Epistaxis
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Introduction
Nosebleeds in young people are normally anterior and are often caused by trauma or nose picking.In older people, nosebleeds are more often posterior and secondary causes such as hypertension and anticoagulation therapy are more commonly implicated.
Clinical tips
Resuscitate your patient as requiredRemember the three Gs –
goggles, gown, and gloves
Direct pressure stops most bleeds
Get help early if simple methods fail
Treatment
Step 1: First aid
First of all relax. A nosebleed is a distressing experience for the patient (and perhaps for you too); so it is always helpful to try to remain calm around your patient
Suit up. Epistaxis can be a bloody affair. Protect yourself. Remember the "three Gs": goggles, gown, and gloves
Resuscitate your patient first if necessary. Don't forget airway, breathing, and circulation
Take a quick but comprehensive history
Make sure that your patient is sitting up and bending slightly forwards to prevent blood from tracking into the pharynx. Most bleeds are from the anterior septum
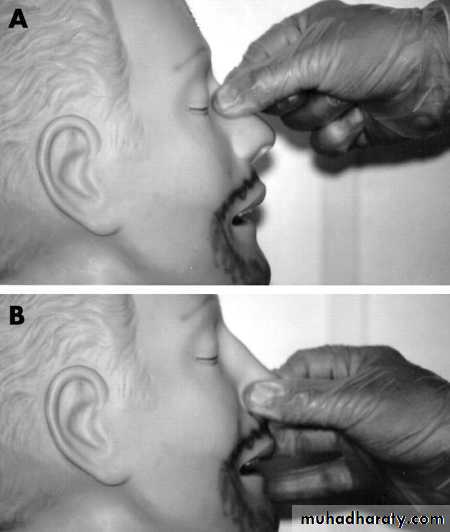
Ask the patient to apply direct pressure by pinching the lower part of the nose for 10-15 minutes (figure 1). This will allow clots to form
At the same time, the patient should be breathing through their mouth and spitting all blood or saliva into a bowl
An ice pack placed over the dorsum of the nose (the area from the nasal bridge to the tip) may help with haemostasis
Bleeding usually stops after direct pressure. If bleeding continues after two attempts at direct pressure, other methods of management should be considered
Stopping the bleeding with direct pressure allows the nasal cavity to be inspected and cautery to be performed. Mild oozing from the septum may stop with silver nitrate cautery, although this is ineffective if bleeding remains brisk. You may want to ask a nurse to help you at this stage
Figure 1 Applying direct pressure to the nose. (A) Incorrect. (B) Correct.
Box 1: HistoryConsider the following:
Which side is bleeding?
How much blood has the patient lost?
Is it a recurrent bleed?
Is it in the pharynx?
Has the patient had recent trauma?
Are there symptoms of hypovolaemia?
What is the past medical history and current medication (for example, aspirin and warfarin)?
• Patients may suffer from nausea and vomiting as a result of swallowed blood. This may precipitate recurrence of epistaxis. Get the patient to lean forward to stop blood going back into the pharynx.
•
Learning bite
You should also examine the nose. You may for example find bleeding and pus caused by vestibulitis, a bacterial infection of the nostril. This can be caused by bacteria entering a wound caused by overzealous picking or as a result of folliculitis of the hairs surrounding the orifice.Step 2: Cautery
Not all patients need cautery. For example, children may not tolerate the discomfort and sting of silver nitrate on raw mucosa.You should consider cautery if you can see the source of bleed, and have adequate lighting and equipment to hand.
• We suggest the following equipment:
• Lidocaine and phenylephrine spray• A headlight or torch
• Nasal specula
• Suctioning facilities
• Silver nitrate cautery sticks As with any procedure, explain to the patient what you intend to do
• Inspect the nasal cavity and clear out any blood or clots with gentle suction
• Spray the nasal cavity with the lidocaine and phenylephrine spray and wait for a few minutes. Although spraying the nasal cavity is not widely practised, we have found this to be of value. Phenylephrine is a potent vasoconstrictor and lidocaine provides local anaesthesia when you inspect the nose for cautery
• Adequate illumination is important. If a headlight is not available, use an
6. otoscope.
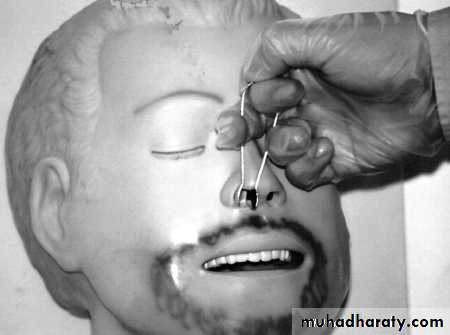
7. Inspect the nasal cavity (figure 2). An obvious site of bleeding may be indicated by a prominent surface blood clot, which is usually at the anterior septumOnce you have identified the bleeding points, apply the cautery for approximately 10 seconds (box 2). Start from the edge of the bleeding point and move centrally in a radial fashion
8. If there is no more active bleeding, the patient may be discharged with an advice leaflet providing there are no other medical problems
• Figure 2 How to hold a nasal speculum.
•
Box 2: Silver nitrate
Precautions:It cauterises everything it touches. So don't touch the facial skin, nasal alae, or other nasal mucosae. Use the nasal speculum, and brace your cauterising hand. Ask your patient to remain still and explain why.
Never cauterise both sides of the nasal septum. This can result in septal perforations.
It may not work if bleeding is active.
Step 3a: Anterior packing
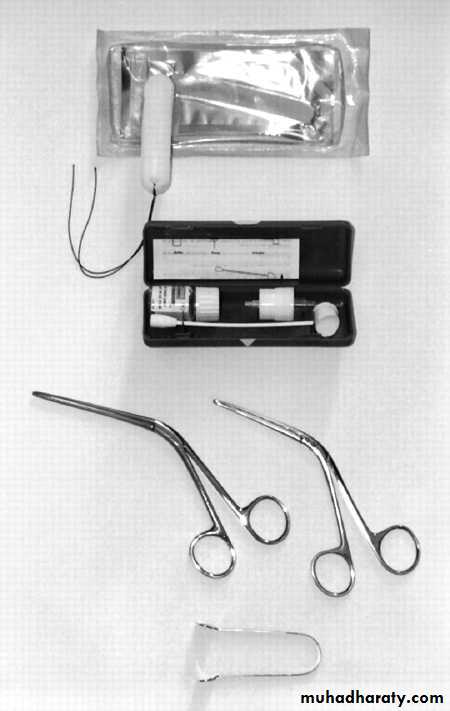
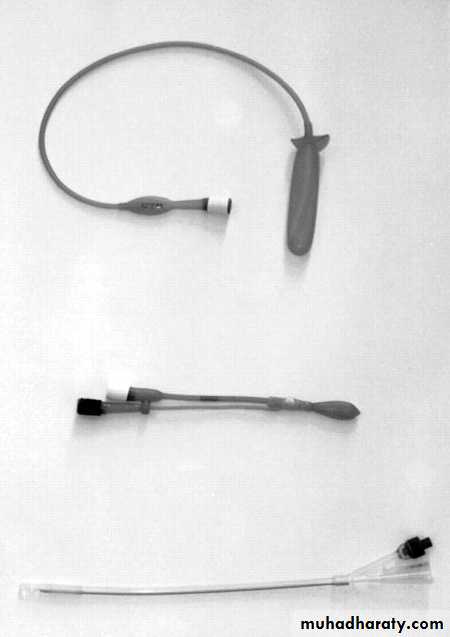
If bleeding continues despite direct pressure and/or after cautery, you may have to consider nasal packing. You should also consider early packing if the patient suffers from hypotension and requires urgent resuscitation or has other medical problems requiring attention.Some of the equipment you will need is (figure 3):
Headlight or torch
Forceps
Ribbon gauze impregnated with bismuth iodoform paraffin paste (BIPP) or Vaseline gauze or Merocel packs
K-Y jelly or Naseptin cream
• Figure 3 Equipment required for Merocel packing. Top to bottom: Merocel pack, lidocaine/phenylephrine spray, forceps, nasal speculum.
•
Merocel packing
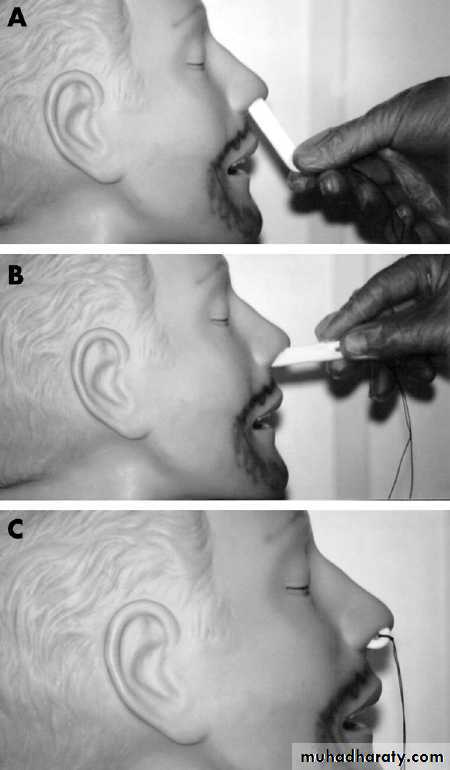
• Lubricate the Merocel pack with a generous amount of K-Y jelly or Naseptin cream• Remember that the floor of the nasal cavity extends horizontally so advance your pack in the manner shown in figure 4
• Ensure that you advance the Merocel pack all the way into the nose
• Pack the other side as well
• Secure the string to the cheek with some tape. Apply a nasal bolster
• Figure 4 A-C Advancing the Merocel pack horizontally
•Packing with ribbon gauze
• Pick the gauze with the forceps approximately 10-15 cm from the tip• Pack the nasal cavity starting from the floor upwards. Remember, the floor of the nose is the roof of the mouth (which is the hard palate)
• Continue to do so by layering the gauze until you reach the cavity roof. Pack the cavity tightly
• Both ends of the ribbon gauze should both protrude from the nostril. You don't want one end dangling down the nasopharynx and causing the patient to gag or, worse, causing laryngospasm
• Secure the gauze. Apply a nasal bolster to control dripping and secretions. A nasal bolster is a small roll of gauze which can be taped to the cheeks
Complications of anterior packing include:
Continued bleedingNasal crusting
Pain
Anosmia
Pack falling out
Posterior migration of the pack causing asphyxia
Breathing difficulties
Aspiration of clots
Perforation of the nasal septum.
Step 3b: Postnasal packing
Continued haemorrhage despite an anterior pack may be due to a posterior bleed.
At this stage, consider placing a postnasal pack. You will need help from a nurse but if you feel out of your depth, ask for help from your colleagues. Many postnasal packs are available commercially, for example Simpson and Brighton balloons (figure 5). The most commonly used is a Foley catheter.
• Remove the anterior pack and re-examine the nasal cavity
• Suction as required. Spray the nasal cavity again• Hold the tip of the catheter with a pair of forceps
• With the patient breathing through the mouth, feed the catheter horizontally along the nasal floor
• Once you see the tip passing beyond the palate into the oropharynx, inflate the balloon with 10 ml of saline
• Gently pull the catheter forwards until you feel resistance. The inflated balloon now acts as a tamponade on the posterior bleed
• At this stage, consider anterior packing (see Step 3A above)
• Secure the catheter with a clip to prevent inadvertent removal. Also ensure that the catheter is not pressing on the nose as alar necrosis may occur. This can be prevented by applying gauze around the nostril
Figure 5 Various types of postnasal pack. Top to bottom: Brighton and Simpson balloons, Foley catheter.
Complications of posterior packing include:
Continued bleedingNasal crusting
Pain
Anosmia
Pack falling out
Posterior migration of the pack causing asphyxia
Breathing difficulties
Aspiration of clots
Perforation of the nasal septum
Cartilage (nasal septum, alar) necrosis from pressure effect of the pack
Learning bite
In any patient with a nosebleed it is vital to ask them if they are taking any relevant medications such as warfarin. If an elderly patient on warfarin has a severe nosebleed and is hypotensive and has a raised INR, then for rapid and complete reversal you should give prothrombin complex concentrate (immediate replacement of vitamin K dependent coagulation factors) and vitamin K (the exact regimen will depend on why the patient is taking warfarin in the first place). Prothrombin complex concentrate is less likely to cause fluid overload than fresh frozen plasma.
General measures
You should admit most patients with a nasal pack. It is routine practice in most NHS hospitals to admit patients with nasal packing but you could send some patients home. Young and fit patients with responsible relatives or friends can be sent home with an anterior pack. All patients with a posterior pack require admission, as the epistaxis is normally more severe and the packs have to remain in situ for approximately two days. Routine bloods should be sent off in those with a bad bleed or those that require admission. Not all patients need have a coagulation profile done.4 It depends on the history. Remember to resuscitate the patient if necessaryPatients should be encouraged to rest. Some patients may benefit from a low dose of diazepam for a calming effect. They should also receive mouth washes to dislodge clots in the oropharynx
Most anterior packs should be removed after 24 hours and the nasal cavity re-examined in case cautery is required
Remember - epistaxis is frequently idiopathic but it can be a manifestation of a possible underlying pathology. Your patient should undergo further investigations according to the history
Learning bite
Always remember to examine the nose. You may discover expected or unexpected findings.For example you may find a perforated nasal septum. Perforation can arise due to trauma, cocaine abuse, an abscess, or certain diseases, such as Wegener's granulomatosis.
Pyogenic granulomas may also occur. These appear as dark red masses in the nose. They are a mass of small blood vessels and connective tissue which forms due to chronic inflammation, after infection, or due to the presence of a foreign body.
All patients with a posterior pack require admission, as the epistaxis is normally more severe and the packs have to remain in situ for approximately two days. You should admit most patients with a nasal pack. It is routine practice in most NHS hospitals to admit patients with nasal packing but you could send some patients home. Young and fit patients with responsible relatives or friends can be sent home with an anterior pack.