Nausea and Vomiting in Pregnancy
د. حسين محمد جمعهاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2012
About 50% of women have nausea and vomiting in early pregnancy, and an additional 25% have nausea alone. The popular term“morning sickness” is a misnomer, as it often persists throughout the day. In about 35% of those who have this condition, nausea and vomiting are clinically significant.
When do nausea and vomiting in pregnancy most typically resolve?
The onset of the nausea is within four weeks of the last menstrual period in most patients.The problem typically peaks at approximately 9 weeks of gestation.
Sixty percent of cases resolve by the end of the first trimester, and
91% by 20 weeks gestation.
Preventable rare maternal complications of hyperemesis gravidarum include peripheral neuropathies due to vitamin B6 and B12 deficiencies and, most serious, Wernicke’s encephalopathy due to thiamine (vitamin B1) deficiency. Characterized by the triad of ophthalmoplegia,gait ataxia, and confusion, this condition may occur after at least 3 weeks of persistent vomiting.
If patients are treated with intravenous dextrose without thiamine, metabolism
of the dextrose rapidly consumes the available B1, triggering acute encephalopathy. In one case series involving 19 patients in whom this complication developed, 74% had neurologic abnormalities on follow-up.Incidence of hyperemesis gravidarum is 0.3 to 1.0%; this condition is characterized by persistent vomiting, weight loss of more than 5%,ketonuria, electrolyte abnormalities (hypokalemia), and dehydration (high urine specific gravity). Although the cause of nausea and vomiting in pregnancy is unclear, the observation that pregnancies with a complete hydatidiform mole (no fetus) are associated
with clinically significant nausea and vomiting indicates that the stimulus is produced by the placenta, not the fetus.
The clinical course of nausea and vomiting during pregnancy correlates closely with the level of human chorionic gonadotropin (hCG) . It is theorized that hCG may stimulate estrogen production from the ovary; estrogen is known to increase nausea and vomiting. Women with twins or hydatidiform moles, who have higher hCG levels than do other pregnant women, are at higher risk for these symptoms.
Another theory is that vitamin B deficiency may contribute, since the use of multivitamins containing vitamin B reduces the incidence of nausea and vomiting. Although it has been suggested that nausea and vomiting may be caused by psychological factors, there are no good data to support this.
Evaluation
Hyperemesis gravidarum must be distinguished from other conditions that may cause persistent vomiting in pregnancy, including gastrointestinal conditions (e.g., appendicitis, hepatitis, pancreatitis, or biliary tract disease), pyelonephritis,and metabolic disorders such as diabetic ketoacidosis, porphyria, or Addison’s disease.An onset of nausea and vomiting more than 8 weeks after the last menstrual period is rare in pregnancy.
The presence of fever, abdominal pain, or headache is atypical in women with hyperemesis and suggests another cause.
Laboratory testing should generally include measurement of levels of urinary ketones, blood urea nitrogen, creatinine, alanine aminotransferase, aspartate aminotransferase,electrolytes, amylase, and thyrotropin (as well as free thyroxine [T4] if thyrotropin is suppressed).
Because hCG cross-reacts with thyrotropin and stimulates the thyroid gland, thyrotropin is typically suppressed in these patients. This apparent hyperthyroidism usually resolves spontaneously.
Management
Women should be advised to avoid exposure to odors, foods, or supplements that appear to trigger nausea; common triggers include fatty or spicy foods and iron tablets. Clinical experience suggests that eating small amounts of food several times a day and drinking fluids between meals may be helpful, as may bland, dry, and high-protein foods.
Traditionally, patients have been advised to manage nausea by keeping crackers at the bedside in the morning and avoiding an empty stomach. Data from randomized trials are lacking to compare different types of diets
for the management of nausea and vomiting in pregnancy. In one crossover study involving 14 pregnant women with nausea, protein-predominant meals reduced nausea more than meals containing equal amounts of calories from carbohydrates and fat or noncaloric meals.
Women who have persistent nausea and vomiting and high concentrations of ketones require intravenous hydration with multivitamins, including thiamine, with follow-up measurement of levels of urinary ketones and electrolytes.
Antiemetic agents should be prescribed in these
Patients.
Pharmacologic Therapies
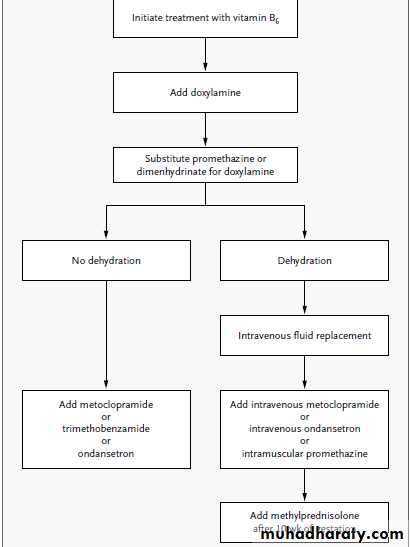
Approximately 10% of women with nausea andvomiting in pregnancy require medication. Pharmacologic therapies include vitamin B6, antihistamines,prokinetic agents, and other medications.Randomized, placebo-controlled trials have shown the effectiveness of vitamin B6 (10 to 25 mg every 8 hours) in the treatment of nausea and vomiting in pregnancy.
Oral vitamin B6 and antihistamine doxylamine are available over the counter in the United States. The combination has been well studied in over 6000 patients and controls, with no evidence of teratogenicity, and, in randomized trials, a 70% reduction in nausea and vomiting. It is recommended by the American College of Obstetricians and Gynecologists as first-line therapy for nausea and vomiting in pregnancy.
Phenothiazine or metoclopramide is usually prescribed if antihistamines fail. Prochlorperazine is also available as a buccal tablet ,which is usually associated with less drowsiness and sedation than oral tablets.Metoclopramide is a prokinetic agent,a dopamine antagonist. It has been associated in rare cases with tardive dyskinesia. The risk of the development of this complication increases with the duration of treatment and the total cumulative dose; treatment for more than 12 weeks should be avoided.
In a recent randomized trial, intravenous metoclopramide and intravenous promethazine had similar efficacy in the treatment of hyperemesis, but metoclopramide caused
less drowsiness and dizziness.
The 5-hydroxytryptamine3-receptor antagonists,such as ondansetron (Zofran), are increasingly used for hyperemesis in pregnancy, but information is limited to inform their use in pregnant women. A randomized trial comparing ondansetron and promethazine in pregnancy showed similar efficacy, but ondansetron was less sedating.
Methylprednisolone is an option in refractory
cases. In a randomized trial involving 40 women,methylprednisolone was superior to promethazine
for treating nausea and vomiting in pregnancy. a meta-analysis of four studies, use of glucocorticoids
before 10 weeks of gestation was associated
with a risk of cleft lip with or without cleft
palate that was increased by a factor of 3 to 4;
higher doses were associated with greater risks.
Thus, it is recommended that glucocorticoids be
used only after 10 weeks of gestation.
Randomized, double-blind trials have provided support for a benefit of ginger in the management of nausea and vomiting in pregnancy.
Management of Refractory Cases
Patients with nausea and vomiting that are not controlled with outpatient regimens require intravenous hydration and nutritional supplementation.Enteral tube feeding may be effective, although some patients continue to have persistent emesis.
Total parenteral nutrition is associated with a substantial risk of line sepsis (25%), steatohepatitis may also occur with the use of lipid emulsion during pregnancy. Given these risks, total parenteral nutrition should be reserved for patients with clinically significant weight loss (>5% of body weight) who have had no response to antiemetic regimens and whose condition cannot be managed with enteral feedings.
Conclusions and Recommendations
It is also important to consider other causes of nausea and vomiting in early pregnancy such as migraine headaches or gastrointestinal disorders. Levels of blood urea nitrogen, creatinine, alanine aminotransferase, aspartate aminotransferase, electrolytes, and amylase should be assessed. Dietary advice (e.g., frequent small meals) may be helpful.Given data from randomized trials suggesting that vitamin B6 and doxylamine are beneficial, I would recommend this combination (vitamin B6 [pyridoxine], 10 to 25 mg every 8 hours, and doxylamine, 25 mg at bedtime and 12.5 mg each in the morning and afternoon). If this regimen is not effective, a phenothiazine,metoclopramide, or ondansetron can be tried in succession. Methylprednisolone should be reserved for refractory cases after 10 weeks of gestation.
Alternative remedies such as ginger and acupuncture may be tried at any time.
Pregnant women with dehydration should receive intravenous fluid replacement with multivitamins,especially thiamine. If, after 12 hours of intravenous therapy, the vomiting continues, hospitalization may be required. Enteral or parenteral nutrition should be reserved for patients in whom weight loss continues despite pharmacologic therapies.NEJM 2010