Abnormal liver function tests
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Abnormal liver function testsBMJ Learning
Abnormal liver function testsAlcoholic liver disease is the most common liver disease in the developed world. Alcoholic liver disease is a major cause of morbidity and mortality in the Western world. Deaths from alcohol related liver disease in the UK rose from 6 per 1000 men in 1980 to 13.5 per 1000 men in 2000, and from 4.1 per 1000 women in 1980 to 7.2 per 1000 women in 2000. Alcohol is the most important cause of cirrhosis in the Western world.
Alcoholic liver disease
This is one of the most common reasons for mildly abnormal aminotransferase levels in the Western world. The quantity and duration of alcohol use are important for establishing a diagnosis.A clue to the diagnosis is that the
AST/ALT ratio in these patients is typically 2:1 or more.
When a patient's history is not reliable, increased GGT levels with normal ALP levels and macrocytosis make alcohol induced liver damage more likely.
Chronic viral hepatitis
Is one of the most common causes of mild abnormality of aminotransferase levels worldwide. Infection by hepatitis C and B viruses has a high prevalence, with 170 000 000 and 350 000 000 infected people in the world, respectively. Positive antibodies to hepatitis C virus in a patient with a history of risk factors for infection (blood transfusion, exposure to dirty needles, intravenous drug use) and mildly abnormal aminotransferase levels strongly suggest current hepatitis C virus infection.
Detection of hepatitis C virus RNA in serum by polymerase chain reaction technique is used to confirm active viral infection and replication.
A negative polymerase chain reaction in patients positive for anti-hepatitis C virus antibodies needs to be repeated in three months to avoid false negatives. If aminotransferases abnormality persists despite negative viraemia you must rule out other causes of liver injury.
There are three main histological stages of alcohol related liver damage:
which can overlap and coexist both histologically and clinically:• Steatosis
• Hepatitis
• Cirrhosis
Steatosis is a predictable histological abnormality that develops in many heavy drinkers. It completely reverses within several weeks of stopping drinking. Steatosis may cause mild abnormalities of liver function tests, including elevated ALT. Steatosis will occur in most adults after a few months of heavy drinking. On its own (that is in the absence of fibrosis or hepatitis) it will reverse on abstinence without long term consequences.
Marked elevation of bilirubin and prothrombin times suggests alcoholic hepatitis in a heavy drinker presenting with jaundice.
ALT levels are usually below 100 IU/l and rarely above 400 IU/l in patients with alcoholic hepatitis. Higher levels suggest another possibly coexistent pathology (for example paracetamol overdose, ischaemic hepatitis, or viral infection).
Alcoholic hepatitis is typically associated with a neutrophilia reflecting the immunological basis of hepatitic damage. Jaundice with a low white cell count suggests cirrhosis with hypersplenism or bone marrow toxicity due to alcohol.
Alcoholic hepatitis may be associated with low grade pyrexia (below 38.0°C). High pyrexia suggests coincidental sepsis (for example spontaneous bacterial peritonitis or aspiration pneumonia).
Positive antinuclear factor is not associated with alcoholic hepatitis and suggests autoimmune hepatitis.
Advanced age, malnutrition, and a high white cell count are adverse prognosis factors in patients with alcoholic hepatitis. Associated renal impairment is a marker of extremely poor prognosis. There is evidence from randomised controlled trials and meta-analyses that corticosteroids may improve prognosis in selected patients with severe alcoholic hepatitis. Abstinence may markedly improved prognosis in end stage alcoholic cirrhosis
Both non-alcoholic steatohepatitis and hazardous drinking may lead to elevated GGT levels. Very high levels (more than five times the upper limit of normal), however, suggest hazardous drinking because alcohol consumption induces levels of GGT. Typically, IgA levels increase with alcoholic liver disease (sometimes associated with polyclonal rises in other immunoglobulins). IgM elevation is typically associated with primary biliary cirrhosis.
A low ratio of ALT:AST suggests non-alcoholic steatohepatitis. An AST level greater than the ALT level suggests alcohol related liver disease.
Alcoholic liver disease is typically associated with marked elevation of MCV.
Urea levels are often low in alcohol related cirrhosis due to reduced hepatic metabolism of protein and reduced protein intake.
Hazardous drinking is defined as a quantity or pattern of alcohol consumption that places patients at risk for adverse health events, while
harmful drinking is defined as alcohol consumption that results in adverse events (eg, physical or psychological harm).
Heavy drinking is defined as a quantity of alcohol consumption that exceeds an established threshold value.
The National Institute of Alcohol Abuse and Alcoholism sets this threshold at
more than 14 drinks per week for men (or >4 drinks per occasion);more than 7 drinks per week for women (or >3 drinks per occasion); and more than 7 drinks per week for all adults 65 years and above. Individuals whose drinking exceeds these guidelines are thought to be at increased risk for adverse health events.
• hazardous drinking was defined as an average consumption of 21 drinks or more per week for men (or 7drinks per occasion at least 3 times a week), and 14 drinks or more per week for women (or 5 drinks per occasion at least 3 times a week).
• Because hazardous and heavy drinking are similarly defined (ie, a quantity or pattern of alcohol consumption that exceeds a specific threshold and may increase risk for adverse health events), we will use 1 term, hazardous drinking, to define this type of drinking disorder.
•
Harmful drinking is defined as alcohol consumption that results in physical or psychological harm. This disorder is also recognized by the WHO and is defined by criteria of the International Classification of Diseases, 10th Revision (ICD-10), which include
• clear evidence that alcohol is responsible for physical or psychological harm,
• the nature of the harm is identifiable,
• alcohol consumption has persisted for at least 1 month or has occurred repeatedly over the previous 12-month period, and
• the individual does not meet the criteria for alcohol dependence.
Recommended amount of alcohol
The amount of alcohol contained in any alcoholic drink is measured in units. A unit is equivalent 10ml of pure alcohol.The recommended daily limits for alcohol consumption are:
no more than 3-4 units per day for men
no more than 2-3 units per day for women
If you regularly exceed the recommended daily limits, you are putting your health at risk.
Pregnant women and women trying to conceive should avoid drinking alcohol. If they do choose to drink, they should not drink more than 1-2 units of alcohol once or twice a week and should avoid getting drunk.
How to measure units
Any drink that you buy will contain a measurement of its alcohol by volume (ABV). ABV is a measurement of how much of that drink is made up of pure alcohol.The easiest way to work out how many units of alcohol a drink provides is:
find out what the drink’s ABV is then multiply that by how many millilitres of liquid are in the drink then divide that by 1,000 So for a standard pint of strong lager:
its ABV would be 5% a pint contains 568ml
5 times 568 equals 2,840
divide that by 100, to give a measurement of 2.8 units
The units found in some standard drink sizes are listed below:
a can of standard lager, beer, bitter – 1.8 units
a can of strong lager, beer, bitter – 2.2 units
a pint of standard lager, beer, bitter – 2.3 units
a pint of strong lager, beer, bitter – 2.8 units
a small glass of wine (125ml) – 1.5 units
a large glass of wine (250ml) – 3 units
a bottle of alcopops – 1.4 units
a glass of spirits (25ml) – 1 unit
a bottle of wine – 9 units
a one litre bottle of standard cider – 4 units
a one litre bottle of strong cider – 9 units
a 700ml bottle of spirits – 27-28 units
Types of alcohol misuse
• hazardous drinking• harmful drinking
• dependent drinking
Hazardous drinking
Hazardous drinking is defined as when a person drinks over the recommended weekly limit (21 units for men and 14 units for women).It is also possible to drink hazardously by binge drinking, even if you stick within your weekly limit.
Binge drinking is when you drink an excessive amount of alcohol in a short space of time – eight units in a day for men, six units in a day for women.
Abinge drinker is defined as someone who drinks over half the recommended number of units for a week in a single session,eight units in a day for men, six units in a day for women, in a short space of time
Hazardous drinking, especially binge drinking, also carries additional risks such as:
being involved in an accidentbecoming involved in an argument or fight
taking part in risky or illegal behaviour when drunk – such as drink driving
Harmful drinking
drinks over the recommended weekly amount and has experienced health problems directly related to alcohol.• depression
• alcohol-related accident
• acute pancreatitis
• high blood pressure ,heart disease
• cirrhosis
• cancer, mouth, liver, bowel and breast.
Dependent drinking
Alcohol is both physically and psychologically addictive and it is possible to become dependent on alcohol.Dependent means that a person
feels that they are unable to function without alcohol and the consumption of alcohol becomes an important – or sometimes the most important – factor in their life.
Depending on the level of dependence, a person can experience withdrawal symptoms if their supply of alcohol is suddenly stopped. Withdrawal symptoms can be both physical and psychological.
Physical withdrawal symptoms include:
hand tremors (‘the shakes’)
sweating
nausea
visual hallucinations
seizures
Psychological withdrawal symptoms include:
Depression ,anxiety ,irritability ,restlessnessinsomnia
Moderately dependent drinkers ,symptoms are mild to moderate.
Severely dependent drinkers do experience withdrawal symptoms, which are usually severe.
Most severely dependent drinkers fall into a pattern of ‘relief drinking’, where they drink to avoid withdrawal symptoms.
Severely dependent drinkers usually have an extremely high tolerance to alcohol, and are able to drink amounts that would incapacitate or even kill most other people.
What Is Binge Drinking?
Binge drinking used to mean drinking heavily over several days. Now, however, the term refers to the heavy consumption of alcohol over a short period of time (just as binge eating means a specific period of uncontrolled overeating).Today the generally accepted definition of binge drinking in the United States is the consumption of five or more drinks in a row by men — or four or more drinks in a row by women — at least once in the previous 2 weeks. Heavy binge drinking includes three or more such episodes in 2 weeks.
Acute alcoholic hepatitis
characterised by hepatocellular injury with associated inflammation and a variable amount of fibrosis. Hepatitis often occurs after prolonged heavy alcohol consumption and typically presents with jaundice, low grade fever, and tender hepatomegaly. Jaundice often paradoxically worsens after several days of abstinence before improving. Patients with severe alcoholic hepatitis may develop significant coagulopathy and acute renal failure due to hepatorenal syndrome. Liver function tests typically show elevated bilirubin and PT with a mildly raised WCC (predominantly a neutrophilia). ALT is usually less than 100 IU/l.Cirrhosis
Aminority of hazardous drinkers go on to develop significant fibrosis of the liver with formation of nodules. This may be associated with normal or near normal liver function tests. Although irreversible, patients may live many years with few obvious effects particularly with cessation of drinking. Decompensation of cirrhosis triggered by sepsis, bleeding, continued excessive drinking, or other causes may be associated with reduced albumin, raised bilirubin, and prolonged coagulation. Portal hypertension may present with varices, ascites, and hepatic encephalopathy.
Calculating Maddrey's discriminant function
• MDF =• bilirubin (µmol/l) + (PT - control (secs) x 4.6)
17Alcoholic hepatitis carries a significant mortality. The most established tool for predicting survival in alcoholic hepatitis is Maddrey's discriminant function (MDF) .An MDF ≥32 indicates a poor prognosis with a risk of mortality around 35%
A newer prognostic score - the Glasgow alcoholic hepatitis score - has more recently been published along with extensive multicentre validation. This score uses patient age, WCC, urea, PT ratio, and bilirubin to predict mortality, and appears more accurate than the MDF for predicting prognosis. It has yet to be applied in large scale clinical trials.
Chlordiazepoxide will be metabolised at a reduced rate and the dosage should be moderated and stopped temporarily if he becomes very drowsy because of drug accumulation, hepatic encephalopathy, or both. However, it should not be omitted because the development of delirium tremens carries significant increased risks to the patient and other people on the ward.
TIPSS provides a minimally invasive method for reducing portal pressure thereby decreasing further variceal bleeds and improving ascites control. It is most effective in patients with cirrhosis without severe synthetic liver failure
but may be used as a "bridge" to transplantation. Liver function may worsen after TIPSS and hepatic encephalopathy may worsen.
Raised ferritin level may result from alcoholic liver disease without haemochromatosis.Ferritin levels may be elevated as part of the acute phase response to alcoholic hepatitis.
Peptic ulcer disease is still the most common cause of gastrointestinal bleeding even in patients with cirrhosis.
The inpatient mortality rate for a first episode of variceal haemorrhage is about 30%.
The role of artificial liver support (using either biomechanical systems or albumin recirculation dialysis based systems such as MARS) is unclear.
These systems may have a role in severe acute liver failure but there is less experience with long term use while awaiting transplantation.
ALT levels are usually below 100 IU/l and rarely above 400 IU/l in patients with alcoholic hepatitis.
Higher levels suggest another possibly coexistent pathology (for example paracetamol overdose, ischaemic hepatitis, or viral infection).
Autoimmune hepatitis
Suspect autoimmune hepatitis in young and middle aged females with concomitant autoimmune disorders (for example, rheumatological diseases and autoimmune thyroiditis). The prevalence of the disease is about 1:6000 to 1:7000. Up to 80% of patients with autoimmune hepatitis may have polyclonal hypergammaglobulinaemia in the absence of liver cirrhosis.Testing for antinuclear antibodies, antibodies to smooth muscle, antiliver-kidney microsomal antibodies, and antibodies to the soluble liver antigen has an important diagnostic role and is used to categorise autoimmune hepatitis.
Type 1 autoimmune hepatitis, characterised by the presence of antinuclear and/or smooth muscle antibodies, is the most common form of autoimmune hepatitis and usually affects young women
Type 2 autoimmune hepatitis is characterised by the presence of antiliver-kidney microsomal antigens antibodies and is a disease with a prevalent onset in childhood
Type 3 autoimmune hepatitis is clinically indistinguishable from type 1 except for the presence of antibodies to the soluble liver antigen
Criteria for diagnosing autoimmune hepatitis are complex and include liver biopsy.
Hereditary haemochromatosis
This is an autosomal recessive condition with a homozygotic frequency of 1:200 to 1:400.The disease is characterised by pathological deposition of iron in the liver, pancreas, and heart. Patients who are homozygous for the C282Y mutation have the greatest risk of iron overload, while iron overload may occur in people who are compound heterozygotes for the C282Y/H63D mutation and in a minority of H63D homozygotes.
Although positive family history and the presence of congestive heart failure and diabetes mellitus may aid the diagnosis, you should also measure serum ferritin, iron, and
transferrin saturation index (serum iron/total iron binding capacity)
in patients with altered aminotransferase levels.
Symptoms of haemochromatosis may arise late during the course of the disease.
High serum ferritin levels and, more importantly, a transferrin saturation index larger than 45% strongly suggest haemochromatosis.
Mutation analysis for the HFE gene may confirm the diagnosis, although a negative test does not exclude the presence of non-HFE-related haemochromatosis. In these patients you should suggest a liver biopsy for both diagnostic and prognostic purposes.
Finally, you should screen first degree relatives of affected patients by genetic testing even if they are asymptomatic and have normal liver enzymes. Normal liver biochemistry can be present in young people.
Fatty infiltration of the liver
with or without associated inflammation and fibrosis, is thought to be the most common cause of mild abnormality of aminotransferase levels in the general population in Western countries. Nevertheless, the exact prevalence of non-alcoholic fatty liver disease is quite difficult to ascertain because the disease is asymptomatic and there are no blood tests to confirm the diagnosis.Furthermore, although risk factors for non-alcoholic fatty liver disease, such as obesity, diabetes mellitus, and hyperlipidaemia, are present in a variable proportion of affected patients they are not specific.
Therefore the initial evaluation of a patient with abnormal liver function tests and suspected non-alcoholic fatty liver disease should include a complete serological evaluation to exclude other causes of liver disease.
Finally, although (liver ultrasonography, computed tomography, or magnetic resonance imaging) may further increase the likelihood of diagnosis, liver biopsy is the only means able to diagnose the disease and assess and stage inflammation and fibrosis (non-alcoholic steatohepatitis). Because there is no definite treatment for non-alcoholic fatty liver disease, you should consider the general clinical context of the individual when deciding whether and when to perform a liver biopsy.
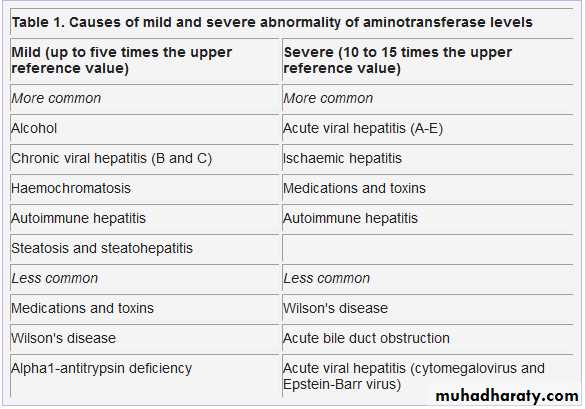
Although there is no universal definition of mild, moderate, and severe abnormality of aminotransferase levels, the degree of abnormality can be practically considered to be:
Mild when the enzyme level is less than five times the upper reference value
Severe when AST and ALT levels are greater than 10 to 15 times the upper reference value.
Although not the rule, chronic liver diseases are often characterised by mild abnormality of aminotransferase levels, whereas severe abnormality is usually encountered in patients with acute hepatic injury.
A normal liver function test does not necessarily exclude liver disease. The following tests usually reflect integrity of hepatocytes or cholestasis rather than liver function:
• Aminotransferase levels
• Gamma-glutamyltransferase (GGT) levels
• ALP levels.
The following tests may provide useful information on how well the liver is
functioning:
• Serum albumin levels
• Bilirubin levels
• Prothrombin time.
Aminotransferases
Alanine aminotransferase (ALT) is considered more specific for hepatocellular injury because it is predominantly represented in the liver, with low concentrations in other tissues.Aspartate aminotransferase (AST) is also expressed in the heart, skeletal muscle, and red blood cells. AST and ALT are released in the bloodstream after hepatocellular injury (not necessarily hepatocellular death).
Alkaline phosphatase
Both liver and bone diseases can cause pathological elevation of serum ALP levels, although increased ALP may originate from the placenta, kidney, intestine, and leukocytes.You can find increased serum ALP levels in some physiological conditions, such as adolescence (bone origin) and pregnancy (placenta origin). Both synthesis and release of ALP are stimulated by cholestasis and release of ALP from liver cell membranes is increased by accumulation of bile salts.
Gamma-glutamyltransferase
This enzyme is present in renal tubules, the liver, pancreas, and intestine. Although GGT levels are higher in organs other than the liver, GGT serum activity comes from the liver. GGT is contained in the microsomes and drugs such as anticonvulsants and oral contraceptives can induce its activity. The mechanisms of GGT alteration are similar to those described for ALP.
You may find abnormal liver function tests in up to 17.5% of the asymptomatic general population, although in 58% of these patients they are not adequately followed up.
Evaluate both the clinical context in which abnormal liver function tests are found and the degree of alteration (mild versus severe)
Suggest liver ultrasonography to evaluate signs of advanced liver disease, fatty infiltration of the liver, and obstacles to bile flow.
Liver biopsy is the only way of accurately staging liver fibrosis, although it is sometimes unnecessary when obvious clinical or instrumental signs of cirrhosis are evident
Although some biochemical scores can help to stage liver disease non-invasively and more sophisticated biochemical markers of liver fibrosis are available, they have not been validated in clinical practice and their practical role has not yet been defined
CA-125 levels may be markedly elevated in patients with ascites due to any cause.
The D-dimer test is non-specific and is raised in most patients with any acute illness.Abdominal ultrasound is useful for assessing liver size, presence of other pathology, and evidence of portal hypertension.
Steroids are useful only when the MDF is greater than 32. The UK and European transplant centres have a widely accepted limit of at least six months' abstinence before transplantation. In many cases this delay allows even dramatically reduced liver function to improve so that transplantation is unnecessary.
Corticosteroids may have a role in treating patients with severe alcoholic hepatitis but should not be started until a sepsis screen has excluded infection. They should also be avoided in patients with gastrointestinal bleeding.
The use of corticosteroids in alcoholic hepatitis to reduce cytokine production and diminish the inflammatory response has been studied for several decades. But consensus has not been reached on their efficacy. Meta-analysis of three randomised trials showed an improvement in 28 day survival, but benefit was not seen at later time points.
The side effects of corticosteroids are justified only in patients with severe alcoholic hepatitis (MDF >32).
Pentoxifylline showed promise in one randomised controlled trial of patients with an MDF ≥32 who were not treated by steroids. The drug was associated with a marked reduction in the incidence of hepatorenal syndrome and improved 28 day mortality with no significant side effects.
No trial has assessed combination therapy with steroids and pentoxifylline.
Because ALP levels may be abnormal due to non-hepatic conditions and GGT can be induced by alcohol and drugs (for example, anticonvulsants), assessing these levels simultaneously may help you interpret the abnormality.
In patients with alcohol induced liver disease,
AST levels can be found in a range below six to seven times the upper reference value in 98% of patients. Alcoholic liver disease is characterised by a low ALT activity. This is explained by the fact that both AST and ALT need vitamin B-6 for their enzymatic reaction, although the effect of vitamin B-6 deficiency is greater on ALT activity than on AST activity and people with alcoholic liver disease usually have vitamin B-6 deficiency.Abnormal GGT levels and normal ALP levels together with an AST predominant pattern and macrocytosis is suggestive of alcohol induced liver disease. In patients with alcoholic liver disease, the AST:ALT ratio is typically above 2 or greater.
• Which one of the following characteristically causes mildly elevated aminotransferase levels (less than five times the upper reference value)?
•
• a : Acute viral hepatitis
• Acute viral hepatitis (A to E) is responsible for increase in aminotransferase levels that may exceed 10 to 15 times the upper reference value.
• b : Ischaemic liver injury
• Ischaemic liver injury is associated with severe increase in aminotransferase levels (up to 70 times the upper reference limit).
• c : Paracetamol overdose
• Paracetamol intoxication is usually associated with severe (10 to 15 times the upper reference value) abnormality of aminotransferase levels and is responsible for more than half of the episodes of acute liver failure in the UK.
• d : Chronic viral hepatitis
• Chronic viral hepatitis together with alcohol abuse, autoimmune liver disease, haemochromatosis, and fatty liver disease are the most common causes of mild abnormality of aminotransferase levels in Western countries.
Liver biopsy can provide invaluable diagnostic information about the degree of necrosis and inflammation (grading) and fibrosis (staging), independently of the cause of liver disease.
In a large series of percutaneous liver biopsies, severe complications had an incidence of 0.1% to 0.3%. The mortality rate was 9/100 000, mainly in patients with cirrhosis or malignant diseases.
In patients with suspected liver cirrhosis liver biopsy cannot provide further diagnostic clues when unequivocal signs of portal hypertension are already present.
All the major (A, B, C, D, and E) and
minor (cytomegalovirus, Epstein-Barr virus, herpes virus, adenovirus) hepatitis viruses can be responsible for increased aminotransferase levels, which may exceed 10 to 15 times the upper reference value. Wilson's disease may also present with severely elevated aminotransferase levels due to massive release of copper and is responsible for fulminant hepatitis.Ischaemic and toxic hepatitis may cause a severe increase in aminotransferase levels (up to 70 times the upper reference limit). Because zone 3 of the hepatic acinus is more prone to ischaemic and toxic damage and is richer in AST, this aminotransferase tends to peak before ALT when hypoxia and toxins are the cause of the hepatic damage. About 60% of cases of severely elevated hepatic AST may be attributable to ischaemic or toxic liver injury.
You should suspect ischaemic or hypoxic damage when precipitating events are present. These can be:
• Hypotension
• Myocardial infarction
• Haemorrhage
• Other low flow haemodynamic conditions.
In these patients, the presence of high serum concentrations of lactate dehydrogenase as a marker of ischaemic damage may further support the diagnosis. In ischaemic hepatic injury, aminotransferase levels tend to decrease rapidly after peaking once the cause has resolved.
The diagnosis of acute hepatitis A and E virus infection and of hepatitis D virus superinfection can be made by virus specific IgM antibody assays and
acute hepatitis B virus infection can be diagnosed by detecting HBsAg and antiHBc IgM antibodies in serum. The diagnosis of acute hepatitis C virus infection relies on molecular biology tests (detection of hepatitis C virus RNA in serum) because anti-hepatitis C antibodies usually become detectable from four to six weeks after the acute onset of the disease. Diagnosis of infection by minor hepatotropic viruses can be made by serological measurement of specific antibodies or by detecting viral antigen in serum.
Both ALP and GGT levels can be mildly abnormal during the course of illnesses that cause either mild or severe abnormality of aminotransferase levels. In this situation they can be interpreted as non-specific markers of generic liver disease. However, some specific liver diseases may present with severely altered levels of these enzymes. In fact, severe abnormality of ALP and GGT levels may be the initial presentation of:
• Primary biliary cirrhosis
• Primary sclerosing cholangitis.
In this regard, a history of itching in a middle aged woman with concomitant autoimmune diseases (autoimmune thyroiditis, rheumatoid arthritis) should prompt testing for antimitochondrial antibodies (positive in 95% of patients with primary biliary cirrhosis).
A history of inflammatory bowel disease (most commonly ulcerative colitis, associated in about 70% of patients) should alert you to primary sclerosing cholangitis.
healthy people, conjugated bilirubin is virtually absent from serum mainly due to the fast process of bile secretion. It becomes elevated once the liver has lost at least half its excretory capacity. Increased conjugated bilirubin levels therefore usually signify important liver disease. Conjugated hyperbilirubinaemia and hypertransaminasaemia may suggest acute viral hepatitis or toxic or ischaemic liver injury. On the other hand, conjugated hyperbilirubinaemia and an increase in ALP together with a negligible increase in aminotransferase levels may be present in cholestatic drug reactions, or can be the late presentation of previously unrecognised autoimmune cholestatic diseases
alcohol withdrawal
People become dependent on alcohol if they have a compulsion to drink on a regular basis.There are three components to alcohol dependence:
• A subjective awareness of a compulsion to drink
• An increase in alcohol tolerance
• Withdrawal symptoms.
Alcohol withdrawal occurs when there is a sudden drop in the level of blood alcohol. Patients are more likely to present in the morning following an overnight alcohol fast. Patients usually develop alcohol withdrawal after a prolonged period of high blood alcohol.
The levels of alcohol associated with withdrawal vary between men and women. In men they are:
10 units of alcohol or more a day for 10 to 20 years. A unit is equivalent 10ml of pure alcohol.
In women they are:
7.5 units of alcohol or more a day for five to 10 years.Alcohol ingestion and elimination
Ethanol is the only form of alcohol found in drinks for human consumption. It has a simple chemical structure and is rapidly absorbed in the small intestine. It is possible to detect alcohol in blood within minutes of its ingestion. Certain factors influence the rate of absorption of alcohol.
The following factors can increase the rate of absorption of alcohol:
• The concentration of alcohol in the drink
• The speed of consumption
• Other chemicals in the drink, such as caffeine and sugar, can change the rate of absorption and the breakdown of alcohol, or they can influence behaviour.
Sex
Women usually have a higher percentage of body fat and a lower percentage of body water than men, which causes them to absorb more alcohol than men.Race
There are no racial differences in the absorption of alcohol
There are genetic differences between ethnic groups in enzymes that metabolise alcohol These genetic differences have been implicated in the high incidence of alcohol sensitivity observed in South East Asian people4
Once within the bloodstream, alcohol begins to affect the central nervous system. Although the initial sensations are of relaxation and well being, excessive consumption affects judgment, perception, and, eventually, self control. Alcohol also affects the autonomic nervous system. It initially acts as a vasodilator and a diuretic. With excessive consumption, it can contribute to hypothermia, dehydration, and electrolyte disturbance.
About 90% of alcohol is metabolised in the liver. The rest is eliminated through urination, exhalation, and perspiration. An average 70 kg man metabolises alcohol at a rate of one unit an hour. Other factors such as weight, age, and intake of food may change this.
The following factors can decrease the rate of absorption of alcohol:
The presence of food in the stomach delays absorptionThe person’s body mass index
Fat slows the absorption of alcohol; patients with a high body mass index usually absorb alcohol more slowly because they have more fat.
Alcohol units
Alcohol consumption should not exceed 28 units for men and 21 units for women in one week.
In a single drinking session, alcohol consumption should not exceed four units in men and three units in women.
Alcohol units are calculated by using:
The volume of alcohol in millilitresThe alcohol strength - this is its percentage alcohol by volume (% ABV).
One unit is equivalent to 10 ml of pure alcohol:
One standard glass of wine 175 ml at 12% ABV = 2.1 units
One bottle of wine 750 ml at 12% ABV = 9 units
One pint of beer 568 ml at 3.5% ABV = 2 units
One pint of beer 568 ml at 5% ABV = 2.8 units
One single glass of spirits 25 ml at 40% ABV = 1 unit.
The two most serious complications of alcohol withdrawal are
delirium tremens and Wernicke’s encephalopathyBenzodiazepines are used in the treatment of alcohol withdrawal
withdrawal are at risk of seizures and hallucinations
It is important to screen all patients who present with alcohol withdrawal for underlying liver disease
How common is alcohol withdrawal?
According to the Institute of Alcohol Studies factsheet for excessive and problem drinking in England and Wales 2007:
26% of adults aged 16 to 64 have a disorder of alcohol use ,Of these, 38% are male and 16% are femaleThis is equivalent to about eight million people in England and Wales,21% of men and 9% of women are binge drinkers A binge drinker is defined as someone who drinks over half the recommended number of units for a week in a single session
About 4% of adults have alcohol dependence - this is equivalent to over one million people.
How alcohol affects the brain
Alcohol affects the body in multiple ways. It increases levels of endogenous opioids and activates serotonin and dopamine in the brain. The effects of alcohol include the sensations of euphoria and well being. These effects contribute to its repeat ingestion and cause alcohol dependence in those people who have the risk factors, for example people who suffer from depression.The damaging effects of long term alcohol dependence are associated with
Activation of the glutamate receptors, known as the N-methyl-D-aspartate receptors, in the brain This causes the sensation of intoxication, loss of judgment, and impaired cognition .Chronic activation of these receptors can lead to cell death - this causes cerebellar degeneration and seizuresCerebellar degeneration is the probable mechanism that causes Wernicke-Korsakoff syndrome
Activation of the gamma-aminobutyric acid A-type receptors
This causes a downregulation of the production of intrinsic gamma-aminobutyric acid.A reduction in the production of gamma-aminobutyric acid occurs with an excess in the consumption of alcohol
Chronic activation of these receptors causes sedative effects and impaired motor skills, such as lethargy and poor coordination.
The consequences of alcohol dependence are:
Metabolic abnormalitiesThese include hypokalaemia, due to renal and extrarenal losses, and hypomagnesaemia,Extrarenal losses occur through perspiration If severe, these abnormalities can also increase the risk of seizures
Hypovolaemia
This is due to fluid loss from vomiting, renal excretion, and vasodilatation.Alcohol activates the autonomic nervous system, which causes vasodilatationHypovolaemia can cause cardiac failureand death
Malnutrition
Thiamine deficiency, vitamin C and folate, and low levels of phosphate predispose to rhabdomyolysis, cardiac failure, and Wernicke-Korsakoff syndrome.
Alcoholic liver disease
It is important not to overlook underlying alcoholic liver disease during the acute presentation of alcohol withdrawal. Altogether, 4% of people who drink about six units of alcohol a day have cirrhosis of the liver. Up to 10% of these patients have evidence of liver disease. Women who drink three to eight units of alcohol a day have a higher risk of developing liver disease than men who drink the same amount. The risk of developing liver disease is related to the amount of alcohol the person drinks. People who drink more than 70 units a week have a 7% risk of developing cirrhosis and about a 20% risk of developing alcoholic liver disease.
Alcohol withdrawal
Alcohol withdrawal often presents with both medical and psychiatric signs and symptoms. A sudden reduction or cessation in alcohol intake causes a reactive hyperactivity of the central and autonomic nervous systems. Onset of alcohol withdrawal can occur as early as six hours after the last drink. Symptoms and signs of withdrawal can last between 24 hours and two weeks. The course of alcohol withdrawal usually occurs in two separate peaks:Simple withdrawal
This has a short duration of one to four days.It is associated with nausea, tremors, anxiety, sweating, and seizuresSeizures that relate to alcohol withdrawal are usually generalised and take place 12 to 48 hours after stopping alcohol ,Seizures occurring more than 48 hours after stopping alcohol are rare
Complex withdrawal
This can sometimes last up to nine or 10 days.Symptoms and signs of complex withdrawal are more severe. It is associated with confusion, hallucinations, paranoia, and delirium tremens.
Complications of alcohol withdrawal
in order of occurrence, are seizures, hallucinations, and delirium tremens:Seizures
50% of seizures occur on admission and 90% occur within nine hours of admission to hospital
Hallucinations
50% of hallucinations occur within 21 hours and 90% occur within 64 hours of admission to hospital
Delirium tremens
Of the people that develop delirium tremens, 50% will develop the symptoms within 46 hours and 90% within 85 hours of admission to hospital.
Delirium tremens and Wernicke's encephalopathy
The two most serious consequences of alcohol withdrawal .
Delirium tremens
Acute episode of delirium caused by a sudden abstinence from alcohol. It occurs in those people with a long history of alcohol consumption and it can take place in up to 20% of patients with alcohol withdrawal. It usually occurs two to three days after the cessation or reduction of alcohol. Without treatment, it can last up to 72 hours and may result in death in 15% to 20% of patients.
The signs and symptoms of delirium tremens include:
• Hallucinations• Excessive sweating
• Profound agitation
• A fever greater than 38.5°C
• Tachycardia.
Complications of delirium tremens include:
ArrhythmiasDehydration
Seizures
Death occurs in 15% to 20% of patients due to cardiovascular and respiratory failure or cardiac arrhythmias,Correct management reduces mortality to less than 1%.
Patients who are most at risk of death from delirium tremens are those with:
A temperature of over 40°C
Tachycardia - a heart rate of greater than 100
Dehydration
A concurrent illness or infection.
alcoholic hallucinations
Alcoholic hallucinations can also occur in the absence of delirium tremens. These are transient tactile, visual, or auditory hallucinations in the setting of clear consciousness. They are often in the form of a conversation in the second person and may be derogatory. You should involve the psychiatry team in the management of these patients
Wernicke's encephalopathy
A reversible condition caused by a deficiency of thiamine (vitamin B-1). People with alcohol dependence often suffer with malnutrition. This is because these patients replace food with alcohol. Thiamine deficiency is the result of malnutrition and a reduction in intake of the vitamin. There is a 70% reduction of thiamine absorption in malnourished patients who are abstaining from drinking alcohol. Absorption is further reduced if these patients continue to drink.It is possible to precipitate Wernicke’s encephalopathy by ingesting glucose or carbohydrate on a background of thiamine deficiency. The mechanism for this is unclear, but is thought to be a result of glucose using up the remaining thiamine stores.
Thiamine deficiency causes lesions to develop within multiple parts of the brain, including the cerebellum, grey matter, thalamus, hypothalamus, and brainstem nuclei. These lesions are due to cellular oedema or cell death.
Wernicke’s encephalopathy usually begins several days after a sudden cessation or reduction in alcohol intake. The classical signs are:
• Ataxia
• Ophthalmoplegia - this is usually of the external recti muscles
• Confusion or impairment of the short term memory.
Only 10% of patients present with these signs. Other signs include:
Nystagmus
Gaze palsies
Confabulation
Confusion.
Management of Wernicke's encephalopathy
If you give treatment early, you can reverse the signs of Wernicke’s encephalopathy. You should treat patients with intravenous thiamine.
Delayed management or incorrect treatment has a mortality rate of 17%. Incorrect treatment includes giving glucose before thiamine. Of the patients that survive, 85% will have permanent brain damage in the form of Korsakoff’s psychosis and 25% will need long term institutionalisation in order to receive full time care.
Wernicke-Korsakoff syndrome
Korsakoff's syndrome can occur in patients with a severe dependence on alcohol and, often as a consequence, malnutrition. The signs of Korsakoff’s syndrome include:Anterograde amnesia
This is an inability to formulate new memories memories prior to the onset of Korsakoff's syndrome remain intact
The preservation of immediate memory
The person is able to recall information immediately after it is mentioned
The preservation of implicit memory
The person is able to learn new motor skills or show an improvement in complex tasks, even if they do not remember learning these skills.This results from a failure of memory formation and storage, although new information is processed normallyConfabulation
The person fabricates stories to fill in the gaps in their memory.This is often due to confusion of past and present events.
Korsakoff’s syndrome is also associated with a loss of spontaneity, drive, and emotional expression. The chronic form of this syndrome is known as Korsakoff's psychosis.
It is possible to improve some aspects of short term memory by:
• Encouraging the patient to stop drinking alcohol
• Improving the patient’s diet
• Advising regular vitamin supplements, including thiamine
• Rehabilitation.
General amnesia is usually irreversible in patients with Korsakoff’s syndrome.
Patients can learn to live independently, but most need residential care. Patients with Korsakoff’s psychosis usually have damage to the brain and the liver due to persistent heavy drinking over many years
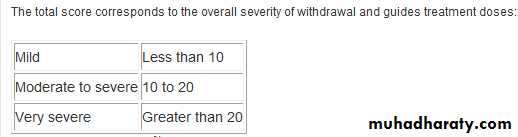
The two most common assessment tools for staging and monitoring alcohol withdrawal are:
• The clinical institute withdrawal assessment for alcohol (revised) scale• The alcohol withdrawal scale assessment.
You should use the assessment tools as part of the clinical assessment of patients with alcohol withdrawal and not as diagnostic instruments. You should repeat the assessment tool every four hours and adjust the management of patients accordingly.
Clinical institute withdrawal assessment for alcohol (revised) scale
This scale is widely used and has good prognostic value. The total score is indicative of the severity of the patient's deterioration during withdrawal. It is also a guide for giving benzodiazepines. With training, you can perform the assessment in less than one minute. The scale includes 10 symptoms and signs; nine of these are given a score between 0 and 7, and one (confusion) between 0 and 4:Nausea and vomiting
TremorSweats
Anxiety
Agitation
Tactile disturbances
Auditory disturbances
Visual disturbances
Headache
Confusion.
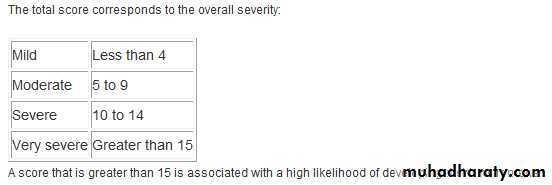
Alcohol withdrawal scale
This scale, for measuring the signs and symptoms of alcohol withdrawal, consists of seven items. You should give a score of 0 to 4 to each item, depending on the severity:Perspiration
Tremor
Anxiety
Agitation
Temperature
Hallucinations (visual, tactile, or auditory)
Orientation.
The symptoms and signs of acute alcohol withdrawal include:
Anxiety, agitation, or irritabilityNausea
Vomiting
Sweating
Insomnia
Fever
Tremor of the hands, tongue, or eyelids
Tachycardia
Hallucinations
Mild systolic hypertension
Anorexia
Seizures.
Assessing the patient
History and examination
While taking the patient's history, it is important to ask about previous episodes of alcohol withdrawal, including any complications of withdrawal and seizures that may have occurred
On examining the patient, it is important to assess their fluid status by examining them for signs of dehydration
While taking the history and examining the patient, you should also look for signs and symptoms of other life threatening conditions associated with alcohol withdrawal. These include:
Intracranial conditions - head injury, intracranial haemorrhage, encephalitis, space occupying lesions
Metabolic abnormalities - patients with alcohol withdrawal can present with hypoglycaemia
Medical problems associated with alcohol dependence - pancreatitis, infections, and decompensated liver disease
Complications of decompensated liver disease - gastrointestinal haemorrhage, spontaneous bacterial peritonitis, and encephalopathy.
Investigations
You should perform the following tests in all patients presenting with alcohol withdrawal:Blood glucose
Full blood count
Urea and electrolytes
Magnesium
Clotting screen
Liver function tests.
You should refer the patient to the gastroenterology team if you suspect that they have alcoholic liver disease. The specialists can request further tests, such as an abdominal ultrasound scan, which can help to confirm the diagnosis.
If you suspect the presence of other pathology, such as a space occupying lesion or spontaneous bacterial peritonitis, you should consider requesting:
A CT brain
A lumbar puncture
Microbiology cultures
Management
The aims of treatment are to:
Prevent the progression of symptoms
Reduce the risk of complications
Reduce morbidity and mortality
Improve patient comfort.1
Once you have diagnosed alcohol withdrawal, you should:
Correct and maintain the fluid and metabolic imbalance. If hypovolaemic, give the patient colloid or crystalloid fluids with the aim of achieving:
A systolic blood pressure of greater than 90 mm Hg
A heart rate of less than 100 beats a minute
A urine output of more than 0.5 ml/kg per hour
Correct any abnormal electrolytes, such as hypokalaemia.
Further treatment of alcohol withdrawal
Patients often experience confusion and delirium tremens at night time or after the dimming of lights. When managing patients with alcohol withdrawal, it is important to reduce sensory deprivation. You should:Manage the patient in a well lit side room
Provide supportive care with nursing staff who have training and experience .
Reassure the patient and give them information that will help them to reorientate into their surroundings
Check the patient’s pulse, respiratory rate, blood pressure, and oxygen saturations every two hours for the first 24 hours. These checks can subsequently be reduced to twice daily from day two You should continue checking these observations every two hours in patients with delirium tremens, until the patient’s symptoms improve.
Sedatives
Benzodiazepines are superior to other sedatives in the management of alcohol withdrawal.You should use intravenous benzodiazepines:
If a patient is not cooperating with treatment
To control agitation and seizures
You can give intravenous diazepam or lorazepam if the patient needs immediate control of their symptoms,This includes patients who are having a seizure or those who are refusing to take oral medication.
You should use chlordiazepoxide in other patients because: It provides a stable course of treatment ,It prevents seizures.
Longer acting benzodiazepines such as chlordiazepoxide provide a stable course of treatment with fewer breakthrough or rebound symptoms. They are also effective at preventing seizures.
These drugs have a lower potential for abuse than short and rapidly acting drugs.
Drug management of alcohol withdrawal
Oral chlordiazepoxide is the most common drug given for alcohol withdrawal.Day one
You should adjust the dose for each patient using a flexible regimen over the first 24 hours. In patients with delirium tremens, you should increase the frequency of observations. You may also need to increase the frequency of medication and continue titrating after 24 hours.
Give a starting dose of chlordiazepoxide 25 mg to 50 mg, depending on the severity of signs and symptoms. Using the clinical institute withdrawal assessment for alcohol (revised) scale, you can start a regimen as follows:
A score of 0 to 9 - you do not need to start treatment
A score of 10 to 14 - give 25 mg of chlordiazepoxide
A score of 15 or more - give 50 mg of chlordiazepoxide
You should assess the patient’s blood pressure, heart rate, and respiratory rate, and repeat the assessment tool every two hours
After clinical assessment and repeating the assessment tool, you can give subsequent doses of 25 mg to 50 mg, depending on the patient's withdrawal status
The baseline dose is the total of the initial and subsequent doses of chlordiazepoxide from the first 24 hours - you should use the baseline dose to calculate dosing regimens .
Day two
You should aim to give chlordiazepoxide four times a dayYou should aim to reduce the baseline dose by about 20%.
If you need to prescribe an extra dose, you should recalculate the total daily dose and continue a 20% dose reduction on the following days
The following is an example drug regimen:
The baseline dose from day one is 300 mg
The total dose for day two is 240 mg - given as 60 mg four times a day
The total dose for day three is 200 mg - given as 50 mg four times a day
The total dose for day four is 120 mg - given as 30 mg four times a day
The total dose for day five is 100 mg - given as 25 mg four times a day.
You can reduce observations to twice daily, unless the patient has complications.
Increase the starting dose in patients with severe alcohol withdrawal
Reduce the starting dose in patients with mild symptoms of withdrawal.
If a patient becomes violent or aggressive, you should refer to your local guidelines on the management of violent patients.
Using other benzodiazepines
You can give other benzodiazepines in equivalent doses; 25 mg of chlordiazepoxide is equivalent to 10 mg of diazepam or 1 mg of lorazepam.It may not be possible to give oral benzodiazepines in some patients with alcohol withdrawal, such as those who are having a seizure. In these patients, you can give either:
10 mg of intravenous diazepam every 30 to 60 minutes at a rate of 1 ml a minute, with a maximum dose of 30 mg in 24 hours
1 mg to 2 mg of intravenous lorazepam every five minutes until the patient is awake and calm or until the seizure stops.
You should monitor the respiratory rate every 15 to 30 minutes and have a continuous measurement of oxygen saturations in these patients.
Alcoholic seizures
you should give either:Intravenous diazepam at a rate of 2 mg a minute to a maximum dose of 10 mg to 20 mg
Intravenous lorazepam at a rate of 2 mg a minute to a maximum dose of 4 mg to 8 mg.
Maintain the patient's airway by using basic airway techniques in these patients. If you cannot do so, fast bleep the anaesthetist to manage the airway. It may be necessary to ventilate the patient.
In elderly patients, you should use the same regimen, but you should prescribe half the dose
Prescribing antipsychotic medication
If the patient has psychotic symptoms such as visual or auditory hallucinations, you should discuss the situation with the psychiatric team. They may be happy for you to give an antipsychotic drug under their supervision.
You should consider referring the patient to the psychiatric team if:
They have a psychiatric illness
Alcoholic hallucinations are present
There is a past or current history of self harm
They have delirium tremens and require regular antipsychotics.
Antipsychotic drugs can increase the risk of seizures. If you need to give antipsychotic drugs, you should refer the patient to a psychiatrist.
Clinical tip
You can give the following drugs to patients with alcohol withdrawal:Mild to severe symptoms: chlordiazepoxide
Recurrent seizures: lorazepam (2 mg intravenously)
Psychotic symptoms: haloperidol (1.5 mg to 5 mg two to three times daily) in combination with chlordiazepoxide.
Management and prevention of Wernicke's encephalopathy
To reduce the risk of Wernicke’s encephalopathy, you should give thiamine to all patients:With alcohol dependence
With suspected alcohol dependence
At risk of alcohol withdrawal
With symptoms of alcohol withdrawal.
You should start thiamine before giving fluids that contain glucose to prevent acute thiamine deficiency and Wernicke’s encephalopathy.
In the United Kingdom, intravenous thiamine is given in the form of Pabrinex ampoules. To prevent Wernicke’s encephalopathy, you should:
Dilute each ampoule in 100 ml of crystalloid
Give each dose over 30 minutes, three times a day for the first 24 to 48 hours
If the patient has Wernicke’s encephalopathy, you should give two ampoules three times a day for at least three days, or until no further clinical improvement is seen.
Patients with long term alcohol dependence and a poor diet often have deficiencies of other vitamins. After discontinuing intravenous thiamine, patients need to continue taking oral supplements for the long term. You should give:
Oral thiamine 200 mg once daily (or 100 mg three times a day)
Oral vitamin B strong, two tablets once a day
Vitamin B-2, B-6, C, D, and folic acid, usually through multivitamin supplements
Dietary and nutritional advice.
The long term management of alcohol withdrawal is as important as the acute management. You should encourage patients to attend support services following an episode of alcohol withdrawal. We believe that patients who attend support services are less likely to drink dangerously, suffer from malnutrition, or develop liver disease. Long term care is usually multidisciplinary and is available through hospitals or health centres.
You should review all patients before discharge. In the United Kingdom, there is some variation in service provision between hospitals. Some hospitals have an alcohol liaison nurse or a liaison psychiatric service for patients with alcohol dependence.
The liaison team will:
Assess all patients prior to discharge from hospitalOffer the patient a referral to social services in order to help them address any social problems which may be contributing to their alcohol dependence
Offer the patient either:
Brief interventions with the liaison nurse or a member of the liaison team
These are interviews to explore why the patient has alcohol dependence and to advise them on how they can prevent harmful drinking in the future
Referral to a psychiatrist
Patients with a history of mental health problems should have a longer course of treatment which is overseen by a psychiatrist.
If there is no alcohol liaison service, you should:
Encourage patients to seek support through local services
Inform the patient's GP and advise them to attend their GP for regular review
Offer a referral to social services
Refer the patient to the dietitian, who they should meet prior to discharge
Be empathic and sympathetic to the patient’s situation
Encourage patients and avoid criticism.
For those patients who do not wish to stop drinking, you should:
Encourage regular monitoring
Review the patient in an outpatient clinic
Advise the patient to continue taking thiamine and other vitamins
Offer dietary advice
Advise the patient to avoid participating in activities, such as driving, that may place themselves or others at risk of harm.
Alcohol withdrawal usually occurs within four days of a sudden reduction or cessation of alcohol.
Seizures occurring after 48 hours are rare.
Fever is associated with alcohol withdrawal, in particular with delirium tremens. You should only give antibiotics if you identify a source of infection.
The mortality rate from alcohol withdrawal is up to 20%. With correct management, this can be reduced to 1%.