Bradycardia
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Key points
Bradycardia is a heart rate of less than 60 beats per minute ,Symptoms can include dizziness, chest pains, and collapse,Bradycardia may be physiological or pathological,Bradycardia can be divided into :• sinus bradycardia,
• sick sinus syndrome, and
• atrioventricular block
Bradycardia can be caused by a wide range of conditions, but is usually degenerative and related to ageing
Electrical pacing is the safest and best approach for treating persistent symptomatic bradycardias
A detailed past medical and drug history may indicate a potential cause of the bradycardia.
Clinical tip
Assess the patient looking for evidence of haemodynamic compromise as a result of the bradycardiaWhy is bradycardia important?
Bradycardia is common. Recent estimates put the prevalence of atrioventricular block at 0.1% in women and 0.2% in men. The effect of these bradycardias on cardiovascular mortality is unclear, but there is significant morbidity and mortality in older patients as a result of falls or collapse. The management of bradycardia includes inserting a permanent pacemaker: around 25 000 are inserted each year in the NHS at a cost of £43m per year.
Clinical identification of bradycardia
Bradycardia is a heart rate of less than 60 beats per minute. It can be normal (physiological), for example during sleep, or a sign of underlying cardiac or non-cardiac pathology. It may also be associated with sinus arrhythmia especially in young people - this causes a variation in heart rate related to respiration. Bradycardia is often asymptomatic but symptoms can include dizziness, collapse, and hypoxic seizures.Classification
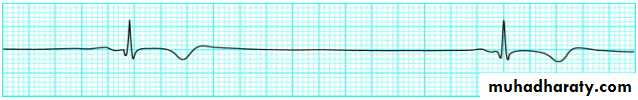
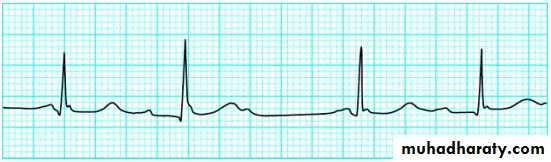
Sinus bradycardiaAs the name implies, sinus bradycardia is a heart rate of less than 60 beats per minute, where every QRS complex is preceded by a P wave, and the PR interval is between 0.12 and 0.20 seconds (between three and five small squares on a normally calibrated ECG).
It is frequently physiological and is often seen in young adults and athletes, and during sleep. A common pathological cause of sinus bradycardia is acute myocardial ischaemia, especially inferior myocardial infarction (thrombus in the right coronary artery) because this arterial territory provides blood supply to both the sinoatrial and atrioventricular nodes. Ischaemia may be associated with severe bradycardia, as seen in Figure 1.
• Figure 1. Sinus bradycardia
•Figure 1. Sinus bradycardia
Other causes of sinus bradycardia include:• Drugs (eg beta blockers, amiodarone, digoxin, rate limiting calcium antagonists)
• Hypothermia
• Hypothyroidism
• Obstructive jaundice
• Sick sinus syndrome
• Raised intracranial pressure.
Sick sinus syndrome
Sick sinus syndrome is the term for situations arising from the failure of the sinoatrial node to generate and conduct impulses. This can present on the ECG as:
Persistent severe sinus bradycardia
• Sinoatrial block
• Sinus arrest
• Tachycardia-bradycardia syndrome.
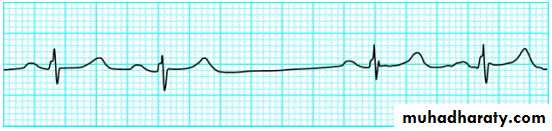
• 2).
• Figure 2. Sinoatrial block•
Figure 2. Sinoatrial block
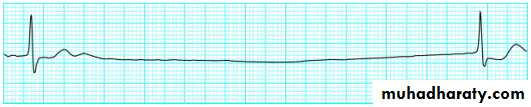
Sinoatrial block is a failure of the impulse generated in the sinus node to depolarise the atria. This results in a pause without P waves. This pause is either two, three, or four times the normal P-P interval (Figure 2).Sinus arrest is a term applied to a period without any P wave activity. It represents failure of impulse formation, rather than transmission, at the sinoatrial node (Figure 3). Again there is a pause, but the pause is NOT a multiple of the normal P-P interval.
• Figure 3. Sinus arrest
•
Figure 3. Sinus arrest
Escape rhythms happen when the normal conduction fails to occur, and are caused by depolarisation from a subsidiary pacemaker located within the atria, atrioventricular junction, or the ventricles. They are always associated with a rate that is slower than the intrinsic sinus rate and therefore result in bradycardia. The morphology and rate of the escape rhythm depends on the location of the pacemaker. For instance, a junctional escape rhythm will have a normal QRS complex and a rate of 50 to 60 beats per minute, whereas a ventricular escape rhythm will have broad QRS complexes and a rate of 15 to 50 beats per minute.
Tachycardia-bradycardia syndrome commonly occurs in sick sinus syndrome, and refers to periods of atrial tachycardia, atrial fibrillation followed by periods of sinus bradycardia, or sinoatrial block.
Atrioventricular block
This can be defined as a problem with the transmission of atrial depolarisation to the ventricles, and is classified according to the severity of that problem into first, second, and third degree. Age related idiopathic fibrosis of the specialised conducting tissue is the most common cause of atrioventricular block. Other causes include:• Myocardial ischaemia or infarction
• Degeneration of the His-Purkinje system
• Infection (for example Lyme disease or diphtheria)
• Drugs
• Immunological disorders (for example systemic lupus erythematosus)
• Cardiac surgery
• Congenital causes
• Cardiomyopathies, especially mitochondrial myopathy and dystrophia myotonica.
First degree
First degree heart block is a delay of more than 0.2 seconds (five small squares) in the PR interval, as measured from the beginning of the P wave to the beginning of the QRS complex. This represents delay in depolarisation of the ventricles after an appropriate P wave. The delay usually occurs at the level of the atrioventricular node and is fixed. This means the PR interval is unchanged from heart beat to heart beat (Figure 4).Figure 4. First degree heart block
Second degree
Second degree heart block can be described as an intermittent or partial failure of conduction between the atria and the ventricles, and is further divided into two main types:• Mobitz type I block
• Mobitz type II block.
In Mobitz type I block (also known as the Wenckebach phenomenon) the delay usually occurs at the atrioventricular node. There is an increasing delay in the transmission of the atrial impulse to the ventricles. On the ECG you see a lengthening of the PR interval with each heart beat. Complete block ultimately occurs, in which a P wave occurs in isolation with no subsequent QRS complex. After this the PR interval returns to normal and the process repeats itself (Figure 5).
• Figure 5. Mobitz type I block
•Figure 5. Mobitz type I block
In Mobitz type II block the PR interval is maintained from beat to beat, although it may be prolonged. Here the problem lies in an intermittent failure in activation of the ventricles from the atria. There are therefore P waves without a following QRS complex. This can be variable, and the greater the failure rate (that is three or more P waves before a QRS complex) the greater the risk of developing complete heart block (Figure 6).• Figure 6. Mobitz type II block
•Figure 6. Mobitz type II block
Third degree (complete heart block)
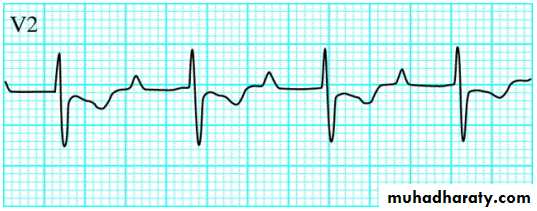
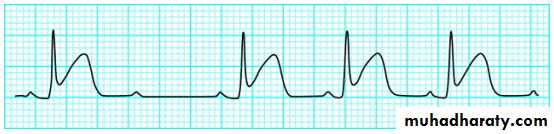
This term applies to complete dissociation between atrial and ventricular depolarisations. The atria often depolarise at a normal rate, while ventricular depolarisation is initiated from a pacemaker within the ventricles themselves, giving a slower depolarisation rate and wide QRS complexes. There are therefore always more P waves than QRS complexes and no consistent relationship between the two. The precise morphology of the QRS complex will vary depending on the location of the pacemaker within the ventricle. The contraction rate of the ventricles without pacemaker activity from the atria is around 40 beats per minute (Figure 7).
• Figure 7. Third degree heart block. (Arrows show P waves) Top: a pacemaker in the bundle of His produces a narrow QRS complex. Bottom: more distal pacemakers tend to produce broader complexes.
•
Figure 7. Third degree heart block. (Arrows show P waves) Top: a pacemaker in the bundle of His produces a narrow QRS complex. Bottom: more distal pacemakers tend to produce broader complexes.
Key management principles
Management options for patients with bradycardia and heart block are limited.If you think the bradycardia is related to an underlying cause (such as drugs, acute myocardial infarction, or pulmonary embolus) you should treat the underlying cause
If the bradycardia or block is asymptomatic the patient often only needs observation. However, there is evidence of prognostic benefit in asymptomatic patients with Mobitz type II and complete heart block for inserting a permanent pacemaker. (Class 2a indication)
Acute management
In the acute situation you should manage patients with symptoms of bradycardia, such as hypotension, chest pain, or dizzy spells, in an area with appropriate resuscitation and monitoring equipment. Symptomatic patients and those with a heart rate of <40 require treatment. Atropine at an initial dose of 0.5-1.0 mg is the first choice, but is effective only for sinus bradycardia.Repeated doses may be necessary (maximum 3 mg) but you should consider pacing if this is ineffective. Also consider using adrenaline, isoprenaline, or aminophylline. Think about glucagon intravenously if you think the bradycardia is due to beta blockers or calcium channel blockers.
Electrical pacing is the safest and best approach in the acute setting. You should use external pacing leads or temporary pacing.