Pregnancy in congenital andvalvular heart disease
Heart 2011د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
Pregnancy has always been a major concern in
patients with heart disease. Although manywomen with pre-existing heart disorders tolerate
pregnancy well, complications are frequent and in
some cases include life threatening conditions for
mother and child. In western countries maternal
heart disease has indeed become the major cause of maternal death during pregnancy.
Furthermore, pregnancy can have a negative impact on the long term course of heart disease. Thus, screening for heart disease, appropriate risk assessment, and counselling are crucial.
In women at risk who nevertheless desire pregnancy or who present already pregnant, adequate measures during pregnancy and delivery that may reduce complications and optimise outcome have to be taken.
The spectrum of heart disease in pregnancy has
changed and differs among regions around theworld. In the western world, the risk of cardiovascular
disease in pregnancy has increased because of
advanced age at first pregnancy and the increasing
prevalence of cardiovascular risk factors such as
diabetes, hypertension, and obesity.
More importantly, the improvement of congenital heart disease treatment has resulted in a significant number of women with heart disease now reaching childbearing age, and these represent the majority of
pregnant women with heart disease. In a prospective
multicentre study comprising 562 consecutive
women and 599 pregnancies, Siu et al reported
congenital heart disease in 74%.
Acquired valvular heart disease was present in 22% of cases, and arrhythmias without structural heart disease in 4%. Coronary artery disease and cardiomyopathies (except for hypertrophic cardiomyopathy) were each reported in <1% of the women. In the nonwestern countries that still struggle with rheumatic fever, acquired valvular heart disease predominates by far.
This article focuses on congenital and valvular heart disease as the two most common pre-existing cardiac disorders in pregnant women.
The European Society of Cardiology (ESC) has
recently published guidelines on the management
of cardiovascular disease during pregnancy. This
document summarises the current knowledge of
pregnancy and heart disease in great detail,
providing comprehensive general considerations
as well as specific sections for each disease with the
scientific background and management recommendations.
The current ESC guidelines for the management of grown-up congenital heart disease also address this issue. We refer to these publications as well as to a newly established website on heart disease and pregnancy (http://www.heartdiseaseandpregnancy.com) for detailed information and guidance to additional literature.
The purpose of the present paper is to summarise
the principles and provide a practical approach to
risk assessment and management of pregnancy in
congenital and valvular heart disease.
PHYSIOLOGIC CHANGES DURING PREGNANCY
AND THEIR IMPACT ON PRE-EXISTING HEARTDISEASE AND ITS TREATMENT
Knowledge of the physiologic changes during
pregnancy and their potential impact on heart
disease helps us to understand the risk of complications and provides the background for risk
assessment in clinical practice.
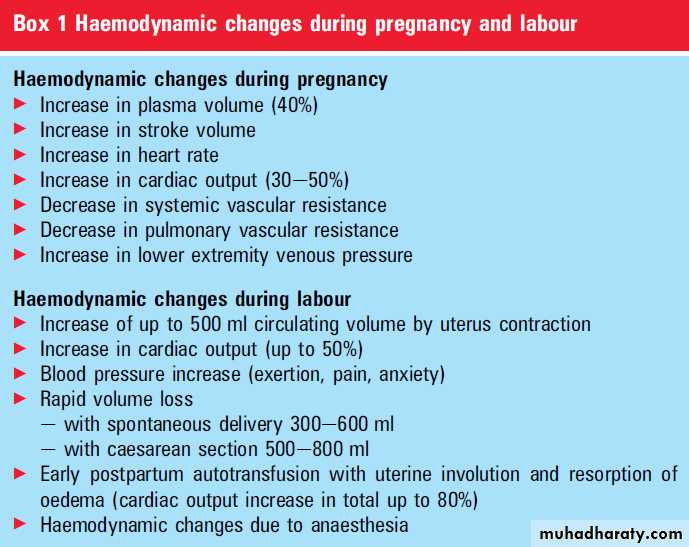
Haemodynamic changes
In order to meet the increased metabolic demandsof the mother and the fetus, pregnancy induces
major changes in the cardiovascular system
including pronounced increases in blood volume
and cardiac output and a reduction in vascular
resistance.
Around the 24th week of gestation, the
increase in plasma volume reaches its maximum of approximately 40% above baseline.
Cardiac output increases during pregnancy to eventually 30-50%.
This increase is primarily generated by a rise in
stroke volume during early pregnancy, while heart
rate becomes the major factor in late pregnancy.
Systemic blood pressure in general falls in early
pregnancy due to vasodilation and may normalise
to pre-pregnancy values in the late phase (box 1).
The increase in cardiac output aggravates the
haemodynamic burden in all obstructive lesionssuch as valvular stenosis, subvalvular, supravalvular,
and major vessel stenoses as well as pulmonary vascular disease.
On the other hand, dynamic obstruction such as in hypertrophic obstructive cardiomyopathy may even decrease due to the rise in preload.
The increase in heart rate with shortening of diastole aggravates the haemodynamic burden of atrioventricular valve stenoses.
In general, aggravation of any moderate to severe
flow obstruction is poorly tolerated.
Aortic regurgitation may benefit from pregnancy
related vasodilation and is in general well tolerated as long as left ventricular function is preserved.
Increasing volume overload may be less well tolerated
in other regurgitant lesions, but this may primarily be related to associated ventricular dysfunction.As a rule, any pre-existing burden of pressure or
volume overload as well as other pre-existing
myocardial disease may make the ventricles unable
to adapt to the requirements of producing a higher
cardiac output and may result in heart failure
during pregnancy.
The pre-existing damage of myocardium will be crucial in this regard and significant ventricular dysfunction already present before pregnancy is always associated with a high risk.
Labour and the postpartum period are also
affected by major haemodynamic changes (box 1).
Uterine contractions, positioning (left lateral versus
supine), pain, anxiety, exertion, bleeding, anaesthesia,
and infection may all contribute.
Significant rises in blood pressure and cardiac output need to be considered. Postpartum, autotransfusion associated with uterine involution and resorption of leg oedema cause a pronounced increase in cardiac
preload and cardiac output. It takes several weeks
for the volume state to resolve from pregnancy
induced changes.
The increased oxygen needs of the mother and
child have to be satisfied. The activated erythropoiesis results in a 20-30% increase in the red blood cell mass.Patients with a pre-existing tendency to
iron deficiency may not be able to adapt to these
changes, especially in cyanotic disorders or because
of constant minimal blood loss under anticoagulation.
Adequate iron supply is crucial in these cases.
Haemostatic changes
Pregnancy is associated with several haemostaticchanges including a rise in coagulation factors,
fibrinogen and platelet adhesiveness, but also
a decrease in fibrinolysis.
This causes a hypercoagulable state and increases the risk of thromboembolism.
The obstruction of venous return by the enlarged
uterus further increases the risk of venous thrombosis.
Any pre-existing haemostatic disorders associated
with the heart defect and diseases highly
sensitive to embolic events are at particular risk.
These include patients with a Fontan circulation,
right-to-left shunt, pulmonary hypertension, and
prosthetic valves.
Structural changes at the vascular tissue level
In women with bicuspid aortic valve associatedaortopathy or connective tissue related diseases
such as Marfan, EhlerseDanlos or Turner
syndrome, in addition to haemodynamic changes,
the hormonal changes occurring during pregnancy
may lead to histological changes in the aorta.
These result in a higher susceptibility to dissection
occurring most frequently in the last third of
pregnancy or the early postpartum period.
Changes in pulmonary vascular disease during
pregnancy are still insufficiently understood, butalterations at the tissue level are likely. Mechanisms
for pulmonary hypertensive crises occurring typically
in the last months of pregnancy and in the first
month after delivery are probably multifactorial.
Pulmonary thrombosis may play a role.
Changes in drug effects During pregnancy, drug effects may be altered significantly by various physiologic changes.
Drug absorption, excretion, and bioavailability can all be affected.
The increase in intravascular as well as extravascular fluid volume affects drug distribution and may require higher drug dosages.
The increase in renal perfusion and higher hepatic metabolism may cause increased drug clearance and again require dosage adaptation. Since the physiologic changes vary during pregnancy, continuous dose adjustment may be necessary. In addition to these considerations, drug use during pregnancy and breastfeeding is limited by the potential side effects for the fetus. Risk and benefit must be carefully weighed (see recommendations for drug use in pregnancy in the current ESC guidelines).
RISK OF PREGNANCY IN PATIENTS WITH
CONGENITAL AND VALVULAR HEART DISEASEPre-existing heart disease may pose a risk to both
mother and child. In addition, the genetic risk has
to be considered and included in patient counselling.
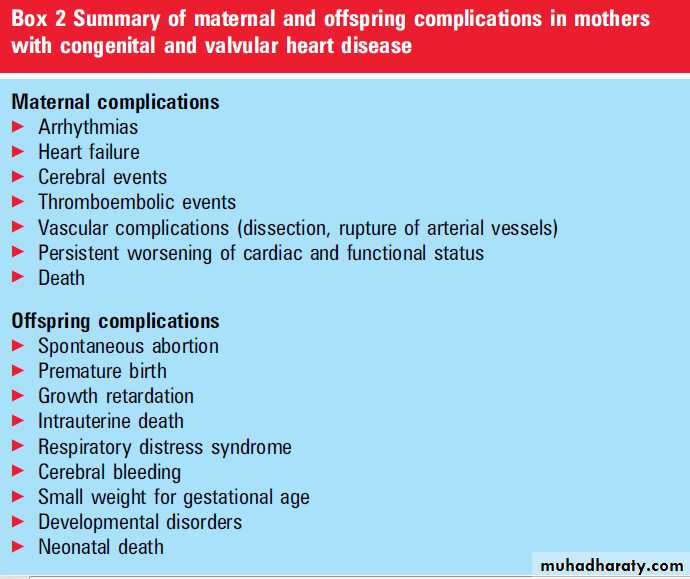
Box 2 summarises the most important
maternal and offspring complications associated
with heart disease in the mother.
In a contemporary cohort of pregnant women,
Siu et al8 compared 302 pregnancies in patientswith heart disease with 572 women without heart
disease. Fetal and cardiac maternal complications
were observed in 18% and 17% of patients with
heart disease compared with 7% and 0% in those
women without, respectively.
While such data demonstrate the overall increased risk, they are not helpful in clinical practice as risk of pregnancy varies widely from very low at one end of the scale to up to 50% maternal mortality at the other
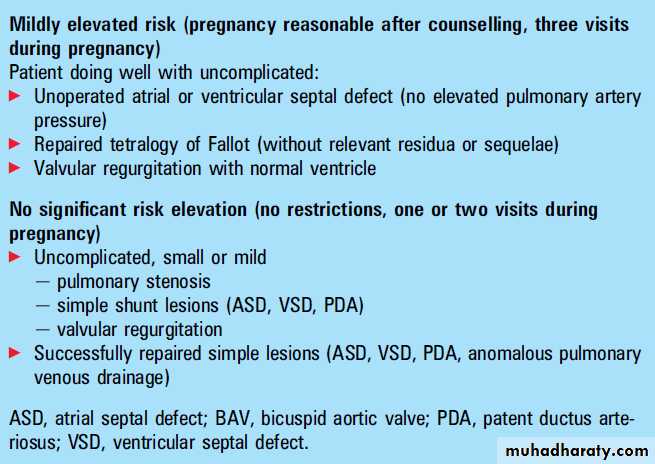
end, depending on the mothers specific condition (box 3).
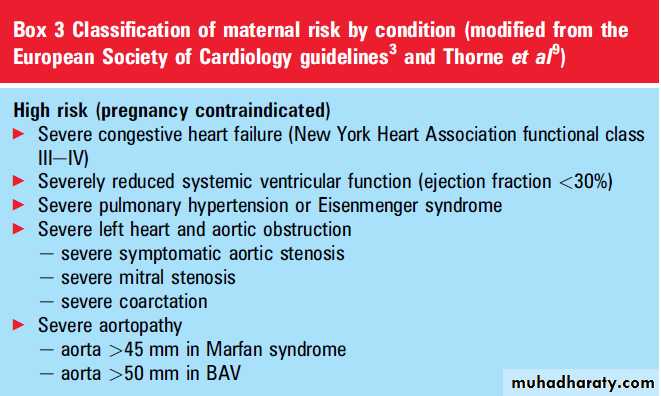
Maternal high risk conditions
Several conditions have been identified that are associated with such high rates of maternal mortality and morbidity that pregnancy must be considered to be contraindicated. Patients must be strongly counselled against pregnancy and, if they present already pregnant, termination should be discussed. These conditions are listed below and in box 3.Poor functional status and systemic ventricular
dysfunctionAny patient presenting with severe congestive
heart failure (NYHA) functional class III-IV) and/or severely reduced systemic ventricular function (ejection fraction <30%), irrespective of the underlying disease, must be considered at high risk and pregnancy must be avoided.
Pulmonary hypertension and Eisenmenger syndrome
A very high maternal mortality rate (30-50% inolder studies and 17-33% in more recent studies)
has been reported for patients with pulmonary
hypertension, occurring mostly late in pregnancy or in the postpartum period.
This high risk must be expected not only in the congenital heart disease group with pulmonary arterial hypertension, but also in those patients with pulmonary hypertension related to left heart valvular disease.
Although most data demonstrating such high
mortality rates refer to severe pulmonary hypertension, and many experts assume patients with pulmonary artery pressure <50% of systemic are at less risk, it has to be emphasised that even
moderate pulmonary vascular disease may worsen
during pregnancy and that there are no data available demonstrating a safe cut-off value.
Patients with Eisenmenger syndrome are in the highest risk group and need special consideration because they present with cyanosis due to right-to-left shunt, which may increase with systemic vasodilation during pregnancy.
Cyanosis poses a particular risk to the fetus.
Live birth is unlikely with maternal
oxygen saturation <85%.
Severe left heart and aortic obstruction
Patients with severe mitral and aortic stenosis(at any level) as well as severe coarctation tolerate
pregnancy poorly and should be treated before or
counselled against pregnancy (see haemodynamic
changes). Symptoms before pregnancy indicate
that patients are at particularly high risk. Asymptomatic patients with a normal exercise test may tolerate pregnancy, but recommendations are
controversial.
Severe aortopathy
The risk for aortic dissection is increased duringpregnancy in patients with aortopathies.
Patients with significant dilatation of the aorta
(>45 mm in Marfan syndrome and >50 mm in bicuspid aortic valve) are at particular risk and should be counselled against pregnancy (box 3).
RISK STRATIFICATION AND COUNSELLING
Risk assessment and counselling should beperformed before women with heart disease
become pregnant. Medical treatment should be
reviewed for appropriateness during pregnancy
(drug safety) and plans for regular follow-up visits
and the mode of delivery should be made.
The ESC guidelines recommend that maternal
risk should be assessed according to a modified
World Health Organization risk classification.
Box 3 summarises the classification which has been
slightly modified for easier use in daily practice. High risk patients in whom pregnancy must be
avoided and those with very low risk requiring no
restrictions are well defined.
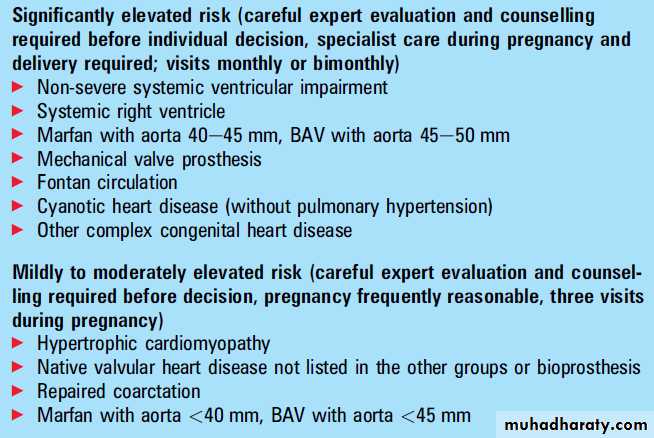
The group in between - patients with more or less elevated risk but no contraindications for pregnancy-remains challenging, however.
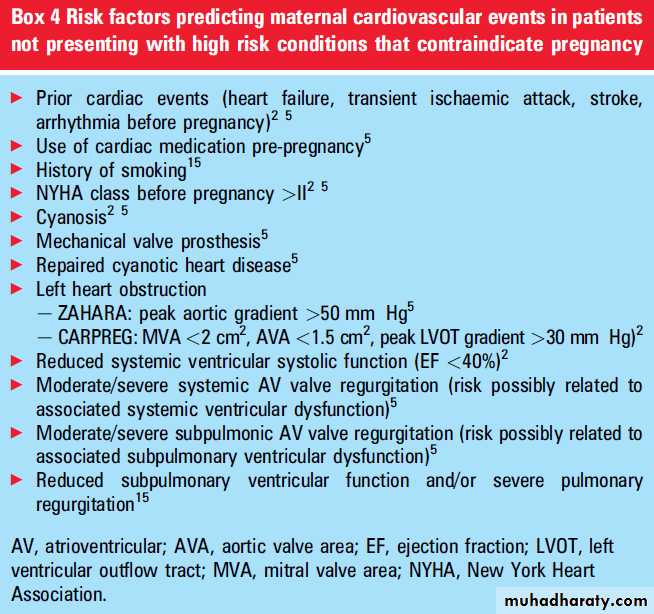
Several studies have tried to identify risk factors that may allow refining risk assessment, particularly in this patient group.
Risk scores
Siu et al, in a study of 599 pregnancies (562women; 74% with congenital heart disease, 22%
with acquired valvular heart disease) identified
prior cardiac events or arrhythmia*, poor functional class or cyanosis*, left heart obstruction* and impaired systolic left ventricular function* as independent predictors of maternal cardiac complications.
Cardiac events were observed in 13% of pregnancies including pulmonary oedema, arrhythmia, stroke, and three cardiac deaths. The
risk for adverse events increased exponentially with
the number of risk factors (5% without a risk
factor, 27% with one, 75% with two or more of the
risk factors listed above*).
This CARPREG risk
score is the most popular one and has been validated
in several studies. In a smaller study of 90
pregnancies, Khairy et al reported impaired
subpulmonary ventricular function and/or severe
pulmonary regurgitation and smoking history to be
independent predictors of maternal cardiac
complications.
The recently published ZAHARA
study, comprising 1302 completed pregnancies inwomen with congenital heart disease, confirmed
history of arrhythmia, poor functional class
(NYHA >II), and left heart obstruction as predictors
of adverse events, and identified use of cardiac
medication pre-pregnancy, mechanical valve prosthesis, repaired or unrepaired cyanotic heart disease, and moderate/severe atrioventricular valve regurgitation (systemic as well as subpulmonary) as
additional risk factors.
The use of cardiac medication pre-pregnancy implies the known risk factor of prior cardiac events. Although not included in former risk scores, mechanical protheses with their high risk of thromboembolic complications during pregnancy as well as complex congenital heart disease are well known risk factors.
Atrioventricular (AV) valve regurgitation, however, has so far not been considered a lesion with significant risk. It has to be emphasised that the ZAHARA study was unable to report details on ventricular function.
Thus, it could be that the increased risk associated
with AV valve regurgitation in this study is related
to associated ventricular dysfunction.
The risk score developed in this study was reported to be superior to the CAPREG score, but has so far not been validated prospectively in other studies.
In general, the proposed risk scores have major
limitations when used in clinical practice.
The results of these studies are significantly affected by patient selection.
Well known risk factors such as pulmonary hypertension and dilated aorta were not identified because of under representation of these patients in the studied population. Impaired ventricular function could not be identified as a risk factor since valid data on ventricular function were not available in the ZAHARA study.
Furthermore, adverse cardiac events that could be easily managed are not separated from more serious events, potentially life threatening complications, persistent worsening of cardiac condition, and death as the most important information for counselling.
For this reason it is recommended to rule out high
risk conditions as the first step (box 3).
For the intermediate risk group, however, consideration of the reported risk factors may be helpful. They are
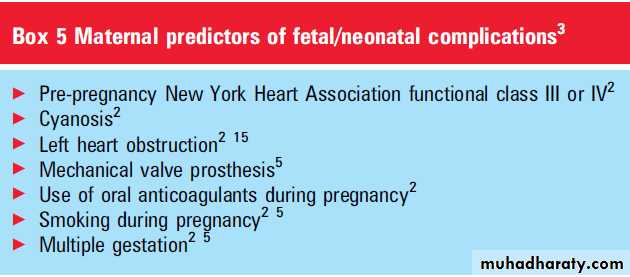
summarised in box 4. Predictors of fetal risk are
summarised in box 5.
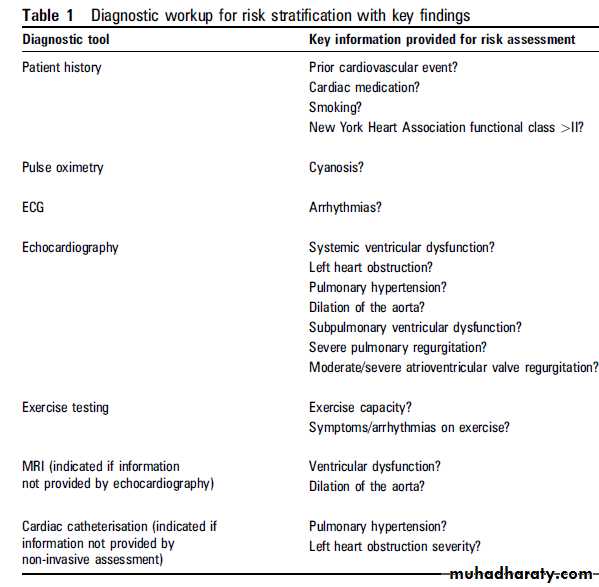
Practical approach to risk assessment (see also table 1)
Patient history
Risk assessment should always start with careful
evaluation of the patients history and available
medical reports that may already provide details
of the patients specific condition (box 3) and identify risk factors such as prior cardiac events,cardiac medication, smoking, and NYHA functional class >II.
Pulse oximetry
Pulse oximetry can exclude or document oxygen
desaturation (cyanosis).
ECG
An ECG documents, among other findings,
arrhythmias.
Echocardiography
Echocardiography enables a diagnosis to be madeor provides confirmation of the specific condition,
including severity assessment, in most patients.
Particular attention should be directed at identifying
and quantifying systemic and subpulmonary
ventricular dysfunction, left heart obstruction,
pulmonary hypertension, and dilation of the
aorta as well as AV valve and pulmonary valve
regurgitation.
Exercise testing
Assessment of exercise capacity before pregnancy isparticularly helpful. Good exercise capacity
without occurrence of symptoms is a predictor of
a low complication rate during pregnancy.
Cardiac MRI
Cardiac MRI may be required if there is uncertainty
following echocardiography about ventricular
function and dilation of the aorta.
Cardiac catheterisation
Cardiac catheterisation is indicated if pulmonary
hypertension requires further evaluation or important
questions cannot be sufficiently answered by
non-invasive techniques, in particular quantification
of obstructive lesions.
Pre-pregnancy risk reduction
Interventions that may lower the risk of pregnancyin patients with heart disease must be carefully
considered. In general, in conditions for which
catheter intervention or surgery is indicated, based
on current guidelines these procedures should definitely
be performed before pregnancy.
For defects that are likely to pose a significant risk to the mother and child, the threshold to intervene may
be lower, although this remains controversial.
Prophylactic intervention must be particularly
considered in patients with left heart obstruction
and dilated aorta.
There is agreement that Marfan patients with an aorta >45 mm should undergo surgery before pregnancy, and patients with a bicuspid valve and an aorta >50 mm should be considered for surgery.
Recent observation of dilation progression strengthens the indication in borderline situations.
American guidelines
recommend intervention for asymptomatic leftheart obstruction with a lower grade of severity
when patients desire pregnancy.
However, there are currently no data to support such recommendations and they were not followed in the European document.
The decision is particularly difficult in valve stenosis when balloon valvulotomy is not an option. In this case, the implantation of a mechanical valve results again in significant risk for pregnancy, and bioprosthetic valves imply the requirement of later reoperation.
General measures
Iron and vitamin supplementation during pregnancyis important. Avoidance of exertion may be
required and indicate early maternal leave. Appropriate measures to prevent venous thromboembolism must be considered and range from physical measures via low dose low molecular weight
heparin (LMWH) to therapeutic anticoagulation,
depending on the individual risk associated with
the specific condition and additional factors.
Intervention during pregnancy
Catheter intervention during pregnancy is reservedfor patients who develop serious problems and are at very high risk. Typically balloon valvulotomy
may be an option in patients with severe aortic
or mitral stenosis who develop heart failure during
pregnancy.
Because of the radiation exposure,the best time for intervention is after the fourth month.
The threshold for cardiac surgery is even higher. It is only recommended when medical treatment or catheter intervention fail and the mothers life is threatened. The best period is between the 13th and 28th weeks of gestation, because earlier surgery carries a high risk of fetal loss or malformation and later surgery has a higher risk of preterm delivery and maternal complications.
Medical treatment
The side effects of medical treatment on the fetusmust be carefully considered. When pharmacological
treatment of heart failure is necessary,b-blockers (metoprolol, bisoprolol), diuretics (furosemide, thiazide) and digoxin can be used. ACE inhibitors and angiotensin receptor blockers are contraindicated because they carry the risk of fetal renal agenesis.
Antihypertensive therapy may consist of
a-methyldopa, hydralazine, or b-blocker.Diuretics may reduce placental perfusion and must
be avoided in the presence of impaired uteroplacental
perfusion such as occurs in pre-eclampsia
with fetal growth retardation.
Several antiarrhythmic drugs can be administered safely.
Verapamil, digoxin, and b-blockers are useful for
rate control in atrial fibrillation or flutter, supraventricular tachycardias can be terminated byadenosine, and electrical cardioversion is feasible
during pregnancy.
Sodium channel blockers such as flecainide are allowed for rhythm control in atrial fibrillation or otherwise not sufficiently controlled ventricular arrhythmias.
Amiodarone is generally not recommended; however, some conditions may require the administration of this potent drug, in which case the lowest effective dose should be given.
Anticoagulation in patients with mechanical valves remains a dilemma.
Oral anticoagulation (OAC) throughout pregnancy is the safest regimen for the mother because unfractionated heparin (UFH) and LMWH carry a higher risk of
thromboembolic events.
However, oral anticoagulation is associated with the risk of embryopathy (dose dependent) and fetal complications including miscarriage, bleeding complications, and fetal death.
The new ESC guidelines recommend that the continuation of OAC throughout pregnancy should be considered when the warfarin dose is <5 mg daily (or phenprocoumon <3 mg), with a switch to heparin before delivery.
When a higher dose is required, discontinuation of OAC between weeks 6 and 12 and replacement by adjusted dose UFH (a PTT≥2X - control; in high risk patients applied as intravenous infusion) or LMWH twice daily (with dose adjustment according to weight and target anti-Xa level 4e6 h post-dose
0.8-1.2 U/ ml) should be considered.
Delivery
High risk delivery requires specialised units. Spontaneous labour may be preferable, but this presents logistic problems in these patients as the presence of a specialised team is required which cannot be provided round the clock in most institutions.Vaginal delivery is preferred in most conditions.
Caesarian delivery may be considered for pretermlabour in patients on OAC, such as those with
prosthetic valves, to allow a safe switch to heparin.
Caesarean section is preferred in patients with aortopathy, severe aortic stenosis, heart failure, or
severe pulmonary hypertension.
Monitoring of blood pressure, pulse oximetry,
and ECG should be used as required, but SwaneGanz catheters should be avoided. Volume changes after delivery can cause complications and may require prolonged monitoring.
Patients with aortopathy or pulmonary hypertension remain at high risk after delivery and also require prolonged observation.
CONCLUSIONS
In patients with congenital and valvular heartdisease, careful risk assessment and counselling are
crucial and should be performed before patients
become pregnant. Patient history, ECG, pulse
oximetry, and echocardiography allow appropriate
risk assessment in most patients, and few require
additional evaluation by MRI/CT or catheterisation.
Where indicated, catheter intervention or
surgical treatment should be performed beforepregnancy. Severe heart failure, severely reduced
systemic ventricular function, severe pulmonary
hypertension, severe left heart obstruction, and
aortopathy are associated with particularly high
risk and require strict counselling against pregnancy.
Other patients must be assigned to groups without relevant risk elevation, patients with mildly elevated risk, mild to moderately elevated, and those with significant risk (but no contraindication) based on their specific condition and additional established risk factors. In particular, the latter two groups require expert evaluation and counselling for decision making. Management of risk pregnancy requires an experienced team comprising the cardiologist, obstetrician, and
anaesthetist in a specialised centre.