Diabetes mellitus
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Studies undertaken by Diabetes UK indicate that the average patient with diabetes type 2 has had their disease for 9-12 years before diagnosis.
In the UK Prospective Diabetes Study, patients with type 2 diabetes were found to have a high incidence of hypertension (35%) and coronary heart disease (18%) at diagnosis.
Structured foot examinations can reduce the rate of ulceration and amputation by 44-85%.
This is a classic neuropathic ulcer. It is punched out and is situated on the sole of the foot underneath the heads of the metatarsals.
Exudative maculopathy
This is exudative maculopathy. Hard exudates are encroaching on the macula.Impaired glucose tolerance occurs when the fasting venous plasma glucose is <7.0 mmol/l and the venous plasma glucose is ≥7.8 mmol/l but <11.1 mmol/l after the oral glucose tolerance test.
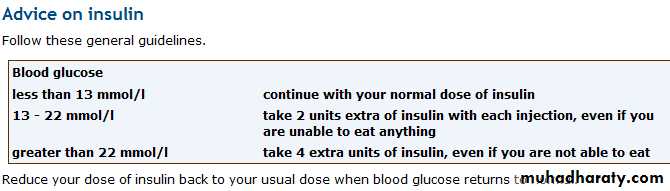
Diabetes mellitusSick day rules for people on insulin
Principle: To provide guidelines for use by health care professionals to assist insulin treated people with blood sugars above 15, resulting from episodes of intercurrent illness. To prevent diabetic ketoacidosis from developing.
Normal insulin should never be stopped.
Additional doses of soluble insulin should be given as necessary to bring down blood sugars and suppress ketone productia (eg. Actrapid 4 hourly).Blood sugars should be checked at least every 4 hours.
Urine should be tested for ketones if people are unwell or blood sugars are 15+.
Maintain an adequate fluid intake (sugar free) of
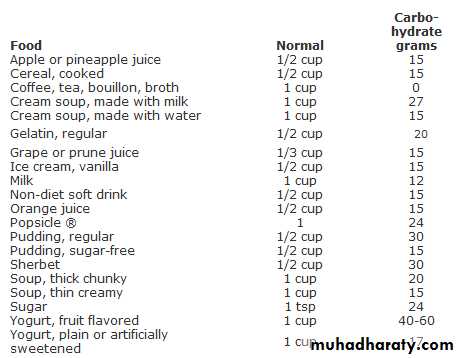
100-200mL (approximately 1 glass) every hourMaintain a regular intake of carbohydrate, regardless of blood glucose. It may be difficult to persuade some patients or relatives of this!
At mealtimes, if unable to eat, but tolerating fluids, take carbohydrate in the form of 200mL of the following;
Ribena and water
Fruit juice
Soup (such as tomato or chicken)
Milk with Drinking Chocolate or Ovaltine
Flat Coca Cola or Lemonade (sugary)
Indications for Hospital Admission
Inability to swallow or keep fluids down
Persistent vomiting
Persistent diarrhoea
Persistently raised glucose (>28 mmol/L) despite increasing insulin
Strongly positive ketonuria
When ketoacidosis is clinically obvious (dehydration, abdominal pain, intractable vomiting, rapid or laboured respirations
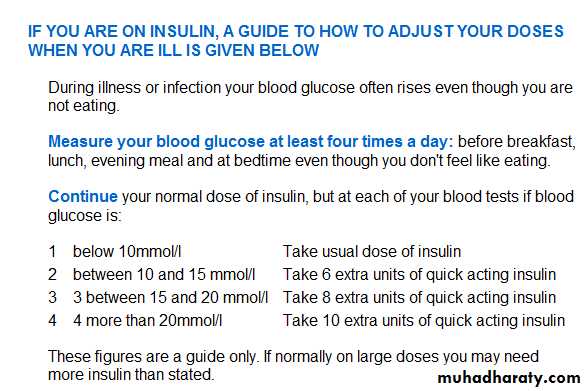
Sick Day Rules
There are some precautions you should take when you are sick in order to avoid acute complications of diabetes especially if you have type 1 diabetes. Part of the body's natural response to the stress of an illness (such as an infection or injury) is to make more sugar. In people with type 1 diabetes this may lead to very high blood sugar levels and a diabetic ketoacidosis. During periods of illness you may experience loss of appetite and reduce your intake of food. Many insulin treated patients reduce or stop insulin due to concerns about hypoglycaemia during intercurrent illness.
Diabetes and illness
What precautions should I take?
Never stop taking your insulin or omit doses. Your blood sugar levels may continue to rise even if you do not eat. If your blood sugar levels are higher than 10 mmol/l you may consider taking a larger or additional dose of insulin.Test your blood glucose more often. If your levels are unstable increase the frequency to every 4 hours or more.If blood glucose readings are higher than 13 mmol/l, and you are unwell or vomiting, check your urine for ketones.Use 'Ketostix' strips to test your urine. Some blood glucose meters allow you to test for ketones as well (MediSense Optium), and this is quite acceptable. However, testing for ketones in the urine is a very sensitive test and there is no necessity to demonstrate ketones bodies in the blood.Drink lots of fluids. Its easy to become dehydrated when you are ill especially if you have a temperature, vomiting or diarrhoea. If you are unable to keep fluids down call your doctor. You also lose fluids through sweating and breathing. Aim to drink at least 3 litres of fluid a day. If this is difficult persist with regular sips. When people are admitted with ketoacidosis they are severely dehydrated and require as much as 6-9 litres of fluids to restore lost volumes.
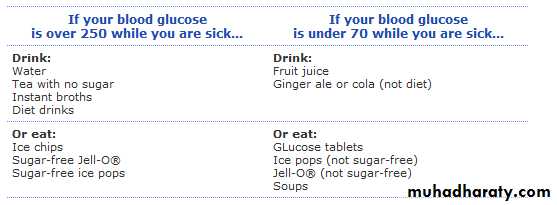
Stick to your normal diet as far as possible. If unable to eat solids take liquids and even sugary drinks if necessary.
I have ketones in the urine
If your blood glucose is continuously more than 17 mmol/l or if you are vomiting, test your urine for ketones. Ketones may appear in the blood and urine due to starvation. They also can indicate a lack of insulin. The presence of ketones in the urine may be a warning of developing ketoacidosis and should be acted upon. Remember ketoacidosis is a life threatening emergency which needs to be identified and treated quickly.Advice on diet
Try to drink 4-6 pints of sugar-free liquids (water, tea) throughout the day.
If you don't feel like eating, replace your solid food with soup, milk, ice cream, fruit juice, sugar, honey, fruit juice.
Know when to call for help!
You or a member of your household should seek assistance in the event of any of the following. Speak to your Specialist Nurse or your GP. If in doubt always seek advice - it is better not to leave it too late!• Unable to eat or drink
• Loss of fluids due to repeated vomiting or diarrhoea
• Very high blood sugar levels (higher than 25 mmol/l) despite taking more insulin
• persistent ketones or 'large' ketones
• blood glucose levels are low
• if you become drowsy or confused
• if you are worried!
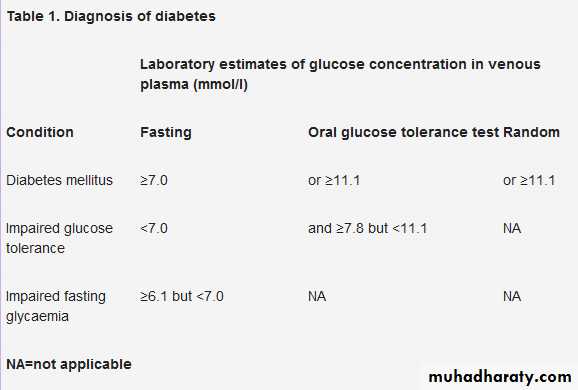
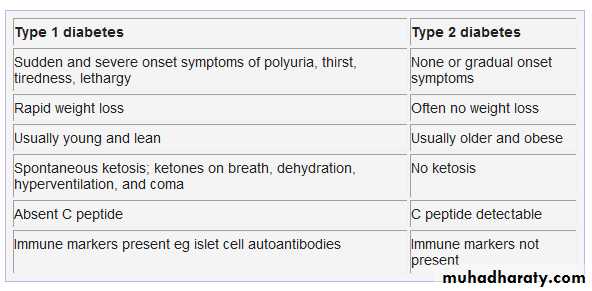
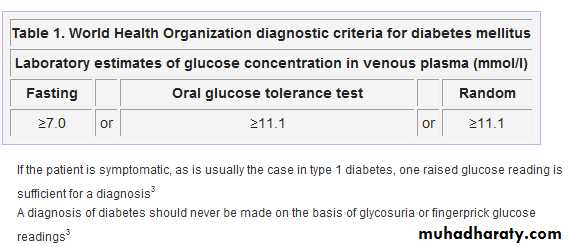
Diabetes should be diagnosed on the basis of a high fasting venous plasma glucose (fasting >8 hours) or a high random blood glucose.Diagnosis should always be confirmed by repeating the test on another day, unless the patient is symptomatic or has unequivocal hyperglycaemia with acute metabolic decompensation. If the patient is symptomatic, one raised glucose reading is enough for diagnosis. If the patient is asymptomatic, you need to be absolutely certain before "labelling" the patient.
The oral glucose tolerance test is no longer recommended as the first line investigation for diagnosis of diabetes. Patients with impaired fasting glucose, however, should be offered an oral glucose tolerance test to exclude the diagnosis of diabetes.
The World Health Organization's diagnostic criteria for diabetes mellitus, adopted by Diabetes UK, are set out in table 1
An oral glucose tolerance test involves an initial fasting blood glucose. The patient is given a 75 g glucose load to drink and a blood sample is repeated two hours later
Patients with glucose intolerance or impaired fasting glucose should be screened annually to exclude diabetes.If a patient is diagnosed with impaired glucose tolerance or impaired fasting glycaemia, the risk of developing diabetes is 4-12% per annum
Proposals by the American Diabetes Association to adopt HbA1c as an alternative method of screening for diabetes have not yet been endorsed by WHO .
Foot examination
Benefits
Patients with diabetes should receive a thorough foot examination at the time of diagnosis and then at least annually. This type of structured programme can decrease the rate of ulceration and amputation by 44-85%. Patients with high risk feet should be identified and given education, regular podiatry, and specially designed shoes which reduce risk of ulceration.
How to do it
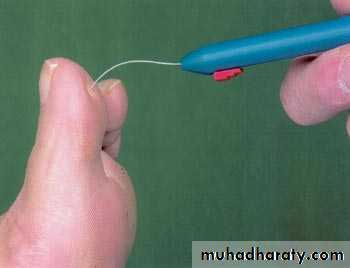
The assessment should include:• Foot sensation using a 10 g monofilament or vibration sense
• Foot structure and biomechanics
• Vascular status (feeling for the presence or absence of foot pulses)
• Skin integrity
• Appropriateness of footwear.
Testing light touch sensation with a monofilament
Charcot foot
Ischaemic ulcerNeuropathic ulcer
Charcot foot
Eye examination
In patients with type 2 diabetes, the NICE recommends that:An initial comprehensive examination of dilated eyes is performed shortly after diagnosis,Subsequent examinations should be done annually, with more frequent examinations if retinopathy is present or progressing,When planning pregnancy, women with diabetes should have a comprehensive eye examination and be counselled on the increased risk of development or progression of retinopathy.Dilated, indirect ophthalmoscopy by an optician or ophthalmologist is an acceptable method of screening for retinopathy.
However, all patients with diabetes should be referred to their local screening service for retinal photography, which remains the National Screening Committee’s standard method for retinopathy screening (two field retinal photography in England, one field retinal photography in Scotland).
Eye examination (including fundoscopy but, ideally, dilated fundal digital photography)
New vessels in optic disc
Pre-proliferative retinopathy with venous beading, cotton wool spots, and some hard exudates
Exudative maculopathy
The main risk factors for developing type 2 diabetes are:Age over 40 years
Obesity (especially central obesity)
Asian, African, or African-Caribbean origin
Past history of hypertension or cardiovascular disease.Family history of diabetes or cardiovascular disease
History of gestational diabetes during pregnancy, or birth of a large baby (birth weight >4 kg) Pregnancy.
Other less common causes of diabetes include:
Pancreatic disease(chronic pancreatitis or cystic fibrosis)
Drugs
(corticosteroids or thiazides)
Endocrinopathies
(Cushing's disease or acromegaly)
Genetic syndromes
(Turner's syndrome or Down's syndrome
Why do people develop type 2 diabetes?
Type 2 diabetes is caused by:
• Progressive failure of the pancreatic beta cells
• Insulin resistance.
Normal beta cells
The normal physiological response of pancreatic beta cells to glucose is:
Initial rapid secretion of insulin, which lasts 5-10 minutes
Sustained, pulsatile second phase release of insulin, which starts 10-20 minutes after initial exposure to glucose.
With beta cell failure in patients with type 2 diabetes
Initial first phase response to insulin is blunted and delayed .Frequency of insulin pulses during the second phase is reduced.Both genetic and environmental factors cause beta cell failure:
There is strong concordance in monozygotic twins .Pima Indians have a high prevalence of diabetes. In this group a high fat diet is associated with impaired insulin secretion responses to glucose.
Insulin resistance
Insulin resistance is characterised by a reduced ability of endogenous insulin to exert its biological action in adipose tissue, liver, and skeletal muscle. It affects about 90% of patients with type 2 diabetes.Genetic and environmental factors cause insulin resistance:
Concordance in monozygotic twins ranges from 45-96%
Insulin resistance is associated with central obesity and physical inactivity.
Although morning blood glucose levels are slightly high, Miss Peabody’s comment that she wakes up "out of sorts" may suggest she is having night time episodes of hypoglycaemia. Increasing her Humulin could worsen night time hypoglycaemia further and cause a further rise in morning blood glucose levels.
The Somogyi effect occurs when hypoglycaemia in the night stimulates glucose counter-regulation, including adrenaline, growth hormone, cortisol, and glucagon release. These hormones serve to increase blood glucose by gluconeogenesis and glycogenolysis. Asking her to set her alarm to 2am will determine if she is developing night time hypoglycaemia and her Humulin I dose may need to be reduced. If she has no nocturnal hypoglycaemia then this pattern is consistent with the dawn phenomenon, in which case increasing her Humulin I would be appropriate. This is the best course of action.
A high carbohydrate diet is not associated with an increased risk of developing type 2 diabetes. However, a high fat diet is associated with an increased risk.
In women, a positive result for microalbuminuria is indicated by an albumin:creatinine ratio ≥3.5.
Therapy with ACE inhibitors is not needed in patient has no microalbuminuria
If a patient is diagnosed with impaired glucose tolerance, the estimated annual risk risk of developing diabetes is 4-12%.
A comprehensive eye examination should be done soon after diagnosis in patients with type 2 diabetes because they may have developed complications.
Lipid management
NICE guidance on the management of lipids in patients with type 2 diabetes recommends annual assessment of cardiovascular risk. Patients considered to be at high risk should be treated with statins.The following patient groups should be considered at high cardiovascular risk:
Aged 40 years or more with type 2 diabetes
Aged 18–39 years with type 2 diabetes and who have at least one of the following:
• Retinopathy (pre-proliferative, proliferative, maculopathy)
• Nephropathy, including persistent microalbuminuria
• Poor glycaemic control (HbA1c >9%)
• Elevated blood pressure requiring antihypertensive therapy
• Raised total blood cholesterol (>6.0 mmol/l)
• Features of metabolic syndrome (central obesity and fasting triglyceride >1.7 mmol/l and/or HDL cholesterol <1.0 mmol/l in men or <1.2 mmol/l in women
• Family history of premature CVD in a first degree relative.
• If CV risk becomes >20% over 10 years these patients should be considered for statins.
Microalbuminuria screening
recommended in patients with type 2 diabetes at diagnosis and annually thereafter.
loss of urinary albumin of 30-300 mg/24 hours.
or
albumin:creatinine ratio in a first morning urine sample,
In men, microalbuminuria is indicated by a ratio ≥2.5
In women, a ratio ≥3.5
Two sequential elevated results four weeks apart are required to confirm microalbuminuria in patients with diabetes .
Structured education
The Diabetes National Service Framework states that all primary care trusts need to commit to offering structured education programmes to people with type 2 diabetes from the point of diagnosis (in addition to usual care).DESMOND - Diabetes Education and Self-Management for Ongoing and Newly Diagnosed is a national education programme for people with type 2 diabetes. Currently delivered from 69 sites across the UK DESMOND encapsulates a patient centered approach to diabetes care providing six hours of structured diabetes education from trained facilitators. Twelve months after attending a DESMOND programme patients with type 2 diabetes achieve greater weight loss, less depression, and higher levels of smoking cessation compared to individuals receiving usual care.
Diabetes mellitus type 1
Key pointsAim for:
Haemoglobin A1c <7.0-7.5% (targets should be individualised for each patient)
Blood pressure <140/80 mm Hg (younger patients and those with early evidence of kidney, eye, or cerebrovascular disease who have a good life expectancy should have a blood pressure <130/80 mm Hg)
Fasting plasma glucose 4.4-6.1 mmol/l
Total cholesterol <4.0 mmol/l
Low density lipoprotein <2.0 mmol/l
Fasting triglycerides <1.7 mmol/l
Aim to achieve the following clinical management targets:
Patients should have a fasting venous plasma glucose of 4.4-6.1
Patients should have a postprandial venous plasma glucose of 4.4-8.0
Patients should have individualised HbA1c targets of <6.5%-7.5%
Patients should have no glucose in their urine
Patients should have a total cholesterol of <4.0
Patients should have a high-density lipoprotein cholesterol of >1.1
Patients should have fasting triglycerides of <1.7
Men should have a body mass index of 20-25
Women should have a body mass index of 19-24
Patients should have a blood pressure of <140/80 (younger patients and those with early evidence of kidney, eye or cerebrovascular disease who have a good life expectancy should have a blood pressure of <130/80 mm Hg.
Non-drug measures
Explain the aims of treatment and the relation between blood glucose and diet and exercise. A dietitian should assess all patientsExplain the importance of a healthy lifestyle, especially physical activity and smoking cessation,the importance of self monitoring with home glucose testing
Explain that poor glucose control will lead to complications
Explain the importance of screening for complications
Explain the importance of regular foot care and foot hygiene
All patients should receive structured care to evaluate their risk of microvascular and cardiovascular complications
Women of reproductive years should be informed of the importance of safe effective contraception to avoid unplanned pregnancy,Pre-pregnancy care is recommended to all women planning pregnancy. The benefits of good pre-conception glycaemic control and high dose folic acid (5 mg) before and during pregnancy should be emphasised.
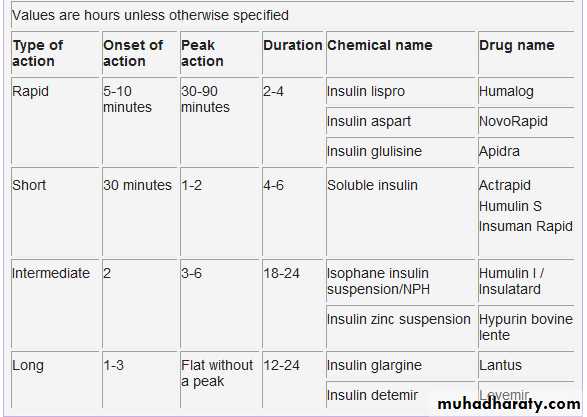
Insulin is available in four main types
Insulin will usually be initiated at 0.25-0.5 units/kg/day and will be titrated according to blood glucose controlThe choice of insulin regimen for patients should be determined by:
Compliance or resistance to injectionsRisk of hypoglycaemia
Lifestyle
Age
Complications (good control is needed to reduce the incidence of complications; however, a blind patient is unlikely to cope with injections four times a day without support from a carer).
Insulin regimens
The most commonly used insulin regimens are:Multiple injection or basal bolus therapy
Short or rapid acting insulin is taken before each meal, long acting insulin is taken before the patient goes to bed.This therapy closely mimics normal physiological insulin secretion
It allows flexibility around timing of meals and exercise.Snacks are needed between meals if short rather than rapid acting insulin is used
Rapid acting insulin can be taken just before, rather than 30 minutes before, meals
Twice daily therapy
Injections of premixed short and intermediate acting insulin are taken before breakfast and before the evening meal.This therapy is usually mixed as 30% short acting insulin and 70% intermediate acting insulin. Two thirds of the total dose is taken at breakfast time.
This therapy is useful for patients who are reluctant to inject frequently.
Regular meals and snacks are needed to prevent daytime hypoglycaemia. Nocturnal hypoglycaemia is common.
Three times daily therapy
This is an injection of premixed short and medium acting insulin before breakfast, short acting insulin before the evening meal, and intermediate acting insulin before bed
It can be considered if twice daily therapy does not maintain control, or if the patient has frequent nocturnal hypoglycaemia
The role of insulin glargine and insulin detemir
Are basal insulin analogues that have a more predictable pharmacodynamic profile than intermediate acting insulins (NPH). Their action profiles tend to be smoother and more prolonged (up to 24 hours), which makes them suitable as the basal component of multiple injection therapy. They are particularly useful for patients who have:• Frequent nocturnal hypoglycaemia using NPH
• A high fasting blood glucose despite maximum tolerated doses of NPH
• Variable blood sugar control on standard insulin therapy.
Insulin detemir shows less variability of absorption than NPH and glargine. However, detemir is often required twice daily, whereas glargine is needed only once daily. It does seem, however, to be associated with less weight gain.
Continuous subcutaneous insulin infusion therapy
recommended as an option for people with type 1 diabetes when:Multiple injection therapy (including the use of insulin glargine or detemir) has failed (that is, in patients where it has been impossible to maintain a concentration of haemoglobin A1c ≤7.5%, or 6.5% in the presence of microalbuminuria, without causing disabling hypoglycaemia).The patient has the commitment and competence to use the therapy effectively.Insulin pump therapy is increasingly being used for children, young people, and women seeking pregnancy.
Intensive control of hyperglycaemia
Benefitsprevents microvascular and neuropathic complications in patients with type 1 diabetes, compared with conventional control. It improves pregnancy outcomes in women with diabetes. There is also a small reduction in cardiovascular risk with intensive treatment.
Side effects
Patients receiving multiple daily injections have more weight gain and hypoglycaemia. Trials have shown no difference in cardiovascular, neuropsychological, or quality of life outcomes compared with conventional treatment.
Evidence
In the diabetes control and complications trial patients receiving intensive treatment had fewer microvascular complications (retinopathy and nephropathy) and neuropathic complications than those receiving conventional treatment. In 1993, a large meta-analysis of 16 small randomised controlled trials in patients with type 1 diabetes found similar results. In 1999, another review of randomised controlled trials in patients with type 1 diabetes found a decrease in cardiac events, but not mortality, with intensive versus conventional therapy
How to achieve intensive control
GoalsThe goals for blood glucose and haemoglobin A1c should be at, or close to, the normal non-diabetic range.
Monitoring
Patients receiving intensive treatment should monitor their blood glucose levels frequently. This means glucose checks at least four times a day.
Regimens
All patients should receive counselling on meal planning and physical activity, including advice to maintain a normal weight. Patients should adjust their insulin dose frequently based on self monitoring of glucose.
Screening
Screening for complications of diabetes is a key part of management.
What's the outlook?
Studies show that mortality rates are twice as high among middle aged people with diabetes than among middle aged people without diabetes.However, intensive control of hyperglycaemia prevents microvascular and neuropathic complications in people with type 1 diabetes compared with conventional control. There is also a small reduction in cardiovascular risk with intensive treatment versus conventional treatment. Recent studies have allayed past concerns about cardiovascular risk with intensive treatment.
Long acting insulin analogues (insulin glargine)
This is recommended as a treatment option in patients with type 1 diabetes. Insulin glargine is a long acting human insulin analogue that is given once a day. It maintains a basal concentration of insulin in the blood that can be raised by supplementary injections of short acting insulin as required. This mimics natural insulin release.Women with diabetes whose HbA1c is above 10% should be strongly advised to avoid pregnancy. If it is safely achievable, women with diabetes who are planning to become pregnant should aim to maintain their HbA1c below 6.1%. They should be reassured that any reduction in HbA1c towards the target of 6.1% is likely to reduce the risk of congenital malformations. They should also be advised to take folic acid 5 mg daily until the 12th week of pregnancy to reduce the risk of neural tube defect.
Important points to remember with insulin
Injection technique
Depth of needle penetration affects absorption of insulin:
Shallow insertion of the needle into the dermis causes pain and poor absorption
Deep injection into the muscle causes pain and more rapid absorption
5-8 mm needles are appropriate for most patients - but you should avoid long needles in thin patients.
The needle should be inserted perpendicular to pinched skin and the insulin should be injected over 5 to 6 seconds.
Site of injection
Encourage patients to rotate the place of insulin injections to reduce the incidence of skin or fat atrophy and hypertrophy. Lack of site rotation is a common cause of day to day variation in control of glucose.Insulin is absorbed:
Fastest from the abdomen.
Slowest from the legs and buttocks.
Other factors that affect absorption of insulin include:
Increases in skin temperature (including exercise or a hot bath), which increase absorption.
Sick day" rules
When patients are unwell they need to be aware of the sick day rules.Never stop taking insulin even if not eating. There may be a need to increase the dose
Test blood glucose more often (at least four times a day)
Drink lots of fluids to prevent dehydration
Replace normal meals with carbohydrate drinks if necessary
Test urine for ketones
Seek medical advice if you develop vomiting or are unsure what to do
Complications from injecting insulin
Complications from injecting insulin include skin changes (atrophy and fat hypertrophy). The risk of infection is low.
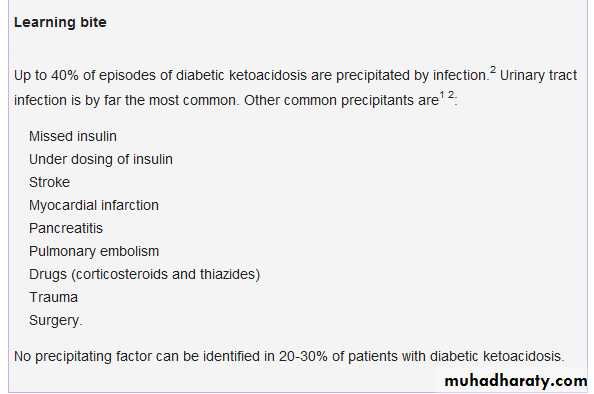
Diabetic ketoacidosis
Diabetic ketoacidosis is a serious acute metabolic complication of diabetes. It can occur in patients with type 1 and type 2 diabetes mellitus, although the occurrence of diabetic ketoacidosis in patients with type 2 diabetes is usually associated with severe illness (for example myocardial infarction). It is a triad of:
• Hyperglycaemia
• Metabolic acidosis
• Ketonuria.
Although mild diabetic ketoacidosis can be managed by frequent intramuscular insulin, continuous intravenous insulin is the treatment of choice for more severe episodes of diabetic ketoacidosis. Subcutaneous insulin injections have poor absorption and so are not indicated in the treatment of diabetic ketoacidosis.
An initial intravenous insulin
bolus of 0.15 units/kg of body weight should be followed by an intravenous insulin infusion at the rate of 0.1 unit/kg/hour. Intravenous insulin should continue until acidosis is corrected.
You should aim for a reduction in blood glucose at a rate of 3-5 mmol per hour. Rapid correction of glucose levels leads to rapid changes in serum osmolality and may precipitate cerebral oedema. Avoid a serum osmolality change more than 3 mosmol/kg/hour.
Blood glucose should be checked every hour and when the glucose levels are <14 mmol/l the intravenous insulin fluid regimen should be changed from normal saline to 5% dextrose, and the insulin rate should be reduced to 0.05-0.1 unit/kg/hour.
You should maintain blood glucose between 8 mmol/l and 12 mmol/l by adjusting insulin and dextrose infusion rates until the acidosis is corrected.
Intravenous insulin therapy should be continued for one to two hours after the initiation of the subcutaneous insulin regimen to ensure adequate plasma insulin levels.
Blood glucose <10 mmol/l, serum bicarbonate ≥18 mmol/l, and a venous pH >7.35 indicate resolution of diabetic ketoacidosis.
Intravenous insulin can be changed to subcutaneous insulin unless the patient is nil by mouth. The intravenous insulin should continue for at least an hour after the subcutaneous insulin is given.
Fluid deficit in diabetic ketoacidosis should be replaced in 24-48 hours to correct dehydration and maintain renal perfusion. You should give around 1-1.5 litres of fluid in the first hour (consider colloid instead of crystalloid if the blood pressure is very low). The rate should be adjusted according to the hydration status, blood pressure, jugular venous pressure, and urine output. Further fluid can be given at a rate of 250-1000 ml/hour.
Learning bite
Actrapid insulin is undergoing a phased withdrawal from the market by manufacturer Novo Nordisk. Insulin analogues such as Novorapid or Humalog are equally effective during the treatment of DKA.
The annual incidence of diabetic ketoacidosis among people with type 1 diabetes is 1-5%. Patients in experienced centres have a less than 5% mortality from diabetic ketoacidosis, although this increases with age and the presence of concomitant illnesses.
15% of patients, diabetes may be diagnosed for the first time when they present with diabetic ketoacidosis.
Serum pH levels in alcoholic ketoacidosis may be misleading because patients may have a mixed acid-base disorder. Patients with alcoholic ketoacidosis may have metabolic acidosis due to ketone formation, metabolic alkalosis due to vomiting (loss of hydrogen ions), and volume depletion.
They may also have respiratory alkalosis secondary to hyperventilation. Serum pH levels can therefore be difficult to interpret because the pH levels may be near normal despite a severe acid-base disturbance in patients with alcoholic ketoacidosis.
In renal tubular acidosis blood glucose levels are normal, there is no ketonuria, and urinary pH is >5.5. The anion gap is normal in proximal renal tubular acidosis.
The anion gap is calculated using the formula:
Anion gap = ((Na+ + K+) - (Cl- + HCO3 -)).
A normal anion gap is 7-9 mmol/l.
Metabolic acidosis with a high anion gap
is seen in• lactic
• alcoholic
• diabetic
• renal
• drugs (such as salicylates, methanol, formaldehyde, ethylene glycol, paraldehyde, or metformin
• rhabdomyolysis.
Metabolic acidosis with a normal anion gap (hyperchloraemic acidosis)
is seen
diarrhoea,
pancreatic fistula,
type 2 (proximal) renal tubular acidosis, and hypoaldosteronism (that is type 4 renal tubular acidosis).
drugs ammonium chloride)
To start to correct the fluid deficit, an infusion of 1-1.5 litres of 0.9% saline in the first hour is appropriate for most patients unless they have a low blood pressure (that is systolic blood pressure <100 mm Hg). Infusion rates should be adjusted according to response to therapy. This should be assessed by changes in blood pressure, presence of postural hypotension, reflex tachycardia, urine output, and electrolytes. It is common practice to deliver 250-1000 ml/hour for the next four hours (4-14 ml/kg/hour).
You should use 0.45% saline instead of 0.9% if sodium levels are >155 mmol/l.
Serum osmolality is calculated by using the formula
2{(Na+)+(K+)} + (glucose)+(urea).Normal is 280-290 mosmol/kg.
High osmolality is associated with confusion and sometimes coma. This is further aggravated by rapid changes in osmolality and worsening acidosis. Cerebral oedema is a complication of treatment of diabetic ketoacidosis (although the pathogenesis is not clear). It could be caused by rapid changes in blood glucose or osmolality.Another complication to watch for during treatment of diabetic ketoacidosis is hypoglycaemia. Changing saline to 5% dextrose when the blood glucose is <14 mmol/l and continuing intravenous insulin plus intravenous fluids to correct acidosis would avoid this.
If you suspect cerebral oedema you should do a CT scan of the brain. This may show effacement of the ventricles. Hyperventilation in an intensive care unit, or intravenous mannitol infusion, or both may help in some patients.
Lumbar puncture could be risky in the presence of cerebral oedema. Papilloedema may be absent because the cerebral oedema develops quickly. Doing a lumbar puncture may lead to coning.
Patients with diabetic ketoacidosis and a high osmolality should be started on a prophylactic dose of heparin or low molecular weight heparin. This is because they are at high risk of thromboembolism. But there are no randomised controlled trials to demonstrate the benefits of heparin.
Amylase can be raised in diabetic ketoacidosis in the absence of pancreatitis.
Patients with diabetic ketoacidosis may have vasodilation and feel peripherally warm, although the core body temperature is reduced. The temperature should not be taken as a marker for the presence or absence of infection.The white cell count may also be high in the absence of infection in patients with diabetic ketoacidosis.
Learning bite
During treatment of diabetic ketoacidosis, ketonuria may worsen.Beta hydroxybutyrate is a strong acid, and frequently the predominant ketone in DKA, but is not detected by the nitroprusside test (the commonest laboratory test). During treatment of diabetic ketoacidosis, beta hydroxybutyrate is converted to acetoacetate, which is detected by the nitroprusside test, leading to the erroneous impression that the diabetic ketoacidosis is worsening. During treatment of diabetic ketoacidosis, tests for ketonuria or ketonaemia should not be used to assess response to therapy.
A nasogastric tube should be inserted in unconscious or drowsy patients. This will help avoid aspiration pneumonia.
Acidosis resolves without bicarbonate (if the pH is >7) when insulin and fluids are given because correction of insulin deficiency blocks lipolysis and fatty acid production is reduced. Bicarbonate infusion in the treatment of diabetic ketoacidosis is not evidence based. It is indicated only in patients with severe diabetic ketoacidosis; that is when the pH is <7 or the venous bicarbonate concentration is <10 mmol/l.
Sodium bicarbonate 100 mmol with 20 mmol of potassium infused over one to two hours is the suggested dose. You should monitor pH and potassium levels every two hours. Bicarbonate infusion can be repeated every two hours until the pH is ≥7. Bicarbonate infusion should be stopped when the pH is >7.
Calcium levels should be monitored during treatment with bicarbonate.
Serum phosphate may be normal or decreased in diabetic ketoacidosis. Serum phosphate concentrations decrease with insulin therapy. Severe hypophosphataemia (PO4 <0.35 mmol/l) could increase the risk of respiratory or skeletal muscle weakness and haemolytic anaemia.
Consider phosphate replacement in patients with anaemia, cardiac dysfunction, respiratory depression, or severe hypophosphataemia. Add 20 mmol phosphates to 1 litre of fluid. Calcium levels should be carefully monitored during phosphate infusion.
The average fluid deficit in an adult is 6-7 litres at the time of presentation. The presence of hyperventilation, fever, vomiting, and increased sweating may increase this fluid deficit further. Dehydration, tachycardia, reduced skin turgor, hypotension, shock, and an altered sensorium or coma indicate the degree of fluid loss and electrolyte disturbance.
Fluid replacement in diabetic ketoacidosis is directed towards correcting this fluid deficit to replenish intravascular as well as extravascular volume loss and to maintain renal perfusion.
Investigations
Unlike type 2 diabetes, patients diagnosed with type 1 diabetes do not typically have established microvascular or macrovascular complications at the time of diagnosis. In adults the following investigations should be reperformed at diagnosis in primary care:Full blood count
Serum creatinine
Urea and electrolytes
Liver function tests
Thyroid function test
Fasting lipid profile
Haemoglobin A1c
Urinalysis for glucose, ketones, and protein (analyse midstream urine if protein is detected)
Microalbuminuria.
You should also consider an electrocardiogram.