Unstable angina and NSTEMI - in association with NICE
د. حسين محمد جمعةاختصاصي الامراض الباطنة
البورد العربي
كلية طب الموصل
2010
National Institute for Health and Clinical Excellence guidelines
This guideline offers best practice advice on the care of adults (18 years and older) with a diagnosis of unstable angina or non-ST segment elevation myocardial infarction (NSTEMI). Treatment and care should take into account patients' needs and preferences. Patients with unstable angina or NSTEMI should have the opportunity to make informed decisions about their care and treatment, in partnership with their healthcare professionals.Families and carers should also be given the information and support they need. This educational module contains information that has been adapted by BMJ Learning from NICE guidance, with the intention of reflecting the content of that guidance and facilitating its implementation. If an individual clinician has any queries or concerns about the relationship between NICE guidance and this educational module they should always refer to the original guidance published by NICE, and this should in all cases be regarded as the only definitive statement of the guidance.
Clopidogrel
clopidogrel treatment should be initiated with a single 300 mg loading dose and then continued at 75 mg once a day (with acetylsalicylic acid (ASA) 75 mg-325 mg daily). Since higher doses of ASA for maintenance therapy were associated with higher bleeding risk it is recommended that the dose of ASA should not be higher than 100 mg.There is emerging evidence about the use of a 600 mg loading dose of clopidogrel for patients undergoing PCI within 24 hours of admission. Clopidogrel does not have UK marketing authorisation for use at doses above 300 mg." The NICE Guideline Development Group (GDG) was not able to formally review all the evidence for a 600 mg loading dose and was therefore not able to recommend this at the time of publication.
• Learning bite
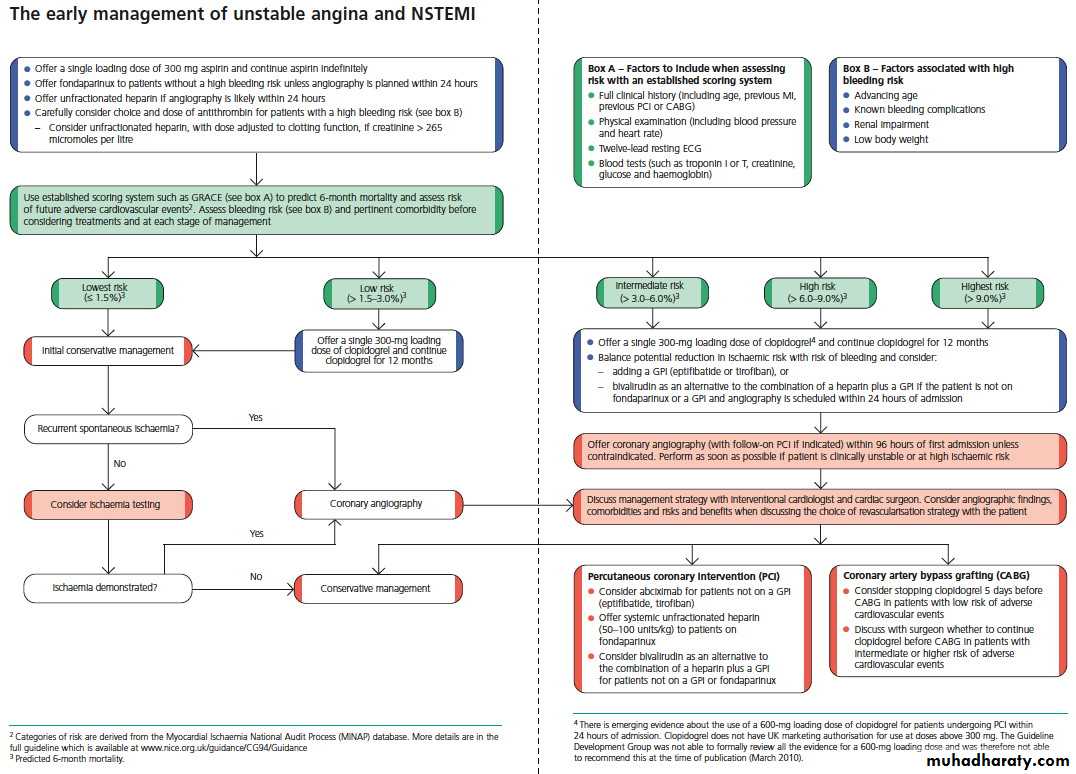
• As soon as the diagnosis of unstable angina or NSTEMI is made, and aspirin and antithrombin therapy have been offered, formally assess individual risk of future adverse cardiovascular events using an established risk scoring system that predicts six month mortality (for example, Global Registry of Acute Cardiac Events (GRACE)).Include in the formal risk assessment:
A full clinical history (including age, previous myocardial infarction (MI), and previous percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG))
A physical examination (including measurement of blood pressure and heart rate)
Resting 12-lead electrocardiography (ECG) (looking particularly for dynamic or unstable patterns that indicate myocardial ischaemia)
Blood tests (such as troponin I or T, creatinine, glucose, and haemoglobin).
Record the results of the risk assessment in the patient's care record.
Use risk assessment to guide clinical management, and balance the benefit of a treatment against any risk of related adverse events in the light of this assessment.
Use predicted six month mortality to categorise the risk of future adverse cardiovascular events as follows:
Predicted six month mortality
Risk of future adverse cardiovascular events1.5% or below
Lowest
>1.5 to 3.0%
Low
>3.0 to 6.0%
Intermediate
>6.0 to 9.0%
High
over 9.0%
Highest
The NICE Guideline Development Group selected six month mortality as the outcome measure for risk stratification because:
Mortality is a hard endpoint, which is available for most clinical trials
Mortality cannot be misinterpreted (as can an endpoint such as myocardial infarction, the definition of which has evolved over time, and varies between trials)
A six month time frame captured the majority of clinical events that occur after presentation with unstable angina or NSTEMI, and which may be influenced by an in hospital intervention (pharmacological or interventional).
• Shorter follow up intervals may miss events related to the index acute coronary syndrome event, and longer follow up may become increasingly influenced by other factors such as the effects of post-discharge secondary prevention interventions. Moreover, trials often do not report findings beyond the six month follow up period.
Key principles
You should adapt your consultation style to the needs of individual patients so that all patients have the opportunity to be involved in decisions about their medicines at the level they wishEstablish the most effective way of communicating with each patient and, if necessary, consider ways of making information accessible and understandable (for example, using pictures, symbols, large print, different languages, an interpreter, or a patient advocate)
Offer all patients the opportunity to be involved in making decisions about prescribed medicines. Establish what level of involvement in decision making the patient would like
Be aware that increasing patient involvement may mean that the patient decides not to take or to stop taking a medicine. If in the healthcare professional's view this could have an adverse effect, then the information provided to the patient on risks and benefits and the patient's decision should be recorded
Accept that the patient has the right to decide not to take a medicine, even if you do not agree with the decision, as long as the patient has the capacity to make an informed decision and has been provided with the information needed to make such a decision
Be aware that patients' concerns about medicines, and whether they believe they need them, affect how and whether they take their prescribed medicines
Offer patients information that is relevant to their condition, possible treatments, and personal circumstances, and that is easy to understand and free from jargon
Recognise that non-adherence is common and that most patients are non-adherent sometimes. Routinely assess adherence in a non-judgmental way whenever you prescribe, dispense, and review medicines
Be aware that although adherence can be improved, no specific intervention can be recommended for all patients. Tailor any intervention to increase adherence to the specific difficulties with adherence the patient is experiencing
Review patient knowledge, understanding, and concerns about medicines, and a patient's view of their need for medicine at intervals agreed with the patient, because these may change over time. Offer repeat information and review to patients, especially when treating long term conditions with multiple medicines
Key points
As soon as the diagnosis of unstable angina or NSTEMI is made, and aspirin and antithrombin therapy have been offered, formally assess individual risk of future adverse cardiovascular events using an established risk scoring system that predicts six month mortality (for example, Global Registry of Acute Cardiac Events (GRACE))
Consider intravenous eptifibatide or tirofiban as part of the early management for patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%), and who are scheduled to undergo angiography within 96 hours of hospital admission
Offer coronary angiography (with follow on PCI if indicated) within 96 hours of first admission to hospital to patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%) if they have no contraindications to angiography (such as active bleeding or comorbidity). Perform angiography as soon as possible for patients who are clinically unstable or at high ischaemic risk
When advising patients about the choice of revascularisation strategy (PCI or CABG), take account of coronary angiographic findings, comorbidities, and the benefits and risks of each intervention. When the role of revascularisation or the revascularisation strategy is unclear, resolve this by discussion involving an interventional cardiologist, cardiac surgeon, and other healthcare professionals relevant to the needs of the patient. Discuss the choice of revascularisation strategy with the patient
To detect and quantify inducible ischaemia, consider ischaemia testing before discharge for patients whose condition has been managed conservatively and who have not had coronary angiography
Before discharge offer patients advice and information about:
Their diagnosis and arrangements for follow up
Cardiac rehabilitation
Management of cardiovascular risk factors and drug therapy for secondary prevention
Lifestyle changes
Clinical tips
NICE Technology Appraisal 182 states "Prasugrel in combination with aspirin is recommended as an option for preventing atherothrombotic events in people with acute coronary syndromes having percutaneous coronary intervention, only when:• Immediate primary PCI for ST-segment-elevation myocardial infarction is necessary
• Stent thrombosis has occurred during clopidogrel treatment
• The patient has diabetes mellitus."
Specific contraindications to prasugrel are:
Hypersensitivity to the active substance or to any of the excipients
• Active pathological bleeding
• History of stroke orTIA• Severe hepatic impairment (Child-Pugh class C).
Prasugrel is currently a black triangle medicine. A black triangle is assigned to a product if the drug is an active substance which has been newly licensed for use in the UK. The black triangle symbol is not removed until the safety of the drug is well established. The MHRA wishes to receive all reports of suspected adverse reactions associated with black triangle products, in order to:
Confirm risk/benefit profiles established during the premarketing phase
Increase our understanding of the safety profiles of new medicines
Ensure that previously unrecognised side effects are identified as quickly as possible.
The common side effects of clopidrogel include bruising, haematoma (normally seen associated with a procedure, surgery, or trauma), epistaxis, gastrointestinal haemorrhage, diarrhoea, abdominal pain, dyspepsia, bleeding at puncture site.
Offer aspirin as soon as possible to all patients and continue indefinitely unless contraindicated by bleeding risk or aspirin hypersensitivity. Offer patients a single loading dose of 300 mg aspirin as soon as possible unless there is clear evidence that they are allergic to it. Aspirin therapy reduces the risk of a vascular event and should be offered to all patients with unstable angina or NSTEMI unless contraindicated (such as by active bleeding, current peptic ulceration, or for those considered clinically to be at a high potential risk of the consequences of bleeding, for example, recent neurosurgery or haemorrhagic stroke).
It should be noted that those at higher risk of bleeding, such as those with renal impairment, may have a higher absolute risk of a vascular event and therefore may have a higher potential absolute benefit from aspirin, which may outweigh even the higher bleeding risk associated with their underlying renal impairment. Individual patient circumstances will dictate the advisability of giving aspirin but in only a small minority would it be anticipated that the risk of prescription will outweigh the benefit. An aspirin loading dose of 300 mg should be given as soon as possible followed by daily maintenance of 75-150 mg.
Consider unfractionated heparin, with dose adjustment guided by monitoring of clotting function, as an alternative to fondaparinux for patients with significant renal impairment (creatinine above 265 µmol/l). Renal impairment significantly increases the bleeding risk. Unfractionated heparin, with dose adjustment guided by monitoring of clotting function, is best in this circumstance.
Fondaparinux has a lower risk of bleeding complications than enoxaparin, at all levels of renal impairment, but patients with creatinine >265 µmol/l were excluded from the large trial (OASIS-5) upon which the recommendation to use fondaparinux as the default antithrombin for patients with creatinine <265 µmol/l was based.
Learning bite
Carefully consider the choice and dose of antithrombin in patients who have a high risk of bleeding associated with any of the following:• Advancing age
• Known bleeding complications
• Renal impairment
• Low body weight.
Learning bite
Offer patients clear information about the risks and benefits of the treatments offered so that they can make informed choices about management strategies. Information should be appropriate to the patient's underlying risk of a future adverse cardiovascular event and any comorbidities.When advising patients about the choice of revascularisation strategy (PCI or CABG), take account of coronary angiographic findings, comorbidities, and the benefits and risks of each intervention.
When the role of revascularisation or the revascularisation strategy is unclear, resolve this by discussion involving an interventional cardiologist, cardiac surgeon and other healthcare professionals relevant to the needs of the patient. Discuss the choice of revascularisation strategy with the patient.
Cardiac rehabilitation should be equally accessible and relevant to all patients after an MI, particularly people from groups that are less likely to access this service. These include people from black and minority ethnic groups, older people, people from lower socioeconomic groups, women, people from rural communities, and people with mental and physical health comorbidities.
Before discharge offer patients advice and information about:
Their diagnosis and arrangements for follow upCardiac rehabilitation
Management of cardiovascular risk factors and drug therapy for secondary prevention
Lifestyle changes.
All patients who smoke should be advised to quit and be offered support and advice, and referral to an intensive support service.
Good evidence exists for the longer term benefits of a comprehensive rehabilitation process following MI. The NICE post-MI guideline found rehabilitation to be cost effective and the GDG felt that this is good evidence that rehabilitation is cost effective in general. Recent NICE guidance recommends that people with MI should receive formal rehabilitation and delivery of secondary prevention measures and they do not distinguish between people with NSTEMI and STEMI.
Although no evidence exists specifically for people with unstable angina, it is part of the same pathophysiological continuum as NSTEMI and so the recommendations would logically apply to both groups.
It is vital that information and education is delivered in an appropriate format to people prior to discharge from hospital given the importance of establishing people on appropriate medication, and the value of people understanding the indications and actions of these medications, and the underlying nature of their cardiac condition and any effect of comorbidity.
Rehabilitation, in its most general sense, actually starts from the moment of diagnosis because from this time onwards there is potential benefit to people from being well informed and psychologically supported, and therefore the distinction between in hospital and post-discharge intervention is somewhat arbitrary. The overriding consideration should be to ensure that the process is continuous and that responsibility for delivery of the components of rehabilitation (education, information, psychosocial support, structured exercise, etc) should be clearly attributed.
Offer coronary angiography (with follow on PCI if indicated) to patients initially assessed to be at low risk of adverse cardiovascular events (predicted six month mortality 3.0% or less) if ischaemia is subsequently experienced or is demonstrated by ischaemia testing. Angiography should be expedited for those who are clinically unstable or at high ischaemic risk.
If untreated, the prognosis is poor and mortality high, particularly in people who have had myocardial damage. Appropriate triage, risk assessment, and timely use of acute pharmacological or invasive interventions are critical for the prevention of future adverse cardiovascular events (myocardial infarction, stroke, repeat revascularisation, or death). The number of people admitted with non ST-segment elevation ACS continues to be high and with worrying trends in the incidence of obesity and diabetes, and lifestyles that involve less exercise, the management of these conditions remains a high priority.
It is recommended that treatment with clopidogrel in combination with low dose aspirin should be continued for 12 months after the most recent acute episode of non-ST segment elevation ACS. Thereafter, standard care, including long term treatment with low dose aspirin alone, is recommended.
Current NICE guidance for drug eluting stents does not recommend any specific duration of clopidogrel therapy in addition to aspirin. However, NICE refers to the recommendations from the American College of Cardiologists/American Heart Association PCI guidelines and the British Cardiovascular Intervention Society advising a duration of at least 12 months, after which time continuation of clopidogrel should be reviewed taking into account the risk of further ischaemic events (particularly the risk of subsequent stent thrombosis) and potential bleeding complications on an individual patient basis.
A 2010 interim analysis of data from two studies (Park S-J, et al. Duration of dual antiplatelet therapy after implantation of drug-eluting stents. N Engl J Med 2010. Published online 15 March suggests no benefit for continuing to use clopidogrel in addition to aspirin for more than 12 months after implantation of drug eluting stents. However, because of limitations, further studies are required to confirm or refute these findings. The findings of this analysis are insufficient to recommend a change in practice.
Learning bite
Consider discontinuing clopidogrel treatment five days before CABG in patients who have a low risk of adverse cardiovascular events. For patients at intermediate or higher risk of adverse cardiovascular events, discuss the continuation of clopidogrel before CABG with the cardiac surgeon and base the decision on the balance of ischaemic and bleeding risk.Consider intravenous eptifibatide or tirofiban as part of the early management for patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%), and who are scheduled to undergo angiography within 96 hours of hospital admission. Consider abciximab, usually in the catheter laboratory, as an adjunct to PCI for patients at intermediate or higher risk of adverse cardiovascular events who are not already receiving a glycoprotein IIb/IIIa inhibitor. Balance the potential reduction in a patient's ischaemic risk with any increased risk of bleeding, when determining whether a GPI should be offered.
Offer coronary angiography (with follow on PCI if indicated) within 96 hours of first admission to hospital to patients who have an intermediate or higher risk of adverse cardiovascular events (predicted six month mortality above 3.0%) if they have no contraindications to angiography (such as active bleeding or comorbidity). Perform angiography as soon as possible for patients who are clinically unstable or at high ischaemic risk.
An early invasive strategy does have benefit, mainly in reducing recurrent ischaemia/infarction in the short term, but also in reducing longer term mortality or reinfarction. However, this benefit appears to be greatest in those people at higher absolute risk of such events (with the most benefit seen in those at the highest risk).
March 2010 the European Medicines Agency updated its warning for clopidogrel containing medicines and the interaction between clopidogrel and proton pump inhibitors.
Clopidogrel is converted in the body to its active form by an enzyme called CYP2C19. As heartburn and stomach ulcers can occur as side effects of clopidogrel, patients taking clopidogrel often take PPIs to prevent or ease their symptoms.
In May 2009 the product information for all clopidogrel containing medicines was amended to discourage the concomitant use of PPIs and clopidogrel unless absolutely necessary.
Since then, the Committee for Medicinal Products for Human Use (CHMP) has become aware of the results of a number of new studies, some of which put in question the clinical relevance of interactions between PPIs as a class and clopidogrel. However, two studies, completed at the end of August 2009, looked into the effect of omeprazole on the blood levels of the active form of clopidogrel.
The studies confirmed that omeprazole can reduce the levels of the active form of clopidogrel in the blood and reduce its antiplatelet effects, therefore supporting the conclusion that there is an interaction between clopidogrel and omeprazole and esomeprazole.
Taking all of the currently available data into account, the CHMP and its Pharmacovigilance Working Party concluded that there are no solid grounds to extend the warning to other PPIs. The class warning for all PPIs has been replaced with a warning stating that only the concomitant use of clopidogrel and omeprazole or esomeprazole should be discouraged.
Learning bite: medicines adherence
Patients discharged following NSTEMI are likely to be on many medicines. It is thought that between a third and a half of all medicines prescribed for long term conditions are not taken as recommended. Addressing non-adherence is not about getting patients to take more medicines per se. Rather, it starts with an exploration of patients' perspectives of medicines and the reasons why they may not want or are unable to use them. You have a duty to help patients make informed decisions about treatment and use appropriately prescribed medicines to best effect.Assessment of LV function is recommended in all patients who have had an MI.
Consider assessing LV function in all patients with unstable angina.Record measures of LV function in the patient's care record and in correspondence with the primary healthcare team and the patient.
It is logical to assess LV function in all people with unstable angina and NSTEMI so that specific treatment for LV dysfunction can be offered to improve symptoms and outcome.
Left ventricular function may improve after an acute ischaemic event with the resolution of myocardial stunning and the onset of healing. It may also deteriorate because of myocardial remodelling or progression of coronary disease. It may therefore also be important to monitor LV function during follow up, because of this potential for change with time.
Learning bite
To detect and quantify inducible ischaemia, consider ischaemia testing before discharge for patients whose condition has been managed conservatively and who have not had coronary angiography.If untreated, the prognosis of patients with non-ST elevation myocardial infarction is poor and mortality high, particularly in people who have had myocardial damage.