Atrial fibrillation: diagnosis and management
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
"Atrial fibrillation is the most common cardiac arrhythmia, the prevalence of which is constantly increasing with advancing age. Despite advances in various treatment modalities, the burden of atrial fibrillation along with the associated morbidity and mortality remains significant.
Key points
The prevalence of atrial fibrillation is increasingMorbidity and mortality from atrial fibrillation predominantly result from the increased risk of stroke and worsening of heart failure
Control of both rate and rhythm have important roles in the management of patients with atrial fibrillation.
Monotherapy with standard beta blockers or rate limiting calcium antagonists is the first line of treatment in active patients requiring rate control.
Anticoagulation with warfarin is underprescribed, especially in elderly people
In patients who are at high risk of thromboembolic events, anticoagulation should be continued indefinitely even if sinus rhythm has been achieved.
Novel highly specific antiarrhythmic agents and direct thrombin inhibitors are being investigated
Why atrial fibrillation is important?
Atrial fibrillation is the most commonly encountered arrhythmia in clinical practice and is associated with considerable morbidity and mortality.In the UK atrial fibrillation affects:
5% of the population older than 65 years
10% of the population older than 75 years.
The number of patients with atrial fibrillation is likely to increase 2.5-fold to threefold by the year 2050, reflecting the growing proportion of elderly people. Men are 1.5 times more likely than women to develop atrial fibrillation.
The presence of atrial fibrillation increases morbidity or mortality by around twofold - this usually results
from stroke and heart failure.
The risk of embolic stroke increases fivefold in the presence of atrial fibrillation.
In the Framingham study database the risk of stroke increased from:
1.5% for patients aged 50-59 years to23.5% for those between 80 and 89 years.
Atrial fibrillation and the associated morbidity therefore represent a significant socioeconomic burden on the healthcare system. Indeed, the direct cost of health care for these patients rose from £244 million in 1995 (0.6-1.2%) to £459 million in 2000 (0.9-2.4%) of total NHS expenditure, based on figures from 2000.
Admissions to hospital and drug prescriptions accounted for 50% and 20% of this cost, respectively. £111 million cost towards nursing homes during this period.
Clinical identification of atrial fibrillation
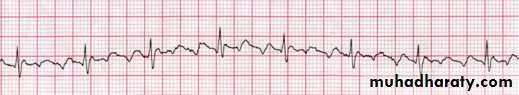
Atrial fibrillation is a supraventricular arrhythmia characterised by complete absence of coordinated atrial contractions. On the electrocardiogram (ECG) P waves are absent and are replaced by fibrillatory waves (Figure 1). Atrial fibrillation is associated with an irregular and frequently rapid ventricular response if the atrioventricular conduction is intact.Regular R-R intervals are possible when impulses are unable to pass through the AV node or the His-Purkinje system, during paced rhythm or when an accelerated ventricular or junctional rhythm dominates.
• Figure 1. Atrial fibrillation: absent P waves and irregular ventricular response
•Atrial fibrillation can also be commonly associated with other arrhythmias such as atrial flutter or atrial tachycardia.
Atrial flutter is a more organised and regular form of atrial activation resulting in a sawtooth pattern or flutter (f) waves on the ECG (Figure 2).
About 90% of atrial flutter involves a counterclockwise rotation in the right atrium. This pattern is often called typical or common atrial flutter. It is identified by the presence of:
A sawtooth pattern (negative flutter waves) in the inferior leads Positive waves in the chest lead V1.
Atrial flutter can arise during treatment of atrial fibrillation with antiarrhythmic drugs. Atrial flutter itself can degenerate into atrial fibrillation or the pattern can alternate between atrial fibrillation and flutter.
• Figure 2. Atrial flutter: flutter waves are clearly seen (sawtooth appearance). The rate of atrial contraction is 300 beats per minute. Ventricular response is regular as there is consistent 4:1 conduction giving a heart rate of 75 beats per minute. Note that the first atrial contraction within each cycle is partly superimposed on the preceding QRS complex
•
It is not uncommon for atrial fibrillation to be asymptomatic and diagnosed incidentally, especially in elderly people and when the ventricular rate is normal. Other patients may experience:
Frequent palpitations
Dizziness
Chest pain
Anxiety
Shortness of breath.
The symptoms of heart failure may be aggravated if atrial fibrillation supervenes.
Classification of atrial fibrillation
based on the temporal pattern of occurrence.
First detected is the first clinical presentation where the patient is still in atrial fibrillation, the onset of which may be unknown.
Paroxysmal is the occurrence of recurrent episodes that typically last minutes to hours, occasionally days (not more than seven), but eventually self terminate,
usually within 48 hours.
Persistent is present when arrhythmia has persisted for more than seven days, is not self terminating, and pharmacological or electrical cardioversion is required to restore sinus rhythm.
permanent when all attempts to restore sinus rhythm have been abandoned. If it is decided to cardiovert or ablate a rhythm that has been termed permanent atrial fibrillation, it should then be regarded as “persistent” atrial fibrillation.
What are the important pathophysiological mechanisms?
The mechanisms are not fully clear, but at least three aspects seem to be important in its genesis and maintenance.1. Enhanced automaticity
There may be enhanced automaticity within "sleeves" of atrial tissue (or sometimes other atrial sites) that extend into the pulmonary veins or vena caval junctions. These foci can act as trigger points to generate multiple atrial ectopics leading to atrial fibrillation. Their elimination or isolation by means of ablation can provide a permanent cure, particularly in people with structurally normal hearts.2. Maintenance of chaotic electrical state
In chronic atrial fibrillation, maintenance of arrhythmia is sustained by multiple re-entrant and randomly circulating wavelets that collide and divide into "daughter wavelets," thereby maintaining the chaotic electrical state. Salvos of ectopic beats arising from the pulmonary veins may repeatedly trigger and perpetuate the arrhythmia.3. Remodelling of atrial tissue
The longer the duration of atrial fibrillation, the more difficult it is to restore sinus rhythm and prevent recurrences. This is due to electrical and structural remodelling of atrial tissue resulting in shortening of atrial refractoriness, loss of myocytes, and progressive fibrosis, thereby maintaining and increasing the duration of atrial fibrillation.What causes atrial fibrillation?
Although rheumatic valvular disease remains the most common cause in developing countries, most patients develop atrial fibrillation against a background of systemic hypertension. They may also have coronary artery disease or heart failure.
Echocardiographic predictors of atrial fibrillation include:
• Large atria• Diminished ventricular function
• Increased left ventricular wall thickness.
Table 1. Causes and risk factors for atrial fibrillation
Cause or risk factorComment/example
Acute causes
Binge drinking,Cardiac and non-cardiac surgery,Myocarditis or pericarditis
Hyperthyroidism,Sympathomimetic medications,Recreational drug abuse
Neurogenic atrial fibrillation
High parasympathetic tone (evening, nocturnal episodes; part of “holiday heart syndrome”)
High sympathetic tone, (daytime episodes; associated with physical and mental stress)
Familial atrial fibrillation
Monogenic disease identified in a small group of patients
Familial variety seen in association with other genetically inherited monogenic (eg hypertrophic cardiomyopathy) or polygenic disorders. A familial pattern is observed because of larger prevalence of the arrhythmia12
Cardiovascular disease
Following myocardial infarction
Hypertension, especially if left ventricular hypertrophy
Congestive heart failure
Valvular heart disease (particularly mitral)
Congenital heart disease, mainly atrial septal defects
Following surgery for congenital heart disease
Sick sinus syndrome
Pulmonary disease
Chronic obstructive pulmonary disease, emphysema
Pulmonary hypertension
Pneumonia, bronchiectasis
Pulmonary embolism
Lung cancer
Other
Obesity
Sleep apnoea
Diabetes mellitus
When atrial fibrillation occurs in normal hearts without signs of any demonstrable cardiovascular or other underlying disease, it is described as
idiopathic or "lone" atrial fibrillation.
What are the key principles of management of atrial fibrillation?
Still represents one of the major therapeutic challenges in medicine. Based on current evidence and guidelines there are four main principles:• Restoring sinus rhythm by pharmacological or electrical means
• Urgent control of the ventricular rate during paroxysmal or persistent atrial fibrillation, and long term rate control in patients with permanent atrial fibrillation
• Preventing recurrence of atrial fibrillation following successful restoration of sinus rhythm
• Preventing thromboembolic consequences of atrial fibrillation.
When a patient is seen in an emergency setting the main priority is to control the rapid ventricular response. Depending on the haemodynamic status of the patient this can be achieved either by urgently restoring sinus rhythm or by controlling the ventricular rate.
Immediate electrical cardioversion is indicated in patients with a rapid ventricular rate who are either haemodynamically unstable or have evidence of acute myocardial ischaemia or heart failure that does not respond promptly to pharmacological measures.
In less acute situations, electrical or pharmacological cardioversion in the emergency department may be appropriate if the arrhythmia has been present for less than 48 hours.
Cardioversion by either means carries a risk of thromboembolism, particularly when the arrhythmia has been present for longer than 48 hours, necessitating initiation of anticoagulation before the procedure. It may therefore become necessary to postpone cardioversion until you can rule out the presence of left atrial thrombus.
In stable, rate controlled patients, this can be achieved by ensuring adequate anticoagulation (international normalised ratio (INR) 2.0-3.0) for a minimum of three weeks before electrical cardioversion
In patients where urgent reversal to sinus rhythm is necessary but where the duration of arrhythmia is either unclear or more than 48 hours you need to arrange a transoesophageal echocardiography to prove the absence of thrombus in the left atrium before electrical cardioversion
In the long run, in many patients the arrhythmia may become resistant to cardioversion and may be accepted as permanent. Recent studies have shown that ventricular rate control for atrial fibrillation may be at least as effective as restoration of sinus rhythm in terms of survival and symptom control, particularly in elderly patients.
Electrical cardioversion
Direct current cardioversion involves delivery of synchronised electrical energy across the chest wall. Success rates vary between 65% and 90%. The success of direct current cardioversion appears to be greater with anteroposterior paddle positioning (sternum and left subscapular) than with anteroapical (ventricular apex and right infraclavicular).Other factors influencing the success of direct current cardioversion include:
• The nature of any underlying heart disease• Transthoracic electrical resistance
• Defibrillator output waveform (biphasic is better than monophasic).
Elective direct current cardioversion is performed under short acting general anaesthesia. In an emergency the need for anaesthesia depends on the nature of the emergency and the level of consciousness. It is also reasonable to perform direct current cardioversion under conscious sedation.
In recent reports, elective direct current cardioversion performed under conscious sedation was shown to be safe and not associated with any intolerable discomfort to the patient.
It is safe to cardiovert patients with implanted devices such as a permanent pacemaker or internal defibrillator provided the implanted device is interrogated immediately after cardioversion for any malfunction. The paddles used for cardioversion should be placed as far as possible from the implanted device, preferably in the anteroposterior position.
Pacemaker output may need to be increased to its maximal output before and a day or two after the cardioversion. This is because cardioversion may cause a major and temporary increase in the pacing threshold.
Brief arrhythmias can arise immediately following direct current cardioversion. These are mainly ventricular and supraventricular premature beats, bradycardia, and short periods of sinus arrest. Ventricular tachycardia or fibrillation can be precipitated in patients with hypokalaemia and digitalis intoxication.
Patients with underlying conduction defects are at risk of developing profound bradycardia, complete heart block, or asystolic periods following cardioversion. These patients are identified by having a slow ventricular response to atrial fibrillation in the absence of rate reducing medications. External or temporary pacemaker facilities must be at hand before attempting cardioversion.
Pharmacological cardioversion
Before considering antiarrhythmic therapy, it is important to realise that around 60% of patients with paroxysmal atrial fibrillation spontaneously cardiovert to sinus rhythm within a few days (mostly within 24 hours). Pharmacological cardioversion is considered in patients who are haemodynamically stable and is frequently successful if initiated within two to seven days of onset of atrial fibrillation.
Pharmacological cardioversion is considered in patients who are haemodynamically stable and is frequently successful if initiated within two to seven days of onset of atrial fibrillation.
Several antiarrhythmic drugs may be effective in a given patient and the initial selection is based mainly on safety.
Current guidelines on the management of atrial fibrillation recommend use of propafenone, flecainide, or amiodarone as the first line choice for pharmacological cardioversion with conversion rates of up to 90%.
Class Ic agents
Class Ic agents (flecainide and propafenone) are safe in patients who do not have evidence of previous myocardial infarction, acute myocardial ischaemia, or ventricular dysfunction.Class III agents
Although not available in the UK, both dofetilide and ibutilide are relatively new class III agents and are particularly useful for cardioverting atrial flutter to sinus rhythm.
In clinical practice, amiodarone is a reasonable alternative to class Ic agents and is the drug of choice in patients with ventricular dysfunction and ischaemic heart disease. Amiodarone also has an added advantage of providing prompt rate control in addition to its antiarrhythmic effect. This rate controlling effect (beta blockade and calcium channel blockade properties) is observed early following intravenous loading; the class III antiarrhythmic properties taking effect between eight and 24 hours.
Intravenous amiodarone should be administered preferably via a central vein or through a large peripheral vein to prevent phlebitis. Most of the toxicity of amiodarone is dose dependent and related to chronic treatment. Amiodarone should still be used with caution in patients with acute ischaemia or myocardial dysfunction because profound hypotension may be induced by intravenous or high dose oral loading.
Sotalol is a beta blocker with class III properties, but is more commonly prescribed to prevent recurrences of paroxysmal atrial fibrillation and to maintain sinus rhythm following successful direct current cardioversion. There is, however, an increased incidence of QT prolongation and polymorphic ventricular tachycardia with use of the drug.
Evidence
In randomised trials comparing flecainide, propafenone, and amiodarone for cardioversion of acute atrial fibrillation, 90%, 72%, and 64% success rates were achieved, respectively, with the use of these drugs. Another study compared oral amiodarone with sotalol and showed that both drugs are equally effective in achieving pharmacological cardioversion of atrial fibrillation to sinus rhythm.Amiodarone was found to be superior to sotalol for maintaining sinus rhythm, but both drugs had similar efficacy in patients with ischaemic heart disease.
Can certain drugs prevent recurrences of atrial fibrillation and provide long term maintenance of sinus rhythm?
The relapse rate of atrial fibrillation following initial cardioversion is high (25-50% at one month).
Maintenance of sinus rhythm after successful cardioversion is achieved by continuing oral therapy with
class Ia (quinidine and disopyramide),
class Ic (flecainide and propafenone), or
class III (sotalol and amiodarone) antiarrhythmic drugs. Pretreatment with these drugs also improves success rates of repeated direct current cardioversion.
Class Ic drugs appear to be more effective and better tolerated than class Ia drugs. Quinidine is less commonly used than disopyramide as it has a higher incidence of drug related proarrhythmias. (Proarrhythmia are new or more frequent occurrences of pre-existing arrhythmias, paradoxically precipitated by antiarrhythmic therapy.)
Sotalol and amiodarone are commonly used to prevent recurrences of paroxysmal atrial fibrillation. Amiodarone may be more efficacious than sotalol in preventing recurrences, but long term use is limited by non-cardiac side effects (such as those affecting the skin, liver, lung, and thyroid gland). Class Ic agents can be combined with sotalol or amiodarone.
It is vital to bear in mind the proarrhythmic effects from use of antiarrhythmic agents. These drugs (amiodarone less often) can prolong the QT interval and lead to dangerous polymorphic ventricular arrhythmias. Regular monitoring of the corrected QT interval (class Ia and class III) and QRS duration (class Ia and class Ic) on the 12 lead ECG is therefore important during outpatient reviews.
The presence of renal insufficiency and electrolyte imbalances also predispose to polymorphic ventricular tachycardia in patients treated with sotalol.
AV nodal blocking agents
In selected patients AV nodal blocking agents (for example beta blockers, calcium channel blockers, and digoxin) can be combined with class I agents (flecainide and propafenone) depending on the level of control of the atrial fibrillation.Recent advances
Evidence is emerging for the role of inflammation and fibrosis in maintaining atrial fibrillation. In recent trials statins, angiotensin converting enzyme (ACE) inhibitors, and angiotensin receptor blockers have been effective in preventing recurrences of atrial fibrillation.
Statins may achieve some efficacy through an anti-inflammatory mechanism, while ACE inhibitors and angiotensin receptor blockers reduce apoptosis and fibrosis. Angiotensin receptor blockers were found to be superior to beta blockade in preventing recurrences of new onset atrial fibrillation in hypertensive patients with left ventricular hypertrophy in a recent subanalysis of the LIFE trial.
Does the presence of structural heart disease affect the choice of antiarrhythmic medication?
In patients with no or minimal structural heart disease, flecainide, propafenone, and sotalol are recommended as first choice of therapy because they are well tolerated and have no long term extracardiac side effects.
Flecainide and propafenone should be avoided in patients with heart failure and coronary artery disease because of the risk of ventricular proarrhythmia and sudden cardiac death.
Sotalol should be avoided in patients with hypertension and left ventricular hypertrophy due to the increased risk of QT prolongation and proarrhythmia.
Amiodarone is the drug of first choice in the presence of heart failure and left ventricular hypertrophy. Patients with coronary artery disease can be prescribed sotalol provided there is no heart failure.
For patients with hypertension but without left ventricular hypertrophy, flecainide and propafenone offer a better safety profile and are recommended.
Which patients with atrial fibrillation should be offered rate control?
It is necessary to provide long term rate control when atrial fibrillation is regarded as permanent.Rate control is also a preferred strategy in patients with paroxysmal atrial fibrillation who are stable at presentation; a significant proportion of these patients can spontaneously revert to sinus rhythm within 24-48 hours.
The aim of rate control in atrial fibrillation is to improve symptoms and prevent worsening of ventricular dysfunction. Recent evidence from randomised trials (AFFIRM, PIAF, RACE, and STAF) has shown that rate control is at least as effective as rhythm control in improving symptoms and functional capacity, particularly in people older than 65 years.
The AFFIRM trial recruited the largest number of patients (n=4060), who were randomised either to rate control with digoxin, standard beta blockers, diltiazem, and verapamil, or to a strategy of obtaining and maintaining sinus rhythm using amiodarone, sotalol, propafenone, and flecainide. Follow up period was 3.5 years. Mortality rates were not significantly different between the two groups, but there was a trend towards more strokes in the rhythm control group due to discontinuation of anticoagulation on regaining sinus rhythm.
What is considered adequate rate control remains controversial. The heart rate is considered to be controlled when the ventricular rate is 60-80 beats per minute at rest and 90-115 beats per minute during exercise.
Rate control is achieved with drugs that predominantly affect conduction through the AV node. Commonly used agents are:
Digoxin
Standard beta blockers (atenolol, propranolol, metoprolol, and sometimes esmolol)Non-dihydropyridine calcium channel blockers (verapamil and diltiazem).
In atrial fibrillation digoxin can usually provide adequate rate control, but does not prevent excessive heart rates during exercise or in other conditions that increase adrenergic activity. Combination therapy with digoxin and beta blockers or calcium antagonists may be necessary, especially in younger, active patients.
Caution with combination therapy must be exhibited in elderly patients who may have underlying degenerative sinus or AV node disease.
In stable patients with acute atrial fibrillation or during hyperadrenergic states (for example due to fluid loss, fever, or hyperthyroidism) calcium antagonists or beta blockers (oral or intravenous) are preferred over digoxin because of their relatively rapid onset of action. Digoxin should therefore be restricted to sedentary, less active patients requiring rate control.
Patients who are not adequately rate controlled on a single agent can be given combination therapy, such as digoxin with beta blockers or calcium antagonists to optimise AV nodal blockade without encountering side effects from the use of large doses of single drugs.
Recent advances: what if rate control fails?
It may at times be difficult to control the ventricular rate and related symptoms in certain patients, particularly with permanent atrial fibrillation. There is then an option to completely block the AV conduction by AV node radiofrequency or cryoablation followed by the implantation of a permanent ventricular pacemaker.Patients with sick sinus syndrome commonly present with episodes of bradycardia alternating with periods of fast atrial fibrillation. These patients may also require the support of a permanent atrial or dual chamber pacemaker to allow increase in the dose of rate controlling medications. Selective atrial pacing methods to prevent recurrences of atrial fibrillation have generally been unsuccessful.
Should all patients with atrial fibrillation be anticoagulated?
Atrial fibrillation once controlled causes little direct damage, but the risk of peripheral thromboembolism remains significant and increases with age from:
1.5% in patients younger than 60 years to
24% in patients older than 80 years
The overall risk of stroke is increased fivefold in the presence of atrial fibrillation. This risk is significantly reduced with the use of warfarin. Warfarin is superior to aspirin but is underprescribed in clinical practice.
Up to 40% of people with a high risk of thromboembolism may not be receiving adequate anticoagulation.
More than half of patients with atrial fibrillation in the community are older than 75 years and a significant proportion of these may be denied warfarin on the assumption of increased risk of haemorrhagic complications. Antithrombotic therapy with warfarin or aspirin should be considered for all patients with atrial fibrillation depending on individual suitability and assessment of risks and benefits.
Old age, hypertension, diabetes mellitus, previous cerebrovascular accidents, left ventricular dysfunction, co-existent ischaemic or valvular heart disease, hyperthyroidism, and presence of prosthetic valves are considered as high risk factors for thromboembolism in atrial fibrillation.
Guidelines on atrial fibrillation recommend that high risk patients, even if they are successfully maintained in sinus rhythm, must receive long term anticoagulation with warfarin unless contraindicated.
In the absence of these factors (age <65 with no other high risk conditions) or when warfarin cannot be given, aspirin is an alternative.
Young patients with structurally normal hearts and no other identifiable risk factors (lone atrial fibrillation) are not at substantial risk and may be treated with aspirin.
Patients with paroxysmal atrial fibrillation should receive long term anticoagulation if they have risk factors for thromboembolism as mentioned above, and not on the basis of frequency or severity of paroxysms.
Treatment with warfarin requires regular monitoring of the INR, which should be adjusted to between 2.0 and 3.0. Risk of intracranial haemorrhage increases significantly at an INR greater than 3.0
Recent advances:
Limitations of warfarin have led to an ongoing search for new anticoagulants with predictable pharmacokinetics and improved safety profiles.Because thrombin plays a key role in the propagation of thrombus formation, orally administered direct and indirect thrombin inhibitors are being investigated. Among these agents, ximelagatran was in the most advanced phase of development, but has been withdrawn due to unpredictable liver damage during long term treatment.
The safety profile of another product, dabigatran, is under trial.
The efficacy and safety of combined antiplatelet treatment, with aspirin plus clopidogrel compared with warfarin or aspirin alone in preventing ischaemic stroke in atrial fibrillation (ACTIVE group of trials) is also under trial. The warfarin arm (ACTIVE-W) was recently withdrawn because there was a higher incidence of ischaemic stroke in those receiving combinations of aspirin and clopidogrel, compared with those receiving warfarin.
Recent advances: non-pharmacological techniques to prevent thrombus formation
In patients with atrial fibrillation, more than 90% of thrombi form in the left atrial appendage.Surgical ligation or removal of the left atrial appendage has previously been tried, mainly in patients undergoing valve surgery.
Recent techniques allow percutaneous left atrial appendage transcatheter occlusion (PLAATO or Watchman devices). A self expanding inert device is placed in the left atrial appendage under fluoroscopic and transoesophageal echocardiographic guidance. Trials are underway to evaluate the long term safety and efficacy of this technique.
Can atrial fibrillation be permanently cured?
Several non-pharmacological treatments are now available that provide symptom control and reduce the risk of stroke. These include:• Catheter ablation therapy
• Device therapy
• Surgery.
These treatments are usually reserved for younger patients with relatively normal hearts. Significant effort is being devoted to percutaneous catheter based ablation of triggers of atrial fibrillation (atrial premature beats, monomorphic atrial tachycardias, atrial flutter).
Most (>90%) of these triggers are now known to arise from sleeves of atrial tissue with abnormal automaticity present within the pulmonary veins.
The procedure involves the use of radiofrequency or cryoenergy to isolate pulmonary veins or other sites generating triggers of atrial fibrillation, the risk of recurrence is high (30-50%) in the first year making further attempts at ablation necessary.
Catheter based techniques can at times lead to systemic embolism and pulmonary vein stenosis, especially if multiple sites are ablated.
The circuit involved in typical atrial flutter lies within the right atrium and can be mapped accurately. The flutter circuit usually involves a narrow bridge of tissue between the tricuspid valve and the inferior vena cava (cavotricuspid isthmus).
Ablation across this area effectively blocks atrial flutter, achieving almost 100% long term success.
The surgical maze procedure is a technique designed to prevent the spread of multiple waves of depolarisation in the atrial tissue. Linear lines of conduction blocks are created in the right and left atrial tissue either by incision or by using newer ablation sources. The resultant linear scarring prevents chaotic activity by allowing depolarisation wavelets to travel in a similar direction.
Nonetheless, the maze procedure is associated with complications arising from major open heart surgery and is therefore usually performed in patients requiring cardiac surgery for other reasons.
Future developments
Several new antiarrhythmics with improved safety profiles and novel mechanisms of action are under investigation. These include:Dronedarone – a modified, deiodinated analogue of amiodarone
Stretch receptor antagonists
Gap junction modulators
Multichannel blockers
Adenosine analogues
Agents with highly selective action on ion channels (for example, vernakalant).
Warfarin is more effective than aspirin or combination therapy with aspirin and clopidogrel for the prevention of thromboembolism in those at high risk of ischaemic stroke. The ACTIVE–W arm of trials was prematurely discontinued.
The rate of ischaemic stroke in atrial fibrillation is related to coexistent cardiovascular disease and is similar in people with recurrent and permanent atrial fibrillation.