Stroke: a guide to diagnosis and assessment
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
Definitions
According to the WHO, a stroke is characterised by:Rapidly evolving symptoms and/or signs of focal loss of central nervous system function - the loss is rarely global Symptoms lasting for more than 24 hours or leading to death.No apparent cause other than a vascular origin.
A transient ischaemic attack presents in the same way as a stroke, but symptoms resolve within 24 hours. In clinical practice, symptoms of a transient ischaemic attack usually tend to resolve within one hour. The processes causing ischaemic stroke and transient ischaemic attack are the same.
The importance of a transient ischaemic attack is that it is a temporary, non-disabling manifestation of cerebrovascular disease, which may progress to a more disabling event. You need to investigate a patient who has had a transient ischaemic attack urgently and start secondary prevention.
Key points
Cerebral infarction causes 85% of strokes; cerebral haemorrhage causes 15%.It is important that you differentiate between these causes, as they are managed differently
Investigations are done to:
Confirm (or refute) the diagnosis of a stroke
Differentiate infarction from haemorrhage
Find out the underlying cause and help prevent recurrent events
Clinical tips
Stroke is an emergency and you should see patients quickly. This applies both to acute treatment and to secondary prevention
Thrombolysis is only licensed for use within three hours of onset
The risk of recurrence is highest in the first few days
In patients with a possible stroke, always check the blood glucose with a capillary prick. Hypoglycaemia may also cause focal (as well as global) neurological symptoms
Learning bite
The following symptoms are common in patients with stroke. They are often confused with each other:Dysphasia: The patient has problems with speech processing and production (remember dysphasia with s for speech)
Dysarthria: The patient has slurred speech. The problem is with articulation rather than speech processing (remember dysarthria ~ articulation).
Dysphagia: The patient has difficulty swallowing (remember g for gullet).
How common is stroke?
Stroke is the third most common cause of death in the UK. The annual incidence is about 200 per 100 000 people, which means that every year about 110 000 people in England and Wales and 15 000 people in Scotland will have a first stroke.Morbidity and mortality
Ten to twenty percent of strokes are fatal. For the survivors, stroke results in many long term problems. These include:• Chronic physical disability
• Dementia
• Depression
• Epilepsy
• Falls.
Stroke is the most common cause of neurological disability in the UK - a third of patients remain disabled. It makes stroke a costly problem - it accounts for up to 6% of all NHS resources.
The different types of stroke
Stroke has a number of different subtypes. You should be aware of these, as their management is different.
There are two main types of stroke:
About 85% of strokes are ischaemic in origin
Fifteen per cent are due to haemorrhage. These can be subdivided into
Intracerebral haemorrhages - about 12-13%
Subarachnoid haemorrhages - about 2-3%.
There are several further ways to classify subtypes of ischaemic stroke. The commonly used Oxfordshire Community Stroke Project(OCSP) classification is the most validated tool for the classification of stroke. It divides stroke subtypes into:
• TACI - Total anterior circulation infarct
• PACI - Partial anterior circulation infarct
• LACI - Lacunar infarct
• POCI - Posterior circulation infarct.
This classification is based on the clinical deficit a patient presents with, and it classifies strokes according to which vascular territory is affected: anterior or posterior circulation, with a lacunar syndrome suggesting small vessel disease. The OCSP classification also provides some prognostic information, with the prognosis being worst in patients with a total anterior circulation infarct and best in patients with a lacunar infarct
(TACI) includes all of:
• Higher dysfunction (dysphasia, visuospatial neglect)• Motor and/or sensory deficit
• Homonymous hemianopia
(PACI) includes:
• Two of the three criteria for a TACI or
• Higher dysfunction alone or
• A limited motor or sensory deficit
(LACI) includes :
Any of:
Pure motor deficit (affecting face, arm, and leg)
Pure sensory deficit (affecting face, arm, and leg)
Sensori-motor deficit (affecting face, arm, and leg)
Ataxic hemiparesis
None of:
Higher dysfunction (dysphasia, visuospatial neglect)
Isolated proprioceptive loss
Features of a posterior circulation infarct
(POCI) includes any of:
Cranial nerve palsy and contralateral motor/sensory deficitBilateral motor and/or sensory deficit
Conjugate eye movement disorder
Cerebellar dysfunction without ipsilateral long tract signs
Isolated homonymous hemianopia
Higher dysfunction alone
A limited motor or sensory deficit
The classification of causes of intracerebral haemorrhage is less standardised.
Common causes of intracerebral haemorrhage include:Hypertensive haemorrhage - usually located in the basal ganglia
Haemorrhage due to amyloid angiopathy. Cerebral amyloid angiopathy is a condition characterised by amyloid deposition in cerebral vessels. This causes the vessel walls to become fragile and vessels to rupture. Haemorrhages due to amyloid angiopathy are often lobar haemorrhages.
Less common causes of intracerebral haemorrhage include:
Arteriovenous malformations
Tumours
Coagulation disorders - for example, if the patient is over anticoagulated.
There are no reliable clinical methods to differentiate between cerebral infarction and cerebral haemorrhage. This can only be done with brain imaging.
Diagnosis of stroke
HistoryWhen taking the history, you should ask the following:
How did the symptoms start?
A sudden onset over seconds to minutes supports a vascular cause. Gradually evolving over weeks or months suggest another cause, such as a tumour.
What symptoms did the patient have? Are the symptoms in keeping with a focal neurological deficit?
Loss of consciousness is rare.
Unilateral weakness
Speech disturbance
Hemianopia - loss of vision in one half of the visual field
Sensory loss.
Learning bite
Amaurosis fugax is transient visual loss in one eye only due to retinal ischaemia. The central retinal artery comes off the internal carotid artery and may be transiently occluded by an embolus.Patients often describe a "shutter" coming down over their eye, resolving after five to 10 minutes.
Does the patient have any vascular risk factors?
HypertensionDiabetes
Hypercholesterolaemia
Previous strokes or transient ischaemic attacks
Ischaemic heart disease
Peripheral vascular disease
Smoking history
Family history of vascular disease
Social history (this is important in deciding longer term rehabilitation and placement. For example, will a younger patient be able to go back to work? Will access to the home be a problem?)
Examination
make sure that airway, breathing, pulse, and blood pressure are stable.
General examination - this may provide information regarding possible risk factors and potential complications.Pulse - atrial fibrillation is a risk factor for cardioembolic stroke.Blood pressure - this is often elevated due to loss of cerebral autoregulation
Heart murmurs - valvular disease may be a source of cardiac emboli.Neck bruits - these may indicate a stenosed carotid artery. A bruit is not definite proof of a stenosis, nor is absence of a bruit a sign that there is no stenosis.
The neurological examination
The Oxfordshire Community Stroke Project classification provides some guidance on the association between the location of the infarct and specific clinical syndromes. For example:A patient presenting with a right hemiparesis, right sided sensory loss, a right hemianopia, and dysphasia has a left hemispheric "total anterior circulation syndrome." This is usually due to occlusion of the left middle cerebral artery, causing infarction of large parts of the left frontal, parietal, and temporal lobe
A stroke causing isolated homonymous hemianopia is most likely due to a contralateral posterior cerebral artery infarct affecting the occipital cortex.
Anterior cerebral artery infarcts typically present with contralateral leg weakness.
Tips on how to localise an infarctIn a lacunar stroke, weakness typically affects the face, arm, and leg equally.
An infarct affecting the motor cortex typically causes weakness that affects the face, arm, and leg to a different extent –
middle cerebral artery infarct, the face and arm are usually much weaker than the leg.
Anterior cerebral artery infarcts typically present with contralateral leg weakness.
If you think a patient with a left sided weakness is dysphasic, ask if the patient is left handed. In the vast majority of right handed people (and also in a large number of left handed people) speech control is located in the left hemisphere, that is, a stroke causing dysphasia would usually be associated with a right sided weakness. Impaired speech in a patient with a left hemiparesis is probably not dysphasia, unless the patient is left handed or has multiple lesions.Differential diagnosis
Four important differential diagnoses to consider are:
• Migraine with aura
• Focal epilepsy
• Brain tumour
• Hypoglycaemia.
Migraine with aura
The onset of symptoms is usually more gradual, and the patient often has a march of symptoms, for example, tingling starting in the hand and slowly wandering up the arm over several minutes. The visual disturbance in migraine tends to be positive, that is, rather than visual loss the patient experiences flashing lights or zigzag lines.Some patients can develop limb weakness in hemiplegic migraine. This can exactly mimic stroke weakness.
A migrainous aura is often followed by a throbbing headache, nausea, and photophobia.
The diagnosis is difficult if there is no headache and the patient has no history of migraine. If you cannot tell the difference with certainty, it is probably wise to err on the side of caution and treat for transient ischaemic attack or stroke, as missing this has potentially serious consequences.
Focal epilepsy
The patient will usually have several stereotyped episodes - where each seizure is typically the same. Symptoms are usually positive, for example, arm jerking rather than weakness. But beware of Todd's palsy after a focal seizure. If the symptoms are new, you should request a scan to look for an underlying structural lesion. The most common cause of epilepsy in elderly people is cerebrovascular disease, so the two may coexist.Brain tumour
The onset of symptoms is usually much more gradual, occurring over weeks or months. Haemorrhage into a tumour may produce sudden symptoms.Hypoglycaemia
Hypoglycaemia can present as a focal neurological deficit. Always check a patient's blood glucose in suspected stroke, and treat it if the patient is hypoglycaemic.
Investigations
Investigations in patients with stroke serve two purposes:
To confirm the diagnosis of a stroke and to refute other diagnoses
To determine the cause.
Investigations to confirm the diagnosis: brain imaging
If the patient has had a stroke, brain imaging should differentiate between a cerebral infarct and a haemorrhage, and show which part of the brain has been affected.CT brain
Most widely used method, as it is widely available and scanning times are relatively short. A disadvantage of CT is the poor resolution it has for structures in the posterior fossa, which are often obscured by artefact from the surrounding bones. Furthermore, it takes at least a few hours for a cerebral infarct to become easily visible on CT. Changes of early infarction on CT may be present but detecting these requires experience and training.
Early infarction (generally less than six hours after onset) - the CT changes are difficult to detect for the untrained eye. They include (Figure 1a):
Loss of grey/white matter differentiation
Loss of definition of the basal ganglia
Loss of sulcal pattern.
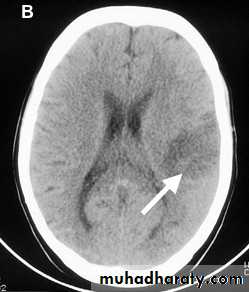
Established infarction (days to weeks after onset) (Figure 1b) - the CT changes are more obvious:
The infarcted area looks dark - the older the darker
Cortical infarcts are typically wedge shaped
Lacunar infarcts look like small black holes. They measure less than 1 cm in diameter and are located subcortically, usually in the basal ganglia or internal capsule.
Figure 1a: Early right frontal infarct. Some loss of sulcal pattern on the right compared with the left.
Figure 1b: Established infarct (some days old) in the left middle cerebral artery territory.
• Cerebral haemorrhage in the acute stage will show up as white. Small haemorrhages may resolve quickly and, even within a few days, they may look similar to infarction. (Figure 1c).
• Figure 1c: Intracerebral haemorrhage in the right hemisphere (solid arrow) with some blood in the right lateral ventricle (broken arrow.)
•
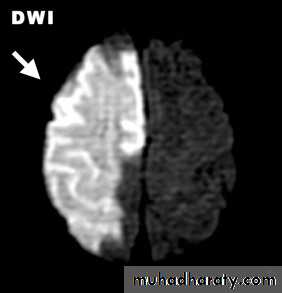
Magnetic resonance imaging
allows more detailed imaging of the brain than CT, in particular, of the posterior fossa structures. Its main limitation is that it is not yet as widely available as CT and that scanning times are longer.also offers scanning sequences that are particularly helpful in stroke. Diffusion weighted imaging shows the brain territory affected by acute ischaemia, very early after the event - even within minutes of the onset of symptoms (Figure 2). This can be helpful when deciding whether to give thrombolysis. As diffusion weighted imaging only shows recent infarcts, it is easier to differentiate new from old infarction, which may be harder to do on CT or standard magnetic resonance imaging.
Figure 2: Diffusion weighted MRI showing acute right middle cerebral artery infarction.
Investigations to determine the cause of the stroke
By finding the cause of a TIA or stroke, you will be able to determine the risk of recurrence. By treating the underlying cause you may be able to reduce that risk. The main investigations are:Vascular imaging to identify vessel stenoses or other vascular pathologies, such as dissection or vasculitis.
Cardiac investigations to identify potential sources of cardiac embolism.
Vascular imaging
Doppler ultrasoundDoppler ultrasound is the least invasive and usually the most readily available method for imaging vessels. Its main disadvantage is that its routine use is generally restricted to the cervical part of the carotid arteries. It is difficult to show the vertebral arteries in detail, and it is not possible to show arterial dissection reliably.
CT angiography and MR angiography
With these methods, it is possible to image the entire vascular tree from the aortic arch upwards, including intracranial vessels. The disadvantages of CT angiography, and to a certain extent also MR angiography, are that they:• Require the administration of contrast media
• Are prone to movement artefact.
• For CT angiography, there is considerable radiation exposure
Intra-arterial angiography
Intra-arterial contrast angiography is the most invasive method for vascular imaging. It carries about a 1% risk of causing a stroke. Its use is restricted to the investigation of more unusual causes of strokes, such as possible vasculitis.Cardiac investigations
ECGThe ECG will help you identify any rhythm disturbances. If a 12 lead ECG is normal and you suspect an underlying arrhythmia, such as paroxysmal atrial fibrillation, you should request a 24 hour ECG.
Echocardiography
You should arrange echocardiography to identify structural lesions which could cause emboli. This is done routinely in many countries, but in the UK, its use tends to be limited to patients in whom there is a suspicion of an underlying cardioembolic source. For example, in patients with:
• An embolic infarct pattern on brain imaging - multiple infarcts in different vascular territories
• A cardiac murmur
• A history of previous cardiac disease
• No obvious vascular risk factors - these are usually young patients.
You should arrange for transthoracic echocardiography first. If this is normal or unsatisfactory, you may need to request transoesophageal echocardiography. This is more invasive, but provides clearer images of the heart, in particular of the left atrium.
Potential structural causes of cardiac embolism include:
• Intracardiac thrombus
• Left ventricular aneurysm with thrombus
• Atrial myxoma
• Bacterial endocarditis
• Valvular lesions
• Patent foramen ovale - (this is controversial).
• Other investigations
• Blood tests will help identify risk factors for stroke. You should check the following blood tests in most patients.• Full blood count - to detect anaemia, polycythaemia, thrombocythaemia, or thrombocytopenia.
• Coagulation - to look for increased bleeding tendency, in particular in cerebral haemorrhage.
• Glucose - always check the blood glucose when a patient presents with an acute neurological deficit, as hypoglycaemia can mimic a stroke. It is also important to diagnose diabetes mellitus where present.
Cholesterol
to identify hypercholesterolaemia.
Urea and electrolytes
look for hyponatraemia which may cause a neurological deficit.
Erythrocyte sedimentation rate
C reactive protein
to screen for an underlying inflammatory disease, but these tests are non specific.
You should only check the following blood tests in selected patients.
Autoantibodies
Anti-nuclear factor, anti-nuclear cytoplasmic antibodies, anti-cardiolipin antibodies - to look for an underlying autoimmune disease, vasculitis, or anti-phospholipid syndrome.Thrombophilia screening
This is of doubtful value, as most thrombophilias increase the risk of venous thromboembolism, and most strokes are arterial in origin unless caused by paradoxical embolism. Some thrombophilic markers, for example, factor V Leiden, are common in the general population. You need to consider whether thrombophilia screening will be useful and whether it will change management in an individual patient.
Learning bite
Paradoxical embolism occurs when a venous embolus passes directly from the right atrium to the left atrium, thus avoiding being filtered out in the lung. From the left side of the heart it can then embolise into the systemic circulation and, for example, cause a stroke. A patent foramen ovale would allow the passage from the right to left atrium.Morning headache is not a typical feature of migraine with aura. Morning headache may indicate
1. increased intracranial pressure,
2. nocturnal carbon dioxide retention,3. or nocturnal hypoglycaemia.
A patient with hemiparesis, hemisensory loss, hemianopia, and dysphasia has a total anterior circulation infarct.
In a lacunar infarct the hemiparesis typically affects face, arm, and leg to an equal extent.
Cranial nerve palsies suggest a lesion in the brainstem and as such may form part of a posterior circulation infarct.
Todd's paresis or Todd's paralysis (or postictal paresis/paralysis, "after seizure") is focal weakness in a part of the body after a seizure. This weakness typically affects appendages and is localized to either the left or right side of the body. It usually subsides completely within 48 hours. Todd's paresis may also affect speech, eye position (gaze), or vision.
The condition is named after Robert Bentley Todd (1809-1860), an Irish-born London physiologist who first described the phenomenon in 1849.[1][2] It may occur in up to 13% of seizure cases.[3] It is most common after generalised tonic-clonic seizures ("grand mal") and may last for hours or occasionally days after the initial seizure. The generally postulated cause is the exhaustion of the primary motor cortex, although no conclusive evidence is available to support this.
The classic presentation of Todd's paresis is a transient weakness of a hand, arm, or leg after partial seizure activity within that limb. The weakness may range in severity from mild to complete paralysis.
When seizures affect areas other than the motor cortex, other transient neurological deficits can take place. These include sensory changes if the sensory cortex is involved by the seizure, visual field defects if the occipital lobe is involved, and aphasia if speech, comprehension or conducting fibres are involved.
Todd's paresis, as defined as any motor deficit after seizure, occurs in 13% of all seizures.[3] This was evaluated in a study of 513 patients with epilepsy with video-electroencephalography. The same study also showed that the mean duration of postictal paresis was 173 seconds, with ranges of 11 seconds to 22 minutes.[3] There have been case reports of longer durations of paresis, ranging to as long as days.[4]
Other post-ictal neurological findings that do not involve activity of the area affected by the seizure have been described. They are thought to be caused by a different mechanism than Todd's paresis, and including paralysis of the contralateral limb,[5] and rare genetic causes of hemiplegia and seizures.[6]
Todd's paresis is more common after any clonic seizure activity, and particularly if generalized tonic-clonic seizures occur.[3]
The cause of Todd's paresis is unknown but there are two hypotheses to its cause. The first is the depletion theory, where the motor cortex is exhausted leading to prolonged neuronal hyperpolarization. The second is that there is transient inactivation of motor fibres caused by activation of NMDA receptors. Neither has been extensively evaluated.
Treatment of Todd's paralysis is symptomatic and supportive because the paralysis disappears quickly. An occurrence of Todd's paralysis indicates that a seizure has occurred. The prognosis for the patient depends upon the effects of the seizure, not the occurrence of the paralysis.
Prognosis
Importance
The most significant issue regarding the Todd's paresis is its differentiation from a stroke. The issue is further complicated by the fact that some strokes trigger a focal seizure during the acute phase. A Todd's paresis in this context may overestimate the extent of neurological deficit due to the vascular process itself resulting in erroneous decisions with regards to acute stroke therapy such as thrombolysis. For this reason a seizure during an acute stroke is generally accepted to be a relative contraindication to thrombolytic therapy, especially in the absence of documented cerebrovascular occlusion using vascular imaging techniques.[7]
An infant with Todd's paresis does not necessarily preclude the diagnosis of a febrile convulsion. This view is as a result of a recent study that showed the incidence of Todd's paresis to be in 0.4% of infants that have been diagnosed with a febrile convulsion.[8]
• What is Todd's Paralysis?
• Todd's paralysis is a neurological condition characterised by a brief period of transient (temporary) paralysis following a seizure. The paralysis - which may be partial or complete - generally occurs on one side of the body and usually subsides completely within 48 hours. Todd's paralysis may also affect speech or vision. The cause is not known. Examination of an individual who is experiencing or who has just experienced Todd's paralysis may help physicians identify the origin of the seizure. It is important to distinguish the condition from a stroke, which requires different treatment.• Is there any treatment?
• Treatment of Todd's paralysis is symptomatic and supportive because the paralysis disappears quickly.
• What is the prognosis?
• An occurrence of Todd's paralysis indicates that a seizure has occurred. The prognosis for the patient depends upon the effects of the seizure, not the occurrence of the paralysis
Robert Bentley Todd
Todd's paralysis is a post-ictal - post-seizure - focal neurologic deficit which following a series of seizures, is characterised by persistent weakness - for several hours or longer - at the affected site. It may occur in association with hemiplegia in which seizures often accompany the outset. It is often confused with a cerebrovascular event.Pathologically, the clinical features may represent neuronal exhaustion after the period of increased activity.
The paralysis resolves spontaneously, usually within minutes or hours, rarely, within days.