Pregnancy in high risk cardiacconditions
Heart 2009د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
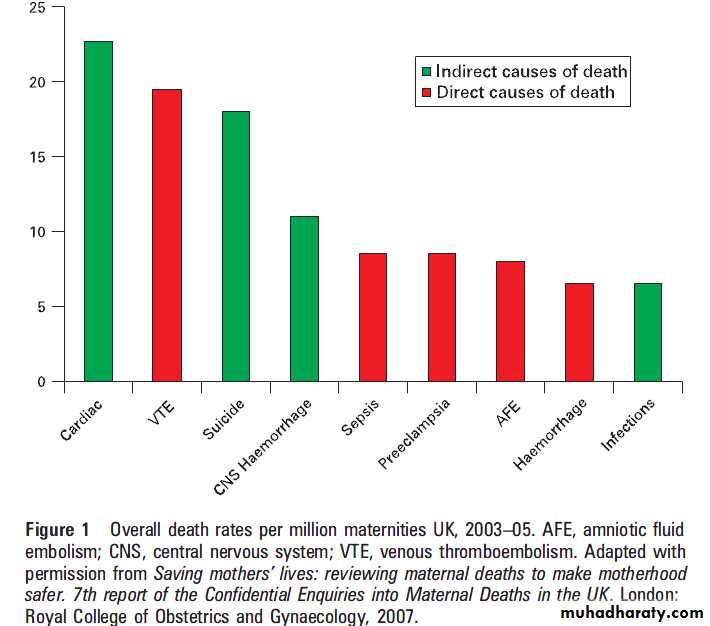
Heart disease is present in 0.5–1% of all pregnant
women and is the biggest killer of pregnant womenin the developed world .Surprisingly, there
have been no signs of decline in this incidence over
the past two decades .In the UK, all
maternal deaths (during pregnancy and within
the first post partum year) are recorded and
examined in detail every 3 years.
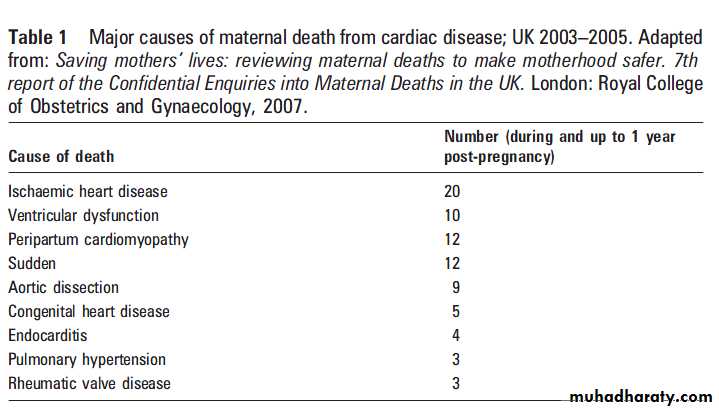
Of the maternal cardiac deaths reported for the 2003–5 triennium, more than half were due to coronary artery disease, puerperal cardiomyopathy and aortic dissection (table 1).
As in previous triennial reports, substandard
care continues to be an important factor,
and contributed to the woman’s death in more
than a third of cases.
These conditions often present acutely and
catastrophically in women with no known preexistingdisease. Rapid recognition of the acute
presentation and appropriate management will
improve their chances of survival.
In addition, identifying risk factors for these conditions should flag up at risk patients for targeted ante- and postnatal care.
Modifiable risk factors such as obesity and smoking appear particularly important for this
group of women and are a growing public healthproblem. In addition, social deprivation and
immigrant status are significant risk factors for
maternal deaths of all causes, including heart
disease, underscoring the need to improve access
to health care for these vulnerable groups.
ACUTE CORONARY SYNDROMES AND ISCHAEMIC
HEART DISEASE
Death from ischaemic heart disease
Maternal deaths from acute coronary syndromes
(ACS) and ischaemic heart disease (IHD) rose four
fold in the triennium from 2000–2 to 2003–5. This
increase is one of the main reasons why cardiac
disease remains the single largest cause of UK
maternal death, accounting for nearly a quarter of
cardiac deaths.
There were 16 deaths from acute myocardial infarction (AMI). Of these, nine were
due to atherosclerosis, four to coronary arterydissection, and one was embolic. Only four late
deaths (42 days to 1 year postpartum) were
reported; this is almost certainly an underestimate,
since the obstetric services whose duty it is to
inform CEMACH (Confidential Enquiry into
Maternal and Childhealth) of pregnancy related
deaths are unlikely to be informed of admissions
for ACS that occur months after delivery.
There were an additional four deaths from heart failure
secondary to atherosclerotic IHD. This spread of
pathologies causing AMI is a reflection both of the
pregnant state and of the cardiovascularly
unhealthy lifestyle led by some women in the
UK. Coronary artery dissection is an uncommon
but recognised complication of pregnancy.
Like aortic dissection, it can occur in pregnancy and the puerperium in the absence of risk factors other
than the hormonal changes of pregnancy.
It is salutary to note that although there was no known pre-existing heart disease in those who died from AMI, every woman who died had identifiable risk factors.
The main risk factors were older age and obesity. The mean age of women dying of myocardial infarction was 35 years, and more than
a third were morbidly obese (body mass index
(BMI) >35). Smoking, hypertension, type II
diabetes and poor antenatal attendance were other important risk factors.
Outcome of acute coronary syndromes in
pregnancyAMI remains an uncommon event, and is estimated
to have occurred in 6.2 per 100 000
deliveries in the USA between 2000 and 2002.
However, pregnancy itself is a risk factor for AMI,
increasing the risk 3–4 fold compared with the
non-pregnant state. Maternal age is a further
factor, with the risk of pregnancy related AMI
being 30 fold higher in women over 40 years
compared to those under 20 years of age.
AMI is currently under investigation by the UK Obstetric
Surveillance System (UKOSS), an organisation
that prospectively investigates selected rare conditions
in pregnancy, to establish the incidence and
outcome.
The risk of death from AMI in pregnancy has been reported to be as high as 37%, but recent
data from the USA suggests the risk to be lower, at
around 5%.
There are several possible explanations for this apparent improvement in survival.
Strategies to identify and treat acute coronarysyndrome in general have improved, with emphasis
on rapid thrombolysis and the development of
widespread primary percutaneous intervention
(PCI). The latter may be of particular benefit to
pregnant women, both because lifesaving thrombolysis
may be withheld for fear of causing haemorrhage, and because PCI is the only effective treatment when the pathology is coronary artery dissection.
An alternative explanation of the apparent
improvement in mortality is that older definitions of AMI only included those with ST elevation;newer definitions are more inclusive and encompass
patients who are likely to have a better
prognosis.
Nonetheless, mortality remains higher than that of the non-pregnant population, and the 2003–5 CEMACH report identified substandard care in around a third of cases.
The most common problems were failure to recognise the symptoms of ACS or ECG changes by the obstetric team and,where rapid PCI was unavailable, withholding of thrombolysis in the face of a large ST segment elevation AMI, because of the risk of bleeding. In the latter situation a balance of risk must be made
between treating an extensive AMI and the risk of
bleeding—a team decision that has to involve
senior obstetric and cardiology staff.
Chest pain in pregnancy is common and may simply be asymptom of heartburn; however, it should never
be ignored as it may also represent AMI, pulmonary
embolism or aortic dissection.
Urgent cardiac review is always appropriate if a pregnant or postpartum woman presents with significant chest pain.
Of note,
troponin is not affected by pregnancy.
Management of ACS in pregnancy and the
puerperiumAs for all life threatening conditions in pregnancy,
the principle of management should be the same as for non-pregnant patients. ACS is one condition
where the mother should be treated first, before
the baby is delivered, whatever the gestational age,because the risk of delivery with an untreated ACS is so high.
Close liaison with the obstetric team is needed in order to monitor the wellbeing of the fetus and plan continuing antenatal or postnatal care.
Urgent PCI is the treatment of choice and consideration must be given to the type of stent deployed.
As a general rule, bare metal stents should be used in preference to drug eluting stents because the risk of stent thrombosis is likely to be lower when clopidogrel has to be stopped in order to avoid major bleeding at the time of delivery.
Aspirin should always be continued. Ideally clopidogrel should be continued for 6 weeks post-stent implantation, then stopped for a week before
delivery and restarted as soon as possible postpartum. Inevitably, there will be situations when
this practice cannot be followed; the cardiologist
and obstetrician must make an individualised joint
plan on the least risky approach.
There are only a handful of case reports on the
use of clopidogrel and small molecule glycoproteinIIb/IIIa receptor antagonists in pregnancy; they
indicate good maternal and fetal outcome, but no
conclusions on safety may be drawn from these
case reports.
The fetal radiation dose from PCI is low; if the maternal back and abdomen are protected and the field size coned down to the area of interest, the increased risk to the fetus of
dying of cancer within 15 years from 60 min
screening in the anteroposterior (AP) projection is
,1:80 000 (data derived from local radiation
protection team for actual case).
As for all procedures that require a pregnant woman to lie prone, a wedge should be placed under the right hip to prevent uterine compression of the inferior vena cava. There are little data on the use of thrombolysis for myocardial infarction in pregnancy; however, the complication rate for thrombolysis for pulmonary embolism in pregnancy is only 1%.
Therefore, if timely PCI is unavailable it is
unreasonable to withhold thrombolysis from a
pregnant woman who presents with an anterior or
anterolateral ST segment elevation AMI. If the
coronary arteries are found to be normal in the face
of an apparent ACS, coronary spasm or embolism
should be considered and infarction imaging
performed to seek evidence of myocardial damage.
Coronary artery bypass grafting in pregnancy
There are few reports of the use of coronary arterybypass grafting in pregnancy.
Maternal mortality from cardiopulmonary bypass surgery is up to 13% and the risk of
fetal loss is 30%.
Medical management of coronary artery disease in
pregnancyAddressing risk factors such as obesity, smoking,
hypertension, hyperlipidaemia and diabetes is particularly important in this group of young patients
who remain at continuing risk of further premature
cardiac events.
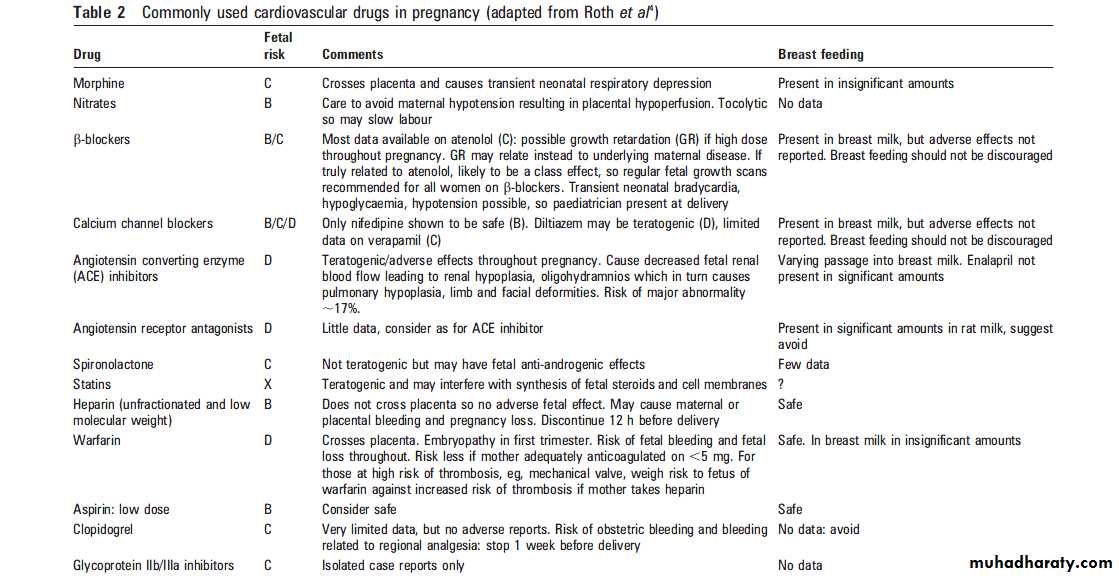
There are little data on the use of many cardiac drugs in pregnancy and breastfeeding,so the risks to the fetus may be unknown, and the risks and benefits must be considered on an individual basis (table 2).
As a general principle drugs should be avoided in pregnancy. However, effective treatment or prevention of a life threatening condition should not be withheld. The rise in pregnancy related deaths from
coronary artery disease is a particularly worrying
trend. At first sight it is at odds with the decline in
coronary mortality seen in the developing world
for the past 30 years—a decline that is largely due
to a reduction in risk factors.
However, in the UK and other countries, there has been a slowing in the reduction of coronary deaths in recent years. This, together with the rise in pregnancy related
coronary deaths in women with cardiovascular
risk factors, may mean that we are due to see
coronary deaths among the general population
again reaching epidemic proportions.
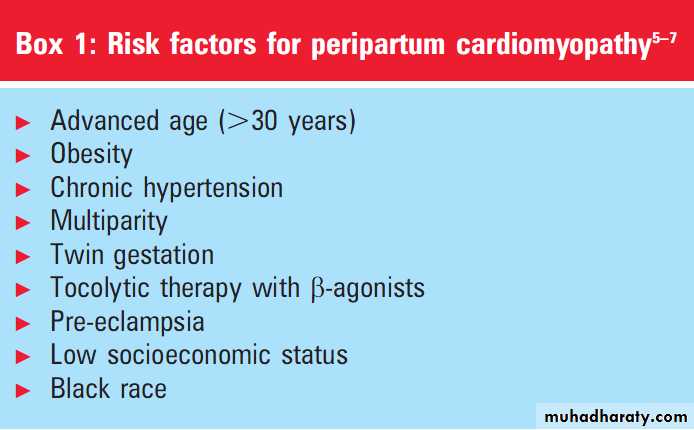
PERIPARTUM CARDIOMYOPATHY
Peripartum cardiomyopathy (PPCM) may be consideredas a subset of dilated cardiomyopathy, since
the clinical and pathologic presentation of PPCM is
similar to that of other types of dilated cardiomyopathy.
Its relationship with a (previous) pregnancy
and the long term prognosis discerns this disorder
from other forms of dilated cardiomyopathy.
The incidence of PPCM is very variable throughout the
world and ranges from 1 per 3000 to 1 per 4000 live
births. Risk factors for PPCM are listed in box 1. It
is most likely, however, that PPCM is multifactorial.
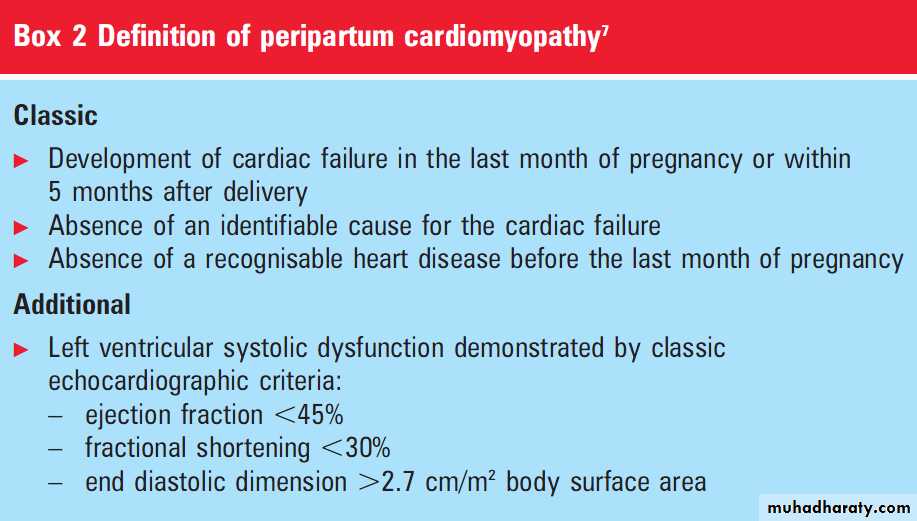
Although the diagnosis of PPCM is one of exclusion, the diagnosis of PPCM is made on the basis of classic and additional signs: timing of the first appearance of the disease and a combination of specific (newly developed) echocardiographic findings (box 2).
The differential diagnosis includes myocardial infarction, severe pre-eclampsia, sepsis, amniotic fluid embolism and pulmonary embolism.
It seems very important, especially with respect to
the prognosis of future pregnancies, to exclude
known causes of heart failure such as pregnancy
induced hypertensive disorders as a cause for PPCM.
Aetiology of PPCM
The aetiology of PPCM is still obscure. It is unlikely that it represents a clinically silent underlying cardiomyopathy that is unmasked by thehaemodynamic stress of pregnancy. A number of
possible causes have been postulated: myocarditis,
abnormal immune response to pregnancy, maladaptive
response to the haemodynamic stress of
pregnancy, accelerated myocyte apoptosis, stress
activated cytokines, viral infection, excessive prolactin
production, abnormal hormonal function,increased adrenergic tone, myocardial ischaemia, malnutrition and prolonged tocolysis. Cases of familial PPCM have also been described.
Management of PPCM in pregnancy and the
puerperium
In general, treatment of PPCM is similar to that of
other forms of congestive heart failure, reducing
afterload and preload and increasing contractility.
This involves salt and fluid restriction, the use of
diuretics to reduce volume overload, and antihypertensive medication to decrease afterload.
Angiotensin converting enzyme (ACE) inhibitors
are contraindicated during pregnancy; their use isoccasionally justified if the benefit to the mother
outweighs the risk to the fetus (table 2). Therefore,
during pregnancy, hydralazine and nitrates can be
used in combination with digitalis and a-blockers.
Postpartum, ACE inhibitors can be added.
Patients unresponsive to oral therapy may be treated with dobutamine, dopamine, and nitroprusside.
Arrhythmias should be treated according to the
usual protocol.
Women with PPCM show a high incidence of thromboembolism.
Anticoagulation with low molecular weight heparins should be considered (twice daily injections—for example, enoxoparin 1 mg/kg twice daily).
The use of immunosuppressive drugs is still under debate. Azathioprine and corticosteroids have both been used in PPCM. Some state that this medication
should only be used after proven myocarditis in
endomyocardial biopsies.
Techniques like intra-aortic balloon pump or
ventricular assist devices may be used as a bridge to heart transplantation. Since more than half of
women with PPCM die suddenly, the aggressive
use of implantable cardioverter-defibrillators
(ICDs) for primary prevention is warranted.
Delivery of women with PPCM
Unless cardiac failure cannot be treated adequately,pregnancy is allowed to proceed to term. Mode of
delivery depends on the maternal haemodynamic
situation and obstetric factors. Women with
adequate cardiac output may tolerate induction
of labour and vaginal delivery.
Prognosis of PPCM
The prognosis of PPCM has improved in recentyears due to better medical therapy. Despite this,
the long-term prognosis is still strongly related to
the recovery of ventricular function. More than
80% of all women with PPCM recover partially or
completely. Approximately 20% die or survive due
to cardiac transplantation.
Based on the ejection fraction at initial diagnosis, a prognosis for long term maternal outcome may be given. Women with an ejection fraction of ≤25% were very likely to receive a heart transplant in subsequent years. Asubsequent pregnancy influenced this negatively.
In women with an ejection fraction >25%, none of the women ended in end stage cardiac disease.
This was also the case after pregnancies in this group of women.
Recurrence of PPCM in a subsequent pregnancy
Strongly dependent on the severity ofPPCM in the index pregnancy and whether left
ventricular systolic function was normal at the
beginning of the subsequent pregnancy.
With an ejection fraction >25% at initial diagnosis of
PPCM, the recurrence rate in a subsequent
pregnancy is 20%. An abnormal ventricular function
at the beginning of pregnancy doubled the
incidence of PPCM to 40%.
AORTIC ANEURYSM, DISSECTION AND
PREGNANCYAortic aneurysm
The overall incidence of thoracic aortic aneurysm is
estimated to be around 6 per 100 000 patient years,
with males being affected 2–4 times more often
than females. The location of the aneurysms is
most often the ascending aorta (60%), followed by
aneurysms of the descending aorta (30%), whereas
arch aneurysms and thoracoabdominal aneurysms
occur less frequently. There are several heritable
disorders that affect the thoracic aorta, predisposing
patients to both aneurysm formation and
aortic dissection including
Marfan syndrome,
bicuspid aortic valve,
Ehlers–Danlos syndrome,
and familial forms of aortic dissection, aneurysm,
or annuloaortic ectasia.
Impact of pregnancy
During pregnancy, important maternal cardiovascularchanges occur, such as an increase in blood
volume, heart rate, stroke volume, cardiac output,
left ventricular wall mass, and end diastolic
dimensions, which starts as early as the fifth week
(fig 3). In addition, hormonal changes occur
which lead to histological changes in the aorta.
Fragmentation of the reticulum fibres, a diminished
amount of acid mucopolysaccharides, and
loss of the normal configuration of elastic fibres
have been observed in the aortic wall of pregnant
patients. So, both haemodynamic and hormonal
mechanisms have been suggested to play an
important role in the increased susceptibility to
dissection in women during pregnancy.
Dissection occurs most often in the last trimester of pregnancy or the early postpartum period. In all
women with enlarged aortic root diameters, the
risks of pregnancy should be discussed before
conception.
Women with previous aortic dissection are at high risk of aortic complications during pregnancy.
Counselling is very important in all patients with known aortic pathology.
Unfortunately, not all patients with aortic pathologyare aware that they are at risk. Therefore,
women with a family history of Marfan syndrome
or other familial aortic pathology should also have
counselling with a complete evaluation including
imaging of the entire aorta before pregnancy.
Marfan syndrome
Marfan syndrome, with a prevalence of 1 per 5000,
is the classical disorder associated with cystic
medial degeneration of the ascending aorta. It is
caused by mutations in the gene that encodes
fibrillin-1, resulting in both a decrease in the
amount of elastin in the aortic wall and a loss of
elastin’s normally highly organised structure.
Women with a normal aortic root diameter have
1% risk of aortic dissection or other serious cardiaccomplication during pregnancy.
When the aortic root diameter exceeds 4 cm the risk of dissection increases to 10%.
The Canadian guidelines
recommend that women with an aortic root
diameter >44 mm should strongly be discouraged
from becoming pregnant; the European guidelines
discourage pregnancy above an aortic root diameter of 40 mm.
There are still insufficient data available on pregnancy in women with Marfan syndrome with aortic root diameters >45 mm.
The risk is lower for pregnancy following elective
aortic root replacement.
Bicuspid aortic valve
Approximately 50% of young men with normally
functioning bicuspid aortic valve (BAV) have an
aortic dilatation. Ascending aortic specimens from
BAV patients have significantly less fibrillin-1
compared to patients with tricuspid aortic valves.
Furthermore, the aortic aneurysms of those with
BAV have more lymphocyte infiltration and smooth muscle cell apoptosis, suggesting degenerative changes similar to those found in Marfan patients.
Although patients with Marfan syndrome
are at a higher risk of aortic dissection compared to BAV patients (44% vs 6%), BAV isresponsible for more cases of aortic dissection (14%
vs 6–9%) due to its higher incidence in the general
population (1%). No data on pregnancy are
available. It is suggested to use the same guidelines
as for Marfan patients, but this is controversial.
Ehlers–Danlos syndrome
Aortic involvement occurs almost exclusively inEhlers–Danlos type IV which is transmitted as an
autosomal dominant trait. The incidence of this
disorder is estimated at 1 in every 5000 to 20 000
live births. During pregnancy women may show
increased bruising, hernias, varicosities, or suffer
rupture of large vessels.
Aortic dissection may occur without dilatation. The course of pregnancy should be closely monitored. Guidelines for elective intervention have not been established because the operative risk in these patients is so high.
Management of aortic dilatation in pregnancy
All patients with aortic pathology should bemonitored by echocardiography at 6–8 week intervals throughout the pregnancy and for 6 months
postpartum.
Each pregnancy should be supervised by a cardiologist and obstetrician who are alert to the possible complications.
Patients with aneurysms of the aorta are often
treated with b-blocking agents, to decrease thedetrimental impact of systole on the aortic wall.
The effectiveness of this treatment is largely
unproven and somewhat controversial, but it has
become standard practice.
The original evidence is based on a small number of Marfan syndrome patients followed for a long period of time.
These data are not directly applicable to those with BAV or others without the Marfan syndrome. Fetal
growth should be monitored when the mother is
taking b-blockers. A recent mouse study demonstrated
that AT1 antagonists are very promising,
exerting their effect by reducing transforming
growth factor-b signalling. However, AT1
antagonists are contraindicated during pregnancy.
Surgical management of aortic dissection and
aortic aneurysm
Chest pain in pregnancy is commonly due to
gastro-oesophageal reflux, but may represent dissection, myocardial infarction or pulmonary embolism—acute life threatening conditions must be
excluded. Transthoracic echocardiography may
show dissection, but urgent computed tomography
or magnetic resonance imaging must be performed.
Aortic dissection in pregnancy is a surgical emergency;
senior cardiothoracic, cardiology, obstetricand anaesthetic consultants must act rapidly to
deliver the fetus (if viable) by caesarean section in
cardiac theatres and proceed directly to repair of
the dissection. The risk of obstetric bleeding due to
anticoagulation during cardiopulmonary bypass
must be weighed against the risk of delaying repair
of the dissection for a few hours post-delivery.
Repair with a composite graft or replacement with
a homograft avoids the need for long term anticoagulants.Pre-pregnancy surgery is recommended if aortic
root enlargement (>4.5 cm, or less in patients with
a low body surface area) is known in a Marfan
syndrome patient or in a patient known to have a
bicuspid aortic valve.
Elective aortic root replacement can be performed with very low morbidity and mortality. When dilatation of the aorta is discovered during pregnancy or progressive dilatation occurs during pregnancy, before 30 weeks of gestation, aortic repair with the fetus in utero is recommended. The risks of surgery for the mother during pregnancy are not much higher than outside pregnancy, but the risks for the fetus are
considerable with a mortality rate of 10–22%.
High flow, high pressure normothermic perfusion and a
perfusion index of 3.0 during cardiopulmonarybypass is probably safest for the fetus.
Hypothermia decreases placental blood flow and
may cause fetal bradycardia, leading to intrauterine
death or severe hypoxic–ischaemic fetal insult.
However, avoiding hypothermia precludes an open
distal aortic repair, which is preferable.
Progesterone per vaginum and continuous fetal
heart monitoring may reduce the risk to the fetus.After 30 weeks of gestation, caesarean section
followed directly by cardiac surgery seems to be
the most promising option to save the lives of the
mother and her unborn child. Cardiac surgery
should be performed in a hospital in which
neonatal intensive care facilities are available.
Delivery
The primary aim of intrapartum management in
patients with aortic root enlargement is to reduce
the cardiovascular stress of labour and delivery. If
the aortic root diameter is<4.5 cm normal
delivery can be performed, but preferably with
expedited second stage.
Delivery by caesarean section is recommended when the diameter exceeds 4.5 cm. Regional anaesthesia is advised to prevent blood pressure peaks, which may induce dissection. Close monitoring and administration of b-blocking drugs should continue up to 3 months
postpartum, because dissection can occur during
this period.
REGISTRY ON PREGNANCY AND HEART DISEASE
Despite increasing numbers of pregnant womenwith heart disease, management is currently based
on a limited body of adequate research. For up to
date information about treatment during pregnancy
and pregnancy outcome a large prospective
observational registry has been initiated by the
European Society of Cardiology and Association
for European Paediatric Cardiology, which is web
based and now open for inclusion to all cardiologists
and obstetricians taking care of patients with
heart disease (www.euroheartsurvey.org; ehs@
escardio.org).
The categories of fetal risk are:
A: Safe. Controlled studies do not show fetal harm; possibility of harm remoteB: Likely to be safe. No fetal harm shown in animal studies, or harm shown in animal studies but not in controlled human studies.
C: Fetal risk possible, only use if potential benefit outweighs the risk. No data, or fetal harm in animal studies, but no studies in humans.
D: Proven fetal risk, use may be justified if maternal benefit outweighs risk.
X: Proven fetal risk that outweighs any possible maternal benefit.