Women and coronary disease
Heart 2008د. حسين محمد جمعه
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
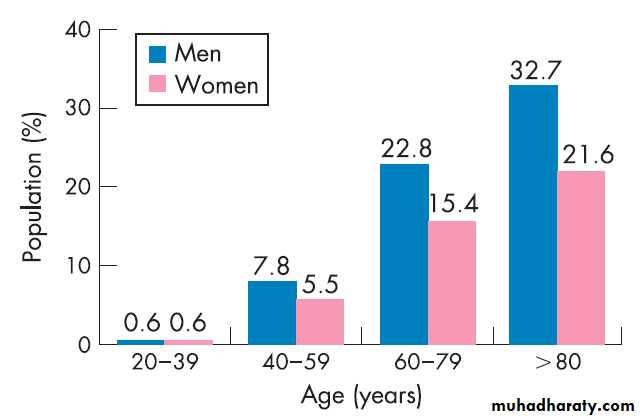
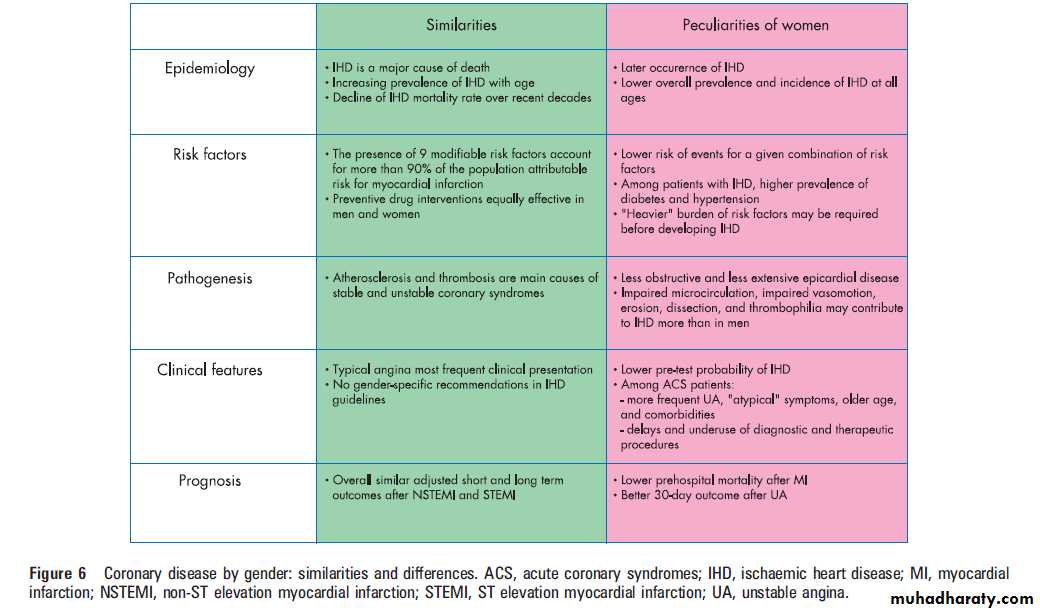
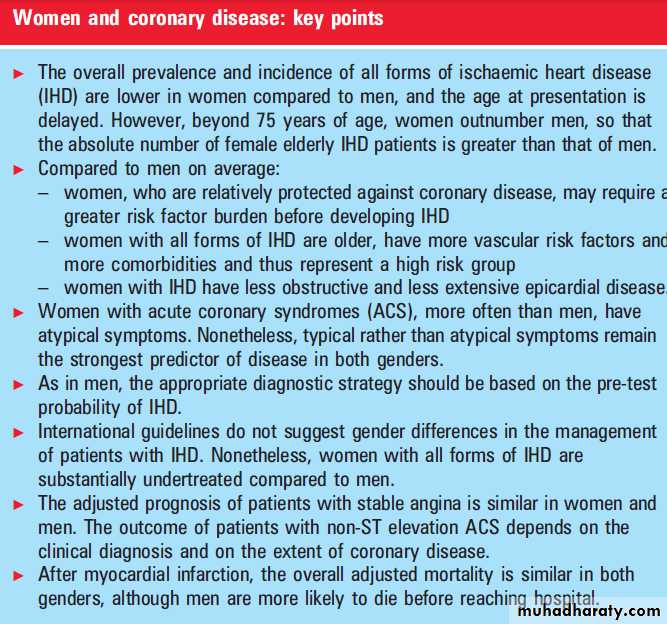
The prevalence and incidence of IHD at all ages
tends to be higher in males than in females,increasing with age in both genders. However, since the female elderly population is larger than that of males, beyond 75 years of age the absolute number of women discharged for IHD overcomes the number of males (364 000 vs 326 000 per year in the USA).
At the time of afirst coronary event, women are approximately 10 years older than men.
In the Framingham Heart Study (FHS), angina was the initial diagnosis of IHD in 61% of women but only in 38% of men; in contrast, men more often exhibit myocardial infarction (MI) or sudden death as first manifestations.Among patients with suspected acute
coronary syndrome (ACS), the discharge diagnosis
in women is more commonly unstable angina
compared to men. Over the past three decades,
the relative risk (RR) of coronary death has
declined similarly in both genders.
CARDIOVASCULAR RISK FACTORS
In the case–control INTERHEART study of 15152patients with MI and 14820 controls, 90% of the
population attributable risk for MI in both genders
was accounted for by the presence of
Nine modifiable risk factors:
raised serum lipoprotein apoB/A1 ratio, smoking, diabetes, psychosocial
stress, hypertension, high waist-to-hip ratio, low
fruit and vegetable intake, lack of regular exercise,
and lack of regular alcohol intake .
Diabetes and hypertension
The prevalence of hypertension in the general population >60 years of age is reported to be higher among women compared to age matched men, although a possible survival bias cannot be excluded.In women, diabetes and hypertension appear to
confer a higher risk of coronary events compared to
men. A possible explanation is that diabetes and
hypertension promote IHD more aggressively in
women than in men, perhaps in relation to the
smaller coronary size.
Alternatively or additionally,we propose that women—who per se are relatively
protected against IHD—may require a greater risk
factor burden compared to men before developing
IHD. Consistent with the latter is the lower
likelihood of disease in women than in men for a
similar combination of risk factors.
A meta-analysis of studies specifically enrolling
diabetic and control subjects, with an averagefollow up of 14 years, found no significant gender
related difference in the risk of coronary death (2.9
for diabetic vs non-diabetic women compared to
2.3 for diabetic vs non-diabetic men, p=0.19) or
non-fatal MI related to diabetes (1.7 for diabetic vs
non-diabetic women compared to 1.6 for diabetic
vs non-diabetic men, p=0.68).
Population based studies, instead, found that women who develop afirst coronary event have a two- to threefold adjusted risk of having diabetes compared to men. Overall, these findings suggest that diabetes and hypertension per se may not increase the risk of
IHD more in women than in men,6 but simply that
women who develop IHD are more frequently
diabetic and hypertensive compared to men
(‘‘higher risk factor burden’’ hypothesis).
Lipids and metabolic syndrome
Beyond 65 years of age, the prevalence of hypercholesterolaemia
(>240 mg/dl, >6.2 mmol/l) is more than twofold greater in women compared to men; as for hypertension.
The odds ratio and population attributable risk for MI associated with a raised lipoprotein apoB/apoA1 ratio are similar in the two sexes.
Low density lipoprotein
(LDL) cholesterol lowering by statins is associatedwith similar reductions in coronary and cerebral
ischaemic events and in overall mortality in men
and women. Whether the presence of metabolic
syndrome confers a higher risk of IHD in women
than in men is not clear. The INTERHEART
study found similar odds ratios for MI associated
with a high waist-to-hip ratio in the two genders.
Smoking and stress
The prevalence of never smokers in the generalpopulation is higher in women than in men (53%
vs 29%). In the ARIC (Atherosclerosis Risk In
Communities) study, current female smokers had a
relative risk of coronary disease of 2.95 vs 1.55 inmen, in line with our hypothesis that women
require a larger cluster of risk factors before
reaching the threshold of IHD.
Perceived high levels of mental stress, compared to low levels, have been associated with an increased risk of fatal IHD in women, but not in men. The
INTERHEART study, on the other hand, found
similar odds ratios for MI in men and women who
smoked or in association with psychosocial stress.
Figure 1 Prevalence of ischaemic heart disease in the USA by age and gender. The prevalence of ischaemic heart disease is lower in women than in men in most classes of age. Reproduced with permission from the Heart Disease and Stroke Statistics—2007 Update.
Family history
The Physicians’ and Women’s Health Studies (totalling 534 154 subject-years) assigned to amaternal history of MI, especially if premature, ahigher relative risk of cardiovascular disease compared with a paternal history.w13 Given the lower prevalence of MI among females (table 1), amaternal history of MI may signal a more unfavourable background.MECHANISMS OF DISEASE
Women with IHD have less obstructive and less extensive epicardial disease than men, suggesting that other mechanisms—such as impaired microcirculation,impaired vasomotion, erosion, dissection,and thrombophilia—may contribute to ischaemia more frequently than in men.Atherosclerosis
Autopsy data indicate that, in the general population,the severity of coronary stenoses is less in
women than in men, a difference that is lost in the
very elderly. Women admitted to hospital for all
forms of ACS have fewer diseased epicardial
arteries compared to men .
Women with a fatal ACS, compared to men, are
more likely to have plaque erosion, rather than
plaque rupture. Among women, plaque erosion
has been associated with smoking and younger
age. Similarly, spontaneous coronary artery
dissection appears to be more prevalent in women
than in men, particularly if young and without
significant coronary atherosclerosis. Thus, on
average, women have less obstructive and less
extensive epicardial disease than men.
Thrombophilia
In a general Scottish population of 8824 subjects(aged 40–60 years, 4309 women), plasma fibrinogen
values were higher in women than in men for
all age strata. In patients with obstructive
coronary disease, women again showed higher
age adjusted plasma levels of fibrinogen, in addition
to higher plasminogen activator inhibitor-1
antigen and factor VII:C, compared to men.
Interestingly, during the first 24 h after trauma or
injury, young/middle aged women are more
hypercoagulable than men.
Overall, the evidence suggests a greater procoagulant potential in women than in men, a condition which may have conferred survival benefits by limiting postpartum bleeds.
Endothelial/microvascular dysfunction and
vasomotionEndothelial dysfunction can predict adverse coronary
events in men and women, independently of
coronary disease severity, but appears to occur
later in women compared to men. Patients with
angina, normal epicardial arteries and a positive
exercise test (cardiac syndrome X), as well as
Japanese patients with microvascular angina, are
more often women than men. Conversely,
epicardial vasospastic disease (variant angina) does
not show a female predilection.
Oestrogens and menopause
Oestrogens have potential protective cardiovasculareffects through high density lipoprotein (HDL)
and LDL cholesterol modulation, inhibition of
smooth muscle proliferation, enhanced nitric
oxide, prostacyclin and vascular endothelial
growth factor synthesis, and progenitor cell stimulation
; however, they also have potential detrimental
effects (increasing triglycerides and
inflammatory and prothrombotic markers).
Whether the lower prevalence of IHD among premenopausal women compared to age matched
men can be attributed specifically to a protective
role of endogenous oestrogens is still not clear.
Randomised trials testing exogenous oestrogens for
the prevention of IHD showed no benefit or evenharm in terms of cardiovascular events.
To explain these findings, a‘‘timing hypothesis’’ has
been proposed,
whereby oestrogens may be cardioprotective only before the development of advanced atherosclerotic lesions.
Other possible biases may concern the type of oestrogen, concomitant progestins, route of administration, and age and risk factors of enrolled women. Currently,
however, the evidence does not support the use of
oestrogens for the primary or secondary prevention of IHD.
The impact of menopause per se on IHD is
difficult to unravel from the concomitant increasein traditional risk factors.
In the Nurses’ Health Study, each 1 year decrease in age of onset of natural menopause was associated with a small, smoke related, increase in the relative risk of IHD. (RR 1.03, 95% confidence interval (CI) 1.01 to 1.05).w29 Bilateral oophorectomy carries an
adjusted relative risk of cardiovascular disease of
4.55 (95% CI 2.56 to 8.01).10 The overall rate of
coronary deaths, however, remains lower in
women than in men up to four decades beyond
the average time of menopause (50–54 years).
Autonomic balance
Women, unlike men, have aprevailing parasympathetic autonomic cardiac tone.
This is consistent with a higher female rate of syncope, hypotension,and bradycardia after MI, and, conversely, with more malignant post-MI tachyarrhythmias and ahigher incidence of sudden cardiac death among men.
PREVENTIVE STRATEGIES
The most important strategy to prevent IHD inwomen is to avoid an underestimation of the risk
of disease.
For primary prevention, in both genders, the use
of aspirin is limited to subjects at high cardiovascular
risk. High risk subjects can be defined as
those with an absolute 10 year probability of a
fatal cardiovascular event >5% when extrapolated
to age 60 years or above, or of MI and coronary
death > 20%.
This risk should be weighed against that of major bleeds with aspirin intake, of approximately 1–2% over 10 years.
Similarly, lipid lowering treatment is currently recommended in both male and female subjects at high cardiovascular risk, who have a total cholesterol > 190 mg/dl (> 5 mmol/l) and/or an LDL cholesterol
> 115 mg/dl (> 3 mmol/l), despite lifestyle changes.
The prevention of IHD events by blood pressure control is of a similar degree in both sexes,
as shown by ALLHAT (Antihypertensive and Lipid
Lowering treatment to prevent Heart Attack Trial)
during 6 years of follow up.
For the secondary prevention of IHD, the
evidence based benefits of several cardiovascular
drugs (aspirin, thienopyridines, statins, inhibitors
of the renin–angiotensin system, b-blockers) are
similar in both genders, despite sex-specific
differences in pharmacokinetics and pharmacodynamics.
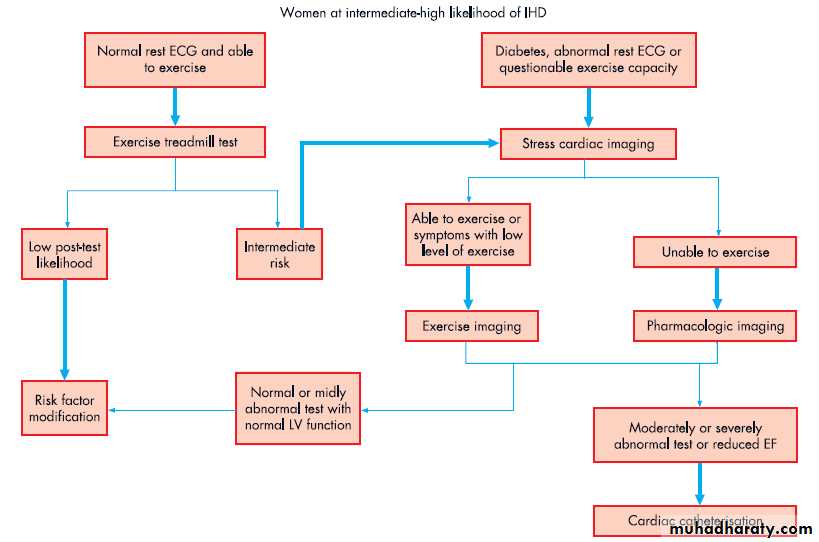
NON-INVASIVE DIAGNOSTIC TESTING
The lower pre-test likelihood of IHD in women
compared to men is associated with a higher
probability of false positive results and thus a
lower specificity of non-invasive diagnostic testing
in women (Bayes’ theorem).
Additionally, the sensitivity of exercise ECG is
lower in women compared to men. The inclusion
of a multiparametric evaluation (for example, the
Duke treadmill score), particularly in women, may
improve the diagnostic accuracy of exercise ECG.
Exercise thallium single photon emission
computed tomography (SPECT) shows a highersensitivity, but not specificity, compared to exercise
ECG in women, although the overall sensitivity
remains lower compared to men.
Technetium-99m sestamibi SPECT yields a higher
specificity compared to thallium SPECT in
women, with similar results in both sexes after
correction for referral bias.
Stress echocardiography
is reported to be the most accurate
provocative test in women (with a higher specificity
and sensitivity compared to SPECT and
exercise ECG) and the most specific test in both
genders.
Coronary calcium score, in both sexes,
may be an important diagnostic tool to rule out
disease, given its high specificity, although its
sensitivity is low.
As in men, the appropriate diagnostic strategy in
women should be based on the pre-test probabilityof IHD. Women with an intermediate–high
pre-test likelihood of IHD should undergo noninvasive
testing .An intermediate–high likelihood of IHD can be defined as women >50 years of age with typical or atypical chest pain, or women ,50 years of age with typical angina, or women with symptoms plus diabetes or other multiple risk factors.
CORONARY ANGIOGRAPHY, PERCUTANEOUS
INTERVENTION AND BYPASS SURGERYWomen undergo cardiac catheterisation less frequently
than men even after MI.
At coronary angiography, women are older and more frequently diabetic and hypertensive. Early studies on balloon angioplasty showed more frequent adverse outcomes and higher dissection rates in women, probably related to comorbidities and smaller coronary size.
In the stent era, several, though not
all, studies show similar adjusted in-hospital
and long term mortality in the two sexes.
Long term rates of other major coronary events and
of restenosis are also similar in both genders.
Vascular complications after percutaneous coronary
intervention (PCI) remain more common in women
than in men.
Current indications for PCI or bypass surgery in the acute and stable patient do not differ according to gender.
Short term mortality is reported to be worse, but long term mortality better, after bypass surgery in women
compared to men.
STABLE ANGINA
Epidemiology and presentationThe CHS (Cardiovascular Health Study) and FHS
reported a lower prevalence and incidence of
angina (defined mostly by physician interview) in
women compared to men .A large Finnish study confirmed a slightly lower, age standardised, annual incidence of angina (assessed by nitrate prescription or by invasive or noninvasive testing) in women, with a male to female ratio of 1.07 (95% CI 1.06 to 1.09). On the contrary, the ARIC study reported a higher
prevalence and incidence of angina, defined by less
restrictive criteria, in women than in men.
In the FHS, angina was the most common first
clinical diagnosis of IHD in women but not in
men. Female patients with angina, compared to
men, are older, more often hypertensive, less
frequently smokers or with prior MI, and report
a higher intensity of pain on a visual analogue
scale. On average, the available data indicate
lower prevalences and incidences of stable angina
in women than in men.
Management and prognosis
In the Euro Heart Survey of 3779 patients withangina, compared to men, women were less likely
to receive non-invasive and invasive diagnostic
procedures, or to be treated by coronary revascularisation and appropriate medical therapy (including the combination of antiplatelet and lipid
lowering drugs), even in the presence of significant
angiographically documented coronary disease.
Several reports indicate a better or similar age
and risk factor adjusted prognosis in women thanin men with diagnosed angina. An important limitation of these studies, however, is the absence of angiography, that isknown to show less extensive coronary disease in women with angina compared to men. In acohort of 1457 patients with stable angina undergoing coronary stenting (32% female), women exhibited similar 1 year relative risk of death,
non-fatal MI and cardiac rehospitalisation compared
to men, even after adjustment for the extent
of coronary disease.
The Euro Heart Survey also found no gender difference in the outcome of the overall population, but assigned an adjusted twofold worse prognosis (death/non-fatal MI at 1 year follow up) to the subgroup of women with
angiographically documented disease compared to
men; this subgroup, however, may have selected
women at particularly high risk. Thus, on
balance, the available data suggest similar outcomes
for men and women with stable angina,
despite a degree of female undertreatment.
ACUTE CORONARY SYNDROMES
Epidemiology and presentation The prevalence and incidence of MI are consistently lower in women than in men, across all classes of age .Among patients withACS, women present more frequently with
unstable angina (UA) and non-ST elevation MI
(NSTEMI) and less frequently with ST elevation
MI (STEMI) compared to men.
Women with ACS report a similar incidence of
chest pain compared to men, but more often an‘‘atypical’’ location (back, jaw, neck), a higher
intensity, and additional nausea, fatigue, dizziness,
dyspnoea, and anxiety/fear.
Thus, symptoms considered ‘‘atypical’’ for men may be ‘‘characteristic’’for women, although not necessarily the most prevalent.
Nonetheless, typical, rather than atypical, symptoms remain the strongest predictor of ACS in both women and men. Women hospitalised for MI are older, and more often hypertensive and diabetic compared to men.
The prevalence of ‘‘normal’’ or non-obstructive
coronary arteries is roughly twofold higher in
women with ACS than in men, particularly for
those with non-ST elevation ACS .
Non-ST elevation acute coronary syndromes (UA/
NSTEMI) A recent study showed a significant underuse of medical treatment on admission and even after discharge in women compared to men with non-ST elevation ACS, despite a higher risk factor profile and the lack of gender differences in treatment guidelines.For both genders, the American College of Cardiology/American Heart Association and the European Society of Cardiology UA/NSTEMI guidelines recommend an early invasive strategy (particularly coronary angiography within 48 h) for patients at high cardiovascular risk. The latter may be defined by the presence of recurrent, rest or low threshold ischaemia, dynamic ST segment changes, elevated troponin concentrations, signs of heart failure, malignant arrhythmias, recent PCI, and prior
coronary artery bypass graft surgery (CABG).
Although not all studies show a significant benefit of
an invasive versus a non-invasive strategy for womenwith non-ST elevation ACS,16 it is important to
consider the lower representation of women than
men in all trials, and the differences across trials in
baseline risk, in timing and type of revascularisation
(CABG vs PCI), and in the use of glycoprotein IIb/
IIIa inhibitors.
The impact of gender on the outcome of non-ST
elevation ACS is debated. Women have a higher
prevalence of non-obstructive coronary disease compared to men, and this subpopulation, in both genders, has a better in-hospital prognosis compared to those with significant disease. At least four studies found male gender independently associated with long term risk of death and even after adjustment for angiographic features, and despite the lesser access of women to invasive and non-invasive diagnostic procedures.
No differences in long term prognosis were found in
other reports on NSTEMI22 or non-ST elevationACS.w67 w75 Finally, one investigation found a worse
prognosis in the subgroup of women with non-ST
elevation ACS and significant coronary stenoses
undergoing PCI compared to men.w64 None of these
studies, however, directly compared patients with
NSTEMI to those with UA.
This comparison was performed within the GUSTO IIb trial that showed a similar adjusted risk of death and reinfarction at 30 days among women and men admitted for NSTEMI, but an independent protective effect of female gender in patients with UA (odds ratio 0.65,95% CI 0.49 to 0.87; p=0.003).
Thus, the available data suggest that the differences in outcome for men and women with UA/NSTEMI largely depend on clinical diagnosis and extent of coronary disease.
Figure 5 A proposed
algorithm for the noninvasiveevaluation of
symptomatic women at
intermediate–high
likelihood of ischaemic
heart disease. See text for
definition of intermediate–
high likelihood. EF, ejection
fraction; LV, left ventricular.
Modified with permission
from Mieres et al.14
ST elevation myocardial infarction
Women with STEMI compared to men are more
likely to present to hospital later, with
atypical symptoms, leading to a more difficult
recognition of MI, a greater delay in obtaining a
first 12 lead ECG, and a more frequent missed
diagnosis.
On average, women have a more frequent history of angina or heart failure and ahigher Killip class.
Even after adjustment for comorbidities and age, women more frequently than men experience in-hospital shock, pulmonary oedema, atrioventricular block, stroke, cardiac rupture, and major bleeds.
In contrast, the incidence of early malignant tachyarrhythmias and sudden cardiac death are more common in men.
When STEMI is diagnosed, women less often receive appropriate treatment, including admission to
a coronary care unit and thrombolysis.
If rapidly feasible, primary PCI is the better
revascularisation strategy in women as in men,
although vascular complications occur more often in
women. Women experience longer door-to-balloon
delays after diagnosis.
Primary PCI seems to offer better myocardial salvage in women, suggesting greater myocardial tolerance to hypoxia than in men.
Following thrombolysis, several but not all studies report higher adjusted in-hospital and 30 day mortality in women than in men. The apparent discrepancies among these investigations may stem from heterogeneity in statistical adjustments, examined populations, and observed time periods (for example, pre-hospital vs in-hospital).
Indeed, the MONICA study (Monitoring trends and determinants in Cardiovascular disease), that took into account pre-hospital deaths, found a lower prehospital but a higher in-hospital mortality rate in
women compared to men, without significant
gender differences in overall 28 day mortality.
This observation (that men are more likely to die before reaching the hospital) has been confirmed by others. Most studies do not find gender
differences in the adjusted long term mortality
rates after STEMI.
Several but not all studies also report a significant interaction between age and gender related outcome after STEMI, with higher mortality rates after hospitalisation in younger women compared with age matched men, but better outcomes among older women. Again, however, when pre-hospital deaths are taken into account, the higher 30 day mortality in younger (,55 years) hospitalised women, compared to age matched men, disappears, turning into a female advantage.
The adjusted mortality rates after primary PCI in women compared to men are reported to be significantly higher or no different during hospitalisation, but similar at 30 days and long term. Taken together, the above data suggest that overall outcome post-STEMI in the two sexes may not differ substantially, but that early pre-hospital deaths occur more often in men, especially if young.
CONCLUSION
As in men, IHD constitutes a major cause of death and morbidity in women, and this fact is underestimatedby both women and cardiologists.
Educational initiatives specifically tailored to
the female population and to the medical
community will enhance awareness and contribute
to reducing undertreatment of women in the acute setting and in the primary and secondary prevention of disease.
Cardiologists must pay particular attention to women hospitalised for IHD because, on average, they are older, with multiple risk factors and comorbidities, and therefore at high risk. Nonetheless, the lower overall
prevalence of coronary disease in women and its
occurrence at a more advanced age suggest a
protective effect of female gender on the development
of IHD.
In perspective, Elizabeth I (1533–1603) might well have cherished her heart of aqueen when she humbly said, ‘‘I have the body of aweak and feeble woman, but the heart of aking’’