Broad complex tachyarrhythmias
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Key points: diagnosis
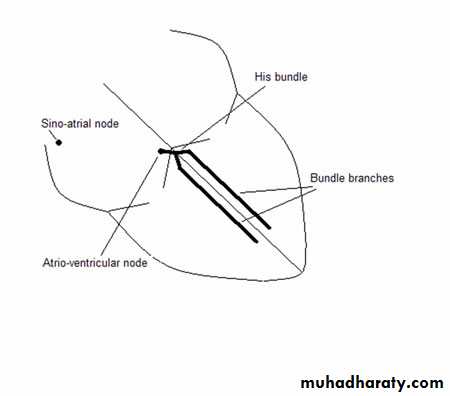
A tachyarrhythmia is defined as a fast heart rhythm of at least three beats, with a rate of over 100 beats per minute. The rate refers to the chamber driving the arrhythmia. Arrhythmias dependent on the atrioventricular node or originating above it are defined as "supraventricular tachycardias" and those below as "ventricular tachycardias" (Figure 1)It is possible in many cases to diagnose the exact mechanism of the tachyarrhythmia by looking at the ECG:
While the patient is having the tachyarrhythmia, and then
When they are in sinus rhythm
It is extremely important to get a high quality 12 lead ECG during the tachyarrhythmia, where possible. You can obtain further information from a rhythm strip or, preferably, from a 12 lead ECG:
At the onset of the tachyarrhythmia
During changes in the tachyarrhythmia
During diagnostic manoeuvres
At its termination
The haemodynamic state of the patient in tachyarrhythmia does not necessarily point towards a particular diagnosis
An initial assessment of the ECG should take in all major abnormalities that might point to a diagnosis, but important points to note are:
Is the QRS complex narrow or broad?
Is atrial activity discernible? (Are there obvious P waves occurring reproducibly? Are they all of similar morphology or do they vary?)
Is there an apparent causal relationship between atrial and ventricular activity?
Figure 1. A schematic of the conducting system. Normal activation spreads from the sino-atrial node through the atrioventricular node, the bundle of His, and the bundle branches and then into the ventricular myocardium.
Key points: treatment
There are a number of principles:Urgent treatment
The patient should be cardioverted if urgent treatment is needed because of haemodynamic instability; for example if the blood pressure is less than 90 mm Hg or if pulmonary oedema is present.
Acute treatment
For ventricular tachycardia intravenous procainamide, lidocaine, and amiodarone are effective. Electrical cardioversion may be needed in many cases. Check serum potassium and replace, aiming for 5 mmol/l. If potassium is low, consider replacing magnesium also.
Chronic treatment
For ventricular tachycardia, discussion with or review by a cardiac electrophysiologist is recommended for consideration of an implantable defibrillator or antiarrhythmic medication.
Broad complex tachyarrhythmias
There are four causes of broad complex tachyarrhythmias:• Ventricular tachycardia
• Pre-excited tachycardia
• Supraventricular tachycardia with aberrant conduction
• Paced rhythm where the rate is greater than 100 beats per minute.
As with narrow complex tachyarrhythmias, an electrophysiological study may be needed to define the exact mechanism.
Ventricular tachycardia
1. Monomorphic ventricular tachycardia
This usually occurs in people with structural heart disease and involves a re-entrant arrhythmia circulating around and/or through an area of scar. The rhythm is usually regular and monomorphic because of the fixed-sized scar, although there may be some variation at the start.
Rates are usually between 150 and 200 bpm but they can vary. There may be some irregularity, particularly at the start of the rhythm. The QRS is broad and bizarre, although if it originates near to the normal conducting system it can be narrower.
Look for signs of independent atrial activity; that is atrial activity that has no relation to ventricular activity. If you see this, the diagnosis is ventricular tachycardia (except in very rare circumstances). This activity may be difficult to see because of the broad QRS and particularly at fast ventricular rates. Independent atrial activity is indicated by a number of ECG findings:
The presence of more QRS complexes than P waves
• Capture beats - this occurs when continuing atrial activity manages to capture the heart producing a normal, slightly early QRS
• Fusion beats - if only part of the ventricle is activated by the ventricular tachycardia and part by atrial activity, fusion is seen. The QRS complex occurs slightly earlier than expected.
It is possible for the atria to be activated regularly by the ventricular tachycardia producing 1:1 retrograde P waves; therefore VA association does not exclude ventricular tachycardia. This would usually occur at slower ventricular tachycardia rates.
Atrioventricular dissociation during tachycardia is also demonstrated by detecting cannon “a” waves in the jugular vein pulse.
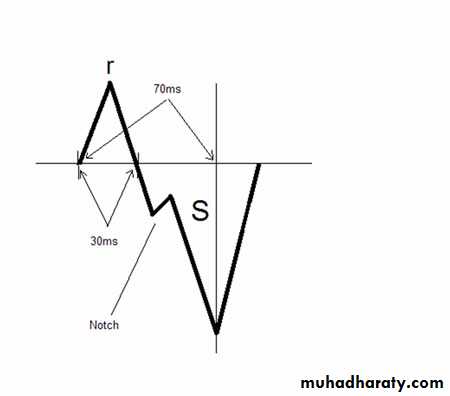
If the QRS complexes have a left bundle branch block type pattern, features suggestive of ventricular tachycardia are:
QRS width >160 ms
An r wave present in V1 or V2 that is >30 ms in width (Figure 20).
Time from the start of the r wave to the nadir of the S is >70ms in V1 or V2 where an rS complex is present
A notched S in V1 or V2
A qR complex in V6
An inferior axis (the QRS complexes are positive in inferior leads) or right axis deviation.
Figure 20. A schematic of a QRS complex, illustrating some features suggestive of ventricular tachycardia.
If there is a right bundle branch block type pattern, features suggestive of ventricular tachycardia are:
QRS width >140 ms
Any pattern in V1 differing from an rSR' with the S wave extending beyond the baseline
The presence of a qR, QR, or RS complex in V1
An R:S ratio in V6 of <1
A superior axis (negative in inferior leads).
Other features suggestive of ventricular tachycardia are:
QR complexes in any lead often suggesting ventricular tachycardia due to an old infarctionA narrower QRS than in sinus rhythm
An RS complex present in the chest leads and the time from the start of the R to the deepest part of the S is >100 ms
Positive concordance (the only differential here is an antidromic tachycardia due to a left posterior accessory pathway)
Negative concordance
(positive concordance means that all of the QRS complexes are clearly positive in all of the chest leads; negative concordance means that they are all negative)
A similar morphology of ventricular ectopics in SR to the tachyarrhythmia.
However, remember that breadth or bizarreness of QRS complex is no longer applicable if there is pre-excitation, with pre-existing bundle branch block, or in the context of class Ic antiarrhythmics. If you are still unsure about the diagnosis, treat the patient as if they have ventricular tachycardia until proved otherwise.
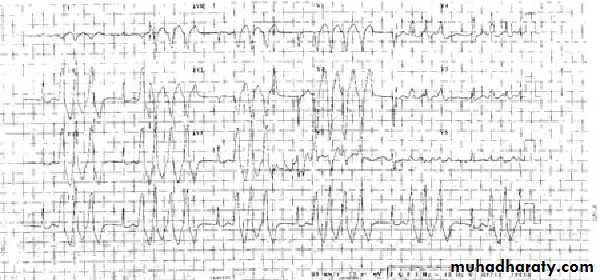
• 2. Polymorphic ventricular tachycardia
• This can occur in two forms:
• Torsades de pointes, which is associated with a prolonged QT interval at rest Polymorphic ventricular tachycardia that is not torsades de pointes. This is disorganised ventricular activity similar to ventricular fibrillation.In torsades de pointes a regular change of axis of ventricular tachycardia occurs around the baseline. It is a specific arrhythmia associated with a prolonged QT interval (drug induced, congenital, hypokalaemia, hypomagnesaemia, bradycardia). When treating, consider:
• Stopping QT prolonging medication
• Potassium and magnesium replacement
• Increasing the underlying sinus rate with temporary pacing or isoprenaline.
• Polymorphic ventricular tachycardia that is not torsades de pointes occurs in the same circumstances as ventricular fibrillation and is treated in the same way.
Learning bite
If a patient receiving antiarrhythmics becomes unwell you should consider whether the antiarrhthmic is causing side effects. For example lidocaine can cause a range of side effects including seizures.In view of the side effects of antiarrhythmics implantable cardioverter defibrillators are being increasingly used, especially in patients with structural heart disease. They also have the advantage of being proved to prolong life in patients with left ventricular dysfunction and a history of sustained ventricular arrhythmias.
In an emergency you may need to treat patients with a broad complex tachyarrhythmia with a DC shock. For patients with a pulse you should start with 100 J or an equivalent biphasic energy. This is the advice of the Resuscitation Council UK. Remember, shocks are painful - if the patient is conscious, sedation should be provided.
3. Normal heart ventricular tachycardia
These are ventricular tachycardias that occur without structural heart disease. There are a number of different forms and all are associated with a good prognosis.You should not diagnose this condition without involving an electrophysiologist. It is important to recognise normal heart ventricular tachycardias because they respond to different antiarrhythmics and are potentially curable without long term sequelae with catheter ablation.
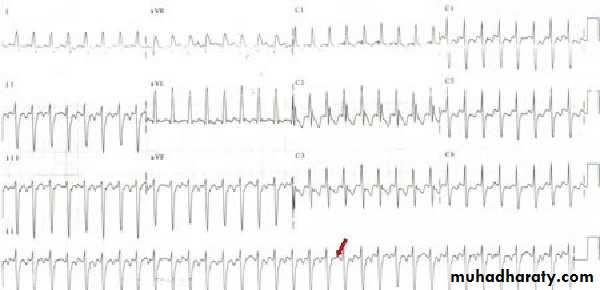
Right ventricular outflow tract ventricular tachycardia
This is a focal ventricular tachycardia located in the right ventricular outflow tract, although a similar arrhythmia can occur elsewhere (Figure 21). It can occur as:Single ectopics
Bursts of ectopics
A more sustained arrhythmia.
The QRS is broad and has a left bundle branch block pattern.
Complexes are positive in the inferior leads.
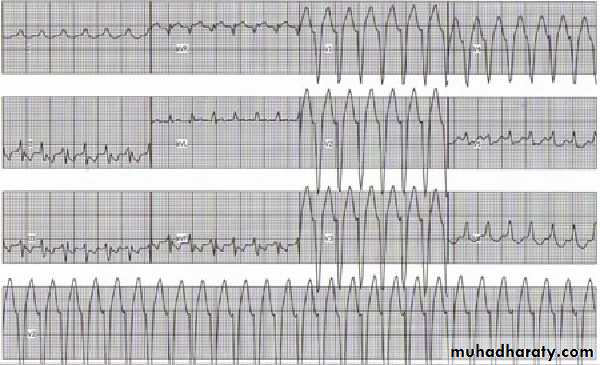
Figure 21. Right ventricular outflow tract ventricular tachycardia. Short bursts of this rhythm are seen. The pattern is of a left bundle branch block morphology with positive complexes in the inferior leads.
Fascicular tachycardia
This is a re-entrant ventricular tachycardia usually circulating around the posterior fascicle of the left bundle, although a rarer form can occur around the anterior fascicle (Figure 22).Figure 22. Fascicular ventricular tachycardia. The QRS complexes are somewhat narrow, with a right bundle branch block, left axis deviation pattern. Atrial activity can be seen, particularly in the inferior leads. However, occasional P waves are missing (arrow) due to retrograde block in the atrioventricular node. This proves that the atrium is not part of the circuit, making the diagnosis ventricular tachycardia.
Pre-excited tachycardia
1. Antidromic tachycardiaThis tachycardia is re-entrant based on an accessory pathway. Activation spreads down through the accessory pathway and returns to the atria via the atrioventricular node (Figure 23). The QRS is broad and bizarre because the ventricle is activated purely from the accessory pathway. Because the circuit is fixed, the rhythm is regular. Retrograde P waves may be visible, although they may be buried in the broad QRS. There may be a delta wave visible in sinus rhythm, although this may be difficult to see if the pathway is latent. Adenosine given in sinus rhythm may make the delta wave more obvious.
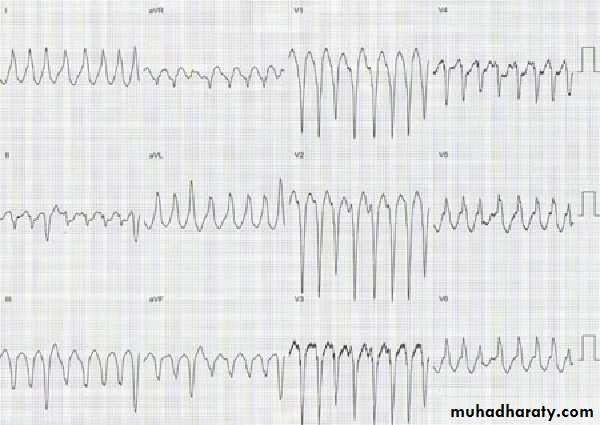
• Figure 23. An ECG of an antidromic tachycardia. The QRS complexes are broad and the rhythm is regular. It is possible to clearly define this as an antidromic tachycardia as opposed to a ventricular tachycardia only when the patient is in sinus rhythm and pre-excitation can be seen on the resting ECG.
•
2. Arrhythmias with a bystander accessory pathway
It is possible to have a tachycardia in a patient who has an antegradely conducting accessory pathway that plays no part in the tachycardia mechanism. Any supraventricular tachycardia can present in such a way. The most well recognised arrhythmia in this group is atrial fibrillation, which can pre-excite the ventricle sometimes producing excessive ventricular response rates with the danger of ventricular fibrillation (Figure 24).• Figure 24. Two ECGs with pre-excited atrial fibrillation. Ventricular activity is fast, broad, and irregular (an FBI tachycardia). Varying degrees of pre-excitation are seen.
•
•
The QRS may be broad and bizarre because the ventricle is activated via the accessory pathway. There may be some variability because the ventricle will also be activated via the normal conducting system. The rate may be regular or irregular depending on the regularity of the underlying arrhythmia. Underlying atrial activity may be visible according to the underlying arrhythmia. Single P waves may be buried in the broad QRS.
Supraventricular tachycardia with aberration
Any supraventricular tachycardia can occur in association with bundle branch block. This will be classic right or left bundle branch block. Always remember that mistaking an aberrant supraventricular tachycardia for a ventricular tachycardia is preferable than mistaking a ventricular tachycardia for a supraventricular tachycardia.The bundle branch block may be pre-existing or can occur due to the sudden rate change.
Right bundle branch block is more usual in this situation. Atrial activation may be poorly visible due to the width of the QRS.
Characteristics of classic right bundle branch block
A prolonged QRS, >120 msAn M-shaped QRS complex in the right sided chest leads (usually the second R wave being larger than the first)
A deep slurred S wave in the lateral chest leads and
lead I.
Characteristics of classic left bundle branch block
A prolonged QRS, >120 ms
Broad, slurred, M-shaped QRS complexes in the lateral chest leads and in lead I
Loss of Q waves in the lateral chest leads and in lead I
Small r waves and deep S waves in the right-sided chest leads.
Learning bite
Monomorphic ventricular tachycardia is the most common form of ventricular tachycardia.
But polymorphic ventricular tachycardia has the worst prognosis.
• Aberration often occurs due to a preceding long-short sequence; that is a long RR interval then a short RR interval often caused by the ectopic that induces the arrhythmia. A compensatory pause may not be seen on termination of the aberration if the underlying arrhythmia continues. This would normally be seen on termination of ventricular tachycardia.
• With aberration, rates conducted faster with a normal QRS are often seen.
Your answer
Correct answera.
Start amiodarone
b.
Fit an implantable cardioverter defibrillator
c.
Start flecainide
• A 60 year old man with ischaemic heart disease and significantly impaired left ventricular dysfunction is admitted to hospital with an episode of ventricular tachycardia. The doctors in the accident and emergency department cardioverted him. What course of action should you advise to prolong his life?
•
amiodarone
Amiodarone is effective against ventricular arrhythmias but does not prolong life.Fit an implantable cardioverter defibrillator
Implantable cardioverter defibrillators prolong life in patients with left ventricular dysfunction and a history of sustained ventricular arrhythmias.
flecainide
Flecainide is contraindicated in patients with cardiac failure.
Your answer
Correct answer
a.
Polymorphic ventricular tachycardia
b.
Fascicular ventricular tachycardia
c.
Right ventricular outflow tract ventricular tachycardia
• Which of the following types of ventricular tachycardia has the worst prognosis?
•Polymorphic ventricular tachycardia
has the worst prognosis. The other types of ventricular tachycardia are often associated with structurally normal hearts, and even though they can be very symptomatic, rarely are life threateningFascicular ventricular tachycardia
associated with a structurally normal heart.
Right ventricular outflow tract ventricular tachycardia
associated with a structurally normal heart.
Your answer
Correct answer
a.
Capture beats
b.
Fusion beats
c.
Classic right bundle branch block morphology
• A 60 year old man comes to the emergency department because he feels unwell. His ECG reveals a broad complex tachyarrhythmia. Which one of the following should make you think that he has a supraventricular tachycardia with aberrant conduction?
Capture beats
Capture beats suggest a ventricular tachycardia.Fusion beats
Fusion beats suggest a ventricular tachycardia.
Classic right bundle branch block morphology
Classic right bundle branch block or left bundle branch block morphology may suggest a supraventricular tachycardia with aberrant conduction.
• A 40 year old man comes to your clinic with palpitations. He had an episode at his GP's surgery two weeks ago and this episode was captured on this ECG.
•
Your answer
Correct answera.
Right ventricular outflow tract ventricular tachycardia
b.
Torsades de pointes
c.
Ventricular fibrillation
• What is the most likely diagnosis?
• Right ventricular outflow tract ventricular tachycardia• This is most likely to be a right ventricular outflow tract ventricular tachycardia. Short bursts of this rhythm are seen. The pattern is of a left bundle branch block morphology with positive complexes in the inferior leads. A diagnosis of right ventricular outflow tract ventricular tachycardia should be made only by a cardiac electrophysiologist.
Your answer
Correct answera.
Amiodarone
b.
Sotalol
c.
Magnesium
d.
Disopyramide
• A 60 year old man is admitted in a collapsed state. His ECG shows torsades de pointes. He is not taking any medication. Which one of the following medications should you consider starting?
•
Amiodarone
Amiodarone can induce torsades de pointes.Sotalol
Sotalol can induce torsades de pointes.
Magnesium
Torsades de pointes often responds to magnesium. The other drugs can induce torsades de pointes.
Disopyramide
Disopyramide can induce torsades de pointes.
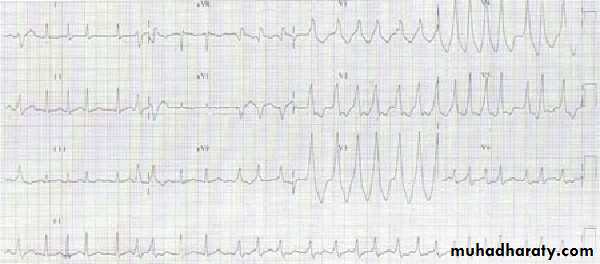
• A 60 year old woman comes to the emergency department because she feels very faint. Her blood pressure is 80/60 mm Hg.
•
Your answer
Correct answera.
Intravenous amiodarone
b.
Emergency synchronised cardioversion
c.
Emergency unsynchronised cardioversion
d.
Intravenous adenosine
• What treatment should you advise?
•This patient is haemodynamically unstable and so should receive an emergency synchronised cardioversion.
Your answer
Correct answera.
Lidocaine
b.
Amiodarone
c.
Verapamil
d.
Adenosine
• A 70 year old man on the coronary care unit has a seizure. He is now in sinus rhythm but has had recent dysrhythmias. He is now receiving medication for this. Which one of the following medications is most likely to be at fault?