Operative Interventions
In obstetricsBy
Dr. Afraa Mahjoob Al-Naddawi
FIBOG, CABOG
The goal of operative delivery is to expedite delivery with a minimum of maternal or neonatal morbidity.
There has been a growing recognition of the short and long term morbidity of pelvic floor injury following operative vaginal delivery.
Caesarean section, particularly in the second stage of labor, also carries significant morbidity and implications for future birth.
Episiotomy:
It is an incision through the perineum made to enlarge the diameter of the vulval outlet and assist child birth.Regarding the prevalence, there is considerable international variation (rates are 50% in US and 99% in eastern Europe).
In UK, rates approximates to the WHO recommendation of 10% of deliveries.
Technique:
an episiotomy is performed in the 2nd stage when the perineum is being stretched and it is deemed necessary.Analgesia (epidural or local infiltration).
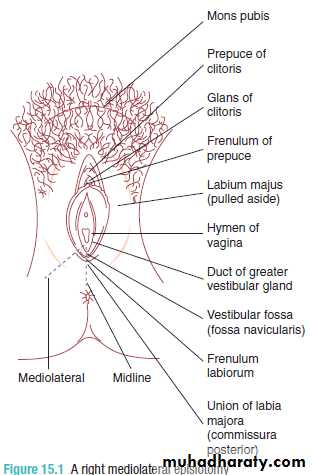
The incision can be either midline or at an angle from the posterior end of the vulva (a mediolateral episiotomy which is usually recommended).
Midline episiotomy is an incision in a comparatively avascular area and results in less bleeding, quicker healing and less pain, however, there is an increased risk of extension to involve the anal sphincter (third/fourth degree tear).
A mediolateral episiotomy should start at the posterior part of the fourchette, move backwards and then turn medially well before the border of the anal sphincter, so that an extension will miss the sphincter.
Complications: hemorrhage, infection, extension to the anal sphincter, dyspareunia.
Perineal trauma
1. First-degree trauma corresponds to lacerations of the skin/vaginal epithelium alone.2. Second-degree tears involve perineal muscles and therefore include episiotomies.
3. Third-degree extensions involve any part of the anal sphincter complex (external and internal sphincters):
i Less than 50 per cent of the external anal sphincter is torn.
ii More than 50 per cent of the external anal sphincter is torn.
iii Tear involves the internal anal sphincter (usually there is complete disruption of the external sphincter).
4. Fourth-degree tears involve injury to the anal sphincter complex extending into the rectal mucosa.
Perineal repair:
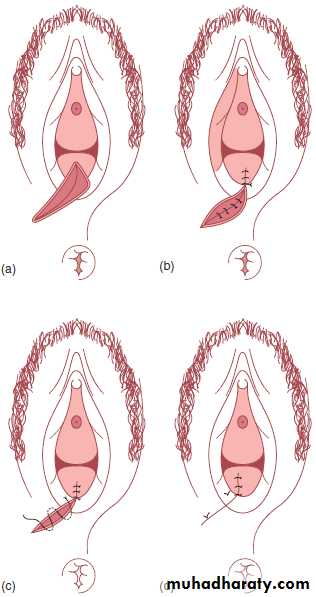
Ensure adequate analgesia, a pad is placed in the vagina to prevent the blood coming from the uterus from obscuring the view, the extent of the cuts and lacerations is checked.first the vaginal mucosa is repaired using rapidly absorbed suture material with continuous stitch.
muscle layer is closed by interrupted suture then the skin is closed either by interrupted suture or continuous subcuticular stitch which produces more comfortable results.
in case of the presence of third or fourth degree trauma, the repair will need a regional or general anesthesia as the local infiltration does not allow relaxation of the sphincter enough to allow a satisfactory repair and the repair here need to be performed by trend practitioner. Repair of the rectal mucosa should be performed first.
After repair, a gentle vaginal examination is done to check for any missed tears and removal of the pad which was placed at the top of the vagina is done.
Finally, a finger is put in the rectum to check that no sutures have passed through into the rectal mucosa and that the sphincter is intact. If sutures are felt in the rectum they must be removed and replaced.
Instrumental vaginal delivery:
It is delivery of a baby vaginally using an instrument for assistance which can be done by forceps or ventouse (vacuum extractor).The incidence of instrumental intervention varies widely within and between countries and may be as infrequent as 1.5% or as often as 26% . In the UK approximately 12% of deliveries are assisted with forceps or ventouse.
Indications for assisted vaginal delivery:
• Fetal indications:• The most common fetal indication are those concerning malposition of the fetal head (occiput transverse and occiput posterior) which occur more frequently with regional anesthesia.
• Presumed fetal compromise.
• Vaginal breech delivery: forceps can be applied to the aftercoming head to control delivery of the vertex.
• Use of elective instrumental intervention for infants of reduced weight is more controversial.
B. Maternal indications:
• The most common is maternal distress, exhaustion or undue prolongation of the second stage of labor. Labor may be deemed prolonged if the second stage last > 2 H in primigravida (3 H if an epidural is in situ) or > 1H in a multipara (2H if an epidural is in situ).
• Medically significant conditions such as aortic valve disease with significant outflow obstruction or mysthenia gravis.
Instrument choice:
The choice of instrument should be based on a combination of indication, experience and training but there are conditions in which ventouse should not be used:• In gestations less than completed 35 weeks because of the risk of cephalhematoma and intracranial hemorrhage.
• Face or breech presentation.
The ventouse, when compared to the forceps is
significantly more likely to:• fail to achieve a vaginal delivery;
• be associated with a cephalohaematoma (subperiosteal bleed);
• be associated with retinal hemorrhage;
• be associated with maternal worries about the baby;
It is significantly less likely to be associated with:
• use of maternal regional/general anesthesia;• significant maternal perineal and vaginal trauma;
• severe perineal pain at 24 hours;
The ventouse is equally likely to be associated with:
• delivery by Caesarean section;• low 5 minute Apgar scores.
Prerequisites for any instrumental delivery:
• Confirmed rupture of the membranes.
• The cervix must be fully dilated (except second twin and rare other situations).
• Vertex presentation with identification of the position.
• For occipitoanterior and transverse positions, no part of the fetal head should be palpable abdominally. For occipito-posterior positions, it is acceptable that one-fifth of the head may be palpable. The presenting part should be at 1 or more below the ischial spines.
• Adequate analgesia/anaesthesia.
• Empty bladder/no obstruction below the fetal head(contracted pelvis/pelvic kidney/ovarian cyst, etc.).
• A knowledgeable and experienced operator with adequate preparation to proceed with an alternative approach if necessary.
• An adequately informed and consented patient (consent must be sought though not necessarily written).
Technique:
• Ventouse:• Suction cup of a silastic or rigid construction is connected via tubing to a vacuum source and now recent development have incorporated the vacuum mechanism into hand held pumps e.g. omni cup.
• metal cups appear to be more suitable for occipito- posterior, transverse and difficult occipitoanterior position deliveries when the infant is large or there is marked caput.
The center of the cup should be positioned directly of the flexion point, this point is located on the sagittal suture 3 cm anterior to the posterior fontanelle and thus 6 cm posterior to the anterior fontanelle.
First the suction pressure is generated to 0.2 kg/cm2 and checking is made to make sure that no maternal tissue is caught under the cup edge.
The pressure is then increased to the operating vacuum pressure which is between 0.6-0.8 kg/cm2.
Safe and gentle traction is then applied in concert with uterine contractions with voluntary expulsive efforts.
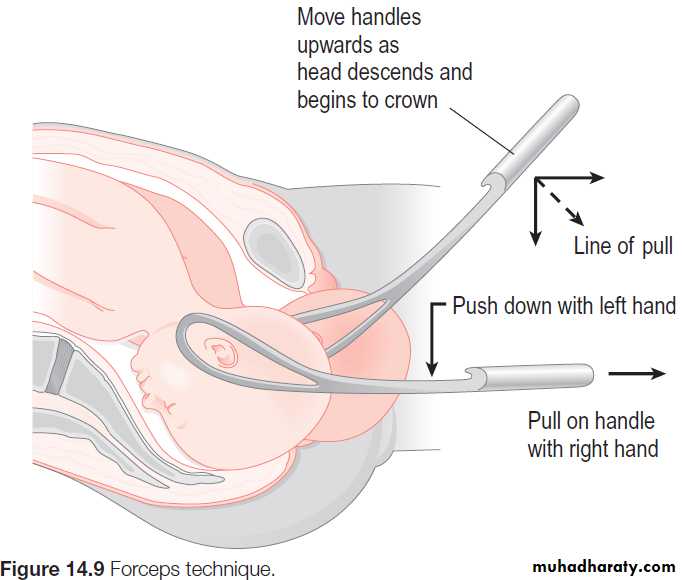
b. forceps:
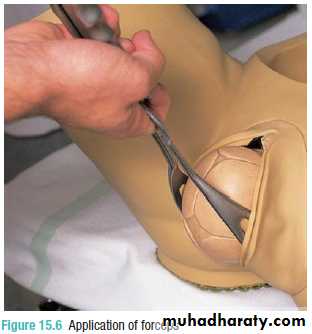
Non rotational forceps are used when the head is occiputoanterior ± 15o such as Neville Barnes or Simpson forceps.
If the head is positioned > 15o from the vertical, rotation must be done before traction using for example Kielland forceps which has sliding lock that facilitate correction of a asynclitism.
The left blade is inserted before the right blade with the operator’s right hand protecting the vaginal wall from direct trauma then the right blade is inserted with the operator’s left hand protecting the vagina.
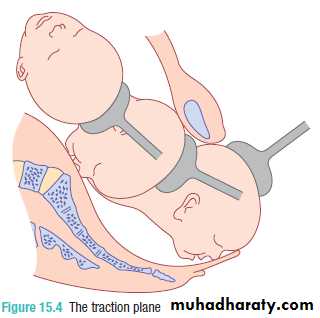
Traction should be applied intermittently in concert with uterine contractions and maternal expulsive efforts and the axis of traction changes during the delivery and it is guided along the “J” shaped curve of the pelvis.
Most studies suggest failure rates of 10–15 per cent. Several factors contribute to delivery failure:
• Inadequate initial case assessment – high head, misdiagnosis of the position and attitude of the head.
• Failure due to traction in the wrong plane.
• Poor maternal effort with inadequate use of Syntocinon to aid expulsive efforts in the second stage.
• Failure to select the correct ventouse cup type and/or incorrect cup position.