Charcot, the father of neurology, famously stated, "Listen and the patient will give you the diagnosis."
د. حسين محمد جمعة
اختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2011
I would like to thank the countless medical students
and residents who teach me and compel me to learn every day.Don't drink your calories
Health tipFructose Consumption and Risk for Gout in Women
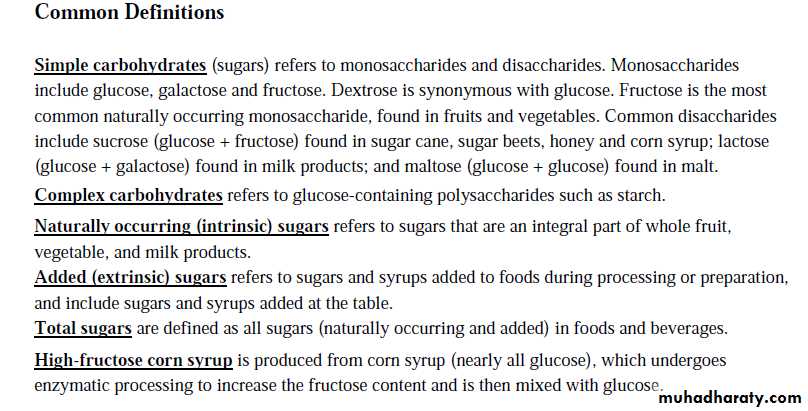
One daily fructose-sweetened soft drink raised risk for gout by 74%.Fructose consumption rapidly raises blood uric acid levels. In a recent study, consumption of fructose in sweetened soft drinks, fruit juices, Might the same be true for women? Validated food-frequency questionnaires from nearly 79,000 women in the prospective Nurses' Health Study were used to answer this question; participants were gout free at baseline and were followed for 22 years.
At the study's end, 778 women had developed gout. After adjustment for multiple variables (e.g., age, body-mass index, medical conditions), daily consumption of one fructose-sweetened soft drink significantly raised risk for gout by 74% (relative risk, 1.74), and daily consumption of two or more soft drinks raised risk by 139 compared with consumption of less than one soft drink per month. Similarly increased risks were found for corresponding consumption of orange juice . Consumption of diet soft drinks was not associated with gout.
Comment: As in men, consumption of fructose — most commonly in sweetened soft drinks and in fruit juices — elevates risk for gout in women. Consumption of fructose-sweetened soft drinks also raises risk for obesity and type 2 diabetes.
These data support the following health tip:
Don't drink your calories.
Prostaglandins whose synthesis involves the cyclooxygenase-I enzyme, or
COX-1, are responsible for maintenance and protection of the GIT,while prostaglandins whose synthesis involves the cyclooxygenase-II enzyme, or
COX-2, are responsible for inflammation and pain.
Anemia can give rise to venous hum in neck and needs to be distinguished from the bruit of carotid artery stenosis.
Venous hum
Systolic and diastolic
Continuous at the root of neck
Disappears easily with compression
Disappears in supine position
Carotid bruit
Systolic
Does not disappear with gentle compression
Does not disappear in supine position
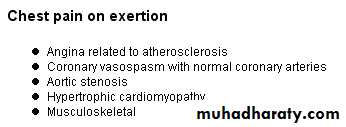
Chest pain of acute pericarditis. It is usually of sudden onset, occurring in the anterior chest and may be pleuritic in nature --- that is, sharp and worsens with inspiration, due to concomitant pleural inflammation. The pain may be alleviated with sitting up and leaning forward while worsened with lying down, and also may radiate to the back, to one or both trapezius ridges. However, the pain can also be dull and steady, resembling the chest pain in an acute myocardial infarction. As with any chest pain, other causes must also be ruled out, such as GERD, pulmonary embolism, muscular pain, etc.
Pericardial friction rub.The most important physical sign .May have up to 3 components: presystolic, systolic, and diastolic.The most frequent component is systolic.
High-pitched, scratching, grating sound
Sometimes only elicited when firm pressure with the diaphragm of the stethoscope is applied at the left lower sternal border .Heard most frequently during expiration with the patient in the sitting position .Rub is often inconstant; it may disappear and reappear the following day.
Diagnosis
Inflammatory markers. A CBC may show an elevated white count and a serum C-reactive protein may be elevated.Molecular markers. Acute pericarditis is associated with a modest increase in serum creatine kinase MB (CK-MB)[2][3] and cardiac troponin I (cTnI)[4],[5] both of which are also markers for myocardial injury. Therefore, it is imperative to also rule out acute myocardial infarction in the face of these biomarkers. The elevation of these substances is related to inflammation of the myocardium. Also, ST elevation on EKG (see below) is more common in those patients with a cTnI > 1.5 µg/L.
Coronary angiography in those patients should indicated normal vascular perfusion. The elevation of these biomarkers are typically transient and should return to normal within a week. Persistence may indicated myopericarditis. Troponin levels increase in 35 - 50% of people with pericarditis.[6]
Electrocardiogram (EKG). EKG changes in acute pericarditis mainly indicates inflammation of the epicardium, since the fibrous pericardium is electrically inert. For example, in uremia, there is no inflammation in the epicardium, only fibrin deposition, and therefore the EKG in uremic pericarditis will be normal.
Typical EKG changes in acute pericarditis includes[7][2]
stage 1 -- diffuse, positive, ST elevations with reciprocal ST depression in aVR and V1. Elevation of PR segment in aVR and depression of PR in other leads especially left heart V5, V6 leads indicates atrial injury.stage 2 -- normalization of ST and PR deviations
stage 3 -- diffuse T wave inversions (may not be present in all patients)
stage 4 -- EKG becomes normal OR T waves may be indefinitely inverted.
Rarely, electrical alternans may be seen, depending on the size of the effusion.
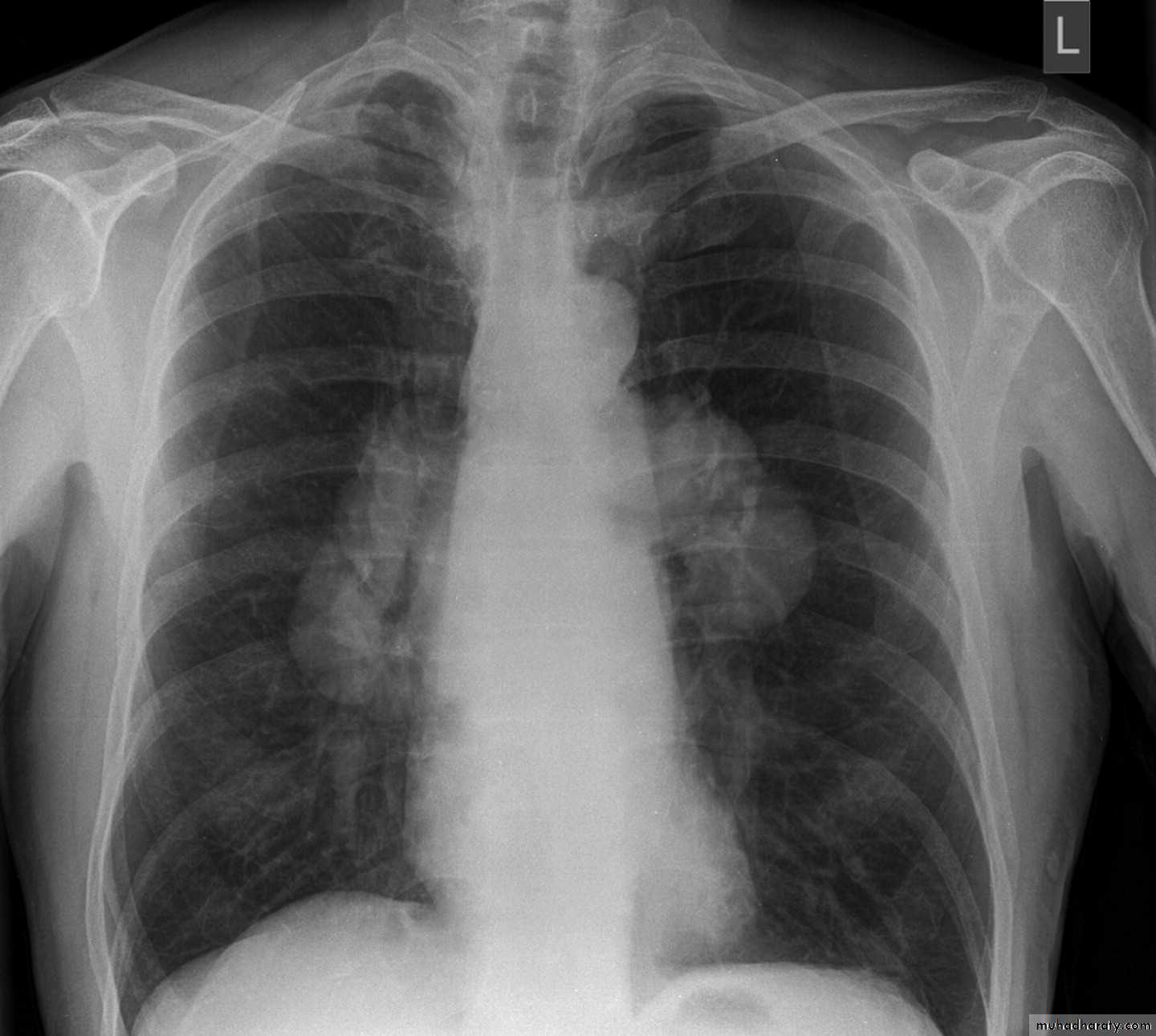
Chest X-ray. Usually normal in acute pericarditis, but can reveal cardiomegaly (enlarged heart) if the pericardial effusion is more than 200 mL. Conversely, patients with unexplained new onset cardiomegaly should always be worked up for acute pericarditis.Echocardiogram. Usually normal in acute pericarditis but can reveal pericardial effusion, the presence of which supports the diagnosis, although its absence does not exclude the diagnosis.
Treatment
Patients with uncomplicated acute pericarditis can generally be treated and followed up in an outpatient clinic. However, those with high risk factors for developing complications will need to be admitted to an inpatient service, most likely an ICU setting.
High risk patients include:
• subacute onset• high fever (> 100.4 F/38 C) and leukocytosis
• development of cardiac tamponade
• large pericardial effusion (echo-free space > 20 mm) resistant to NSAID treatment
• immunocompromised
• history of oral anticoagulation therapy
• acute trauma
• failure to respond to seven days of NSAID treatment
Pericardiocentesis is a procedure whereby the fluid in a pericardial effusion is removed through a needle. It is performed under the following conditions:[9]
• presence of moderate or severe cardiac tamponade
• diagnostic purpose for suspected purulent, tuberculosis, or neoplastic pericarditis
• persistent symptomatic pericardial effusion
NSAID in viral or idiopathic pericarditis. In patients with underlying causes other than viral, the specific etiology should be treated. With idiopathic or viral pericarditis, NSAID is the mainstay treatment. Goal of therapy is to reduce pain and inflammation. The course of the disease may not be affected. The preferred NSAID is ibuprofen because of rare side effects, better effect on coronary flow, and larger dose range. Depending on severity, dosing is between 300–800 mg every 6–8 hours for days or weeks as needed.
An alternative protocol is aspirin 800 mg every 6–8 hours.[8] Dose tapering of NSAIDs may be needed. In pericarditis following acute myocardial infarction, NSAIDs other than aspirin should be avoided since they can impair scar formation. As with all NSAID use, GI protection should be engaged. Failure to respond to NSAIDs within one week (indicated by persistence of fever, worsening of condition, new pericardial effusion, or continuing chest pain) likely indicates that a cause other than viral or idiopathic is in process.
Colchicine can be used alone or in conjunction with NSAIDs in prevention of recurrent pericarditis and treatment of recurrent pericarditis. For patients with a first episode of acute idiopathic or viral pericarditis, they should be treated with an NSAID plus colchicine 1–2 mg on first day followed by 0.5 daily or BID for three months.
Corticosteroids are usually used in those cases that are clearly refractory to NSAIDs and colchicine and a specific cause has not been found. Systemic corticosteroids are usually reserved for those with autoimmune disease.
Pericardial rub is a very specific sign of acute pericarditis. However, absence of this sign does not rule out disease. This rub can be best heard by the diaphragm of the stethoscope at the left sternal border arising as a squeaky or scratching sound, resembling the sound of leather rubbing against each other. This sound should be distinguished from the sound of a murmur, which is similar but sounds more like a "swish" sound than a scratching sound. The pericardial rub is said to be generated from the friction generated by the two inflamed layers of the pericardium; however, even a large pericardial effusion does not necessarily present a rub. The rub is best heard during the maximal movement of the heart within the pericardial sac, namely, during atrial systole, ventricular systole, and the filling phase of early ventricular diastole.
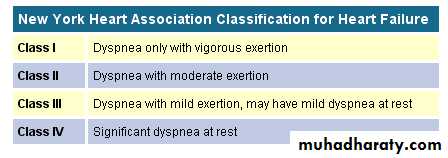
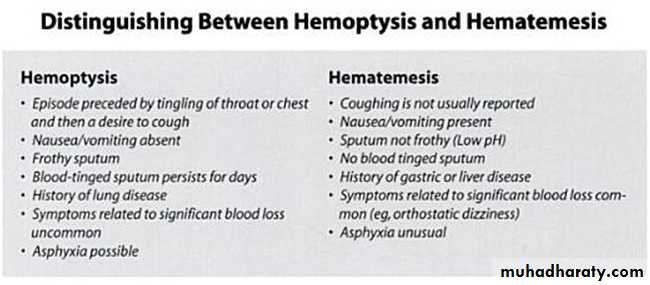
Orthopnea
This early symptom of heart failure may be defined as dyspnea that develops in the recumbent position and is relieved with elevation of the head with pillows. As in the case of exertional dyspnea, the change in the number of pillows required is important.In the recumbent position, decreased pooling of blood in the lower extremities and abdomen occurs. Blood is displaced from the extrathoracic to the thoracic compartment.
The failing LV, operating on the flat portion of the Frank-Starling curve, cannot accept and pump out the extra volume of blood delivered to it without dilating. As a result, pulmonary venous and capillary pressures rise further, causing interstitial pulmonary edema, reduced pulmonary compliance, increased airway resistance, and dyspnea.
In contrast to orthopnea, which may be relieved by immediately sitting up in bed, paroxysmal nocturnal dyspnea may require 30 minutes or longer in this position for relief. Episodes of this may be so frightening that the patient may be afraid to resume sleeping, even after the symptoms have abated
Orthopnea occurs rapidly, often within a minute or two of recumbency, and develops when the patient is awake. Orthopnea may occur in any condition in which the vital capacity is low.
Marked ascites, whatever its etiology, is an important cause of orthopnea. In advanced LV failure, orthopnea may be so severe that the patient cannot lie down and must sleep sitting up in a chair or slumped over a table.
Cough, particularly during recumbency, may be an "orthopnea equivalent." This nonproductive cough may be caused by pulmonary congestion and is relieved by the treatment of heart failure.
Paroxysmal nocturnal dyspnea
usually occurs at night and is defined as the sudden awakening of the patient, after a couple hours of sleep, with a feeling of severe anxiety, breathlessness, and suffocation. The patient may bolt upright in bed and gasp for breath. Bronchospasm increases ventilatory difficulty and the work of breathing and is a common complicating factor of paroxysmal nocturnal dyspnea. PND more specific for cardiac disease.On chest auscultation, the bronchospasm associated with a heart failure exacerbation can be difficult to distinguish from an acute asthma exacerbation, although other clues from the cardiovascular examination should lead the examiner to the correct diagnosis. Both types of bronchospasm can be present in the same individual.
Acute pulmonary edema
is defined as the sudden increase in pulmonary capillary pressure (usually more than 25 mm Hg) as a result of acute and fulminant left ventricular failure. It is a medical emergency and has a very dramatic clinical presentation. Patient appears extremely ill, poorly perfused, restless, sweaty, with an increased work of breathing and using respiratory accessory muscles, tachypneic, tachycardic, hypoxic and coughing with frothy sputum that on occasion is blood tinged.• Poor technique will fail to elicit signs
• or will produce false results.Dyspnea
• Heart Failure• Ischemic heart disease (anginal equivalent)
• Pulmonary Embolism
• Lung Disease including COPD & Asthma
• Severe Anemia
Icterus - Yellow discoloration of the sclera.
Jaundice - Yellow discoloration of the skin.Eastchester Clapping Sign: A Novel Test of Parietal Neglect
The authors describe what happens when patients with parietal neglect are asked to clap. They clap their functioning hand against the air, stopping at the midline as if meeting the other hand there. Patients without neglect reach across the midline to clap against the paralyzed or neglected hand. The test is called the Eastchester Clapping Sign (ECS) to acknowledge that Eastchester High School students originally raised the issue in a psychology class.Journal Watch Neurology January 12, 2010
The authors tested the sign in 14 patients with hemispatial neglect who were admitted to a stroke service and evaluated for acute stroke. Twelve patients tested positive for the ECS and had new right-hemisphere strokes involving the parietal lobe; one patient tested positive after bleeding into a right-hemisphere infarct; and one patient with a parietal perfusion deficit without infarct tested positive periodically as her blood pressure fluctuated.
The authors suggest that using this rapid screening test in the acute setting may allow more nondominant acute strokes to be diagnosed and may correct the current imbalance in the numbers of patients with dominant versus nondominant hemispheric infarctions who receive tissue plasminogen activator (t-PA) treatment.
Comment: The Eastchester Clapping Sign is a quick, easy bedside test with a clear endpoint. The article contains no observations regarding a possible correlation with any of the myriad other parietal tests. Therefore, the proposition that this test will allow more use of t-PA in nondominant-hemisphere infarctions remains speculative. Nor does the small number of cases allow comment about the several anatomical sites associated with neglect phenomena. Nevertheless, the test is very appealing. I predict it will be widely used, so answers to these questions will be forthcoming.
The liver receives 80% of its blood supply via the hepatic artery and 20% via the portal vein, which drains blood from the gut via the splanchnic circulation. The normal portal venous pressure is 2-5 mmHg and is determined by the portal blood flow and portal vascular resistance. When portal venous pressure rises above 12 mm, portal hypertension is said to be present.
Ulcers arterial ulcers tend to be on the borders / sides of the foot, neuropathic ulcers on the plantar surface of the foot, venous ulcers tend on be on the medial aspect of the leg superior to the medial malleolus.
Capillary refill should be less than 3 seconds.
Buerger's Test (assessment of arterial sufficiency(
With the patient supine, note the colour of the feet soles. They should be pink. Then elevate both legs to 45 degrees for more than 1 minute. Observe the soles. If there is marked pallor (whiteness), ischemia should be suspected. Next check for rubor on dependency. Sit the patient upright and observe the feet. In normal patients, the feet quickly turn pink. If, more slowly, they turn red like a cooked lobster, suspect ischemia.The timing of the appearance of jaundice in neonate helps with the diagnosis. Jaundice appearing in the first 24 hours is quite serious and usually requires immediate treatment. When jaundice appears on the second or third day, it is usually "physiologic." However, it can be a more serious type of jaundice. When jaundice appears on the third day to the first week, it may be due to an infection. Later appearance of jaundice, in the second week, is often related to breast milk feedings, but may have other causes.
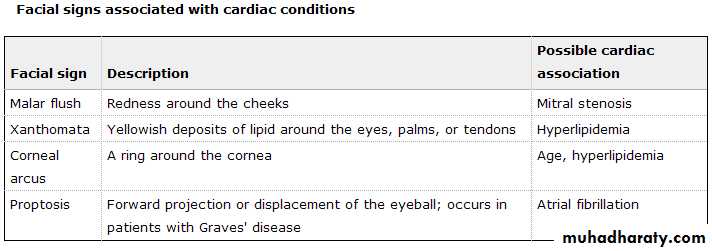
• Look in the eyes for any signs of jaundice (particularly beneath the upper eyelid), anaemia (beneath the lower eyelid) and corneal arcus. You should also look around the eye for any xanthelasma.
A thrill is a palpable murmur whereas a heave is a sign of ventricular hypertrophy.
A thrill feels like avibration and a heave feels like an abnormally large beating of the heart. Feel for these all over the praecordium.Because urine can darken from hyperbilirubinemia before jaundice is visible, the onset of dark urine indicates the onset of hyperbilirubinemia more accurately than the onset of jaundice
In cases of isolated elevation of alkaline phosphatase, γ‑glutamyl transpeptidase (GGT) should be obtained; levels are elevated in hepatobiliary disease but not if the high alkaline phosphatase level is due to a bone disorder.
The liver receives a dual blood supply consisting of the hepatic portal vein and hepatic arteries.
Supplying approximately 75% of the liver's blood supply, the hepatic portal vein carries venous blood drained from the spleen, gastrointestinal tract, and its associated organs.
The hepatic arteries supply arterial blood to the liver, accounting for the remainder of its blood flow. Oxygen is provided from both sources; approximately half of the liver's oxygen demand is met by the hepatic portal vein, and half is met by the hepatic arteries.Blood flows through the sinusoids and empties into the central vein of each lobule. The central veins coalesce into hepatic veins, which leave the liver and empty into the inferior vena cava.
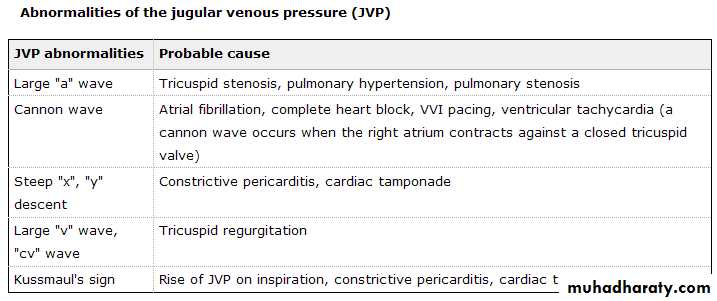
The JVP
The first beat represents that atrial contraction (a) andThe second beat represents venous filling of the right atrium against a closed tricuspid valve (v) and not the commonly mistaken 'ventricular contraction'.
The paradoxical increase of the JVP with inspiration (instead of the expected decrease) is referred to as the
Kussmaul's sign and indicates impaired filling of the right ventricle. The differential diagnosis :
• Constrictive pericarditis
• Restrictive cardiomyopathy
• Pericardial effusion or tamponade
• severe right-sided heart failure
• Tricuspid stenosis
• Cardiac tumors
• Causes of an absent knee and ankle reflex with extensor plantars ((upper and lower motor neurone lesion)): 1. subacute combined degeneration of the spinal cord 2. motor neurone disease 3. syphilitic tabo-paresis 4. Friedreich's ataxi5. conus medullaris or cauda equina lesion - at the conus medullaris the spinal root entry zones and the pyramidal tracts are in close proximity - they may be damaged by a small lesion such as a neurofibroma 6. multiple sclerosis - involvement of the corticospinal tract leads to hyperreflexia and extensor plantars. sensory involvement break the reflex arc, the reflexes disappear 7. pellagra 8. diabetes mellitus + cervical myelopathy
• 9. spinal cord compresion at the 3rd and 4th lumber levels
Delayed relaxation phase of deep tendon reflexes
Differential Diagnosishypothyroidism
neurosyphilis
parkinsonism
pernicious anemia
sarcoidosis, myasthenia gravis
schizophrenia
diabetes mellitus
glucose administration
sprue
medications (propranolol, procainamide, reserpine, potassium), hypothermia, leg edema, normal puerperium, female sex, age
The diagnosis of SLE is based on the past or present appearance of 4 out of 11 criteria.
anemia, leukopenia, lymphopenia, or thrombocytopenia, a positive test for antinuclear antibodies (ANA),
serositis (eg, pleural effusion or pericarditis),
arthritis, malar rash,
immunologic disorder (eg, positive antidouble-stranded DNA titers, positive antiSmith antibody test, positive antiphospholipid antibody test, or false-positive syphilis [VEDRL] titer)
discoid rash, photosensitivity, oral ulcers, renal disease, and neurologic disorders. Generalized lymphadenopathy has been described, but this finding cannot be employed to confirm a diagnosis of SLE.
The hallmark of SLE is autoantibody production against self-antigens, particularly DNA, as well as other nuclear antigens, ribosomes, platelets, coagulation factors, immunoglobulin, erythrocytes, and leukocytes. Elevated levels of immunoglobulin, particularly antidouble-stranded DNA antibodies, are associated with circulating and tissue-bound immune complexes. Hypergammaglobulinemia, decreased C3 and C4 levels, and an elevated ESR are all findings that may be seen in SLE, but they are nonspecific and may be found in a number of rheumatologic disorders.
Hyporeflexia is a common clinical sign in patients with hypercalcaemia.
NSAIDs should not be prescribed in patients with hypercalcaemia as they reduce renal blood flow thus inhibiting urinary calcium excretion.Bisphosphonates inhibit bone resorption by osteoclasts, and are the first line pharmacological treatment of hypercalcaemia of malignancy; calcitonin use is limited by its association with anaphylaxis.
Electrocardiogram changes in hypercalcaemia include bradycardia, prolonged PR interval, short QT interval, widened T waves and arrhythmias.
Pulsus paradoxus
decreased right heart functional reserve, e.g. myocardial infarction and tamponade.right ventricular inflow or outflow obstruction, e.g. superior vena cava obstruction and pulmonary
embolism, and decreased blood to the left heart due to lung hyperinflation (e.g. asthma, COPD)
and anaphylactic shock.
List of causes
Cardiac:
cardiac tamponade
pericardial effusion
pulmonary embolism
cardiogenic shock
Pulmonary:
tension pneumothorax
asthma
Non-pulmonary and non-cardiac:
anaphylactic shock
superior vena cava obstruction
Exposure to sunlight aggravates
pellagra, Hartnup's disease, lupus erythematosus, Darier's disease, rosacea, scleroderma, actinic lichen planus, and lymphocytoma.
Erythema nodusum
INFECTIONS:bacteria: Streptococci, leptospirosis, cat-scratch disease, psittacosis, yersinia. viruses: EBV.OTHER: TB, tularaemia, histoplasmosis, coccidiodomycosis.Toxoplasmosis
DRUGS:
sulphonamides, oral contraceptive pill. bromides
SYSTEMIC DISEASES:
SLE, vasculitis, regional enteritis, ulcerative colitis, Behçet Syndrome. lepromatous form of leprosy . sarcoidosis
Potential causes of erythema multiforme include:
INFECTIONS:viruses: herpes simplex 1 and 2, hepatitis B, EBV, enteroviruses.
small-agents: mycoplasma pneumoniae.
bacteria: Group A Streptococcus, eosinia.
other: mycobacterium TB, histoplasma, coccidioides.
NEOPLASIA:
Leukaemia, lymphoma.
ANTIBIOTICS:
penicillins, sulphonamides, isoniazid, tetracycline.
ANTICONVULSANTS:
phenytoin, phenobarbitone, carbamazepine.
OTHER:
aspirin, radiation, etoposide, NSAIDs, sunlight, pregnancy.
Increased skin fragility is seen in a number of disorders and is used as a clinical test in bullous disorders (Nikolsky's sign) epidermolysis bullosa . Other causes include Pemphigus vulgaris, porphyria cutania tarda and drug reactions (especially pseudoporphyria). Other causes of increased skin fragility (not associated with bullae) include long term corticosteroid therapy, Ehlers-Danlos syndrome and Scurvey (vitamin C deficiency ).
Nikolsky's sign
Nikolsky's sign is part of the clinical evaluation of bullous skin disorders.
If a bulla extends laterally with pressure it suggests that the epidermis detaches from the
skin. Or on normal skin a palpable separation (bulla) may be produced.
Positive in pemphigus vulgaris, staphylococcal scalded skin syndrome, acute
Generalized exanthematous pustulosis (drug reaction), drug-induced pemphigoid (NOT
Idiopathic pemphigoid) and toxic epidermal necrolysis.
• Rib-notching on chest x ray
• Due to neurofibromas of intercostal nerves.Cotton-wool spots are tiny white areas on the retina, the layer of light-sensing cells lining the back of the eye. Caused by a lack of blood flow to the small retinal blood vessels, they usually disappear without treatment and do not threaten vision. They can, however, be an indication of a serious medical condition.
yellow flecks are called hard exudates.
• Diabetes and hypertension are the most common causes of cotton-wool spots. The presence of more than eight cotton-wool spots has been associated with a higher risk of the more severe form of diabetic retinopathy known as proliferative diabetic retinopathy. …
Cotton-wool spots
• Cotton-wool spots are also a common sign of (HIV). infection . They are present in more than half of the people with full-blown AIDS. Their presence can be an important sign of the severity of HIV-related disease,
• central retinal vessel occlusion .
• Also seen in vasculitis (SLE scleroderma…). leukemia, syphilis, pancreatitis ,trauma.etc
Hard exudates ( yellow flecks )
chronic vascular leakage :
Diabetic retinopathy
Hypertensive retinopathy
Coat's disease
Capillary hemangioma of the retina
Choroidal neovascularization
Retinal arterial macroaneurysm
Mechanism:
Increased vascular permeability allowing the leakage of fluid and
lipoprotein into the retina resulting in thickening of the macula
Resorption of the edema commonly results in precipitation of lipid
residues within the outer plexiform (Henle's) layer
Clinical features:
Symptoms: various degree of decreased vision if involving the
macula
Signs:
Discrete white-yellow lipid deposits in the posterior pole
Commonly seen in a circinate pattern peripheral to the areas of leakage
May present as large, confluent exudation
Macular star and/or circumpapillary hard exudates can be seen in Leber's stellate neuro-retinitis or end-stage hypertensive retinopathy
Management: treat the underlying diseases.
Yellow flecks
are called hard exudates. They are the lipid residues of serous leakage from damaged capillaries. The commonest cause is diabetes. Other causes are retinal vein occlusion, angiomas (Von Hippel-Lindau Disease), other vascular dysplasias, and radiation-induced retinal vasculopathy.Cotton wool spots. caused by retinal nerve fiber layer microinfarcts. Exploded retinal ganglion cell axons extrude their axoplasm like toothpaste. Expect to find cotton wool spots arrayed around the optic disc and along the temporal vascular arcades.
Cotton wool spots have a myriad of causes. Any process that occludes small retinal arterioles will do this: hypertension, diabetes, HIV, severe anemia or thrombocytopenia, hypercoagulable states, connective tissue disorders, viruses, lues, Behçet's and many others.
•
Bronchophony and whispered pectoriloquy occur when the patient's spoken or whispered voice is clearly transmitted through the chest wall. Voice transmission results from alveolar consolidation, as occurs with pneumonia.
Egophony is said to occur when a patient says the letter “E” and the examiner hears the letter “A” on auscultation, as occurs with pneumonia.
Small pupils
Horner's syndromeold age
pontine haemorrhage
Argyll Robertson pupil
drugs
poisons (opiates, organophosphates).
dilated pupils
Holmes-Adie (myotonic) pupil
third nerve palsy
drugs
poisons (atropine, CO, ethylene glycol).
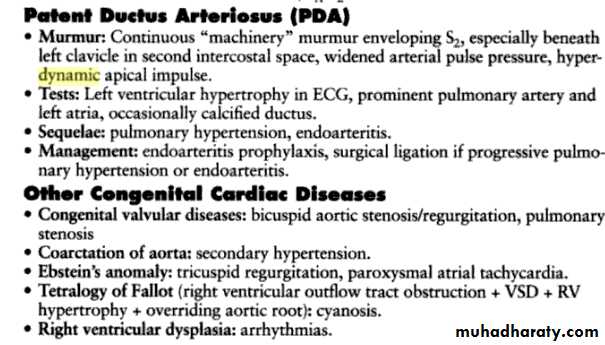
In adults who were born with a large left-to-right shunt through the ductus arteriosus, pulmonary vascular obstruction (Eisenmenger syndrome) with pulmonary hypertension, right-to-left shunting, and cyanosis have usually developed. Severe pulmonary vascular disease results in reversal of flow through the ductus; unoxygenated blood is shunted to the descending aorta;
and the toes, but not the fingers, become cyanotic and clubbed, a finding termed differential cyanosis.
The leading causes of death in adults with patent ductus are cardiac failure and infective endocarditis; occasionally severe pulmonary vascular obstruction may cause aneurysmal dilatation, calcification, and rupture of the ductus. Clubbing of toes but not fingers is also seen in coarctation of the aorta.
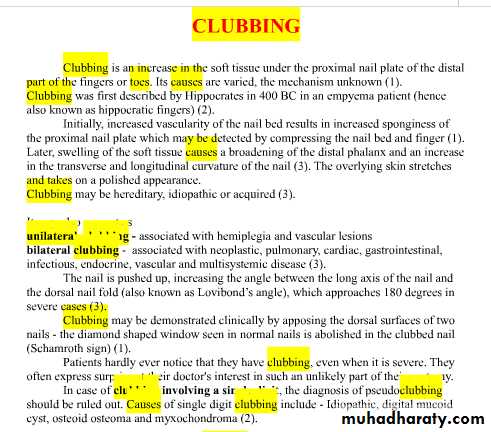
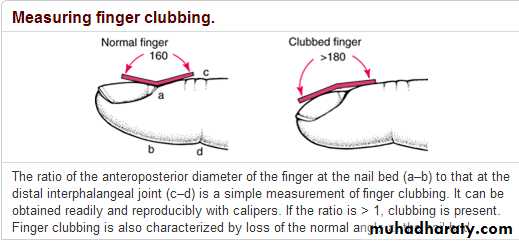
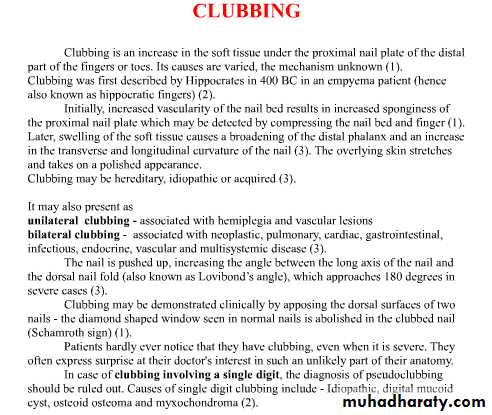
Pseudo-clubbing
overcurvature of the nails in both the longitudinal and transverse axes, with preservation of a normal Lovibond angle. may be seen in :• chronic renal failure
• Hyperparathyroidism
• sarcoidosis.
Clubbing is potentially reversible if the underlying condition is treated early enough but the changes may be irreversible once collagen deposition has set in.
Acropachy is an alternative term for clubbing.
As clubbing progresses, the angle between the nail and the nail base (called the Lovibond angle) becomes obliterated. Normally, the angle is less than or equal to 160°. With increasing convexity of the nail, the angle becomes greater than 180°. In early clubbing, the nail may feel springy instead of firm when palpated and the skin at the base of the nail may become smooth and shiny. In individuals without clubbing, if two opposing fingers are placed together, a diamond-shaped window will appear. In clubbing, this window is obliterated and the distal angle formed by the two nails becomes wider. This is known as Schamroth's window test.
Imaging
This is not usually required to diagnose clubbing but plain radiographs of the digits may help to elucidate the cause. Osteolysis is often seen in patients with congenital cyanotic heart disease, whilst bone hypertrophy suggests a pulmonary condition. CT and MRI scanning of other areas may be required to assist in diagnosing the underlying primary cause.Unidigital clubbing is seen following median nerve injury and, rarely, with sarcoidosis.
Unidigital clubbing is seen following median nerve injury and, rarely, with sarcoidosis.
Recurrent clubbing may occur during pregnancy in otherwise healthy women.Familial clubbing is of no clinical import (unless associated with pachydermoperiostosis).
Inhibitors of cytochrome CYP3A, including:
DiltiazemVerapamil
Ketoconazole and other azole antifungals
Macrolide
Ritonavir (Norvir)
Grapefruit products or grapefruit juice Chronic alcohol excess induces hepatic enzymes. However, acute intake exerts an inhibitory effect
Cytochrome P450 isoenzymeCYP 3A4
Strong inhibitors
itraconazole, ritonavir, clarithromycin)
Mild–moderate inhibitors
Erythromycin,diltiazem,verapamil,fluconazole.
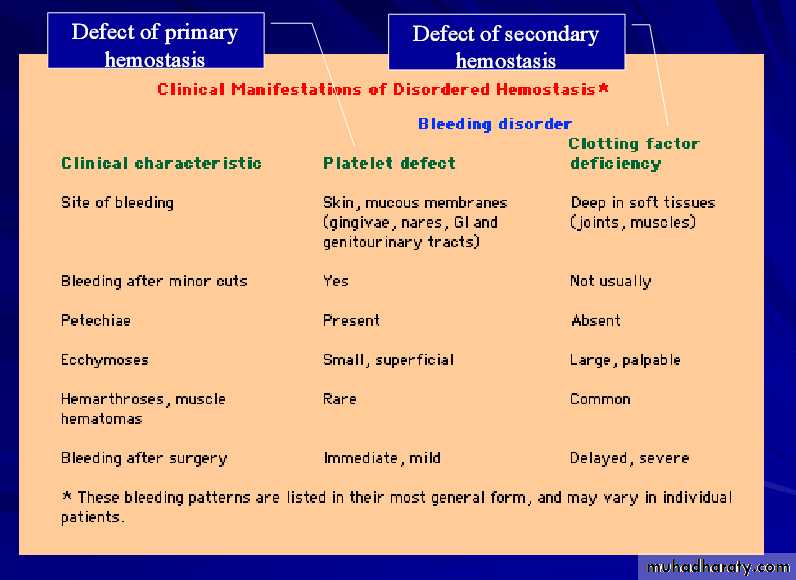
Purpura (from the Latin, purpura, meaning "purple") is the appearance of red or purple discolorations on the skin that do not blanch. caused by bleeding underneath the skin. measure 0.3-1 cm, whereas petechiae measure less than 3 mm, and ecchymoses greater than 1 cm. This is common with typhus and can be present with meningitis caused by meningococcal meningitis or septicaemia. In particular, meningococcus, a Gram-negative diplococci organism, releases endotoxin when it lyses. Endotoxin activates the Hageman factor (clotting factor XII), which causes disseminated intravascular coagulation. The DIC is what appears as a rash on the affected individual.
• Platelet disorders
• ITP• Secondary thrombocytopenic purpura
• Post-transfusion purpura
• Vascular disorders
• Microvascular injury, as seen in senile (old age) purpura, when blood vessels are more easily damaged
• Hypertensive states
• Deficient vascular support
• Vasculitis, as in the case of Henoch-schӧnlein purpura
• Coagulation disorders
• DIC
• Scurvy (vitamin C deficiency) - defect in collagen synthesis due to lack of hydroxylation of procollagen. It results in weakened capillary walls.
A petechia is a small (1-2mm) red or purple spot on the body, caused by a minor hemorrhage (broken capillaries).The most common cause of petechiae is through physical trauma such as a hard bout of coughing, vomiting or crying, which can result in facial petechiae, especially around the eyes. Petechiae in this instance are completely harmless and usually disappear within a few days. Petechiae may be a sign of thrombocytopenia when platelet function is inhibited (e.g., as a side effect of medications or during certain infections), or in clotting factor deficiencies.They may also occur when excessive pressure is applied to tissue (e.g., when a tourniquet is applied to an extremity or with excessive coughing).
Infections
• hemorrhagic fever• Cerebral malaria
• Congenital syphilis
• Dengue fever
• Ebola
• Endocarditis
• H1N1
• Infectious mononucleosis
• Rocky mountain spotted fever
• Scarlet fever
• Typhus
Non-infectious conditions
• Hypocalcemia• Idiopathic thrombocytopenic purpura
• Leukemia
• Aplastic anaemia
• Childhood protein-energy malnutrition such as Kwashiorkor or Marasmus
• Erythroblastosis fetalis
• Henoch-Schönlein purpura
• Kawasaki disease
Causes of petechia
A bruise, also called a contusion, is a type of relatively minor hematoma of tissue in which capillaries and sometimes venules are damaged by trauma, allowing blood to seep into the surrounding extracellular space. Bruises can involve capillaries at the level of skin, subcutaneous tissue, muscle, or bone. Bruises may be referred to by size as ecchymosis (1-3 cm), purpura (3-10 mm), or petechia (<3 mm), although these terms can also refer to internal bleeding not caused by trauma.
larger bruises may change color due to the breakdown of hemoglobin from within escaped red blood cells in the extracellular space. The striking colors of a bruise are caused by the phagocytosis and sequential degradation of hemoglobin to biliverdin to bilirubin to hemosiderin, with hemoglobin itself producing a red-blue color, biliverdin producing a green color, bilirubin producing a yellow color, and hemosiderin producing a golden-brown color.
Blood pressure measurement in the legs
cuff, applied at the midthigh, and by listening over the popliteal artery. If possible, the patient should be in a prone position. The bladder of the cuff should be about 40% of the circumference of the thigh, and the length should be about 75% to 80% of this circumference. Normally, the systolic blood pressure in the legs is usually 10% to 20% higher than the brachial artery pressure.Despite a lack of scientific evidence, it is recommended that patients who have undergone axillary node dissection avoid having blood pressure measurements done on the affected side. For those who have had bilateral axillary node dissection, blood pressure measurements should be obtained in the leg. For those patients who have had a mastectomy without lymph node dissection (ie, prophylactic mastectomy), blood pressure can be obtained in either arm. These recommendations should be followed for life .
The danger of having a blood pressure test on an at-risk arm or an arm affected by lymphedema is that the squeeezing involved can cause possible further damage to already fragile lymphatics and blood vessels. If this occurs, it would cause worsening of the lymphedema.
• Gallop rhythm an auscultatory finding of three (triple r.) or four (quadruple r.) heart sounds; the extra sounds occur in diastole and are related either to atrial contraction ,to early rapid filling of a ventricle ,or to concurrence of both events (summation gallop)
• Gallop rhythms may be heard in young or athletic people, but may also be a sign of serious cardiac problems like heart failure. an abnormal heart rhythm characterized by three clear sounds in each beat, resembling the sound of a horse's gallop. there are two types of gallop rhythm called third and fourth sounds, which may be very close together so that they sound like one sound.
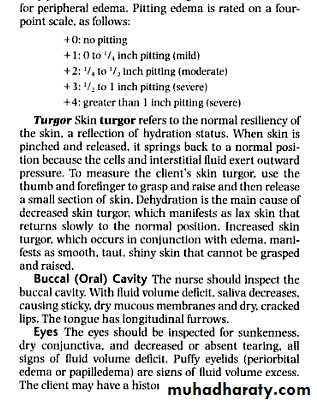
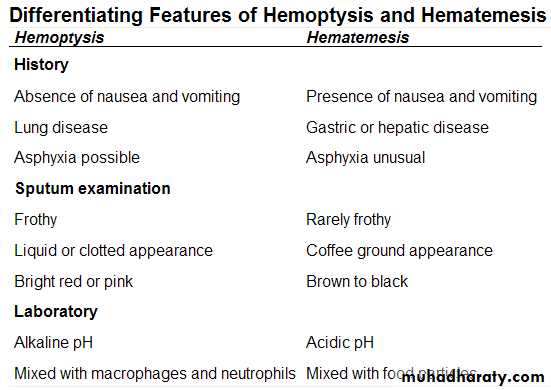
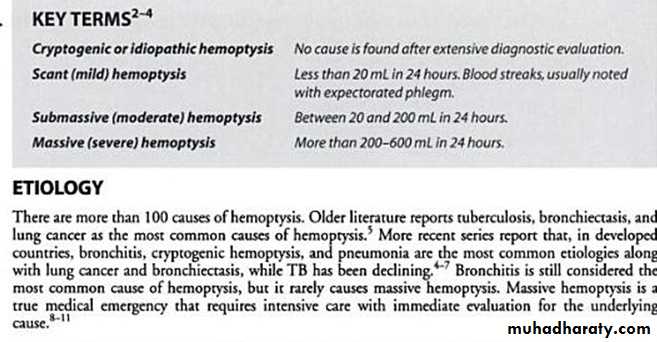
Signs of hemoptysis include:
Any respiratory symptoms, such as a coughBright red blood
Blood that has a liquid or clotted, frothy appearance
Signs of hematemesis include:
A history of excessive alcohol use or liver disease
Any esophogastric symptoms, such as nausea or vomiting Brown or black blood
Blood that looks like coffee grounds
Dark-colored, tar-like stools (melena)
In bleeding from the lungs, on the other hand, there is an excited pulse, the blood-pressure is high, the patient brings up blood when coughing, the blood is bright red in color--rather inclined to be frothy, because the air is mixed with it--and the reaction is alkaline.
Causes of Stretch marks:
PubertyPregnancy
Steroid therapy
Cushing syndrome
Overweight
Rapid weight gain
Diabetes
Sinusoidal hypertension results from compression of the portal venous channels in the fibrotic liver and leads to the development of portosystemic anastomoses. The anastomosis at the gastro-oesophageal junction between the oesophageal branch of the left gastric vein (portal system) and the oesophageal veins of the azygos system (systemic circulation) results in the development of gastro-oesophageal varices.
Other important anastomoses occur at sites where the portal and systemic veins come together:
Rectal varices: anastomoses between the superior (portal) and inferior (systemic) rectal veins.
Umbilical varices: the recanalised umbilical vein in the round ligament (ligamentum teres) drains into the epigastric veins to form dilated varices over the abdominal wall—the caput medusa.
Stomal varices: collaterals can develop at the site of previous surgery, such as around an ileostomy or colostomy.
Between 30% and 60% of patients with cirrhosis will develop varices at some point, and bleeding will occur in 25-50% of them. Factors associated with the risk of variceal bleeding include size of the varix, pressure within the varix, tension in the variceal wall, and the severity of the underlying liver disease. Infection may precipitate bleeding, as may the use of non-steroidal anti-inflammatory drugs.
The main endoscopic treatments
for oesophageal varices are:band ligation or injection sclerotherapy with a sclerosant such as ethanolamine. Band ligation) is the preferred treatment because randomised controlled trials have shown that it is superior to injection sclerotherapy in terms of bleeding control, number of complications, and survival.
Terlipressin, a synthetic analogue of vasopressin, and octreotide, a somatostatin analogue, reduce portal pressure and portal blood flow and effectively control bleeding in acute oesophageal variceal haemorrhage .Terlipressin also improves survival compared with placebo, but it can have ischaemic side effects. Meta-analyses of randomised trials have shown that combining endoscopic treatment with drugs improves bleeding control but does not affect mortality compared with endoscopic treatment alone .
Radiologically placed shunts, such as the transjugular intrahepatic portosystemic stent shunt (TIPSS) are now favoured over surgical procedures. Studies comparing TIPSS with endoscopic treatment show superiority in controlling bleeding but no difference in survival; in addition, the group treated with TIPSS had an increased risk of encephalopathy
The non-selective β blocker propranolol has been shown to reduce azygos blood flow and variceal pressure by causing splanchnic vasoconstriction and reducing cardiac output. A meta-analysis showed a reduction in risk of bleeding with β blockers but minimal improvement in survival. Several randomised studies comparing prophylactic variceal band ligation with β blockade have shown a reduction in bleeding with band ligation, but most studies have failed to show a reduction in mortality.
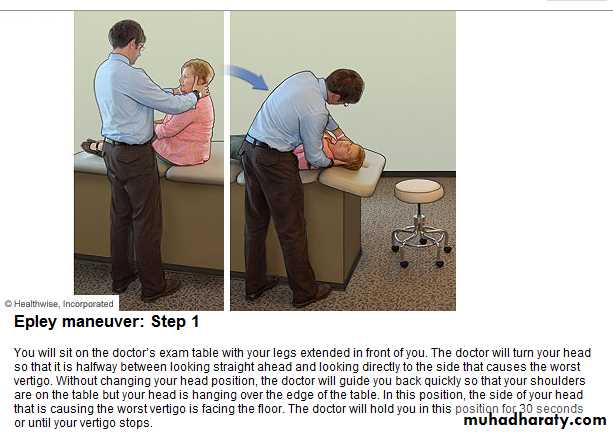
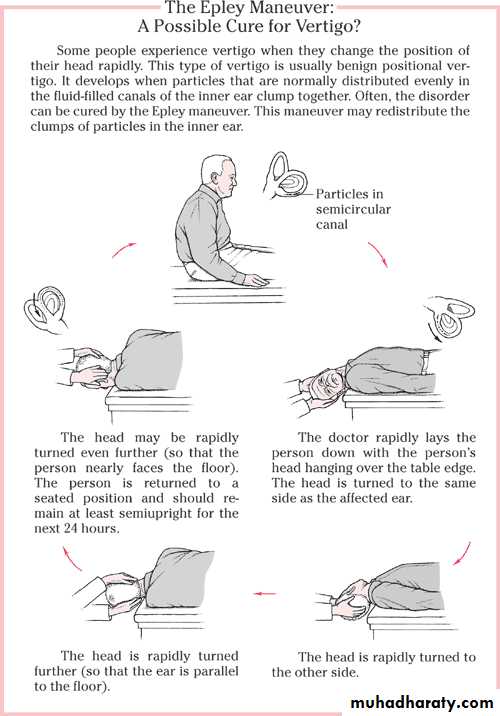
The Epley maneuver should initially be performed by a trained therapist or medical physician; after that, it can be modified and performed at home.Avoid rapid changes in head position that might provoke benign paroxysmal positional vertigo.
It's best to perform the Epley maneuver before going to bed at night.
Prop your head up with a couple of pillows when sleeping until your symptoms have resolved.
Avoid extending your head back on a repeated basis until your symptoms have resolved.
If you experience weakness, headache, numbness or changes in vision immediately discontinue the Epley maneuver and seek medical attention.
The Epley maneuver works for benign paroxysmal positional vertigo only. Therefore the Epley maneuver should be performed at home only after BPPV has been confirmed.
The Epley maneuver is safe and relatively effective when properly performed. Benign paroxysmal positional vertigo can nevertheless recur
Step 1
Begin by sitting upright in the middle of your bed. Rotate your head horizontally towards the ear causing your symptoms approximately 45 degrees(one minute).Step 2
Keep your head and neck at this 45 degree angle and gently lie down. Maintain this position for one minute. This position will likely provoke transient dizziness or vertigo.
Step 3
While still lying flat on your back slowly rotate your head towards your good ear as far as possible or approximately 90 degrees. Maintain this position for one minute, may again provoke transient dizziness or vertigo.
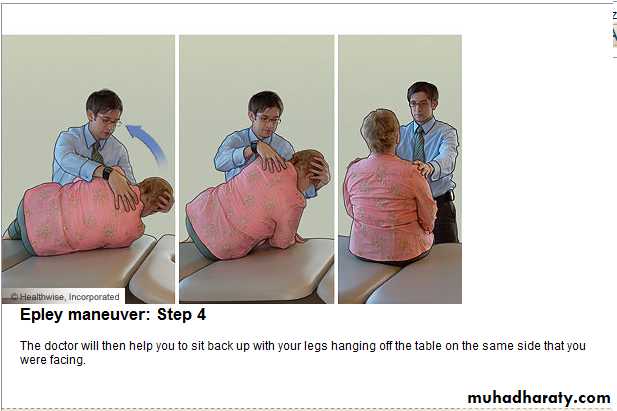
Step 4
With your head still rotated maximally towards your good ear slowly roll your entire body on to your "good side". Keep your head and neck fixed as much as possible. If done properly you should be able to stare down at the floor. Maintain this position for one minute.
Step 5
Finally to complete the Epley maneuver return to a sitting position with your head up but flexed forward approximately 45 degrees. (one minute).
Step 6
Most reference sources state that the Epley maneuver should take five minutes to complete. Three complete cycles should be performed prior to going to bed.
Photosensitive facial eruptions typically affect the nasal bridge, brow, cheeks, and chin, with relative sparing under the brow, chin, and postauricular regions. Phototoxic drug reactions usually have the appearance of sunburn and are limited to sun exposed areas, such as the face, back of hands, and "V" of the neck area. These reactions are common and usually predictable. They can occur in anyone who receives a sufficient amount of a phototoxic drug, together with sufficient exposure to ultraviolet light. The diagnosis can be confirmed by performing monochromator light testing, a specialised form of phototesting.
The ultraviolet spectrum is divided into three parts, which differ depending on the wavelength: ultraviolet A, ultraviolet B ("sunburn" radiation), and ultraviolet C. Only ultraviolet A and B cause photosensitivity reactions because ultraviolet C is blocked by the atmospheric ozone. Light interacting directly with the drug (or its metabolite) in the skin generates reactive oxygen species, which can lead to substantial chemical activity and damage to surrounding tissue
Common drugs that cause photoallergic reactions
DoxycyclineThiazide
Sulphonamides
Sulphonylureas
phenothiazines.
Less common triggers include quinine, quinidine, tricyclic antidepressants, antimalarials, and non-steroidal anti-inflammatory drugs.
Causes of Gum hypertrophy:
The following medical conditions are some of the possible causes of Gum hypertrophy. There are likely to be other possible causes, so ask your doctor about your symptoms. Infection
Viruses
Bacteria
Fungi
Dental disease
Poor dental hygiene
Drugs eg. phenytoin, nifedipine, cyclosporin
The number of conditions causing focal or diffuse swelling of the gums is far out of proportion to the size of this organ and the fact that physicians frequently pay little attention to it unless the patient mentions it. The best approach is to apply the mnemonic VINDICATE to the gums and the list of possible causes will quickly come to mind. Vascular.Inflammatory. Neoplasms. Deficiency . Intoxication. Congenital. Autoimmune.Trauma . Endocrine
V—Vascular disorders are not a significant cause of swollen gums.
I—Inflammatory lesions include gingivitis, whether viral (aphthous stomatitis), fusospirochetal (“trench mouth”), or to monilial. Focal abscesses of the gums are common. Alveolar abscesses also cause focal swelling of the gums.N—Neoplasms remind one of monocytic leukemia and multiple myeloma, which are associated with diffuse hypertrophy and local tumors such as a sarcoma, papilloma, odontoma, and squamous cell carcinoma.
D—Deficiency diseases include scurvy and most vitamin deficiencies.
I—Intoxication suggests the common diffuse hyperplasia in patients with epilepsy taking diphenylhydantoin and related drugs, including barbiturates.C—Congenital or acquired malformations remind one of the gingivitis secondary to malocclusion, poor-fitting crowns or orthodontal appliances, and periodontal cysts, secondary to chronic periapical granuloma.
A—Autoimmune and allergic diseases include the hypertrophy of thrombocytopenic purpura and the contact gingivitis from dentures, mouthwashes, and toothpastes.
T—Trauma to the gums may cause local hematomas and fractures.
E—Endocrine disorders suggest several conditions that may cause gum hypertrophy. Gingival hyperplasia in pregnancy, the giant cell granulomas of hyperparathyroidism, juvenile hypothyroidism, pituitary dysfunction, and diabetes mellitus are the most important
Causes of Hirsutism
• Hirsutism is a condition with excess growth of hair in a male pattern. This male pattern of hair distribution indicates growth of hair in places like chest, areola, face, lower abdomen, upper back, lower back, buttocks, inner thighs and external genitalia. It is generally caused by excess male sex hormone - androgens, and the causes of hirsutism include any condition which increases the blood level of androgens.
• The causes of hirsutism can be broadly classified in to five categories:
• Hormone system related• Tumor related
• Drugs
• Miscellaneous
• Unknown
Although the terms hirsutism and hypertrichosis often are used interchangeably, hypertrichosis actually refers to excess hair (terminal or vellus) in areas that are not predominantly androgen dependent.
The exact mode of action of drugs on hair follicles is not known, but the same mechanisms do not appear to be involved in all patients.
Drug-induced hirsutism can be distinguished from drug-induced hypertrichosis, in which a uniform growth of fine hair appears over extensive areas of the trunk, hands, and face and is unrelated to androgen-dependent hair growth
• Cushing's syndrome - defined as excess secretion of steroids including androgens
• Congenital adrenal hyperplasia - An enzyme deficiency leading to excess production of androgen• Acromegaly - Excess growth hormone and insulin resistance
• Hyperprolactinemia
• Hypothyroidism
• Polycystic ovarian disease - ovarian disease with multiple cysts and increased blood androgen levels
• Obesity
Hormone system related causes of hirsutism
Tumor related causes of hirsutism:
• Ovarian tumors
• Arrhenoblastoma
• Gonadoblastomas
• Lipoid cell tumors
• Dysgerminoma
• Brenner's tumor
• Granulosa -theca cell tumors
• Adrenal tumors, adenoma, carcinoma
Miscellaneous causes of hirsutismCauses of hirsutism under this category include:Syndromes of excessive insulin resistance
Functional adrenal hyperandrogenism
Hypereactio luteinalis of pregnancy - transient increase in androgen levels during pregnancy
Thecoma of pregnancy - Transient androgen secreting tumor during pregnancy
True hermaphroditism - condition where both male and female internal sex organs are present
Unknown causes of hirsutism:
The affected person is healthy till puberty and thereafter develops hirsutism. In this category the hirsutism is usually familial. There will be an associated obesity and insulin resistance. Some of the patients in this category have normal blood androgen levels. In these patients the cause of hirsutism is increased sensitivity of the body to normal androgens• minoxidil
• Phenytoin• Cyclosporine
• Diazoxide
• Androgens
• Oral contraceptives - containing progesterone
• Penicillamine
• Heavy metals
• Acetazolamide
Drug-induced hirsutism
Drugs that can induce hirsutism by their inherent androgenic effects include dehydroepiandrosterone sulfate (DHEA-S), testosterone, danazol, and anabolic steroids. Currently used low-dose oral contraceptives are less likely to cause hirsutism than were previous formulations.
Drugs such as phenytoin, minoxidil, diazoxide, cyclosporine, streptomycin, psoralen, penicillamine, high-dose corticosteroids, metyrapone, phenothiazines, acetazolamide, and hexachlorobenzene presumably exert their effects independently of androgens..
.
Alcohol-induced pseudo-Cushing syndrome
Cushing's syndrome
Diabetes
Marfan syndrome
Obesity
Overweight
Pregnancy
Puberty
Rapid weight gain
Steroid therapy
Striae gravidarum
Stretch marks (striae) are pink, reddish or purplish indented streaks that often appear on the abdomen, breasts, upper arms, buttocks and thighs. Stretch marks are very common in pregnant women, especially during the last half of pregnancy
They represent linear dermal scars accompanied by epidermal atrophy.
4 types of exercise contractions
There are many types of exercise to choose from which all have their own benefits. What's common among all is they require some form of muscular contraction. There are four different types of muscle contraction.
• Isotonic
• Eccentric
• Isometric
• Isokinetic
Isotonic
All lifting exercises require Isotonic contractions. This happens when the muscle shortens as it contracts. An example of isotonic contraction can be seen when we flex the bicep muscle. Stand with one arm straight and the palm of the hand facing up. Roughly measure the length from the start of the biceps muscle to the point where it meets the shoulder. Now curl the hand towards the shoulder, the biceps muscle shortens as it contracts. When you reach the end point take another rough measurement of the biceps again, it will be much shorter.Another example are the triceps muscle (opposite of biceps). Do the same experiment again this time measure the triceps and start at the curled position. The triceps shortens as the arm straightens.
Other examples are....
lifting objects above the head - front shoulder (anterior deltoid) shortenslifting object up from lying position - chest muscle shortens
lifting body up from squat position - quadriceps muscle shortens as legs extend
doing a sit up
throwing a ball
swinging a bat
In fact, Isotonic contractions are the most common, many exercises and activities involve this type of contraction.
Eccentric
Eccentric contraction is the opposite of isotonic, the muscle lengthens as it gains tension. These are much less common and not as beneficial as the common Isotonic. An example is when someone manages to pull your arm straight while at the same time you are try to keep the arm locked in one position. In other words, the load is too great!
Other examples are...
running downhill
walking downstairs
landing on the ground from a jump
This type of contraction is not always recommended!
Isometric
An Isometric contraction occurs when there is tension on a muscle but no movement is made causing the length of the muscle to remain the same. This type of contraction is also referred to as a static contraction. Some bodybuilders make up their own exercises using Isometric contraction in order to develop strength, an example is when someone attempts to curl one arm upwards but is held by using equal resistance from the other arm.• attempting to lift an immoveable object
• holding a weight at arm's length
• some wrestling movements
The above examples are advanced forms of exercise and should not be attempted when losing weight
Isokinetic
Similar to the Isotonic contraction, the Isokinetic contraction causes the muscle to shorten as it gains tension. The difference is Isokinetic requires a constant speed over the entire range of motion, therefore this type of contraction require special equipment to exercise properly. An example is an arm stroke when swimming, the even resistance from the water offers a constant speed at maximal contrationsThe third heart sound is benign in youth and some trained athletes, but if it re-emerges later in life it may signal cardiac problems like a failing left ventricle as in dilated congestive heart failure (CHF). S3 is thought to be caused by the oscillation of blood back and forth between the walls of the ventricles initiated by inrushing blood from the atria. The reason the third heart sound does not occur until the middle third of diastole is probably because during the early part of diastole, the ventricles are not filled sufficiently to create enough tension for reverberation. It may also be a result of tensing of the chordae tendineae during rapid filling and expansion of the ventricle.
In other words, an S3 heart sound indicates increased volume of blood within the ventricle. A left-sided S3 is best heard in the left lateral decubitus position and at the apex of the heart, which is normally located in the 5th left intercostal space at the midclavicular line. A right-sided S3 is best heard at the lower-left sternal border. The way to distinguish between a left and right-sided S3 is to observe whether it increases in intensity with inspiration or expiration. A right-sided S3 will increase on inspiration whereas a left-sided S3 will increase on expiration.
S4 is caused by the atria contracting forcefully in an effort to overcome an abnormally stiff or hypertrophic ventricle. The S4 heart sound is associated with any process that increases the stiffness of the ventricle, including:
hypertrophy of the ventricle
long-standing hypertension
aortic stenosis causes ventricular hypertrophy
fibrosis of the ventricle (eg. post-MI)
Congestive Heart Failure
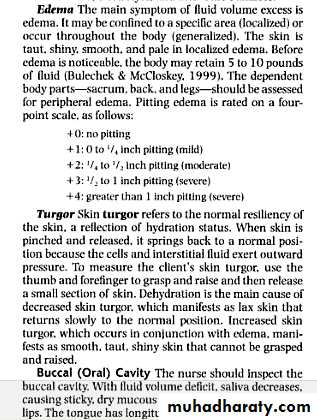
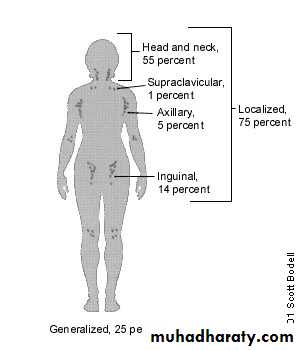
lymph nodes greater than 1 cm in diameter are considered to be abnormal. Supraclavicular nodes are the most worrisome for malignancy. A three- to four-week period of observation is prudent in patients with localized nodes and a benign clinical picture. Generalized adenopathy should always prompt further clinical investigation. When a node biopsy is indicated, excisional biopsy of the most abnormal node will best enable the pathologist to determine a diagnosis.
The body has approximately 600 lymph nodes, but only those in the submandibular, axillary or inguinal regions may normally be palpable in healthy people. Lymphadenopathy refers to nodes that are abnormal in either size, consistency or number. There are various classifications of lymphadenopathy, but a simple and clinically useful system is to classify lymphadenopathy as "generalized" if lymph nodes are enlarged in two or more noncontiguous areas or "localized" if only one area is involved.
Distinguishing between localized and generalized lymphadenopathy is important in formulating a differential diagnosis. In primary care patients with unexplained lymphadenopathy, approximately
three fourths of patients will present with localized lymphadenopathy and one fourth with generalized lymphadenopathy
Medications That May Cause Lymphadenopathy
Allopurinol (Zyloprim) Atenolol (Tenormin) Captopril (Capozide) Carbamazepine (Tegretol) Cephalosporins Gold Hydralazine (Apresoline)
Penicillin Phenytoin (Dilantin) Primidone (Mysoline) Pyrimethamine (Daraprim) Quinidine Sulfonamides Sulindac (Clinoril)
Adapted with permission
Lymph Node Groups: Location, Lymphatic Drainage and Selected Differential Diagnosis
LocationLymphatic drainage
Causes
Submandibular
Tongue, submaxillary gland, lips and mouth, conjunctivae
Infections of head, neck, sinuses, ears, eyes, scalp, pharynx
Submental
Lower lip, floor of mouth, tip of tongue, skin of cheek
Mononucleosis syndromes, Epstein-Barr virus, cytomegalovirus, toxoplasmosis
Jugular
Tongue, tonsil, pinna, parotid
Pharyngitis organisms, rubella
Posterior cervical
Scalp and neck, skin of arms and pectorals, thorax, cervical and axillary nodes
Tuberculosis, lymphoma, head and neck malignancy
Suboccipital
Scalp and head
Local infection
Postauricular
External auditory meatus, pinna, scalp
Local infection
Preauricular
Eyelids and conjunctivae, temporal region, pinna
External auditory canal
Right supraclavicular node
Mediastinum, lungs, esophagus
Lung, retroperitoneal or gastrointestinal cancer
Left supraclavicular node
Thorax, abdomen via thoracic duct
Lymphoma, thoracic or retroperitoneal cancer, bacterial or fungal infection
Axillary
Arm, thoracic wall, breast
Infections, cat-scratch disease, lymphoma, breast cancer, silicone implants, brucellosis, melanoma
Epitrochlear
Ulnar aspect of forearm and hand
Infections, lymphoma, sarcoidosis, tularemia, secondary syphilis
Inguinal
Penis, scrotum, vulva, vagina, perineum, gluteal region, lower abdominal wall, lower anal canal
Infections of the leg or foot, STDs (e.g., herpes simplex virus, gonococcal infection, syphilis, chancroid, granuloma inguinale, lymphogranuloma venereum), lymphoma, pelvic malignancy, bubonic plague
Consistency. Stony-hard nodes are typically a sign of cancer, usually metastatic. Very firm, rubbery nodes suggest lymphoma. Softer nodes are the result of infections or inflammatory conditions. Suppurant nodes may be fluctuant. The term "shotty" refers to small nodes that feel like buckshot under the skin, as found in the cervical nodes of children with viral illnesses.
Matting. A group of nodes that feels connected and seems to move as a unit is said to be "matted." Nodes that are matted can be either benign (e.g., tuberculosis, sarcoidosis or lymphogranuloma venereum) or malignant (e.g., metastatic carcinoma or lymphomas).
The anatomic location of localized adenopathy will sometimes be helpful in narrowing the differential diagnosis. For example, cat-scratch disease typically causes cervical or axillary adenopathy, infectious mononucleosis causes cervical adenopathy and a number of sexually transmitted diseases are associated with inguinal adenopathy
Supraclavicular lymphadenopathy has the highest risk of malignancy, estimated as 90 percent in patients older than 40 years and 25 percent in those younger than age 40. Having the patient perform a Valsalva's maneuver during palpation of the supraclavicular fossae increases the chance of detecting a node. Lymphadenopathy of the right supraclavicular node is associated with cancer in the mediastinum, lungs or esophagus. The left supraclavicular (Virchow's) node receives lymphatic flow from the thorax and abdomen, and may signal pathology in the testes, ovaries, kidneys,
Although rarely present, a paraumbilical (Sister Joseph's) node may be a sign of an abdominal or pelvic neoplasm. pancreas, prostate, stomach or gallbladder.
Although rarely present, a paraumbilical (Sister Joseph's) node may be a sign of an abdominal or pelvic neoplasm.
In patients with generalized lymphadenopathy, the physical examination should focus on searching for signs of systemic illness. The most helpful findings are
rash, mucous membrane lesions, hepatomegaly, splenomegaly or arthritis . Splenomegaly and lymphadenopathy occur concurrently in many conditions, including mononucleosis-type syndromes, lymphocytic leukemia, lymphoma and sarcoidosis
Generalized Lymphadenopathy Because generalized lymphadenopathy almost always indicates that a significant systemic disease is present.If a diagnosis cannot be made, the clinician should obtain a biopsy of the node. The diagnostic yield of the biopsy can be maximized by obtaining an excisional biopsy of the largest and most abnormal node (which is not necessarily the most accessible node). If possible, the physician should not select inguinal and axillary nodes for biopsy, since they frequently show only reactive hyperplasia.
Localized Lymphadenopathy The decision about when to biopsy is more difficult. Patients with a benign clinical history, an unremarkable physical examination and no constitutional symptoms should be reexamined in three to four weeks to see if the lymph nodes have regressed or disappeared. Patients with unexplained localized lymphadenopathy who have constitutional symptoms or signs, risk factors for malignancy or lymphadenopathy that persists for three to four weeks should undergo a biopsy.
Biopsy should be avoided in patients with probable viral illness because lymph node pathology in these patients may sometimes simulate lymphoma and lead to a false-positive diagnosis of malignancy.
Etiologies of Lymphadenopathy
I. Generalized lymphadenopathyInfections
Viral
upper respiratory infections
Infectious mononucleosis
CMV
Acquired immunodeficiency
Rubella
Varicella
Measles
Bacterial
Septicemia
Typhoid fever
Tuberculosis
Syphilis
Plague
Protozoal - Toxoplasmosis
Fungal - Coccidioidomycosis
Autoimmune disorders
Juvenile rheumatoid arthritis
Systemic lupus erythematosus
Drug reactions (eg, phenytoin, allopurinol)
Serum sickness
Storage Diseases
Gaucher disease
Niemann-Pick disease
Neoplastic and proliferative disorders
Acute leukemias
Lymphomas (Hodgkin, non-Hodgkin)
Neuroblastoma
Histiocytoses
II. Regional lymphadenopathy
Cervical
Viral upper respiratory infection
Infectious mononucleosis
Rubella
Catscratch disease
Streptococcal pharyngitis
Acute bacterial lymphadenitis
Toxoplasmosis
Tuberculosis/atypical mycobacterial infection
Acute leukemia
Lymphoma
Neuroblastoma
Rhabdomyosarcoma
Kawasaki disease
Submaxillary and submental
Oral and dental infectionsAcute lymphadenitis
Occipital
Pediculosis capitis
Tinea capitis
Secondary to local skin infection
Rubella
Roseola
Preauricular
Local skin infection
Chronic ophthalmic infection
Catscratch disease
Mediastinal
Acute lymphoblastic leukemia
Lymphoma
Sarcoidosis
Cystic fibrosis
Tuberculosis
Histoplasmosis
Coccidioidomycosis
Supraclavicular
Lymphoma
Tuberculosis
Histoplasmosis
Coccidioidomycosis
Axillary
Local infection
Catscratch disease
Brucellosis
Reactions to immunizations
Lymphoma
Juvenile rheumatoid arthritis
Abdominal
Acute mesenteric adenitis
Lymphoma
Inguinal
Local infection
Diaper dermatitis
Insect bites
Lymphogranuloma venereum
Syphilis
“History tells you what it is, and the examination tells you where it is." The history and examination allow the neurologist to arrive at the etiology and pathology of the condition
• Episodic hypotension
• Monitoring treatment• “Nondipping” blood pressure that does not drop overnight Suspected autonomic neuropathy
• Suspected overtreatment with resultant iatrogenic hypotension
• Suspected “white coat” hypertension and discrepant readings between home and clinic
Key Indications for Ambulatory Blood Pressure Monitoring
Palpable thyroid nodules are found in about 5% of adults .In several large studies, FNA biopsies yielded the following findings: 70% benign, 10% malignant or suspicious for malignancy, and 20% nondiagnostic or yielding insufficient material for diagnosis. Characteristic features of malignancy mandate surgery. A diagnosis of follicular neoplasm also warrants surgery, as benign and malignant lesions cannot be distinguished based on cytopathology or frozen section..
Thyroid Nodule
The management of patients with benign lesions is more variable. Many authorities advocate TSH suppression, whereas others monitor nodule size without suppression. With either approach, thyroid nodule size should be monitored, ideally using ultrasound. Repeat FNA is indicated if a nodule enlarges, and a second biopsy should be performed within 2–5 years to confirm the benign status of the nodule.
Nondiagnostic biopsies occur for many reasons, including a fibrotic reaction with relatively few cells available for aspiration, a cystic lesion in which cellular components reside along the cyst margin, or a nodule that may be too small for accurate aspiration. For these reasons, ultrasound-guided FNA is indicated when the FNA is repeated. Ultrasound is also increasingly used for initial biopsies in an effort to enhance nodule localization and the accuracy of sampling. Ultrasound characteristics are also useful for deciding which nodules to biopsy when multiple nodules are present.
Sonographic characteristics suggestive of malignancy include microcalcifications, increased vascularity, and hypoechogenicity within the nodule .
Drugs that can cause jaundice:
AldometAminosalicylate
Chemotherapy drugs
Erythromycin
Flucytosine
Oral contraceptives
Tolbutamide, chlorpropamide
Phenothiazines:
Chlorpromazine
Fluphenazine
Stelazine
Thioridazine
Prochlorperazine
Propylthiouracil
Rifampin
Steroids
Sulfa drugs:
Testosterone
Tiopronin
Allopurinol
Aminoglycosides
Amphotericin B
Bacitracin
Carbamazepine
Cephalosporins
Chloral hydrate
Cisplatin
Colistin
Furosemide
Gentamicin
Guanethidine
High-dose aspirin
Indomethacin
Drugs that can increase BUN measurements include
MethicillinMethotrexate
Methyldopa
Neomycin
Penicillamine
Polymyxin B
Probenecid
Propranolol
Rifampin
Spironolactone
Tetracyclines
Thiazide diuretics
Triamterene
Vancomycin
Drugs that can decrease BUN measurements include:
Chloramphenicol
Streptomycin
Medications safe in G6PD
GeneralDrugs previously thought contraindicated in G6PD
May not apply to Class I G6PD
Analgesics
Acetaminophen
Aspirin
Auralgan
Cardiovascular Agents
Procainamide
Quinidine
Neurologic Agents
Trihexyphenidyl
Levodopa
Phenytoin
Antibiotics
Chloramphenicol
Chloroquine
Isoniazid
Probenecid
Proguanil
Pyrimethamine
Miscellaneous
Vitamin C
Colchicine
Diphenhydramine
Patients with (G6PD) deficiency should heed the following precautions:
Avoid oxidant drugs such as the antimalarial drugs primaquine, chloroquine, pamaquine, and pentaquine.
Avoid nitrofurantoin.
Avoid nalidixic acid, ciprofloxacin niridazole, norfloxacin, methylene blue, chloramphenicol, phenazopyridine, and vitamin K analogues.
Avoid sulfonamides.
Avoid exposure to certain chemicals such as those in mothballs. Dapsone
The following substances should also be avoided in individuals with glucose-6-phosphatase dehydrogenase (G6PD) deficiency:
Acetanilid
Doxorubicin
Isobutyl nitrite
Naphthalene
Phenylhydrazine
Pyridium
Delayed relaxation phase of deep tendon reflexes
Differential Diagnosishypothyroidism
neurosyphilis
parkinsonism
pernicious anemia
sarcoidosis, myasthenia gravis
schizophrenia
diabetes mellitus
glucose administration
sprue
medications (propranolol, procainamide, reserpine, potassium), hypothermia, leg edema, normal puerperium, female sex, age
The incidence of Down syndrome is estimated at one per 800 to one per 1000 births.In 2006, the Centers for Disease Control and Prevention estimated the rate as one per 733 live births in the United States (5429 new cases per year. Approximately 95% of these are trisomy 21.
Although the probability increases with maternal age, 80% of children with Down syndrome are born to women under the age of 35,reflecting the overall fertility of that age group. Recent data also suggest that paternal age, especially beyond 42,also increases the risk of Down Syndrome.
Current research (as of 2008) has shown that Down syndrome is due to a random event during the formation of sex cells or pregnancy. There has been no evidence that it is due to parental behavior (other than age) or environmental factors.
What are a couple's chances of having a child with Down syndrome?In the usual circumstance, the chances depend upon the age of the mother. The odds of having a child with Down syndrome at age 35 are approximately 1 in 350. Under age 25, the odds are about 1 in 1400 and at age 40 the odds are about 1 in 100. (Thompson, et al., 1991)
The chances of a parent of a child with Trisomy 21 having another child with Down syndrome is approximately 1 in 100.
If the child has a translocation, the recurrence risk can be as high as 100% or as low as 2%. Parents of children with translocation type of Down syndrome should have chromosome analysis to detect a carrier state.
When is prenatal diagnosis recommended?Until recently, the answer was to offer amniocentesis to all pregnant women age 35 or older and to those women who had a previous child with Down syndrome. Now some doctors reccommend screening tests for all pregnancies.
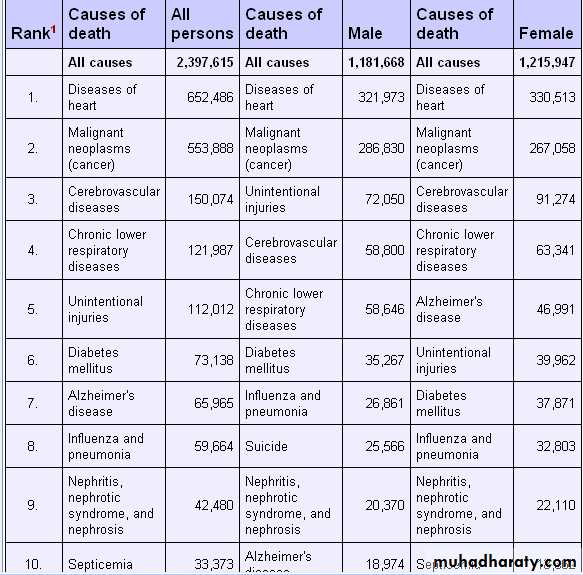
Breast cancer is the second leading cause of death from cancer in American women.
10 Leading Causes of Death in the U.S., 2004
Death rates from the four most common cancers lung, breast, prostate, and colorectal
What's the leading cause of cancer death in women in the United States? The answer might surprise you, because it is lung cancer, not breast cancer. According to the American Lung Association, lung cancer accounts for almost twice as many deaths as breast cancer. And while smokers are more likely to develop the disease, one in every five people with lung cancer has never touched a cigarette.
Hyperprolactinaemia – drugs that are responsible
include dopamine antagonists:• Antipsychotics (Haloperidol, Sulpiride)
• Metoclopramide
• Domperidone
• SSRIs
Andropause or male menopause is a name that has been given to a menopause-like condition in ageing men. This relates to the slow by steady reduction of the production of the hormones testosterone and dehydroepiandrosterone in middle-aged men, and the consequences of that reduction,which is associated with a decrease in Leydig cells.
Unlike women, middle-aged men do not experience a complete and permanent physiological shutting down of the reproductive system as a normal event. A steady decline in testosterone levels with age (in both men and women) is well documented,
In 1944, Heller and Myers identified symptoms of what they labeled the "male climacteric" including loss of libido and potency, nervousness, depression, impaired memory, the inability to concentrate, fatigue, insomnia, hot flashes, and sweating. Heller and Myers found that their subjects had lower than normal levels of testosterone, and that symptoms improved dramatically when patients were given replacement doses of testosterone.
Andropause has been observed in association with Alzheimer's disease.
Some researchers prefer the term "androgen deficiency of the aging male" ("ADAM"), to more accurately reflect the fact that the loss of testosterone production is gradual and asymptotic in contrast to the more abrupt change associated with menopause The "D" is sometimes given as "decline" instead of "deficiency. In some contexts, the term "partial androgen deficiency in aging males" ("PADAM") is used instead.
Andropause is usually caused by a very gradual testosterone deficiency and an increase in sex hormone-binding globulin (SHBG) that occurs from age 35 onwards.
By contrast, women have a sudden onset of menopause around age 51. Testosterone declines 10% every decade after age 30 (1% per year).
The term "male menopause" may be a misnomer, as unlike women, men's reproductive systems do not cease to work completely in mid-life; some men continue to father children late into their lives
(at age 90 or older).
Causes of respiratory muscle weaknessRespiratory muscle weakness has several causes, which may be subdivided into neural abnormalities, disorders of the neuromuscular junction, and abnormalities of muscle tissue.
Causes of diaphragmatic muscle weakness
• Neural abnormalitie• Upper motor neurone:Cerebral infarction or haemorrhage
• Lower motor neurone:
• Guillain-Barré syndrome
• Trauma
• Mediastinal malignancies
• Herpes zoster
• Motor neurone disease
• Vasculitis
• Hereditary sensorimotor polyneuropathy
• Critical illness polyneuropathy
• Alcoholism
• Diabetes
Abnormalities of the neuromuscular junction
• Toxins (such as botulinum)DrugsMyasthenia gravis
• Abnormalities of muscle function
• Muscular dystrophiesMyopathiesAcid maltase deficiencyHypothyroidismSystemic lupus erythematosis ("shrinking lung syndrome")Mechanical ventilation induced diaphragmatic dysfunction
Most arm lymphedema is a secondary condition caused by
removal of lymph nodes for cancer biopsy, damage to the lymphatics from radiation or even chemotherapy for breast cancer.
Other causes can include
burns, various infections, injury or trauma. primary lymphedema
ARM LYMPHEDEMA
Light Arm Exercises That Can Help Prevent/Manage Lymphedema
Because light exercise after breast cancer surgery and lymph node removal can help reduce the chances of lymphedema, patients should discuss how and when to begin arm exercises. Some patients find that taking painkillers (analgesics) 30 minutes prior to exercising helps alleviate discomfort.The following are suggestions of exercises following breast cancer surgery from the Wessex Cancer Trust, an independent charity that provides information and support to patients with cancer. Each exercise may be performed five times in a row, three times a day (morning, afternoon, evening).
With palms up and elbows straight, stretch arms high above head, linking fingers together. Bend elbows and clasp hands at the back of the neck. Push elbows out as far as possible and then bring them together to touch in front of the body. Repeat. Place hands behind the back and lace fingers together. Slide hands as far as possible up the body toward the neck.
Place hands on shoulders (on the same side of the body) and move elbows up and then down toward the sides of the body.
Place hands on shoulders and make circular movements with the elbows. Circles should be as large as possible. Change directions periodically.
After breast stitches have been removed, stand with one foot in front of the other. Hold on to a chair or table. Lean forward and swing the arm that was involved in the surgery backwards and forwards, and then from side to side as far as it will go. Hold a small weight to gain momentum. Increase movement until arm reaches shoulder height. Keep elbows straight.
Stand with one foot in front of one another. Hold onto a chair or table for support. Lean forward and swing the arm on the side of the surgery in circles, first clockwise and then counter-clockwise. Keep elbows straight.
Face toward a wall. Place hands on the wall and inch fingers up the wall. Try to go higher each day until arms are fully straight over head.
Prevention of Arm Lymphedema
Avoid InfectionTreat even small injuries/hangnails with care.
Do not have blood drawn from the affected arm, unless absolutely necessary.
Have someone else get dishes out of the oven when feasible.
Wear rubber gloves when doing dishes. Wear canvas gloves while gardening and doing yard work. Wear a thimble while sewing. Shave underarms with an electric razor.
Avoid chemical hair removers.
Use insect repellant to protect against bug bites or bee stings.
Avoid sunburn by using sunscreen with SPF of at least 15.
Reapply sunscreen after swimming and as directed on the sunscreen label. Don't allow injections, vaccinations on the affected arm. Do not have manicures on the affected hand. Do not cut cuticles or hangnails. Don't hold a cigarette in the affected hand.
Avoid Constriction .
Avoid clothing with elastic sleeve bands or with tight arms. Don't wear a watch or rings on affected arm. Avoid carrying a heavy purse or bag with the affected arm.
Have blood pressure taken on the unaffected arm, if possible. Underclothing, such as bras, should not leave pressure marks
When traveling in a car or plane for long distances, keep the affected arm above the level of the heart, if at all possible. Avoid Muscle Strain .
Avoid heavy lifting if your muscles are not used to heavy lifting. Avoid vigorous, repetitive movements such as scrubbing, pulling, hammering. Sports such as tennis, racquetball and golf have the potential to strain muscles because of sudden and forceful strokes. Begin any new exercise/activity involving the arms gradually and with caution.
alpha1 antitrypsin, a serine protease inhibitor produced mainly in the liver that protects lung tissue against proteolytic damage from neutrophil elastase. As a result of decreased serum α1antitrypsin concentrations, excess protease in the alveoli destroys alveolar walls and results in emphysema. Smoking is the most important risk factor for developing emphysema. Non-smokers with α1antitrypsin deficiency may not develop lung disease.
A small proportion of adults with antitrypsin deficiency develop liver fibrosis, with progression to cirrhosis and hepatocellular carcinoma. This is caused by accumulation of unsecreted antitrypsin polymers within hepatocytes.
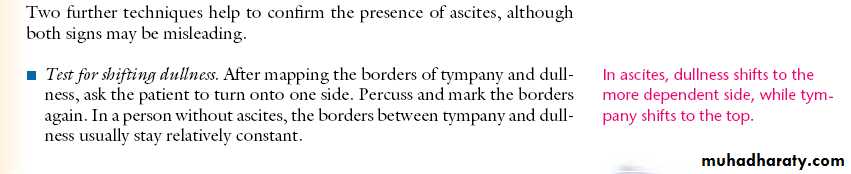
BMJ February 2010
Chest radiographyin patients with alpha1 antitrypsin deficiency typically shows hyperinflation and reduced lung markings; it can also show bulla formation associated with emphysematous changes. Areas are also described as oligaemic—lacking the usual pattern of branching blood vessels. The lung bases are often affected in these patients, whereas in patients with typical COPD emphysema is usually apically distributed.
How would you manage this condition?Smoking cessation is the most important factor and has the greatest effect on survival. Treatment is similar to that for standard COPD and should follow the guidelines for this disease: short and long acting inhaled β2 agonists, anticholinergics, inhaled corticosteriods and pulmonary rehabilitation. Disease specific treatment includes enzyme replacement, which is used commonly in the United States but rarely outside of trials in the United Kingdom. Observational trials have suggested benefit for this treatment, but no controlled trial has confirmed this. All patients with COPD, but especially those with early onset disease (third or fourth decade), should be investigated for α1antitrypsin deficiency.
Annual influenza and pneumonia vaccines should be offered. Long term home oxygen therapy has also been shown to increase survival. Genetic counselling should be considered.
Lung transplantation may be considered in patients at risk of early death who are otherwise healthy before disease becomes too severe .
Gupta Y K et al. BMJ 2010;341:bmj.c3404
• ©2010 by British Medical Journal Publishing GroupSymmetrical lobular enlargement of both pulmonary hila, with no signs of cardiomegaly or vascular abnormality This appearance is consistent with bilateral hilar lymphadenopathy.
Hilar adenopathy appears as round or lobulated abnormal soft tissue arising from the hilaLack of coexistent signs of cardiac disease, such as cardiomegaly or abnormal pulmonary vasculature, helps to distinguish it from pulmonary artery enlargement. Bilateral adenopathy, characterised by roughly symmetrical hilar enlargement, should be distinguished from unilateral disease, which suggests alternative diagnoses .If in doubt about whether hilar abnormality represents adenopathy, further imaging is indicated .
Bilateral hilar lymphadenopathy
The most common causes are sarcoidosis, lymphoma, and leukaemia in addition to fungal, viral, and tuberculous infection.The most common cause (70-90% of cases) is sarcoidosis. Half of these patients are asymptomatic and are diagnosed after chest radiography is performed for other reasons.Unless a patient presents with other characteristic clinical findings of sarcoidosis, such as erythema nodosum and uveitis, confirmation by further imaging or biopsy (or both) is usually needed.
Other inflammatory causes of bilateral hilar lymphadenopathy are less common and include the occupational lung diseases silicosis and berylliosis. Although these conditions classically present with multiple small nodules on chest radiography, they can also be radiographically indistinguishable from sarcoidosis, in which case a history of exposure is suggestive.
Although almost any lung infection can cause enlargement of the draining pulmonary lymph nodes, bilateral hilar adenopathy is most commonly seen in primary tuberculosis, particularly in children, and in fungal infections such as histoplasmosis and coccidioidomycosis. (anthrax) and Yersinia pestis (plague), often with associated lower lobe airspace opacities, and in viral infection with rubella, Epstein-Barr virus (glandular fever), echovirus, and varicella.
Of the many cancers that cause hilar adenopathy, lymphoma, leukaemia, and metastases more commonly cause bilateral, as opposed to unilateral, disease. Bilateral hilar lymphadenopathy is more common in Hodgkin’s lymphoma than in non-Hodgkin’s lymphoma, which often exhibits parenchymal involvement without mediastinal adenopathy. Around 25% of patients with leukaemia have hilar or mediastinal adenopathy, which is more common in lymphocytic forms, particularly chronic lymphocytic leukaemia. Primary tumours that commonly metastasise to hilar nodes include bronchogenic tumours, as well as tumours of the kidney, testis, head and neck, and breast.
The ventricular contractions are too weak and unable to open the aortic valve , but at the same time they are good enough to close the mitral valve. To open the aortic valve it has to generate at least 60-80 mmhg pressure , while mitral valve closes even as LV generates 8-14 mmhg .(LV/LA pressure cross over). So intermitently the second heart sound is missed while S1 is retained, producing more heart sounds and less pulse count in the periphery, this intermittent absence of S2 results in totally irregular S1 /S 2 relation.
Pulse deficit
If heart rate is higher than 100 beats per minute, finding third and fourth heart sounds is impossible.
Cooling down
Cooling down, also called warming down, is the term used to describe an easy exercise that will allow the body to gradually transition from an exertional state to a resting or near-resting state. Depending on the intensity of the exercise, cooling down can involve a slow jog or walk, or with lower intensities, stretching can be used. Cooling down helps remove lactic acid which can cause cramps and stiffness and allows the heart rate to return to its resting rate. Contrary to popular belief, cool down does not appear to reduce delayed-onset muscle soreness. Cool downs should involve a gradual yet continuous decrease in exercise intensity (i.e. from a hard run to an easy jog to a brisk walk), stretching, and rehydration. Durations can vary for different people, but 5–10 minutes is considered adequate.Heart rate
During aerobic exercise, peripheral veins, particularly those within muscle, dilate to accommodate the increased blood flow through exercising muscle. The skeletal-muscle pump assists in returning blood to the heart and maintaining cardiac output. A sudden cessation of strenuous exercise may cause blood to pool in peripheral dilated veins and the heart must beat faster and harder to adequately oxygenate the body and maintain blood pressure. A cool-down period allows a more gradual return to venous tone, and allows a gradual decline in heart rate that reduces stress on the organ. Besides, as the heat rate increases, there is more oxygen supply to body, which helps the breaking down of lactic acid and hence prevent it from causing harm to body.Warming up
A warm-up is usually performed before participating in technical sports or exercising. A warm-up generally consists of a gradual increase in intensity in physical activity (pulse raiser), a joint mobility exercise, stretching and a sport related activity. For example, before running or playing an intense sport one might slowly jog to warm muscles and increase heart rate. It is important that warm ups should be specific to the exercise that will follow, which means that exercises (of warm up) should prepare the muscles to be used and to activate the energy systems that are required for that particular activity. The risks and benefits of combining stretching with warming up are mixed and in some cases disputed. Warming up prepares the body mentally & physically.
Benefits
A warm-up will improve the effectiveness of training and should be done before every training session. This is fundamental to a safe practice.Direct physical effects: Release of adrenaline, Increased heart rate,Enables oxygen in the blood to travel with greater speed ,Increased production of synovial fluid located between the joints to reduce friction, Allows joints to move more efficiently, Dilation of capillaries ,Enables oxygen in the blood to travel at a higher volume, Increase of temperature in the muscles, Decreased viscosity of blood, Facilitates enzyme activity, Encourages the dissociation of oxygen from haemoglobin, Greater extensibility and elasticity of muscle fibres, Increased force and speed of contraction Increase of muscle metabolism, Supply of energy through breakdown of glycogen, Increase in speed of nerve impulse conduction.
A comprehensive warm-up programme has been found to decrease injuries in soccer.
Validation of the ABCD2 Score for Predicting Stroke Risk After Transient Ischemic Attack
An ABCD2 score >2 is associated with significantly increased risk for stroke within 90 days.The ABCD2 score has been endorsed internationally as a simple method for identifying patients with transient ischemic attack (TIA) who are at high risk for early stroke and require admission, yet multiple external validation studies have demonstrated mixed results. In a multicenter case series study, investigators prospectively applied the score to 148 consecutive patients with TIA at three hospitals in Greece and Singapore.
Journal Watch Emergency Medicine May 14, 2010
The 7-point ABCD2 score is based on the following:
Age 60 = 1 pointBlood pressure at presentation 140/90 mm Hg = 1 point
Clinical features: unilateral weakness = 2 points; speech disturbance without weakness = 1 point
Duration of symptoms: 10–59 minutes = 1 point; 60 minutes = 2 points
Diabetes mellitus = 1 point
Patients with higher ABCD2 scores had significantly higher incidences of stroke at 7 days and 90 days. The score accurately predicted high 7-day and 90-day stroke risk (area under the receiver operating characteristic curve, 0.72 and 0.75, respectively). Patients with scores >2 were five times more likely to suffer stroke at 90 days than those with lower scores.
Comment: This study supports the clinical use of the ABCD2 score. We should follow the American Heart Association/American Stroke Association recommendation that patients with scores >2 be admitted to the hospital for urgent diagnostic evaluation.
Transient loss of consciousness—initial assessment, diagnosis, and specialist referral: summary of NICE guidance
spontaneous loss of consciousness with complete recovery, affecting a quarter to half of the population at some point in their lives. The condition has many possible causes, including cardiovascular disorders (ranging from cardiac arrhythmias to vasovagal syncope), epilepsy, and psychogenic attacks. Diagnosis is often inaccurate, inefficient, and delayed, and management varies considerably.
Ask the person with suspected transient loss of consciousness, and any witnesses ,to describe what happened:
• Before the event (circumstances, posture, prodromal symptoms)
• During the event (appearance and colour; movement; any tongue biting or injury; and duration of transient loss of consciousness)
• During the recovery period (confusion, weakness down one side).
Assess and record:
• Details of any previous transient loss of consciousness• Medical history and any family history of cardiac disease
• Current medication
• Vital signs
• Lying and standing blood pressure if appropriate
• Other cardiovascular and neurological signs.
Electrocardiography, additional tests, and transfer of records
Atrial arrhythmia (sustained)Inappropriate persistent bradycardia
Conduction abnormality (for example, complete right or left bundle branch block or any degree of heart block)
Left or right ventricular hypertrophy
Long QT interval (corrected >450 ms) and short QT interval (corrected <350 ms)
Pathological Q waves
Ventricular pre-excitation
Any ventricular arrhythmia (including ventricular extrasystoles)
Brugada syndrome
Paced rhythm
Any abnormalities in ST segment or T wave, especially abnormal T wave inversion
Important abnormalities in a 12 lead electrocardiogram
If you suspect an underlying problem causing (or additional to) the transient loss of consciousness, conduct relevant examinations and investigations (for example, check blood glucose levels if hypoglycaemia is suspected, or haemoglobin levels if anaemia or bleeding is suspected).
Making a judgment based on initial assessment
Red flags: refer the patient within 24 hours for a specialist cardiovascular assessment by the most appropriate local service if the person has any of the following:• Transient loss of consciousness during exertion
• New or unexplained breathlessness
• Heart failure
• Family history of sudden cardiac death in people younger than 40 years and/or an inherited cardiac condition
• A heart murmur
• Any of the important electrocardiographic abnormalities listed
If the patient has no features suggesting an alternative cause of transient loss of consciousness (note that brief seizure activity can occur during uncomplicated faints), diagnose uncomplicated faint or situational syncope, or suspect orthostatic hypotension when there are suggestive features as follows:
Uncomplicated faint (the “three Ps”):
posture (a faint may follow prolonged standing or the patient may have a history of similar episodes prevented by lying down); provoking factors (such as a medical procedure);
prodromal symptoms (such as sweating before transient loss of consciousness) .
• Situational syncope, in which syncope is clearly and consistently provoked by straining (such as with micturition), coughing, or swallowing .
Orthostatic hypotension, in which the history is typical and lying and standing blood pressure (with repeated measurements while standing for three minutes) confirms orthostatic hypotension.
Suspect epileptic seizures
• A bitten tongue• Head turning to one side during transient loss of consciousness
• No memory of abnormal behaviour even though such behaviour has been witnessed by someone else before, during, or after transient loss of consciousness
• Unusual posturing
• Prolonged jerking of limbs
• Confusion after transient loss of consciousness.
• Prodromal déjà vu, or jamais vu (a feeling that something is happening for the first time, despite knowing rationally that it has happened before)
For people with suspected vasovagal syncope who experience recurrent episodes adversely affecting their quality of life, or are at high risk of injury, consider a tilt test only to assess whether the syncope is accompanied by a severe cardioinhibitory response (usually asystole).
For people with suspected carotid sinus syncope and for people with unexplained syncope who are aged 60 years or older, offer carotid sinus massage in a controlled environment as a first line investigation.
For people with suspected cardiac arrhythmia as a cause of syncope, or with unexplained syncope (including those aged 60 years and older who have had a negative result for carotid sinus massage), offer ambulatory electrocardiography (and do not offer a tilt test before this procedure).
Choose the type of ambulatory electrocardiography according to the frequency of the patient’s transient loss of consciousness:
-Several episodes a week: offer Holter monitoring (up to 48 hours), then if no further loss of consciousness occurs offer an external event recorder
- Episodes every one to two weeks: offer an external event recorder, then if necessary offer an implantable event recorder
- An episode less than once every two weeks: offer an implantable event recorder.
they must not drive while waiting for their assessment, and they must discuss driving with the specialist
Skin examination: Chronic kidney disease can cause any of the following:
Xerosis due to sebaceous and eccrine sweat gland atrophyPallor due to anemia
Hyperpigmentation due to melanin deposition
Sallow or yellow-brown skin due to urochrome deposition
Petechiae or ecchymoses due to platelet dysfunction
Uremic frost, the deposition of white-to-tan urea crystals on the skin after sweat evaporation, is rare.
The differential diagnosis for yellowing of the skin is limited. In addition to jaundice, it includes carotenoderma, the use of the drug quinacrine, and excessive exposure to phenols. Carotenoderma is the yellow color imparted to the skin by the presence of carotene; it occurs in healthy individuals who ingest excessive amounts of vegetables and fruits that contain carotene, such as carrots, leafy vegetables, squash, peaches, and oranges.
As serum bilirubin levels rise, the skin will eventually become green if the process is long-standing; the green color is produced by oxidation of bilirubin to biliverdin.
Unlike jaundice, where the yellow coloration of the skin is uniformly distributed over the body, in carotenoderma the pigment is concentrated on the palms, soles, forehead, and nasolabial folds. Carotenoderma can be distinguished from jaundice by the sparing of the sclerae.
Quinacrine causes a yellow discoloration of the skin in 4–37% of patients treated with it. Unlike carotene, quinacrine can cause discoloration of the sclerae.
Depending on the calorie level, recommendations for added sugars vary from 5 teaspoons per day (or 80 calories) for a daily energy expenditure of 1800 calories for an average adult woman and 9 teaspoons per day (or 144 calories) for a daily energy expenditure of 2200 calories for an average adult man.
For reference, one 12-ounce can of cola contains ≈8 teaspoons of added sugar, ≈130 calories.
In conclusion, to achieve and maintain healthy weights and decrease cardiovascular risk while at the same time meeting essential nutrient needs, the AHA encourages people to consume an overall healthy diet that is consistent with the AHA’s 2006 diet and lifestyle recommendations. Women should eat or drink no more than 100 calories per day from added sugars, and men should eat or drink no more than 150 calories per day from added sugars.
Two mechanisms result in cyanosis:
• systemic arterial oxygen desaturation and• increased oxygen extraction by the tissues. Based upon these mechanisms, two types of cyanosis are described: central and peripheral.
• In addition, dermatologic conditions may result in blue skin color that mimics cyanosis in the absence of increased levels of deoxygenated blood in the capillary beds.
Central cyanosis — Central cyanosis is evident when systemic arterial concentration of deoxygenated hemoglobin (Hb) in the blood exceeds 5 gm/dL (3.1 mmol/L) (oxygen saturation ≤85 percent) .Of note, cyanosis cannot be detected by observation in patients with severe anemia (Hb <5 gm/dL (3.1 mmol/L)).
Peripheral cyanosis — Patients have a normal systemic arterial oxygen saturation. However, increased oxygen extraction results in a wide systemic arteriovenous oxygen difference and increased deoxygenated blood on the venous side of the capillary beds.
The increased extraction of oxygen results from sluggish movement of blood through the capillary circulation. Causes include vasomotor instability, vasoconstriction caused by exposure to cold, venous obstruction, elevated venous pressure, polycythemia, and low cardiac output.
Infectious
Tuberculosis
HIV
Endocarditis
Endocrine
Menopause*
Hyperthyroidism*
Phaeochromocytoma
Carcinoid syndrome
Acromegaly
Diabetes
Neurological
Parkinsonism
Neuropathies
Malignancies
Myeloproliferative disorders
Lymphoma
Medication
Antidepressants* (SSRIs, especially vanlafaxine and tricyclics)
Hormonal agents (tamoxifen, GnRH agonists)*
Antipyretics (aspirin, NSAIDs)*
Intoxication*
Withdrawal from alcohol or other substances*
Causes of generalised sweating
Hyperhidrosis, hot flushes, and night sweats are commonly associated with the menopause, which occurs at a median age of 51 years. Sweating and flushing occur in up to 51% of women before menopausal transition, 35-50% during perimenopause, and 30-80% after the menopause. Episodes typically start with an unpleasant sensation or sudden onset of a sensation of heat in the face and upper chest, which quickly becomes generalised. It lasts for a few minutes and is associated with profuse perspiration and sometimes palpitations. These flushes are thought to be due to thermoregulatory dysfunction, initiated at the level of the hypothalamus by oestrogen withdrawal.
Although sweating in a woman of menopausal age is common, clinicians should not immediately conclude that it is only due to menopausal hot flushes. Measuring gonadotrophins (luteinising hormone and follicle stimulating hormone) and oestradiol can be helpful. Raised luteinising hormone and follicle stimulating hormone with a low oestradiol concentration confirm menopausal status.
Thyroid function is an important investigation as hyperthyroidism can lead to sweating and to menstrual irregularities with oligomenorrhoea. This should be evident with a low concentration of thyroid stimulating hormone in the context of a raised free thyroxine (fT4) or free triiodothyronine (fT3).
Other endocrinological causes of sweating are rare but it is important they are not missed, and clinical suspicion should lead to referral to a specialist centre. Investigations may include determining serum
insulin-like growth factor-I concentration if features in keeping with acromegaly are present. Carcinoid syndrome must be excluded in a patient with episodic flushing, usually by measuring 24 hour urinary excretion of 5-hydroxyindoleacetic acid (5HIAA), which is the end product of serotonin metabolism. This test has a sensitivity of 75% and specificity of up to 100%.
Although rare, phaeochromocytomas and paragangliomas should be considered in a patient with sustained or paroxysmal hypertension alongside sweating. Plasma fractionated metanephrines are the first line test, with a sensitivity of up to 100%, but because specificity is 85-89% some groups advocate 24 hour urinary metanephrines, which have a sensitivity and specificity of 98%. Investigations for these conditions should be performed in local specialist centres .
Methemoglobin
Normal hemoglobin unbound to oxygen is called reduced hemoglobin and is symbolized HbFe+2. Methemoglobin (metHb), the oxidized form of hemoglobin, is HbFe+3. Normally, as much as 2% of hemoglobin is in the form of metHb. Because metHb is unable to bind with oxygen, arterial oxygen saturation is reduced by the same amount that metHb is increased.MetHb imparts an intense bluish tinge to the skin; therefore, the cyanosis that comes with Methemoglobinemia is not related to reduced hemoglobin but to oxidized hemoglobin.
therefore, the cyanosis that comes with Methemoglobinemia is not related to reduced hemoglobin but to oxidized hemoglobin.
Although excess metHb reduces the measured SaO2, PaO2 is not affected; this is because metHb does not affect transfer of oxygen from the atmosphere to the lungs. Note that standard pulse oximeters, which measure SaO2 using 2 wavelengths of light, do not measure metHb (or carboxyhemoglobin). However, a new generation of pulse oximeters that uses 8 wavelengths of light does have the ability to measure carboxyhemoglobin and metHb (Barker 2006).
Sulfhemoglobin
a rare condition caused by sulfur binding with hemoglobin so that oxygen cannot be bound.
Unlike metHb, the iron moiety remains in the reduced state (HbFe+2).
Sulfhemoglobin is similar to metHb in causing low SaO2 but not affecting PaO2 and in imparting an intense bluish color to the skin.
Pseudocyanosis
a bluish tinge to the skin and/or mucous membranes that is not associated with either hypoxemia or peripheral vasoconstriction. Most causes are related to metals (eg, silver nitrate, silver iodide, silver, lead) or drugs (eg, phenothiazines, amiodarone, chloroquine hydrochloride). One report describes blue-gray discoloration in a man who for years ingested colloidal silver for a urinary tract infection ; his oxygen levels were normal.One report describes a girl with intensely blue skin from food coloring. Consider pseudocyanosis when the patient has no cardiopulmonary symptoms and the skin does not blanch under pressure. To be sure of the diagnosis, obtain a pulse oximetry or arterial blood gas measurement
Methemoglobinemia usually occurs as a drug reaction, especially to nitrite or nitrate-containing compounds (eg, nitroglycerin) and to some topical anesthetics. Dahshan and Donovan report a case of severe methemoglobinemia from topical benzocaine in a toddler. Dapsone, a drug used in HIV and non-HIV conditions, can also cause methemoglobinemia
Is CT Indicated for Patients With Isolated Syncope?
Syncope is defined as a sudden and brief loss of consciousness associated with loss of postural tone, from which recovery is rapid, spontaneous, and complete. Such events comprise up to 3% of all emergency department (ED) visits and up to 6% of all hospital admissions.The clinical evaluation of syncope begins with a thorough history, physical examination, and electrocardiogram. However, after careful evaluation, no readily diagnosed etiology of the syncopal event can be found in nearly 60% of patients.Even after a more thorough evaluation, which may include additional laboratory and imaging studies, no definitive cause may be found in as many as 57% of cases.As a result, the clinician may have continuing concern that these patients are at risk for life-threatening events.
Current guidelines have questioned the need for a "routine" computed tomography (CT) scan of the head to evaluate patients with isolated syncope.Yet, this remains a common practice in the United States.
Clinicians who order routine head CTs in patients with isolated syncope may be investigating the possibility of:
• Subarachnoid hemorrhage;
• Intraparenchymal hemorrhage;
• Subdural hemorrhage;
• Early infarct;
• Acute infarct; or
• Brain mass.
However, studies suggest that a head CT might provide new diagnostic information in only a fraction (4%) of patients with syncope.According to Day and colleagues, patients with positive findings on a head CT displayed either a focal neurologic deficit or had a history consistent with seizure.
Another study describes 117 patients who had head CTs following syncope, with no positive findings, the results support the findings of previous studies by demonstrating that routine head CTs are not indicated in isolated syncopal events.
It is important to understand that strokes and syncope do not typically go together. Strokes generally do not lead to syncope, and most syncopal events do not present as stroke-like syndromes.One rare exception may occur in the setting of global bilateral cerebral ischemia or basilar artery disease affecting the reticular activating system, leading to ischemia that may present as a stroke-like syndrome.
In theory, vertebrobasilar migraine also could lead to a syncopal event. However, in the evaluation of a patient with potential vertebrobasilar ischemia or transient ischemic attacks, magnetic resonance imaging and magnetic resonance angiograpy (not a CT scan) would be indicated.
Finally, in patients with sudden onset of a severe headache in the setting of a possible syncopal event (with concern for a subarachnoid hemorrhage), emergent head CT on arrival to the ED should be considered. Patients who present to the ED after a brief syncopal event, without focal neurologic symptoms, headache, altered mental status, or associated scalp trauma, and who are not taking anticoagulants, are unlikely to benefit from a routine head CT.
Summary of Key Points
Patients who present to the ED with significant scalp trauma associated with syncope, patients with head trauma post-syncope who are taking oral anticoagulants, and patients with sudden onset of severe headache (with concern for subarachnoid hemorrhage) in the setting of syncope are candidates for head CTs.Patients without a history of trauma, lack of ongoing or persistent headache or neurologic deficits, or history of recent seizure activity in the setting of a syncopal event are unlikely to benefit from a routine head CT in the ED.
Medscape 09/17/2010
Jargon buster
First degree relatives: mother, father, daughter, son, sister, brother.Second degree relatives: grandparent, grandchild, aunt, uncle, niece, nephew, half sister, and half brother.
Third degree relatives: first cousins.
Coeliac antibody screen
The coeliac screen should include:• IgA tissue transglutaminase.
• IgA deficiency
Your diagnosis based on a combination of:
• Serology
• Histology (which will show villous atrophy on a duodenal biopsy)
• Resolution of symptoms on a gluten free diet.
IgA deficiency may give a screening result that is falsely negative. If your patient has IgA deficiency, you should use IgG tissue transglutaminase to confirm the diagnosis.
The neonatal heel prick is a common procedure for taking a blood sample from the heel of newborn infants. A pinprick puncture is made in the heel of the infant's foot, and blood from the foot is soaked into pre-printed collection cards known as Guthrie cards
The blood samples can be used for a variety of genetic tests, including:
Other potential tests include:
It is recommended that the screening test be performed when the infant is between 48 and 72 hours of age. False positives and negatives can sometimes occur when the screening tests are performed before 48 hours.
In the UK, the NHS test for:
What is the Guthrie test and why is it done?
The Guthrie, or heel prick test is a screening test carried out on your newborn baby in the days after birth (typically day 6 or 7). The Guthrie is offered to all infants in the U.K. with the aim of screening for up to 5 disorders (depending on your health authority). Blood is taken from your baby’s heel. The sample is analysed for the following conditions:
• Phenylketonuria all UK areas
• Congenital Hypothyroidism all UK areas
• Cystic Fibrosis most UK areas
• MCAD Deficiency fewer UK areas
• Sickle Cell Disease fewer UK areas
Phenylketonuria is condition that affects the individual’s ability to metabolise a particular type of amino acid – phenylalanine. A build up of this can lead to severe mental handicap. Simply avoiding exposure to phenylalaine can minimise the effects of the condition.
Congenital Hypothyriodism is characterised by a lack of the growth hormone thyroxine. Without this hormone, normal growth cannot occur. This condition is treated with supplements of the growth hormone.
Cystic Fibrosis is an inherited condition that affects the lungs and digestive system.
MCAD (Medium Chain acyl-CoA Dehydrogenase) Deficiency is a condition in which fat metabolism is impaired. Modification of the diet can reduce symptoms.
Sickle Cell Disease affects the shape of red blood cells and reduces their ability to carry oxygen around the body.
These conditions can all be treated to a greater or lesser extent, which is why it is so worthwhile screening for them.
• Heterophile antibodies are antibodies induced by external antigens (heterophile antigens) that cross-react with self-antigens. For example, antibodies against group A streptococcal cell walls can also react with human heart tissues. These are considered heterophile antibodies.
• In clinical diagnosis, the heterophile antibody test specifically refers to a rapid test for antibodies produced against the Epstein-Barr virus (EBV), the causative agent of infectious mononucleosis.
Preventing Medical Harm: Still Far to Go
Rates of overall and preventable harms did not change significantly between 2002 and 2007.Research has shown that interventions targeted to specific medical procedures can prevent specific types of medical errors or iatrogenic harms. What is not clear is whether initiatives to promote patient safety during the past decade have lowered the overall rate of medical errors in hospitals. To find out, researchers retrospectively reviewed 2400 hospitalizations at 10 randomly selected North Carolina hospitals from 2002 through 2007; the authors chose North Carolina because they consider its hospitals to be leaders in patient safety initiatives.
Using a standardized method for identifying potential medical harms, the researchers found 25 harms per 100 admissions — 63% of the harms were considered preventable. Among the most common harms were hypotension, hypoglycemia, respiratory failure, hemorrhage, oversedation, hospital-acquired infections, pressure ulcers, and various surgical mishaps. The key finding: The rates of overall and preventable harms did not change significantly between 2002 and 2007.
Comment: These results are disappointing but not surprising. Focused patient safety initiatives (e.g., procedures to prevent nosocomial infection or electronic technologies to reduce prescribing mistakes) surely contribute to patient safety. In my view, however, medical harms often result from errors in clinical reasoning and suboptimal diagnostic and therapeutic decision making; until these types of errors are addressed, a dramatic decline in medical harm is unlikely.
— Allan S. Brett, MD
Published in Journal Watch General Medicine December 16, 2010
Managing a high international normalised ratio
The anticoagulation nurse phones you for advice about a 73 year old woman on warfarin for atrial fibrillation whose normal international normalised ratio range falls between 2.0 and 3.0. She has recently been started on clarithromycin for a chest infection and her international normalised ratio has now come back at greater than 9.0.What should you advise?
What should you advise?
A Stop warfarinB Stop warfarin and administer vitamin K and fresh frozen plasma
C Stop warfarin and convert to intravenous heparin (high risk of stroke)
D Stop warfarin, administer vitamin K, and restart warfarin when her international normalised ratio is less than 5
E Stop warfarin, stop clarithromycin, and seek haematology advice
Answer
Answer D is correct.
British National Formulary (BNF) guidelines state:
For an international normalised ratio greater than 8.0, no bleeding or minor bleeding: stop warfarin and give phytomenadione (vitamin K-1) 2.5-5 mg by mouth using the intravenous preparation orally (unlicensed use) or 0.5-1 mg by slow intravenous injection (if complete reversal is required give 5-10 mg by slow intravenous injection). Repeat the dose of phytomenadione if the international normalised ratio is still too high after 24 hours; restart warfarin when the international normalised ratio is less than 5.0.For an international normalised ratio of 5.0-8.0, no bleeding: stop warfarin.
For an international normalised ratio of 5.0-8.0, minor bleeding: stop warfarin and give phytomenadione (vitamin K-1) 1-2.5 mg by mouth using the intravenous preparation orally (unlicensed use). Restart warfarin when the international normalised ratio is less than 5.0.Unexpected bleeding at therapeutic levels: always investigate the possibility of underlying cause, such as unsuspected renal or gastrointestinal tract pathology.
FNA is a useful investigation for patients presenting with a solitary thyroid nodule. However, diagnosis depends on the material aspirated and there is a false negative rate of between 1% and 6%.
• FNA is extremely accurate at diagnosing papillary carcinoma.
• Follicular cells can be found with follicular adenoma and carcinoma. Therefore, the diagnosis of follicular carcinoma cannot be made with FNA.
• Colloid and macrophages in the aspirate strongly suggest benign disease.
When esophageal varices are discovered, they are graded according to their size, as follows:Grade 1 – Small, straight esophageal varices
Grade 2 – Enlarged, tortuous esophageal varices occupying less than one third of the lumen
Grade 3 – Large, coil-shaped esophageal varices occupying more than one third of the lumen
The esophageal varices are also inspected for red wheals, which are dilatated intra-epithelial veins under tension and which carry a significant risk for bleeding.
Classification of esophageal varices
GradeEndoscopic appearance
I.
Dilated venes (< 5mm) still at the level of the surrounding tissue
II.
Dilated, straight venes (> 5 mm) protruding into the esophageal lumen but not obstructing it
III.
Large, tense and winding venes already obstructing the esophageal lumen considerably
IV.
near complete obstruction of the esophageal lumen with impending danger of hemorrhage (cherry red spots)
Ösophagusvarices grade II and III
Esophageal varices grade II (right) und grade III (left). Cherry red spots are signs of imminent hemorrhage (right). They correspond to areas of especially thin and altered variceal wall.
Further examples of esophageal varices grade II.
Simple carbohydrates, like sugar and corn syrup, are created in a factory – while complex carbohydrates in vegetables and whole grains are designed by nature, and help you maintain your health.
What endocrine tumors cause flushing?
Neuroendocrine tumors, including pheochromocytoma, vasoactive intestinal peptide–producing tumors, medullary thyroid carcinoma, and carcinoid tumors,may all secrete substances that cause flushing,hypotension or hypertension, diarrhea, and respiratory symptoms in various combinations.
Except in neonates, a tuberculin skin test should always be done before administering BCG. A reactive tuberculin skin test is a contraindication to BCG. Someone with a positive tuberculin reaction is not given BCG, because there is a high risk of severe local inflammation and scarring, not because of the common misconception that tuberculin reactors "are already immune" and therefore do not need BCG.
People found to have reactive tuberculin skin tests should be screened for active tuberculosis.
BCG is given as a single intradermal injection at the insertion of the deltoid. If BCG is accidentally given subcutaneously, then a local abscess may form (a BCG-oma) that may ulcerate, and often requires treatment with antibiotics. However, it is important to note an abscess is not always associated with incorrect administration, and it is one of the more common complications that can occur with the vaccination.
Numerous medical studies on treatment of these abscesses with antibiotics have been done with varying results, but the consensus is that once pus is aspirated and analysed, providing there are no unusual bacilli present, the abscess will generally heal spontaneously in a matter of weeks
ESR is a measure of the height of erythrocytes that fall through plasma in a Westergen or a Wintrobe tube over a period of 1 hour. ESR can be greatly influenced by the shape and number of red blood cells as well as other plasma constituents like fibrinogen, globulins, and albumins. It can be spuriously high in the absence of inflammation, as in anemia, nephritic syndrome, and hypergammaglobulinemia, and it can be spuriously normal in cryoglobulinemia and hemoglobinopathy.
ESR increases steadily with age, and the upper limit varies with sex; hence, ESR is difficult to interpret compared to CRP.
The concentration of CRP in serum is
more sensitive than ESR to evaluate and monitor inflammation, and it isindependent of factors that affect ESR. It correlates better with disease activity, and the rise in CPR level is seen
much earlier than that of other acute-phase reactants, usually 4 to 6 hours after tissue injury.
Both ESR and CRP levels can be elevated in a wide variety of conditions including trauma, infection, infarction, neoplasms, and inflammatory arthritis. Usually ESR and CRP levels correlate well, but in some patients levels may be discordant for reasons that are unclear. They are very useful in monitoring disease activity in rheumatologic conditions such as rheumatoid arthritis, polymyalgia rheumatica,2 and giant cell arteritis.
Some studies have shown that the pretreatment ESR value is of some prognostic value in polymyalgia rheumatica. Most patients with active lupus have normal or minimally elevated CRP levels, and markedly elevated concentrations of CRP in SLE should raise a suspicion of bacterial infection. Other causes for elevated CRP in SLE patients include serositis, synovitis, and vasculitis.
Prosthetic valves
Prosthetic mitral valve sounds:opening sound analogous to opening snap
closing sound coincides with S1
Prosthetic aortic valve sounds:
opening sound analogous to ejection click
closing sound coincides with S2
The combination of a history of calf pain on walking, absent peripheral pulses, and an ankle-brachial pressure index less than 0.9 indicate the presence of peripheral arterial disease with 95% sensitivity and specificity in these patients. However, peripheral vascular calcification can falsely raise the ankle-brachial pressure index (>1.3), particularly in patients with diabetes. Colour flow duplex ultrasound is indicated in any patient with dry gangrene, pain at rest, or a foot ulcer that is slow to heal
Peripheral arterial disease
The direct oral thrombin inhibitor dabigatran has a predictable anticoagulant effect and may be an alternative therapy to warfarin for patients who have acute venous thromboembolism. For the treatment of acute venous thromboembolism, a fixed dose of dabigatran is as effective as warfarin, has a safety profile that is similar to that of warfarin, and does not require laboratory monitoring. oral dabigatran, administered at a dose of 150 mg twice daily
Dabigatran versus Warfarin in the Treatment of Acute Venous Thromboembolism
December 6, 2009 NEJM
Heparin
This week’s question is on heparin and is taken from the onExamination revision questions for the MRCS Part 1 exam.Which of the following is true regarding heparin?
A It enhances antithrombin III activity
B It has no effect on platelet aggregation
C It induces thrombocytopenia in 20% of patients
D It is a strongly acidic protein
E It readily crosses the placenta
Answer
Answer A is correct.
Heparin is a strongly acidic mucopolysaccharide (not protein) and, as the name heparin implies, is derived from the liver.
Heparin has many actions, but principally it enhances antithrombin III activity, which in turn inhibits activated factors XII, XI, X, IX, and thrombin.
Heparin also activates lipoprotein lipase in plasma, lowering the plasma triglycerides and inhibiting platelet aggregation by fibrin.
A side effect in up to 5% of patients is heparin induced thrombocytopenia.
As heparin is so strongly acidic, it binds avidly to proteins and so it crosses the placenta and other membranes poorly.
Tuberculosis
Frequently Asked Questions about Tuberculosis by
DEPARTMENT OF RESPIRATORY MEDICINE, QUEEN ELIZABETH HOSPITAL in Malaysia.January 16, 2010
What does the result sputum direct smear AFB >50/L or 2/3L mean?>50/L means more than 50 AFBs are seen on one line on the slide under the microscope.2/3L means only 2 AFBs are seen on 3 lines on the slide. The letter L does not stand for litre. Obviously >50/L is more infectious than 2/3L and you can use this result to monitor your patient progress while on TB treatment.
When is it mandatory to admit a TB patient to the ward? Admit your TB patient if he develops complications such as massive haemoptysis or pneumothorax, if you suspect your patient will be non-compliant to treatment, poor family support or no proper home. TB involving the vital organs such as the brain, heart, adrenal glands, kidneys, spine etc also need admission.
What category of TB patient is infectious? Only pulmonary tuberculosis (TB of lung parenchyma) is infectious in the following order:-Smear positive case – very infectiousSmear negative but culture positive – less infectiousSmear negative and culture negative – not infectiousAll extra pulmonary TB are non-infectiousWhen does a smear positive TB patient become non-infectious? As a general rule, if the AFB germs are sensitive to the first line TB drugs, the patient will be non-infectious after one month of treatment.
What is the duration of treatment for TB lymphadenitis? At least 9 months. What is the duration of treatment for other extra pulmonary TB? Should be longer than 9 months since it is difficult to assess response to treatment in extra pulmonary TB unlike pulmonary tuberculosis where you can use chest X-ray. The duration is not fixed and you have to use good clinical judgment to decide the duration of treatment. The longer the duration of treatment, the less chance of relapse.
When do you give Isoniazide prophylaxis and what is the duration of prophylaxis? Isoniazide prophylaxis is a controversial issue but Isoniazide prophylaxis is given in only 2 conditions
• children under 5 years old who are contacts of smear positive cases with positive Mantoux AND
• HIV positive patients with positive Mantoux. The duration of prophylaxis is between 9 months to 1 year. IT IS IMPORTANT TO EXCLUDE ACTIVE TUBERCULOSIS BEFORE YOU DECIDE GIVING PROPHYLAXIS.
My patient develops mild pruritus or mild skin rash after initiation of TB treatment, what should I do? If it is just pruritus or very mild skin rash, reassure the patient and give symptomatic treatment; it is better to continue the TB drugs and advise the patient to come back if it gets worse. You can also give symptomatic treatment for mild gastro-intestinal upset.
My patient develops severe skin rash with anti-TB drugs; what should I do? Stop the TB drugs and review the patient regularly till the rashes subside. Thereafter, you start drug challenge (one drug at a time). The first drug you give is Isoniazide; please give full dose (based on patient's body weight) on the first day then followed by full dose of Rifampicin, Pyrazinamide, Ethambutol and or Streptomycin if necessary. Do not give low dose on day 1 and then increase gradually on day 2 and so on. The idea is to identify the offending drug. After you have identified the offending drug, please consult a respiratory physician for further advice.
My patient has raised liver enzymes; can I give anti-TB drugs? give anti-TB drugs if the liver enzymes are only twice elevated but if more than three times the normal limit, you have to wait till they normalize. If the patient develops hepatitis, you have to stop the treatment and wait till the hepatitis resolves. You may do re-challenge to identify the offending drug causing hepatitis. Giving lower dosage is NOT the way to prevent hepatitis as this can lead to resistance. In some cases where patients are very ill and smear positive with severe hepatitis, I do not do re-challenge as it is time consuming and I will advise you the alternate regimen to use.
My patient has TB but she is pregnant, are the TB drugs safe in pregnancy? Just give EHRZ. Streptomycin is contraindicated in pregnancy.My patient has TB but has renal failure; what regimen do I give? Just use HRZ regimen and prolong the duration of treatment. Streptomycin and Ethambutol are contraindicated in renal failure.
What is the re-treatment regimen for relapsed TB cases (cured of TB in the past and now AFB smear is positive again)?WHO recommends 2 months of SEHRZ, 1 month of EHRZ and 5 months of EHR ALL DAILY. Please send sputum for AFB culture and sensitivity in all relapsed PTB cases to ensure no resistant TB. Please review the AFB culture results.
What are the ‘10 principles’ of TB management? The ‘10 principles’ are: NEVER ADD A SINGLE DRUG TO A FAILING REGIMEN (repeat this 10 times and it becomes the ‘10 principles’). A single drug in a failing regimen is as good as monotherapy and this will lead to resistance to that drug.
How effective is BCG vaccination in preventing TB? BCG vaccination has been proven to be effective in reducing the risk of miliary TB and TB meningitis in children. It is not effective in preventing TB in adults. We are waiting for better TB vaccines in future.
Is steroid useful in tuberculous pleural effusion? No. I would not advocate steroid in tuberculous pleural effusion. A Spanish study and a report from South Africa showed no benefit of steroid in tuberculous pleural effusion. It is more important to achieve early complete drainage of the pleural effusion to prevent pleural fibrosis.
In a population-based study of over 30 000 subjects with no previous history of thyroid dysfunction, the prevalence of overt and subclinical hypothyroidism among women who were current smokers was significantly lower than for never-smokers
Graves' ophthalmopathy may be unilateral and may present before the onset of hyperthyroidism or for the first time many years after successful treatment.
It is more common in smokers.
Discuss the MMR vaccine and reassure the mother that risks,even in children with severe egg allergy, are very low. Ensure that other fears about the MMR vaccination, such as the unfounded bad publicity about MMR and autism, are discussed.
Although the vaccine is cultured in fibroblasts derived from chick embryos, the amount of egg protein in the vaccine is negligible and is most unlikely to trigger a reaction.
BMJ 2011;343:
The British Society for Allergy and Clinical Immunology and the National Institute of Allergy and Infectious Diseases recommend that all
children with an egg allergy, no matter how severe, should still have their MMR vaccine as per the usual immunisation schedule. Appropriate resuscitative facilities should always be available when any vaccinations are given, irrespective of egg
allergic status.
BMJ 2011;343:
Roughly, transudates are a result of increased pressure in the portal vein(>8 mmHg, usually around 20 mmHg), e.g. due to cirrhosis, while exudates are actively secreted fluid due to inflammation or malignancy. As a result, exudates are high in protein, high lactate dehydrogenase , have a low PH (<7.30), a low glucose level, and more white cell .
Transudates have low protein (<30g/L), low LDH, high pH, normal glucose, and fewer than 1 white cell per 1000 mm³. Clinically,
the most useful measure is the difference between ascitic and serum albumin concentrations. A difference of less than 1 g/dl (10 g/L) implies an exudate.
Portal hypertension plays an important role in the production of ascites by raising capillary hydrostatic pressure within the splanchnic bed.
Regardless of the cause, sequestration of fluid within the abdomen leads to additional fluid retention by the kidneys due to stimulatory effect on blood pressure hormones, notably aldosterone. The sympathetic nervous system is also activated, and renin production is increased due to decreased perfusion of the kidney. Extreme disruption of the renal blood flow can lead to hepatorenal syndrome. Other complications of ascites include spontaneous bacterial peritonitis (SBP), due to decreased antibacterial factors in the ascitic fluid such as complement.
In gastroenterology, the puddle sign is a physical examination maneuver that can be used to detect the presence of ascites. It is useful for detecting small amounts of ascites -- as small as 120 mL;
shifting dullness and bulging flanks typically require 500 mL.
Patient lies prone for 5 minutes
Patient then rises onto elbows and knees
Apply stethoscope diaphragm to most dependent part of the abdomen
Examiner repeatedly flicks near flank with finger. Continue to flick at same spot on abdomen
Move stethoscope across abdomen away from examiner
Sound loudness increases at farther edge of puddle
Sound transmission does not change when patient sits
In relation to auscultatory percussion, the puddle sign is more specific, but less sensitive.
Assessing for Ascites
A large belly with bulging flanks associated with an everted umbilicus suggests ascites, as normally, obesity protrudes forwards.This is a sensitive, but not very specific, sign.Fluid-filled flank will be dull on percussion.
Abdominal pain has several possible mechanisms and clinical patterns and warrants careful clinical assessment. Be familiar with three broad categories of abdominal pain:
1-Visceral pain occurs when hollow abdominal organs such as the intestine or biliary tree contract unusually forcefully or when they are distended or stretched. Solid organs such as the liver can also become painful when their capsules are stretched. Visceral pain may be difficult to localize. It is typically, though not necessarily, palpable near the midline, at levels that vary according to the structure involved.
Visceral pain varies in quality and may be gnawing, burning, cramping, or aching. When it becomes severe, it may be associated with sweating, pallor, nausea, vomiting, and restlessness.
2- Parietal pain originates in the parietal peritoneum caused by inflammation.It is a steady aching pain that is usually more severe than visceral pain and more precisely localized over the involved structure. It is typically aggravated by movement or coughing. Patients with this type of pain usually prefer to lie still.
Abdominal tenderness occurs as a result of irritation of the parietal peritoneum. While inflammation or irritation of the visceral peritoneum will cause abdominal discomfort, anorexia, and poorly localized pain, it will not cause tenderness and rigidity of the abdominal wall. Irritation or inflammation of the parietal peritoneum will stimulate the pain fibers of the parietal peritoneum and abdominal wall, creating the symptoms of localized pain and the signs of tenderness, rigidity, and rebound tenderness. Thus, if there is diffuse irritation of the peritoneum, as in diffuse peritonitis, there will be diffuse tenderness and rigidity.
3-Referred pain is felt in more distant sites, which are innervated at approximately the same spinal levels as the disordered structure. Referred pain
often develops as the initial pain becomes more intense and thus seems to radiate or travel from the initial site. It may be felt superficially or deeply but is usually well localized.
Pain may also be referred to the abdomen from the chest, spine, or pelvis, thus complicating the assessment of abdominal pain.
The abdominal wall skin should be inspected carefully for abnormalities.
Cullen's and Grey Turner's signs (bluish discoloration of the umbilicus and flanks, respectively) are related to intra-abdominal and retroperitoneal bleeding, and it is believed the blood dissects along fascial planes to reach these areas. Thus, one would want to question the patient diligently for causes of such bleeding—severe pancreatitis, trauma, or ruptured ectopic pregnancy.The skin should be inspected for striae, or "stretch marks," and surgical scars. The skin of the abdomen should also be checked carefully for engorged veins in the abdominal wall and the direction of blood flow in these veins. This is performed by placing the tips of the index fingers together, compressing a visible vein. The fingertips are then slid apart, maintaining compression, producing an empty venous segment between the fingers. A finger is removed from one end and the vein is watched for filling. The procedure is then repeated, but the opposite finger is removed and the vein again checked for filling.
Above the umbilicus, blood flow is normally upward; below the umbilicus, it is normally downward.
Obstruction of the inferior vena cava will cause reversal of flow in the lower abdomen.
In addition to these large dilated veins, note should be made of any spider angiomas of the abdominal wall skin.
dynamic auscultation:
respiration:
right sided murmurs are louder during inspiration,expiration has the opposite effect
squatting:
Increases venous return and peripheral resistance and results in almost all murmurs becoming louder the exception is in hypertrophic, obstructive cardiomyopathy where the dilatation of the left ventricle partially relieves the outflow obstruction
Valsalva manoeuvre:
this is expiration against a closed glottisThe patient is asked to hold his nose with his fingers, close his mouth and to breath out maximally (like straining at passing stool).
mitral valve prolapse - the systolic murmur becomes elongated
aortic stenosis - the systolic ejection murmur becomes softer mitral regurgitation - the systolic murmur becomes softer
hypertrophic cardiomyopathy - the late systolic murmur becomes louder