaces vitamin K dependent coagulation factors, but the correction of the coagulopathy is partial.
Intravenous vitamin K alone would not bring the INR back to normal as quickly as the other agents
In patients taking warfarin
cranberry juice can cause the INR to rise and therefore cause bleeding
Large doses of vitamin K can render a patient "warfarin resistant" for a week or more.
Dental surgeryYou do not need to stop anticoagulation for dental surgery provided the INR is <3.
Safe practice tip
The practice of starting all patients on a three day dose regimen of 10 mg, 10 mg, 5 mg, and taking an INR on day four is unsafe.
A warfarin induction protocol
DayINR
Dose
1
<1.4 1.5-2.0 and patients >60 years >2.0
10 mg 5 mg None
2
No test required
10 mg 5 mg (if INR >1.4 on day 1 and patients >60 years)
3
<2.0 2.0-2.1 2.2-2.5 2.6-2.9 3.0-3.3 3.4-4.0 >4
10 mg 5 mg 4 mg 3 mg 2 mg 1 mg None
4
<1.4 1.4-1.5 1.6-1.7 1.8-1.9 2.0-2.3 2.4-3.0 3.1-4.0 4.1-4.5 >4.5
>8 mg 8 mg 7 mg 6 mg 5 mg 4 mg 3 mg Miss 1 day then 2 mg Miss 2 days then 1 mg
interactions with azole antibiotics, macrolides, quinolones, non-steroidal anti-inflammatory drugs, including selective cyclo-oxygenase-2 inhibitors, selective serotonin reuptake inhibitors, omeprazole, lipid-lowering agents, amiodarone, and fluorouracil, suggests that coadministration with warfarin should be avoided or closely monitored."Patients taking drugs that accelerate the metabolism of warfarin (for example rifampicin, barbiturates, and carbamazepine) will require more warfarin.
As a general rule the most common medicines causing clinically significant drug interactions with warfarin include NSAIDs, antibiotics, and amiodarone.
Recommended action following a high INR or bleeding
INR/bleedingAction
3.0 <INR <6.0 (target 2.5) or 4.0 <INR <6.0 (target 3.5)
Reduce or stop warfarin Restart when INR <5.0
6.0 <INR <8.0
Stop warfarin Restart when INR <5.0
INR >8.0, no bleeding or minor bleeding
Stop warfarin Restart when INR <5.0 If other risk factors for bleeding, give vitamin K 0.5-2.5 mg orally
Major bleeding
Stop warfarin Admit to hospital Give factor concentrate (prothrombin complex concentrate) plus intravenous vitamin K
Surgery
Unless there is a high risk of thromboembolism you should discontinue anticoagulation temporarily in preparation for surgery.Dental treatment
Patients whose INR is in therapeutic range (<4.0) do not need to stop anticoagulation for dental extraction. Oral tranexamic acid mouthwash can prevent bleeding after dental extraction.
Endoscopy without biopsy
Patients whose INR is in the therapeutic range (<3.0) do not need to stop anticoagulation for endoscopy.
In patients with renal failure (creatinine clearance <30 ml/min) there is a danger that low molecular weight heparin will accumulate (it is predominantly excreted by the kidneys). In this situation, unfractionated heparin is the treatment of choice. Alternatively, if you give low molecular weight heparin you must reduce the dose and monitor the patient closely
Thrombocytopenia, should it occur, usually appears between day 5 and 21 of treatment. If the platelet count is significantly reduced (30-50% of the initial value) you must stop therapy immediately and consider alternative therapy.
The anticoagulant effects of low molecular weight heparin are only partially reversible with protamine. The anticoagulant effects of unfractionated heparin can be reversed by protamine given by intravenous injection. A dose of 1 mg of protamine neutralises 80-100 units of unfractionated heparin when administered within 15 minutes of the heparin dose. Less is needed if protamine is given after a longer period because of the short half life of intravenous unfractionated heparin
Heparin can suppress adrenal secretions of aldosterone and lead to hyperkalaemia, particularly in patients with:
Diabetes mellitus
Chronic renal failure
Pre-existing metabolic acidosis
A raised plasma potassium.
The risk of hyperkalaemia appears to increase with the duration of therapy, but it is usually reversible. You should measure plasma potassium in at-risk patients before starting heparin therapy and you should monitor this regularly.
Pharmacokinetics of heparins
At usual intravenous doses the half life of unfractionated heparin is 45-60 minutes. The bioavailability of subcutaneous unfractionated heparin is less than 50%.Low molecular weight heparins have a half life of about four hours. They are 90-100% bioavailable after subcutaneous injection.
Absolute contraindications to anticoagulation are:
Potential bleeding lesionsActive peptic ulcer, oesophageal varices, aneurysm, and proliferative retinopathy
Recent organ biopsy
Recent trauma or surgery to the head, orbit, or spine
Recent stroke
Confirmed intracranial or intraspinal bleed
Uncontrolled hypertension
Infective endocarditis.
A history of heparin-induced thrombocytopenia or thrombosis is an absolute contraindication for using heparin.
Homozygous protein C deficiency (risk of skin necrosis) and a history of warfarin related skin necrosis are absolute contraindications to warfarin.
Relative contraindications to anticoagulation are:
History of gastrointestinal bleeding
Liver disease
Renal failure
Alcoholism
Mental impairment
Thrombocytopenia
Coagulation disorders
Interacting drugs, in particular non-steroidal anti-inflammatory drugs
Poor concordance
Poor attendance for regular blood tests
West Haven Criteria
The severity of hepatic encephalopathy is graded based on the level of impairment of autonomy, changes in consciousness, intellectual function, behavior, and the dependence on therapy.Grade 1 - Trivial lack of awareness; Euphoria or anxiety; Shortened attention span; Impaired performance of addition or subtraction
Grade 2 - Lethargy or apathy; Minimal disorientation for time or place; Subtle personality change; Inappropriate behaviour
Grade 3 - somnolence to semistupor, but responsive to verbal stimuli; Confusion; Gross disorientation
Grade 4 - coma
St John's wort can induce the metabolism of paracetamol leading to an increased rate of toxic intermediary formation (NAPQI). Other drugs that induce hepatic microsomal enzymes include:
• Phenytoin
• Phenobarbitone
• Rifampicin
• Carbamazepine
• Chronic ethanol ingestion.
Use of methionine is significantly limited by its lack of proved efficacy and high incidence of adverse effects, in particular nausea and vomiting. Acetylcysteine can be given orally, but is also associated with vomiting, and activated oral charcoal can significantly reduce the absorption of both methionine and oral acetylcysteine.
Intravenous acetylcysteine is therefore the treatment of choice.
Paracetamol overdose
threshold of toxicity
>150 mg/kg or 12 g
The best option is to determine serum paracetamol concentration at four hours and determine the need for acetylcysteine after calculating risk by referring to the nomogram. In addition, the following blood tests can help in the clinical assessment of patients with significant paracetamol poisoning:
Plasma glucose
Serum electrolytes including bicarbonate and lactate
Liver biochemistry
Full blood count
Arterial blood gases.
Original work on paracetamol poisoning in the late 1960s showed that serum concentrations >300 mg/kg at four hours after ingestion were always associated with hepatotoxicity. Serum concentrations less than 120 mg/kg at four hours after ingestion were unlikely to be associated with liver damage.
The standard treatment thresholds remain the same in the UK for adults and children at 150 mg/kg
Clinical tip
Around 73% of patients will present with dyspnoea and about 30% with tachycardia. Consider pulmonary embolism in patients with:Underlying malignancy
New onset atrial fibrillation
Chest wall pain (a rare, but recognised, cause of pulmonary embolism). Up to 50% of leg thrombi embolise.
Signs of a deep vein thrombosis are present in about 25% of patients with pulmonary embolism
Some 25% to 50% of patients with venous thromboembolism have an identifiable inherited thrombophilia, for example:
• Factor V Leiden gene mutation
• Deficiency of antithrombin III• A prothrombin gene defect
• Protein C deficiency
• Protein S deficiency.
These usually need to interact with an additional acquired risk factor to cause venous thromboembolism.
Only factor V Leiden (a genetic test) can be tested for while the patient is on anticoagulants. All other risk factors must be tested for off anticoagulation.
Who to screen for thrombophilia
Patients younger than 50 with recurrent idiopathic pulmonary embolism (ie those with more than one episode of proved venous thromboembolism, in whom no cause can be identified). Some 50% of these patients will have an identifiable thrombophilia.Those with a strong family history (ie where symptomatic venous thromboembolism has been proved in several family members in more than one generation).
Rare causes of pulmonary embolism include
Air embolismFollowing neck vein cannulation, bronchial trauma, and intrauterine manipulation (rare).
Small amounts of air can be tolerated,
but large amounts can lodge in the pulmonary vasculature and cause mechanical obstruction and death.
Venous air emboli may cause:
Raised venous pressure
Cyanosis
Hypotension
Tachycardia
Syncope.
Treatment is by lying the patient on their right side, with head down and feet up, to allow air to collect and stay at the cardiac apex. From here it can be aspirated. This may be done by ultrasound guided needle aspiration
British Thoracic Society pre-test probability scor
A standard assessment of pre-test clinical probability might include:
APatient has clinical features compatible with pulmonary embolism (raised respiratory rate, ± haemoptysis, ± pleuritic chest pain)
Plus two other factors:
1
Absence of another reasonable clinical explanation
2
Presence of a major risk factor
A plus 1 and 2:
High pre-test clinical probability
A plus 1 or 2:
Intermediate pre-test clinical probability
A alone:
Low pre-test clinical probability
The score includes clinical features consistent with pulmonary embolism (including a raised respiratory rate, haemoptysis, and pleuritic chest pain).
Heart rate is not included in most standard scores. The pre-test clinical probability score should always be used with the D-dimer test .
A low pre-test clinical probability score, combined with a negative D-dimer test has about a 90% sensitivity at excluding pulmonary embolism.
A negative test is unhelpful in those with a high clinical probability (and therefore should not be done in this situation).
D-dimer test
This is useful only for excluding pulmonary embolism, and should be used only with the pre-test clinical probability assessment. D-dimers are released as a result of fibrinolysis, and indicate the presence of intravascular thrombus.
A negative D-dimer test reliably excludes pulmonary embolism in patients with a low pre-test clinical probability.
Pregnancy
The diagnosis can be difficult to make in women who are pregnant. The standard pre-test clinical probability score should be used, recognising that pregnancy is a major risk factor for venous thromboembolism.The D-dimer test is of no use in this situation because it is raised (in the absence of pulmonary embolism) from about six weeks' gestation, and remains elevated until about three months post-partum.
Leg ultrasound
Up to 50% of patients with a clinically obvious deep vein thrombosis will have a high probability V/Q scan,and conversely around 70% of patients with proved pulmonary embolism will have a proximal deep vein thrombosis.
Caval Filter. Consider when a patient has recurrent thromboembolism despite adequate anticoagulation or when anticoagulation is contraindicated. They are usually for short term use only. They do prevent emboli though there are no data to show they affect mortality. May also be indicated in patients who survive acute massive pulmonary embolism (in whom a second pulmonary embolism may be fatal)
Unfractionated heparin has a quicker onset of action than low molecular weight heparin, and it is recommended in massive and submassive pulmonary embolism,
or where rapid reversal of anticoagulation may be needed.
A good listener appears interested, does not interrupt, and maintains focus.
A good listener listens with their eyes as well as their ears. A good listener appears interested, does not interrupt, and maintains focus.What is shock and why is it important?
Shock is a clinical state with diverse causes that occurs as a consequence of inadequate tissue perfusion, leading to an insufficient oxygen supply for the patient's metabolic requirements. This imbalance results in tissue hypoxia and lactic acidosis, which, if not promptly reversed, leads to progressive cellular injury, multiple organ failure, and death.
Shock is an important cause of morbidity, accounting for 34% of admissions to the intensive care unit, with mortality rates of 50-60% for septic shock and 60-80% for cardiogenic shock.
The pathophysiology of shock: global oxygen delivery and tissue oxygenation
Global indices of tissue oxygenationTo manage shock correctly you need to understand the principles of oxygen delivery and oxygen consumption. In an individual patient, the total amount of oxygen delivered to the tissues is the product of cardiac output and the arterial oxygen content. The arterial oxygen content depends on:
• Arterial oxygen saturation
• Haemoglobin levels
• The amount of oxygen dissolved in the plasma.
Normally, only 20-30% of the delivered oxygen is extracted by the tissues (oxygen extraction ratio). The remaining oxygen returns to the venous circulation and can be measured using a central venous catheter (central venous oxygen saturation) or in the pulmonary artery using a pulmonary artery catheter (mixed venous oxygen saturation).
Generally, shock is associated with a fall in oxygen delivery secondary to
• a reduction in cardiac output,
• arterial oxygen saturation, or
• haemoglobin levels.
To meet their oxygen requirements and maintain a constant oxygen consumption, the tissues adapt to the lower levels of oxygen delivered to the tissues by extracting a larger fraction of the delivered oxygen.
Tissues, however, cannot extract more than 60% of the oxygen delivered. Therefore, if oxygen delivery falls below a critical value, tissue hypoxia will result in a low mixed venous oxygen saturation (<65%) or central venous oxygen saturation (<70%) and anaerobic metabolism with increased lactate concentration.
Table 1: Causes of cardiogenic shock
CategoriesCauses
Myocardial diseases
Myocardial infarction or ischaemia
Cardiomyopathies
Myocarditis
Arrhythmias
Ventricular more commonly than supraventricular
Valvular diseases
Acute aortic regurgitation
Critical aortic stenosis
Mitral regurgitation caused by rupture of a papillary muscle or chordae tendineae
Ventricular septal defects
Obstructive
Pulmonary embolism
Tension pneumothorax
Constrictive pericarditis
Pericardial tamponade
Shock can be classified into three categories based on the cause.
1. Hypovolaemic shock
Hypovolaemia is the most common cause of shock. Inadequate circulating volume results from:
• Blood loss (trauma or gastrointestinal bleeding)
• Fluid loss (diarrhoea or burns)
• Sequestration of fluid in the third space (obstruction of the bowel or pancreatitis).
2. Cardiogenic shock
3. Vasodilatory shock
the tissue hypoxia is caused by an ineffective tissue oxygen extraction and the loss of vasoregulatory control leading to inappropriate vasodilatation and maldistribution of blood flow. Cardiac output is typically preserved or increased.
Causes of vasodilatory shock include:
• Severe sepsis (accounting for about 3% of hospital admissions and 15% of admissions to intensive care)
• Neurogenic shock after cerebral or spinal cord injury, leading to loss of vasomotor tone and bradycardia
• Anaphylaxis
• Drug reactions
• Adrenal failure
• And rarely conditions associated with the formation of peripheral shunts, such as chronic liver failure and Paget's disease.
Managing patients with shock
Shock is a medical emergency that requires prompt recognition and early, targeted interventions. The initial management of shock comprises general measures common to all types of shock, and specific interventions that vary according to the specific cause.
The goals of initial resuscitation are:
Mean arterial pressure >65 mm Hg
Central venous pressure 8-12 mm Hg
Urine output >0.5 ml/kg/h
Central venous oxygen saturation >70% (or a mixed venous oxygen saturation >65%)
Haematocrit 30%.
The predominant effects of dopamine are dose-related,
At low rates of infusion (0.5-2 mcg/kg/min) dopamine causes vasodilation that is presumed to be due to a specific agonist action on dopamine receptors in the renal, mesenteric, coronary, and intracerebral vascular beds. The vasodilation in these vascular beds is accompanied by increased glomerular filtration rate, renal blood flow, sodium excretion, and urine flow. Hypotension sometimes occurs.At intermediate rates of infusion (2-10 mcg/kg/min) dopamine acts to stimulate the beta1-adrenoceptors, resulting in improved myocardial contractility, increased SA rate and enhanced impulse conduction in the heart. There is little, if any, stimulation of the beta2-adrenoceptors (peripheral vasodilation). Dopamine causes less increase in myocardial oxygen consumption than isoproterenol, and its use is not usually associated with a tachyarrhythmia,increases systolic and pulse pressure with either no effect or a slight increase in diastolic pressure. Blood flow to the peripheral vascular beds may decrease while mesenteric flow increases due to increased cardiac out put . At low and intermediate doses, total peripheral resistance (which would be raised by alpha activity) is usually unchanged.
At higher rates of infusion (10-20 mcg/kg/min) there is some effect on alpha-adrenoceptors, with consequent vasoconstrictor effects and a rise in blood pressure. The vasoconstrictor effects are first seen in the skeletal muscle vascular beds, but with increasing doses they are also evident in the renal and mesenteric vessels.
At very high rates of infusion (above 20 mcg/kg/min), stimulation of alpha-adrenoceptors predominates and vasoconstriction may compromise the circulation of the limbs and override the dopaminergic effects of dopamine, reversing renaldilation and natriuresis.
Dobutamine is considered a direct
beta1-adrenergic agonist. It also has mild beta2- and alpha1-adrenergic effects at therapeutic doses. These effects tend to balance one another and cause little direct effect on the systemic vasculature. In contrast to dopamine, dobutamine does not cause the release of norepinephrine. It has relatively mild chronotropic, arrhythmogenic, and vasodilative effects. Increased myocardial contractility and stroke volumes result in increased cardiac output. Decreases in left ventricular filling pressures (wedge pressures) and total peripheral resistance occur in patients with a failing heart. Blood pressure and cardiac rate generally are unaltered or slightly increased because of increased cardiac output. Increased myocardial contractility may increase myocardial oxygen demand and coronary blood flow. MechanismSynthetic sympathomimeticamine
Overall effect similar to Dopamine with
Selective for Beta1-Adrenergic Receptors,
Increased cardiac contractility and Heart rate
Beta2-Adrenergic Receptors, Mild increase in vasodilation
Does not directly affect renal or splanchnic flow
Relatively mild Alpha1-adrenergic Receptors,effect
Vasoconstriction countered by more potent beta effect
Minimal effects on myocardial oxygen demand
Favorable balance between oxygen supply and demand
Preferred in cardiogenic shock over dopamine
Increased perfusion balances inotropic strain
Benefit lost if not titrated to avoid tachycardia
Does not increase infarct size
Does not elicit arrhythmia
Indications
cardiogenic shock
Often used in combination with Dopamine
• Moderate dosages of each (7.5 ug/kg/min)
• Maintains critical organ perfusion
• Less pulmonary congestion than with Dopamine alone
• Not shown to alter mortality
• May alter secondary organ injury outcomes
Septic Shock
May be useful in enhancing left ventricular function
Epinephrine is preferred agent in Septic Shock
Not usually indicated in non-cardiogenic shock.
Adverse Effects
Tachycardia
Arrhythmia
Provokes Myocardial ischemia if tachycardia occurs
Headache
Nausea
Tremor
Hypokalemia
Neurogenic
Neurogenic shock is associated with bradycardia and a vasoparalysis with a low central venous pressure.
Septic
Septic shock in the established phase is often characterised by a high cardiac index, high central venous oxygen saturation, and low central venous pressure.
Cardiogenic
Patients usually have hypotension, reduced central venous oxygen saturation, reduced cardiac index, and a raised central venous pressure.
Anaphylactic
Anaphylactic shock is often characterised by a high cardiac index, high central venous oxygen saturation, and low central venous pressure.
Hypovolaemic
Hypovolaemic shock is characterised by a low cardiac index, low central venous oxygen saturation, and low central venous pressure.
A central venous catheter
The oxygen saturation of blood sampled from a central venous catheter is the central venous oxygen saturation.
A peripheral venous line
The oxygen saturation of blood sampled from a peripheral line is generally used to assess global tissue hypoxia.
Stroke is the third most common cause of death in the UK.
Morbidity and mortalityTen to twenty percent of strokes are fatal. For the survivors, stroke results in many long term problems. These include:
• Chronic physical disability
• Dementia
• Depression
• Epilepsy
• Falls.
Stroke is the most common cause of neurological disability in the UK - a third of patients remain disabled. It makes stroke a costly problem - it accounts for up to 6% of all NHS resources.
There are two main types of stroke:
About 85% of strokes are ischaemic in origin
Fifteen per cent are due to haemorrhage. These can be subdivided into
Intracerebral haemorrhages - about 12-13%
Subarachnoid haemorrhages - about 2-3%.
There are several further ways to classify subtypes of ischaemic stroke. The commonly used Oxfordshire Community Stroke Project(OCSP) classification is the most validated tool for the classification of stroke. It divides stroke subtypes into:
• TACI - Total anterior circulation infarct
• PACI - Partial anterior circulation infarct
• LACI - Lacunar infarct
• POCI - Posterior circulation infarct.
Differential diagnosis
Four important differential diagnoses to consider are:
• Migraine with aura
• Focal epilepsy
• Brain tumour
• Hypoglycaemia.
OCSP classification also provides some prognostic information, with the prognosis being worst in patients with a total anterior circulation infarct and best in patients with a lacunar infarct.
(TACI) includes all of:
• Higher dysfunction (dysphasia, visuospatial neglect)
• Motor and/or sensory deficit
• Homonymous hemianopia
(PACI) includes:
• Two of the three criteria for a TACI or
• Higher dysfunction alone or
• A limited motor or sensory deficit
(LACI) includes :
Any of:
Pure motor deficit (affecting face, arm, and leg)
Pure sensory deficit (affecting face, arm, and leg)
Sensori-motor deficit (affecting face, arm, and leg)
Ataxic hemiparesis
None of:
Higher dysfunction (dysphasia, visuospatial neglect)
Isolated proprioceptive loss
Features of a posterior circulation infarct
(POCI) includes any of:
Cranial nerve palsy and contralateral motor/sensory deficit
Bilateral motor and/or sensory deficit
Conjugate eye movement disorder
Cerebellar dysfunction without ipsilateral long tract signs
Isolated homonymous hemianopia
Higher dysfunction alone
A limited motor or sensory deficit.
Tips on how to localise an infarct
In a lacunar stroke, weakness typically affects the face, arm, and leg equally.
An infarct affecting the motor cortex typically causes weakness that affects the face, arm, and leg to a different extent –
middle cerebral artery infarct, the face and arm are usually much weaker than the leg.
Anterior cerebral artery infarcts typically present with contralateral leg weakness.
A stroke causing isolated homonymous hemianopia is most likely due to a contralateral posterior cerebral artery infarct affecting the occipital cortex.
CT brain
Most widely used method, as it is widely available and scanning times are relatively short. A disadvantage of CT is the poor resolution it has for structures in the posterior fossa, which are often obscured by artefact from the surrounding bones. Furthermore, it takes at least a few hours for a cerebral infarct to become easily visible on CT. Changes of early infarction on CT may be present but detecting these requires experience and training.Magnetic resonance imaging
allows more detailed imaging of the brain than CT, in particular, of the posterior fossa structures. Its main limitation is that it is not yet as widely available as CT and that scanning times are longer.
also offers scanning sequences that are particularly helpful in stroke. Diffusion weighted imaging shows the brain territory affected by acute ischaemia, very early after the event ,even within minutes of the onset of symptoms. This can be helpful when deciding whether to give thrombolysis.
As diffusion weighted imaging only shows recent infarcts, it is easier to differentiate new from old infarction, which may be harder to do on CT or standard magnetic resonance imaging.
Potential structural causes of cardiac embolism include:
• Intracardiac thrombus• Left ventricular aneurysm with thrombus
• Atrial myxoma
• Bacterial endocarditis
• Valvular lesions
• Patent foramen ovale - (this is controversial).
Morning headache is not a typical feature of migraine with aura. Morning headache may indicate
1. increased intracranial pressure,
2. nocturnal carbon dioxide retention,3. or nocturnal hypoglycaemia.
As soon as the diagnosis of unstable angina or NSTEMI is made, and aspirin and antithrombin therapy have been offered, formally assess individual risk of future adverse cardiovascular events using an established risk scoring system that predicts six month mortality (for example, Global Registry of Acute Cardiac Events (GRACE))
Offer coronary angiography (with follow on PCI if indicated) within 96 hours of first admission to hospital to patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%) if they have no contraindications to angiography (such as active bleeding or comorbidity). Perform angiography as soon as possible for patients who are clinically unstable or at high ischaemic risk
Consider intravenous eptifibatide or tirofiban as part of the early management for patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%), and who are scheduled to undergo angiography within 96 hours of hospital admission.
Consider abciximab, usually in the catheter laboratory, as an adjunct to PCI for patients at intermediate or higher risk of adverse cardiovascular events who are not already receiving a glycoprotein IIb/IIIa inhibitor.
Unstable angina or NSTEMI
Predicted six month mortality
Risk of future adverse cardiovascular events1.5% or below
Lowest
>1.5 to 3.0%
Low
>3.0 to 6.0%
Intermediate
>6.0 to 9.0%
High
over 9.0%
Highest
Aspirin should be offered to all patients with unstable angina or NSTEMI unless contraindicated (such as by active bleeding,
current peptic ulceration,
or for those considered clinically to be at a high potential risk of the consequences of bleeding, for example, recent neurosurgery or
haemorrhagic stroke).
It is recommended that treatment with clopidogrel in combination with low dose aspirin should be continued for 12 months after the most recent acute episode of non-ST segment elevation ACS. Thereafter, standard care, including long term treatment with low dose aspirin alone, is recommended.
Learning bite
Consider discontinuing clopidogrel treatment five days before CABG in patients who have a low risk of adverse cardiovascular events. For patients at intermediate or higher risk of adverse cardiovascular events, discuss the continuation of clopidogrel before CABG with the cardiac surgeon and base the decision on the balance of ischaemic and bleeding risk.What are varicose veins?
Varicose veins are enlarged tortuous veins associated with reflux of blood due to incompetent valves. They are conventionally defined as being more than 4 mm in diameter.Reticular veins are defined as dilated non-palpable subdermal veins smaller than 4 mm in diameter .
Telangiectasies (usually called thread veins or spider veins): these are dilated intradermal venules less than 1 mm in diameter which may be isolated or occur in patches or blushes.
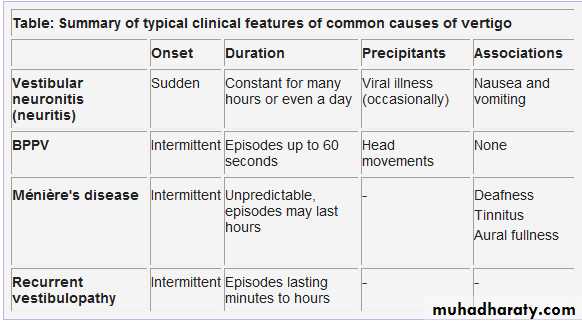
There are three main vestibular reflexes:
• Vestibulo-ocular reflex (VOR) - stabilises eyes• Vestibulospinal reflexes (VSR) - stabilise body and head
• Vestibulo-vegetative reflexes (autonomic reflexes) - clinically important but poorly understood.
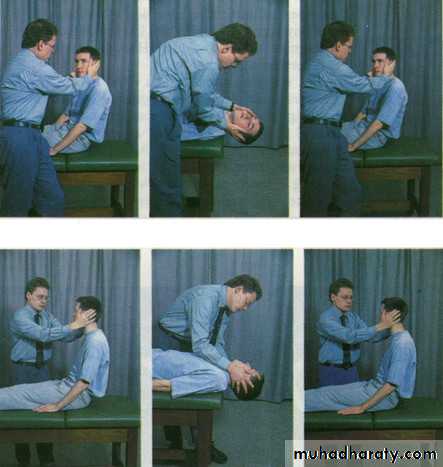
Learning bite: Dix-Hallpike manoeuvre
This manoeuvre is used as a diagnostic test, used particularly when you suspect benign paroxysmal positional vertigoYou should explain the procedure to the patient, and warn them that they may experience vertigo symptoms during it, but that the symptoms usually subside quickly. You should ask them to keep their eyes open throughout and stare at your face. Check that the patient does not have any neck injuries or other contraindications to rapid spinal movements
Ask the patient to sit on an examination couch with their legs extended, close enough to the edge so that their head will hang over when they are laid flat
Figure 1. Dix-Hallpike manoeuvre (with permission BMJ publishing Lempert et al 1995)
Stand on their left side, take hold of their head with both your hands, and turn their head 45° towards you. (This tests the left posterior canal). Observe their eyes for 30 seconds. (Signs and symptoms usually occur when you turn the patient's head towards the lesion - if you suspect disease of the right ear, you may wish to start on their right side.) I personally would start with the non-affected sideKeeping the patient's head in the same position, lie them down quickly until their head is hanging over the edge of the couch (still turned 45° towards you) Observe their eyes for 30 seconds
Lift the patient back up to sitting position, and repeat the test on their right side
In a patient with BPPV, you will typically see a characteristic pattern of nystagmus emerge after 5-20 seconds, when the patient's head is hanging towards the side of the lesion. This is called torsional or rotatory nystagmus and has two components: a quick movement towards the side of the lesion and a slow component away from it.
An upward beating nystagmus is often superimposed on this movement.
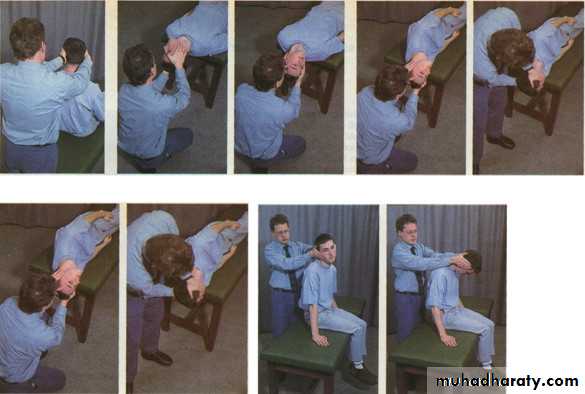
Learning bite - the Epley manoeuvre: a canalith repositioning procedure
A recent systematic review concluded that canalith repositioning procedures like the Epley manoeuvre are generally safe and effective for patients with BPPV.23It is thought to work by rotating the posterior canal backwards, and so directing particulate material out of the canal into the utricle.
You should perform each manoeuvre and hold it until any positional nystagmus has disappeared: this indicates that the movement of endolymph has stopped. You may need to repeat the whole procedure three or four times, until nystagmus no longer appears.
You should explain the procedure to the patient, and warn them that they may experience vertigo symptoms during it, but that the symptoms usually subside quickly. You should ask them to keep their eyes open throughout. Check that the patient does not have any neck injuries or other contraindications to rapid spinal movements - you need to execute movements during the procedure rapidly (in less than one second)
Ask the patient to sit on an examination couch with their legs extended, close enough to the edge so that their head will hang over the edge when they lie down.
Stand behind the patient and hold their head in both of your hands
Figure 3: Epley Procedure (with permission BMJ publishing Lempert et al 1995)
Turn the patient's head 45° towards the affected ear, keeping their head in that position, lean the patient back rapidly until their head is over the edge of the couch. Hold until nystagmus dissipatesRotate the patient's head through 90°, so that it is facing 45° away from the affected ear, then (keeping their head steady, still hanging back over the couch edge) ask the patient to roll their body to straighten their neck. Hold .Ask the patient to keep their body still, while you turn their head 45° to face the floor. Hold.While keeping the patient's head turned to the side, help them to sit up.
With the patient sitting up, move their head into the centre line, as you move it forward 45° (chin on chest).