Anaphylaxis
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Anaphylaxis is a severe, life threatening, systemic reaction that can affect people of all ages. The underlying mechanism is the release of biologically active chemical mediators from mast cells or basophils, or from both.
Anaphylaxis involves one or both of:
• Respiratory difficulty (which may be due to laryngeal oedema or asthma)
• Hypotension (which may present as fainting, collapse, or loss of consciousness).
Anaphylaxis occurs in an acute and unexpected manner. You should give rapid treatment with adrenaline (epinephrine), steroids, and antihistamines to save life.
Your answer
Correct answera.
Shellfish allergy
b.
Egg allergy
c.
Vasovagal reaction
d.
Latex allergy
• A 35 year old man comes to see you. He is keen to have his thyroid function tested because his younger sister has just been diagnosed with hypothyroidism. His mother also suffered from this at an early age. You agree to do some blood tests. But within a few minutes of taking his blood he becomes acutely breathless with marked facial and tongue oedema. He tells you that he ate a prawn mayonnaise sandwich three hours earlier.
It is possible that he had a vasovagal reaction to venepuncture, but facial and tongue oedema are more consistent with an allergic reaction. The most likely cause of his reaction is latex allergy. His reaction occurred immediately after you took his blood. Much clinical equipment contains latex (for example, gloves, tourniquets, and sphygmomanometer cuffs). You should think of latex allergy if an allergic reaction occurs during a medical or dental procedure.
Your answer
Correct answera.
0.5 ml intramuscular adrenaline 1:1000
b.
0.5 ml subcutaneous adrenaline 1:1000
c.
0.5 ml intravenous adrenaline 1:1000
d.
0.5 ml intravenous adrenaline 1:10 000
• What dose of adrenaline would you give the patient?
You should give adrenaline as a priority to patients with anaphylaxis (respiratory difficulty, which may be due to laryngeal oedema or asthma, or hypotension, which may present as fainting, collapse, or loss of consciousness).The alpha adrenergic stimulation increases peripheral vascular resistance, improving blood pressure and coronary perfusion, reversing peripheral vasodilation, and decreasing angio-oedema.
Beta adrenergic stimulation produces positive inotropic and chronotropic cardiac effects, and
beta2 receptor stimulation causes bronchodilation.
You shouldn't give a subcutaneous injection because the adrenaline will be absorbed too slowly.
Intravenous administration is potentially dangerous and should be performed only during ECG monitoring by a trained physician.
• Learning bite
• Another differential diagnosis is angio-oedema.•
Angio-oedema may be associated with urticaria in 50% of cases. Angio-oedema involving the upper respiratory tract may result in life threatening airway obstruction. Angio-oedema usually responds to treatment with antihistamines and, in severe cases, steroids.
In a patient presenting with angio-oedema in the absence of urticaria adverse drug reactions (especially angiotensin converting enzyme (ACE) inhibitors and non-steroidal anti-inflammatory drugs) and C1 esterase inhibitor deficiency should be considered.
Tricyclic antidepressants (such as imipramine) and monoamine oxidase inhibitors (such as phenelzine) increase the effects of adrenaline and therefore increase the risk of cardiac arrhythmias.
You should give half the usual dose in patients taking these drugs. You should ideally stop these drugs and prescribe a safer alternative if there is an ongoing possibility that the patient may need adrenaline again.
Cocaine and amphetamines sensitise the heart to adrenaline. You shouldn't give adrenaline autoinjectors to patients who regularly use these drugs. You should give adrenaline only if the reaction is severe and does not respond to other interventions, including fluids, antihistamines, and steroids. They should be monitored with an ECG during administration if this is required.
Angiotensin converting enzyme inhibitors and angiotensin receptor blockers are associated with angio-oedema without urticaria. Any patient who gets anaphylaxis with angio-oedema while taking these drugs should stop them and take a suitable alternative.
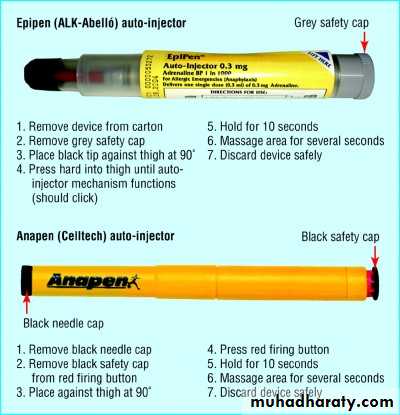
Learning bite
Techniques for using the two adrenaline autoinjectorsBefore you give the injection the patient reminds you that he suffers from mild hypertension, for which he takes atenolol 50 mg once a day. He is not taking any other medications and there are no documented drug allergies. You should halve the dose of adrenaline because of the increased risks associated with unopposed alpha-adrenergic stimulation of adrenoreceptors and reflex vagotonic effects. These can cause hypertension, coronary artery constriction, and bronchoconstriction.
You shouldn't give beta blockers to any patient you consider to be at risk of anaphylaxis without specialist advice. This includes eye drops containing beta blockers.
All patients who have had an anaphylactic reaction should be observed in an appropriate setting with resuscitation facilities for six to eight hours because of the risk of them having a "biphasic" or late reaction. This occurs in between 5% and 20% of patients with anaphylaxis. Giving antihistamines and steroids at the initial reaction may reduce the risk of a biphasic reaction.
You give 100-500 mg hydrocortisone and 10-20 mg chlorphenamine both intramuscularly. You then admit the patient to hospital.
Your patient later sees an allergist who diagnoses latex allergy. The allergist advises him about avoiding latex. He also prescribes two adrenaline autoinjectors. The patient returns to you a week later and asks when he should use the autoinjectors.
Patients should use an adrenaline autoinjector only when they get anaphylaxis.
You should tell patients to look for signs of:Respiratory difficulty (wheezing, shortness of breath, swelling of the tongue or throat)
Hypotension (blurred or lost vision, unsteadiness, dizziness, and a feeling that they are about to faint).
Cross reactive allergy
Allergic reactions to latex seem to be against proteins naturally present in latex sap. Patients who are allergic to latex may also be allergic to bananas, avocados, chestnuts, and kiwi fruit because of structurally similar proteins in these fruits that cross react. People who are allergic to avocado, chestnuts, or bananas have an increased risk of latex allergyAnother common cause of allergic reaction is drugs. For example, beta-lactam antibiotics may cause allergic reactions. Angio-oedema due to angiotensin converting enzyme inhibitors is not allergic in nature but due to bradykinin accumulation and occurs in 0.1% to 1% of patients prescribed these drugs. Most reactions occur within a few weeks of starting the drug, but reactions may occur up to 10 years after starting the drug.
• Learning bite
• Urticaria• Urticaria is a characterised by appearance of wheals which may accompany angio-oedema. Acute urticaria may be caused by sensitivity to foods, drugs such as antibiotics, non-steroidal anti-inflammatory drugs and opiates, blood products, and radio contrast media. It should be noted that urticaria can occur as a feature of viral infections or febrile illnesses. In 50% of cases the cause is not identified. The mainstay of acute urticaria management is the avoidance of allergen/cause and treatment with antihistamines.
Key points
Anaphylaxis is a severe, life threatening reaction.The severity of previous reactions does not reliably predict the severity of subsequent reactions
Using adrenaline (epinephrine) early in an anaphylactic reaction is associated with improved outcomes
Intramuscular adrenaline is the first line treatment for anaphylaxis. You should reserve intravenous adrenaline for unresponsive anaphylaxis or circulatory collapse (intravenous adrenaline should be given under cardiac monitoring).
Guidelines for managing a patient with anaphylaxis
Give oxygen
If the patient has wheeze, stridor, respiratory distress, or clinical signs of shock give adrenaline 1:1000 0.5 ml (500 µg) intramuscularly. Repeat the adrenaline after five minutes if the patient does not improve
Then give chlorphenamine 10-20 mg intramuscularly or slowly intravenously
For patients with severe or recurrent reactions and for patients with asthma, give hydrocortisone 100-500 mg intramuscularly or slowly intravenously
If clinical manifestations of shock don't respond quickly to drug treatment give 1-2 litres of fluids intravenously (crystalloid may be safer than colloid)
Salbutamol may be helpful if bronchospasm is severe and if it doesn't respond rapidly to treatment
If profound shock is immediately life threatening give cardiopulmonary resuscitation if necessary. Consider adrenaline 1:10 000 slowly intravenously (this is dangerous and should only be given by an experienced physician)
Clinical tips
You should give half doses of adrenaline to patients who are taking tricyclic antidepressants or beta blockersThe dose of adrenaline in an Epipen is 300 µg. The patient may need a second dose
Communication
Always tell your patients if they are allergic to a drugGive the patient information about medic alert bracelets
Tell your patients to mention their allergies to any other doctor they see
Always write the patient's allergies at the front of the notes
Put a system in place so all your staff know the patient has an allergy
You should observe all patients who have had an anaphylactic reaction in an appropriate setting with resuscitation facilities for six to eight hours. This is because of the risk that they may have a biphasic reaction.
Angio-oedema due to angiotensin converting enzyme inhibitors occurs in 0.1% to 1% of patients who take these drugs. Reactions can start at any time in the first year, and may even occur years after starting the drug.
If a patient develops angio-oedema while taking an angiotensin converting enzyme inhibitor you should immediately stop the drug, even if they have been on it for a long time. The frequency and severity of attacks increase if patients continue taking the drug. The reaction is a class effect, so all angiontensin converting enzyme inhibitors are contraindicated.
You should never prescribe these drugs for patients who have idiopathic angio-oedema. Patients who have had a reaction to angiotensin converting enzyme inhibitors have an increased risk of reacting to angiotensin receptor blockers.
In patients with anaphylaxis, beta blockers should be avoided because of the risks of adrenaline resistance and unopposed alpha adrenergic stimulation, which can cause hypertension, bradycardia, bronchoconstriction, and coronary artery constriction.
Clonidine is a centrally acting antihypertensive with an extensive side effect profile and would not be the initial second line agent in this situation.
Angio-oedema to ACE inhibitors is a class effect rather than an idiosyncratic effect and a history of idiopathic angio-oedema or previous ACE inhibitor induced angio-oedema is an absolute contraindication to their use.
In patients who are intolerant to ACE inhibitors because of angio-oedema there is a risk of cross reactivity with angiotensin II blockers; therefore these should be prescribed only in patients with strong clinical indications, such as left ventricular impairment or diabetic nephropathy, where the benefit exceeds the risks.
Patients who become hypotensive should lie flat and, if possible, raise their legs to increase venous return. Placing these patients suddenly into an upright position is potentially dangerous: it may precipitate a cardiac arrest (electromechanical dissociation) due to contraction of the empty heart.