Pruritus: a guide to diagnosis and treatment
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Key points
Pruritus is a complex symptom that can be caused by skin diseases, systemic diseases, nerve damage, and psychiatric causesThe most common causes of itch are insect bites, dry skin, contact dermatitis, and atopic dermatitis.
Chronic itch has emotional and cognitive components and impairs quality of life.
Secondary skin lesions characteristic of pruritus include excoriations, lichenification, prurigo nodules, and hyperpigmentation (or hypopigmentation in dark skin)
A variety of central and peripheral mediators is involved in causing pruritus. Your treatment should address these
Clinical tips
Elicit a detailed history, including the precise quality, timing, and distribution of itch, so you can institute focused therapyGood skin care may relieve pruritus. This includes adequate protection from harsh environments such as extreme cold and cleansing practices that do not dry the skin
In addition to good skin care, topical or oral medications may be necessary to treat pruritus.
Sedating antihistamines, antidepressants, opiate antagonists, and kappa agonists, as well as drugs involved with nerve transmission such as gabapentin and pregabalin, may be useful in some patients not responding to conventional treatment.
What is itch?
Itch is a symptom rather than a disease. The only tissues from which itch can be evoked are skin, mucous membranes, and cornea. It is a primary symptom in a diverse range of skin diseases and also occurs in various systemic diseases.Skin diseases that commonly cause itch include:
Dry skinInsect bite reactions
Contact dermatitis
Atopic eczema
Psoriasis
Seborrhoeic dermatitis
Scabies
Urticaria
Lichen planus
Scars
Superficial fungal diseases
Lichen simplex chronicus.
Systemic diseases that cause itch include:
Chronic renal diseaseCholestasis
Hyperthyroidism
Haematological disease and lymphoreticular malignancy
Hodgkin's disease
Polycythemia vera
Myeloid and lymphatic leukaemia
Myelodysplasia
Systemic mastocytosis
Solid malignant tumours (paraneoplastic manifestation)
HIV infection
Aquagenic pruritus
Dermatomyositis
Scleroderma
Drugs (such as opioids, chloroquine, allopurinol)
Hydroxyethyl starch.
Psychogenic itch is seen in the delusional state of:
Parasitophobia
Obsessive-compulsive disorder
Depression.
It is also seen in patients with anorexia nervosa.
Neuropathic itch that is associated with itch includes peripeheral neuropathy:Postherpetic neuropathy
Nerve entrapment including brachioradial pruritus.
Diabetes.
Neuropathic itch has been associated with demyelinating disorders such as:
Multiple sclerosis
Brain tumours
Cerebrovascular events.
Epidemiology
Itch has been found to be a common skin complaint in all age groups. Among adults in Norway the prevalence of pruritus was found to be about 8%. Itch has a higher prevalence in people older than 65. At least 50% of people aged 70 or older will have prolonged bouts of troublesome pruritus. Idiopathic itch in older people is common and presents a diagnostic and therapeutic challenge.Definitions
Several definitions are important when discussing itch.Chronic pruritus
Chronic pruritus is an itch that lasts more than six weeks. Chronic itch may continue when treatment stops depending on the origin and state of the symptom. It has a significant impact on quality of life. It can totally destroy a patient's social life and lead to suicide in severe cases (as with patients who have chronic pain).
Because chronic pruritus is unrelenting, it is likely that stress, affective factors, and environmental factors such as heat and dryness may be superimposed on the original damaged tissue and contribute to the intensity and persistence of pruritus.
Intractable pruritus
Another form of itch in chronic sufferers is intractable pruritus. Intractable pruritus is defined as a chronic itch state in which the cause cannot be removed or otherwise treated and in the generally accepted course of medical practice no relief or cure of the cause of itch has been found after reasonable efforts.You should refer affected patients to a specialist. It is important to acknowledge that such patients are encountered weekly in dermatology clinics and they do suffer. They need a more holistic approach by an interdisciplinary team, with involvement of patients and their families. Treatment integrates pharmacological and non-pharmacological approaches.
Clinical features
If a patient scatches a lot, secondary skin lesions develop. Secondary skin lesions induced by scratching include:Excoriations
Lichenification
Prurigo nodules
Hyperpigmentation (or hypopigmentation in dark skin)
Bruising.
Excoriations
Excoriations result from erosion of the skin by mechanical means, which appears in the form of a scratch or abrasion (Figure 1).Figure 1 Excoriations in a patient with atopic eczema
Lichenification (lichen simplex)
Lichen simplex is a well developed thickened plaque with marked accentuation of the skin creases that develops due to continuous rubbing and scratching (Figure 2). Postinflammatory hyper- or hypopigmentation can happen. The common distribution of lichenified plaques is in areas where the patient can easily scratch and rub (the nape of the neck, below the elbow and the ankle, buttock and genitalia).Figure 2. Lichenified plaques in a patient with localised itch with stasis dermatitis
Prurigo nodulesPrurigo nodules are excoriated papules that in chronic pruritus lead to nodule formation (Figure 3). These are usually distributed on the extensor side of the limbs and upper back. Prurigo nodules are frequently associated with emotional stress and obsessive-compulsive disorder, but they can be also be a manifestation of itch in patients with chronic renal failure.
Figure 3. Prurigo nodules
Shiny finger nailsThe finger nails may be shiny because of prolonged rubbing (Figure 4).
Figure 4. Shiny nails due to repetitive scratching
The butterfly sign
The middle of the back that cannot be reached may show normal skin or relative hypopigmentation, in contrast to the hyperpigmentation of the areas subjected to persistent scratching. This results in a butterfly pattern.Diagnosis
It is important to take a detailed history. You should find out whether the patient has generalised or localised itch. Localised itch may be associated with a circumscribed compression of neuronal structures by local diseases (for example genitoanal pruritus in prostate cancer). Localised itch associated with burning could be associated with neuropathy, such as damage to cervical nerves in brachioradial pruritus.A careful history also includes a full allergy and drug history because drugs such as opiates, aspirin, penicillin, and antimalarials can induce itch. A simple question, such as whether pruritus occurs in other family members, can indicate the possibility of scabies and prevent unnecessary investigation. A positive review of systems, especially in relation to general health, such as weight loss, night sweats, and tremor, could point to a systemic cause.
The most important points you should find out from a patient with pruritus are:
Duration - years, weeks, daysLocalisation - generalised, localised, where
Severity
Effect on sleep
History of itch in other personal contacts
Characterisation - burning, pricking, formication
Periodicity - paroxysmal, continuous, occuring in short bouts, nocturnal
Factors that exacerbate itch - heat, water, dryness
Factors that alleviate itch - drugs or cooling agents
Drugs - opiates, aspirin, penicillin, antimalarials
History of atopy
Travel history.
Examination
You should undertake a thorough physical examination with particular attention to:
Lymph nodes (lymphoreticular malignancy)
Organomegaly of the liver and spleen (lymphoreticular malignancy and paraneoplastic manifestion)
Fine tremor (hyperthyroidism)
Signs of jaundice and anaemia
The genital area, finger webs, the ulnar border of palms, wrists, elbows, axilla, and nipples (typical for scabies).
Some pruritic states have specific clinical patterns. Despite severe pruritus, chronic urticaria usually does not show secondary skin lesions associated with scratching. Neuropathic itch in disease entities such as postherpetic neuralgia and brachioradial pruritus involves itch in the relevant nerve distributions.
Investigations
Most patients with pruritus with rash will not need further tests. A detailed history and examination will reveal the cause.Investigations for patients with pruritus on the skin with a rash include a skin biopsy and laboratory investigation. Patients with itch on primarily normal, non-inflamed skin may need laboratory and radiological tests, adapted to the patient's history and pre-existing diseases.
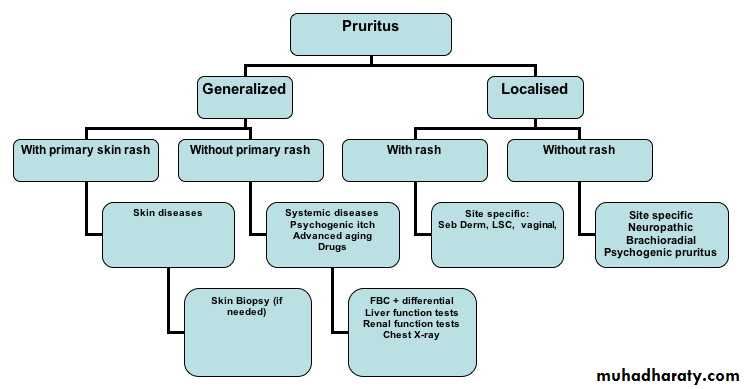
FBC = full blood count; LSC = lichen simplex chronicus; Seb Derm = seborrhoeic dermatitis.
Figure 6 is an algorithm for diagnosing and investigating a patient with itch.
TreatmentThere are no specific antipruritic drugs with a general purpose. Treating pruritus depends on identifying and removing the cause, whether systemic or cutaneous.
If it isn't possible to treat the cause there are several preventive and therapeutic treatment options. These include:
Emollients and moisturisers
Barrier creams
Colloidal oatmeal, sodium bicarbonate, and tar baths
Mild low pH cleansers
Corticosteroids (topical and oral)
Immunomodulators (topical and systemic)
Antihistamines (topical and oral)
Coolants and counterirritants
Capsaicin
Topical anaesthetics (EMLA)
Lauromacrogols
Topical salicylates
Topical N-palmitoylethanolamine, a low potency cannabinoid agonist
Opiate antagonists and agonistsSelective serotonin reuptake inhibitors
Gabapentin
Pregabalin
Thalidomide
Phototherapy
Complementary medicine eg acupuncture
Behavioural therapy.
Preventive measures to reduce itch
Commonly used topical treatments include emollients and moisturisers, which restore and preserve the barrier function of skin. Emollients and barrier repair creams are not specific treatments for itch but often reduce pruritus through improved barrier function. Barrier creams help the stratum corneum to retain water. They are often effective treatments for itch associated with dry skin and atopic dermatitis.Acidifying the stratum corneum may also reduce itch. High pH solutions and soaps damage the skin barrier function.
Acidic pH solutions are less damaging.
The sensation of itching is heightened if the skin is warm. Patients should therefore take measures to cool the skin, including having tepid showers, wearing light clothes, and using air conditioning where appropriate. Cooling lotions, such as calamine lotion or menthol, up to 3%, may help.
Other preventive measures to reduce itch you should recommend to your patients include:
Bathe in lukewarm water rather than hot water or cold water (hot and cold water can dry the skin)Restrict time in the shower or bath
Apply moisturiser immediately after bathing
Use a humidifier at home, especially in winter.
Wear light and loose clothing that absorbs sweat
Avoid wearing wool or tight clothingAvoid cleansers containing alcohol
Use coolants such calamine lotion or menthol 3%
Avoid rapid changes in environmental humidity
Avoid hot or spicy foods
Avoid alcohol.
Which topical treatments are effective?
A topical approach to relieving itch is particularly helpful for pruritus resulting from skin inflammation and damage to the stratum corneum. Although capable of relieving pruritus due to inflammatory skin disease, corticosteroids are not intrinsically antipruritic.Antihistamines are antipruritic only if the pruritus is caused by histamine, as in urticaria or insect bite reactions.
There are many topical formulations for pruritus, although most have not been subjected to controlled trials. The most common ones are:
Creams
Lotions
Ointments
Gels.
Topical steroids
Topical steroids provide relief of itching associated with inflammatory skin diseases such as contact dermatitis and atopic dermatitis. They come in different strengths from mild to potent. You should not use topical corticosteroids to treat generalised chronic itch without rash.Combinations of topical steroids and emollients, as well as keratolytics, are particularly effective for treating atopic eczema. As you move up the strength of the agent, there is a greater chance it will work, but there is also a greater risk of side effects such as skin atrophy, bruising, telangiectasia and stretch marks.
Topical immunomodulators
Topical immunomodulators that inhibit T lymphocyte activation, such as tacrolimus and pimecrolimus, are used primarily for atopic dermatitis of mild to moderate severity. But these medications are promising antipruritic treatments in other inflammatory pruritic diseases, such as:Contact dermatitis
Lichen planus.
Facial seborrhoeic dermatitis.
A good response has been achieved in diseases involving genitoanal pruritus, such as:
Lichen sclerosus et atrophicans
Genital psoriasis
Scrotal eczema
Genitoanal pruritus of undetermined origin.
Common side effects of these agents are burning and stinging sensations
Topical antihistamines
Commonly used for insect bite reactions and localised itch, but are not effective for chronic itch.
Doxepin, which is a tricyclic antidepressant with potent H1 and H2 antihistamine and atropine-like (anticholinergic) properties, is the most effective treatment. It has been shown to relieve pruritus in patients with:
Atopic dermatitis
Localised itch.
It is available as a 5% cream. It is not suitable for children. Percutaneous absorption of doxepin causing drowsiness, occurs in about 25% of patients, and limits its usefulness. Allergic contact dermatitis and skin burning sensations are other relatively common side effects.
Coolants and counterirritants
Menthol, camphor, and phenol stimulate the nerve fibres that transmit the sensation of cold, thereby masking the itching sensation. They have been used for centuries. These agents could be compounded with aqueous cream to make a 1% to 2% cream. Menthol 1% to 3% cream is popular with patients who have pruritic skin; higher concentrations can induce skin irritation. All these compounds can cause skin irritation.13Capsaicin
Topical capsaicin, the active compound in the chili pepper, causes release of neuropeptides (including substance P) from C fibres and induces desensitisation of C fibres with long term use. Unfortunately, concordance is poor because initial application causes an intense transient burning sensation at application sites. This usually resolves after a few days or by applying a topical anaesthetic.Topical anaesthetics
Topical anaesthetics, including pramoxine 1% cream and a eutectic mixture of lidocaine and prilocaine 2.5% cream (EMLA), have a documented antipruritic effect, as does lidocaine 3% in an acid mantle cream and lotion. Topical anaesthetics have been used effectively in neuropathic itch, such as postherpetic neuralgia and brachioradial pruritus.Polidocanol is a non-ionic surfactant with both local anaesthetic properties and moisturising effects. It was found to significantly reduce pruritus in patients with:
Atopic dermatitis
Contact dermatitis
Topical salicylates
Topical acetylsalicylic acid significantly reduces itch in patients with lichen simplex chronicus.17 Topical salicylic acid solutions are keratolytic and may also increase hydration and soften the stratum corneum by decreasing its pH. Don't apply topical salicylates in acute inflammatory skin processes and in young children.Topical low potency cannabinoid agonist (N-palmitoylethanolamine)
Recent evidence of cannabinoid receptors on cutaneous nerve fibres supports the use of cannabinoid receptor agonists as topical antipruritics. Activation of these receptors by a topical cannabinoid agonist could significantly suppress pain as well as itch sensation and erythema. A cream with the cannabinoid agonist palmitoylethamolamine showed promising results in pilot trials of pruritus in18:
Atopic dermatitis
Uraemic pruritus
Prurigo nodularis.
Other topical measures that may reduce generalised itch associated with inflammatory skin diseases
Wet wrap occlusive dressings with a moisturiser and a mild potency topical corticosteroid applied for one week (wet pyjama treatment) have shown an excellent antipruritic effect in severe generalised atopic eczema.19 Bathing agents such as colloidal oatmeal baths, sodium bicarbonate baths, and tar baths can also reduce the sensation of itch. Mild low pH cleansers and moisturisers have a soothing effect on itch.
Oral antihistamines
First generation H1 antihistamines have marked sedative and anticholinergic actions.Second generation (low sedation) antihistamines have lower lipophilicity and consequently are associated with less drowsiness and other unwanted side effects.
Sedative (first generation) useful in severe chronic urticaria with or without angioedema because they suppress pruritus and alleviate associated anxiety. Hydroxyzine 25-50 mg is especially valuable in this context. These medications should be taken at bed time.
Second generation antihistamines such as loratadine, desloratadine, and cetirizine are suitable in the daytime for relief of pruritus due to urticaria. The role of these non-sedating antihistamines is limited in other pruritic disorders.
Opiate antagonists and agonists
µ-opioid antagonists, such as naloxone and naltrexone, have been used for treating pruritus associated with:• Cholestasis
• Chronic renal failure
• Lymphoproliferative disease
• Dermatological diseases such as atopic dermatitis.
Naltrexone is effective for treating some patients with severe, intractable pruritus. However, such µ-antagonists are associated with significant side effects including nausea and vomiting, hepatotoxicity, difficulty sleeping, and reversal of analgesia.
Butorphanol is a commercially available opioid agonist-antagonist analgesic with both kappa-agonist activity and µ-antagonist activity. Previous studies have found that epidural butorphanol was effective in relieving pruritus associated with epidural morphine. It has been used to treat pruritus of chronic renal failure, cholestasis, lymphoma, and idiopathic generalised pruritus based on non-controlled case series and our personal experience.
Intranasal butorphanol is an effective treatment for many patients with chronic, severe, and intractable pruritus due to systemic diseases and inflammatory skin diseases.
Nalfurafine hydrocholoride is a kappa opioid that has been launched in Japan for the treatment of pruritus of chronic renal failure.
Selective serotonin reuptake inhibitors
The oral antidepressant mirtazapine has been shown to relieve itch in some patients. Mirtazapine is a central presynaptic alpha-2 noradrenergic inhibitor and specific serotonergic antidepressant. It has been shown to be effective in a low dose of 15 mg at night when used to treat24 25:Systemic pruritus
Pruritus of skin inflammations
Nocturnal itch.
In case reports the selective serotonin reuptake inhibitor paroxetine was demonstrated to influence severe pruritus due to:
Polycythemia vera
Paraneoplastic pruritus
Psychogenic itch.
Other selective serotonin reuptake inhibitors do not appear to reduce itch.
Gabapentin/pregabalin
Studies have shown that gabapentin is effective for treating itch, particularly:Uraemic itch
Brachioradial pruritus
Itch induced by multiple sclerosis
Other types of neuropathic itch.
Pregabalin is a new neuropathic pain medication that has a similar structure and function to gabapentin with fewer side effects and can reduce neuropathic itch or alter the sensation of itch in systemic diseases.
Another drug that has effect on inhibition of itch via its effect on nerve fibres is thalidomide, it has been shown to be effective for prurigo nodularis and severe itch related to HIV, but due to high costs and side effects is rarely used. It is absolutely contraindicated in pregnancy.
Systemic immunomodulators such as azathioprine and cyclosporine and the new biologics such as anti-tumour necrosis factor have recently been shown to reduce itch in inflammatory skin disease such as atopic eczema and psoriasis.
Neurokinin 1 inhibitors - a novel therapy
Recent reports suggest that an NK-1 antagonist aprepitant, an antiemetic given to cancer patients, exhibits antipruritic effects for generalised pruritus and itch associated with lymphoma. Substance P as mentioned above has a role in itch and is known to activate the neurokinin receptor. A major drawback is the high cost of this medication.Phototherapy
Phototherapy has been used for more than a decade to treat different types of itch. Different wavelengths of phototherapy and techniques include UVB, UVA, combined UVA/UVB, long-narrow band UVB, and photochemotherapy with psoralens (PUVA) applied systemically or topically or as a bath.Phototherapy is beneficial for itch associated with:
Atopic dermatitisPsoriasis
Chronic renal failure.
Remissions may last for as long as 18 months. Recent reports have suggested that narrow band UVB may be as effective for treating pruritus as broad band UVB or PUVA.
Behavioural therapy
In recent years it has become increasingly clear that stress and other psychogenic factors are important in itch. Several studies have shown that behavioural modification therapy reduces the intensity and perception of itch. Other possible behavioural interventions include stress reduction and biofeedback. These treatments are especially effective for treating chronic pruritus associated with psychogenic cofactors.Complementary medicine
Patients with chronic itch seek complementary medicine in a similar way that chronic pain patients do. Recent studies suggest that acupuncture has a role in itch reduction in atopic eczema.Specific treatment recommendations
Table 1 outlines some more information on itch associated with specific cutaneous and systemic conditions and their treatment. The level of evidence in many treatments is based on case series and non-controlled studies and reflects expert opinion.
Level of evidence in parenthesis is marked as:
A for double blind studiesB for clinical trials containing 20 or more patients
C for clinical studies with fewer than 20 patients, case series, and expert opinion.
Table 1. Treatment recommendations for itch associated with specific conditions
DiagnosisTreatment recommendation
Comment
Pruritus in atopic eczema
Emollients and moisturisers (B)Colloidal oatmeal (B)Polidocanol and topical salicylatesTopical corticosteroids (A)Topical immunomodulators (A)
Whether itch in patients with atopic eczema precedes skin lesions or vice versa is an unresolved issue. What is certain is that a vicious itch-scratch cycle exists in atopic patients, in which scratch damage enhances pruritus.
Pruritus in moderate to severe atopic eczema
Oral sedating antihistamines (C)Sodium bicarbonate and tar baths (C)Phototherapy (A)Pruritus in severe atopic eczema
Double layer wet pyjama++ (B)Oral immunomodulators +++ (A)Selective serotonin reuptake inhibitors(B)Opiate antagonists (B)
Pruritus in psoriasis
Topical corticosteroidsTopical tar (A)Salicylic acidPhototherapy for severe itch (A)Selective serotonin reuptake inhibitors may be indicated (C)Biologics ; anti TNF (A)
Itch in patients with psoriasis is a significant but under-recognised problem. Several studies have demonstrated that itch is a principal symptom of psoriasis. Among patients with psoriasis, 77% experience pruritus daily.33
Pruritus due to end stage renal disease
Phototherapy (B)Low dose gabapentin after dialysis (A)Nalfurafine (kappa agonist) (A)* Butorphanol* Currently only approved in JapanOne of the most distressing symptoms of chronic renal failure. It affects 20-60% of patients with chronic renal disease, especially those on dialysis. Scratching is common and patients may be heavily excoriated or the skin may appear lichenified or present with prurigo nodules. It has a significant impact on sleep and quality of life.34 35
Pruritus in haematological disease and lymphoreticular malignancy
Selective serotonin reuptake inhibitors (B)Butorphanol (C)Phototherapy (B) Aprepitant (C)Itch is common in haematological disorders. In widespread cutaneous T cell lymphoma (CTCL) and erythrodermic forms of CTCL, including Sézary syndrome (T cell leukaemia), itch is often severe and difficult to manage. In polycythemia vera, it occurs in about 50% of patients, is often precipitated by contact with water ("bath itch"), and is associated with raised blood histamine levels.
Drug induced pruritus
Oral antihistamines and oral corticosteroids, if stopping the drug is not possible (C)Pruritus can be a side effect of a wide variety of medications. These include:
Opiates
Oral aspirin
Antibiotics such as penicillin
Antimalarial drugs such as quinidine and chloroquine.
The plasma cell expander hydroxyethyl starch accumulates in skin cells including nerve fibres and causes intense itch. Drugs that can cause cholestasis can cause itch secondary to this.
Pruritus of endocrine disease
Hyperthyroid related itch: treatment of the underlying disease including beta blockers (C)For dry skin in hypothyroidism, use emollients (C)
Generalised intractable itching is a recognised feature of thyrotoxicosis and may be a presenting symptom. Hypothyroidism is less frequently associated with itch.
Pruritus of cholestasis
Opioid antagonists including naloxone and naltrexone (A)Kappa agonist butorphanol (C)Combination of bile salt lowering and opioid antagonist strategies (BHighly distressing and persistent. Often begins with an acral distribution, but later becomes more generalised. Patients with cholestatic pruritus have elevated plasma opioid levels in addition to elevated bile acids.
Pruritus in infectious disease
Treat the underlying infectionCauses include:
Scabies and mites
Viral infections such as rubella and varicella
Tropical and intestinal parasites such as trichinosis, onchocerciasis, and schistosomiasis.
Bacterial infections are rarely associated with itch except for cutaneous staphylococcal infections such as:
Folliculitis
Impetigo.
Fungal skin infections causing itch include dermatophytic infections and candidal skin infections.
Pruritus in HIV infection
Eosinophilic folliculitis: a combination of permethrin 5% and topical mid potency corticosteroids (C)For severe cases of HIV prurigo: thalidomide (C)Itch is an early symptom of HIV infection. It may be associated with skin disease (scabies, pediculosis, xerosis). It can be a result of systemic causes (hepatic disease, renal disease, lymphoma, adverse drug reaction, systemic and skin infection including Staphylococcus aureus and pityrosporum) or it occurs as a primary symptom of HIV.36 Eosinophilic folliculitis is an intensely pruritic eruption characteristically occurring in people with a CD4 count less than 300/µl.
Pruritus as a manifestation of solid malignant tumours
Selective serotonin reuptake inhibitors (B)Opiate antagonists and agonists and gabapentinNeurokinin 1 antagonists
Significantly less common in solid tumours than in lymphoproliferative disease.39 Although pruritus may occasionally be present years before the tumour becomes detectable, full investigation for a causative solid tumour is probably not worthwhile.
Pruritus associated with pregnancy
Topical corticosteroidsOral non-sedating antihistamines (B)Pruritus associated with pregnancy can be caused by primary skin rash such as polymorphic eruption of pregnancy or intrahepatic cholestasis.
Postherpetic neuralgia
Gabapentin and pregabalinTopical capsaicinTopical anaesthetics (C)(All controlled studies assessed pain as an end point but not itch)
Data suggest that pruritus commonly accompanies acute zoster and postherpetic neuralgia, particularly lesions affecting the head, face, and neck.40
Psychogenic itch
Psychogenic itch: antipsychotics and psychological therapies, if acceptedPatients with depression, fibromyalgia, and other somatoform disorders: selective serotonin reuptake inhibitors,40 gabapentin, or pregabalin (C)Delusions of parasitosis is one of the more challenging types of itch. The patient often brings "evidence" in the form of collected fragments, although on examination the material proves to be non-specific debris. The patient holds a false belief that they are infested with parasites. The patients often refuse to see a psychiatrist.Patients with depression, fibromyalgia, and other somatoform disorders can have severe itch.
Pruritus associated with burns and scars
Intralesional injections of corticosteroids (B)
Burn scars are associated with significant pruritus. Keloids are frequently associated with itch at the periphery of the lesion.
Complications
Patients with chronic pruritus often have:Difficulty sleeping
Difficulty concentrating
Decreased sexual desire and sexual function
Agitation
Depression.
Also, eczematous lesions resulting from scratching can become infected, particularly in patients with atopic dermatitis.
a : Penicillin
Pencillin can cause itch with rash.
b : Thiazides
Thiazides can cause itch with rash.
c : Sulphonylurea
Sulphonylurea can cause itch with rash.
d : Morphine
This is the most common of these drugs to cause itch without rash.
e : Azathioprine
Azathioprine does not cause itch, in fact it is an effective treatment for itch caused by atopic eczema.
Itch in patients with psoriasis is a significant but under-recognised problem. Several studies have demonstrated that itch is a principal symptom of psoriasis. Among patients with psoriasis, 77% experience pruritus daily.
Wet pyjama treatment effectively reduces the itch and erythema.
Which one of the following statements about the antidepressant mirtazapine is correct?It has beneficial effects in patients with malignant cholestasis, lymphoma, uraemia, and inflammatory skin disease (severe atopic eczema and chronic neurotic excoriations). It has been reported to be particularly beneficial for nocturnal pruritus.