ACQUIRED IMMUNODEFICIENCYSYNDROME ICD-10 B20-B24(HIV infection, AIDS)
Dr. Nadia AzizC.A.B.C.M.
Community medicine department
Baghdad medical college
Objective
1- Define the acquired immunodeficiency syndrome2- Identify the causative agent
3- Identify the mode of transmission & the high risk group
4- Identify the ways of prevention & management
Introduction
Acquired Immunodeficiency syndrome (AIDS) is a term first used in 1981 by epidemiologists concerned about the emergence of a cluster of diseases associated with loss of cellular immunity in adults who had no obvious reason for presenting such immune deficiencies.Introduction
AIDS is the late clinical stage of infection with the human immunodeficiency virus (HIV). Within weeks to months after infection with HIV, many persons develop an acute self-limited mononucleosis-like illness lasting for a week or two.They may then be free of clinical signs or symptoms for months or years before other clinical manifestations develop.
Introduction
More than a dozen opportunistic infections and several cancers were considered to be sufficiently specific indicators of the underlying AIDS.
Other Presentations
Includes:Tuberculosis, pneumococcal disease and non-typhoid salmonellosis, which are not
diseases of high virulence.
Bacterial pneumonia is one of the commonest presentations.
Diagnosis
All HIV-infected persons are regarded as AIDS cases if:1- CD4 cell count of under 200/mm3
or
2- CD4 T-lymphocyte percentage of total lymphocytes under 14%, regardless of clinical status.
Diagnosis
The most commonly used screening test:1- EIA or ELISA is highly sensitive and specific.
2- Western blot test.
detectable antibodies within 1–3 months after infection
3- HIV antigen
4- PCR tests to detect viral nucleic acid sequences..
Diagnosis
Passively transferred maternal anti-HIV antibodies often cause falsely positive anti-HIV EIA tests in these children even up to the
age of 15 months.
Case-fatality
In the absence of effective anti-HIV treatment, the AIDS case-fatality rate is high.Survival time in many developing country studies is often under 1 year,
In industrialized countries 80%–90% of untreated patients used to die within 3–5 years after diagnosis.
Infectious agent
Human immunodeficiency virus (HIV), a retrovirus.Two serologically and geographically distinct types with similar epidemiological characteristics,
HIV-1 and HIV-2.
The pathogenicity of HIV-2 may be lower than that of HIV-1
Occurrence
AIDS was first recognized as a distinct clinical entity in 1981.Of the estimated 40 million persons (34–46 million) living with HIV infection or AIDS worldwide.
The largest elements were estimated at 25–28.2 million in sub-Saharan Africa. In sub-Saharan Africa, AIDS is called "slim disease."
Occurrence
Globally, AIDS caused an estimated3.1 million deaths in 2003 (2.5–3.5 million)
Reservoir
Humans HIV is thought to have recently evolved from chimpanzee viruses.Mode of transmission
Person to person transmission through1- Unprotected (heterosexual or homosexual) intercourse
2- Contact of abraded skin or mucosa with body secretions such as blood, CSF or semen.
3- The use of HIV- contaminated needles
4- Transfusion of infected blood or its components
5- The transplantation of HIV-infected tissues or organs.
Mode of transmission
the presence of a concurrent sexually transmitted disease, (ulcerative) can facilitate HIV transmission.Mode of transmission
6- HIV transmitted from mother to child (MTCT or vertical transmission).
From 15% to 35% of infants born to HIV-positive mothers are infected through placental processes at birth.
HIV-infected women can transmit infection to their infants through breast-feeding and this can account for up to half of mother-to-child HIV transmission.
Incubation period
Variable.The time from infection to the development of detectable antibodies is generally 1–3 months.
The time from HIV infection to diagnosis of AIDS range from less than 1 year to 15 years or longer.
HIV infection, AIDS
The only factor that has been shown to affect progression from HIV infection to the development of AIDS is age at initial infection:adolescent and adults (males and females) who acquire HIV infection at an early age progress to AIDS more slowly than those infected at an older age.
Period of communicability
Begins early after HIV infection and extends throughout life.Infectivity increases:
1- During the first months
2- With viral load
3- With worsening clinical status
4- With the presence of other STIs
Susceptibility
Factors increase susceptibility
1- Presence of other STIs (ulcerative)
2- Not being circumcised for males, a factor possibly related to the general level of penile hygiene.
Interaction with other infections
1-The major interaction is with Mycobacterium tuberculosis infection.Persons with latent tuberculous infection who are infected with HIV develop clinical tuberculosis at an increased rate.
Lifetime risk of developing tuberculosis is multiplied by a factor of 6–8
Interaction with other infections
2- Other adverse interactions with HIV infectioninclude pneumococcal infection, non-Typhiod salmonellosis, falciparum malaria and visceral leishmaniasis.
Methods of control
A- Preventive measures1) Public and school health education must stress that having multiple and especially concurrent and/or overlapping sexual partners or sharing drug both increase the risk of HIV infection.
Programs for school-age youth should address the needs and developmental levels of both
students and those who do not attend school.
Preventive measures
2) The only absolutely sure way to avoid infection through sex to abstain from sexual intercourse or to engage in mutually monogamous sexual intercourse onlyIn other situations, latex condoms must be used correctly
Preventive measures
3) Expansion of facilities for treating drug users reduces HIV transmission.
Preventive measures
4) HIV testing and counselling for:• persons who are ill or involved in high-risk behaviors
• attenders at antenatal clinics, to diagnose maternal infection
• couple counselling (marital or premarital)
d) confidential HIV counselling and testing for the “worried well”.
Preventive measures
5) All donated units of blood must be tested for HIV antibody, only donations testing negative can be used.People who have engaged in behaviors that place them at increased risk of HIV infection should not donate plasma, blood, organs for transplantation, tissue or cells (including semen for artificial insemination).
Preventive measures
6) Care must be taken in handling, using and disposing of needles or other sharp instruments. Health care workers should wear latex gloves, eye protection and other personalprotective equipment in order to avoid contact with blood or with fluids.
Preventive measures
7) WHO recommends immunization of asymptomatic HIV infected children with the EPI vaccines.Those who are symptomatic should not receive BCG vaccine.
B. Control of patient, contacts and the immediate environment:
1) Report to local health authority: Class 2
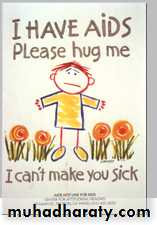
2) Isolation: Isolation of the HIV-positive person is unnecessary, ineffective and unjustified.
B. Control of patient, contacts and the immediate environment:
3) Notification of contacts and source of infection: The infected patient should ensure notification of sexual and needle sharing partners whenever possible.Notification by the health care provider is justified only when the patient, after counselling, still refuses to notify his/her partner(s), and this will not harm the index case.
B. Control of patient, contacts and the immediate environment:
Prior to the development of relatively effective antiretroviral treatment1- Prophylactic use of oral trimethoprim-
sulfamethoxazole, with aerosolized pentamidine is recommended to prevent P. carinii pneumonia.
2- All HIV infected persons should do tuberculin skin tests and be evaluated for active TB.
B. Control of patient, contacts and the immediate environment:
3- If active TB is found, anti tuberculosis treatment should be given.If no active TB is found, patients who are tuberculin-positive or were recently exposed should be offered preventive treatment with isoniazid for 12 months
Treatment
AIDS must be managed as a chronic disease, antiretroviral treatment is complex,involving a combination of drugs:
resistance will rapidly appear if a single drug is used.
The drugs are toxic and treatment must be lifelong.
Treatment
A successful treatment is not a cure, although it results in suppression of viral replication.
In general, a protease inhibitor and two
non-nucleoside reverse transcriptase inhibitors should be used initially.
Post Exposure Prophylaxis
The factors to consider before recommending post exposure prophylaxis (PEP) includes:1- The nature of the exposure
2- Whether the exposed worker might be pregnant
3- The local occurrence of drug resistant
HIV strains.
Post Exposure Prophylaxis
Include a basic 4-week regimen of two drugs (zidovudine and lamivudine) for most HIV exposuresAn expanded regimen that includes the addition of a protease inhibitor (indinavir or nelfinavir)