LEPROSY(Hansenʼs disease)
A Little History …
Gerhard Henrik Armauer Hansen was a physician which first identified Mycobacterium leprae as the cause of leprosy in 1873FYI
7/29/1841-2/12/1912
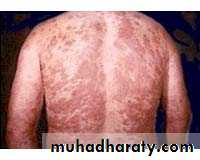
EPIDEMIOLOGY1. Identification—A chronic bacterial disease of the skin, peripheral ,nerves and (in lepromatous patients) the upper airway.
Two polar forms:
i) lepromatous (multibacillary) leprosy
ii) tuberculoid (paucibacillary) leprosy
Borderline leprosy has features of both polar forms and is more labile.
Indeterminate leprosy
is characterized by hypopigmented maculae with
ill-defined borders; if untreated, it may progress to
tuberculoid, borderline or lepromatous disease.
EPIDEMIOLOGY
Case definition (WHO operational definition)
A case of leprosy is a person having one or more of the following, who has yet to complete a full course of treatment:
● Hypopigmented or reddish skin lesion(s) with definite loss of sensation
● Involvement of the peripheral nerves (definite thickening with loss of
sensation)
● Skin smear positive for acid-fast bacilli.
EPIDEMIOLOGY
The operational case definition includes retrieved defaulters with signs of active disease and relapsed cases who have previously completed a full course of treatment. It does not include cured persons with late reactions or residual disabilities.EPIDEMIOLOGY
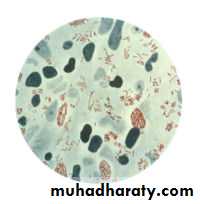
Laboratory criteria include the presence of alcohol-acid-fast bacilli in skin smears (scrape-incision method).Leprosy cases can be classified as follows:
- Multibacillary leprosy: more than 5 patches or lesions on the skin
- Paucibacillary leprosy: 1 to 5 patches or lesions on the skin.
EPIDEMIOLOGY
2. Infectious agent—Mycobacterium leprae. which cannot be grown in bacteriological media or cell cultures.EPIDEMIOLOGY
3. Occurrence—During 2006, 260000 persons were diagnosed with leprosy, over half of them in India.Control has improved with the introduction of multidrug therapy (MDT).
WHO has targeted the disease for elimination (less than 1 case/10 000 population) and this has been achieved in all but three(Brazil,Nepal and Tanzania) of the 122 countries endemic in 1985.
Newly recognized cases in the USA are few .Most of these cases are in immigrants and refugees whose disease was acquired in their native countries.
EPIDEMIOLOGY
4. Reservoir—Humans are the only significant reservoirs.Feral armadillos, and monkeys have been found naturally affected .5. Mode of transmission—The disease is in all likelihood transmitted from the nasal mucosa of a patient to the skin and respiratory tract of another person.
Transmission requires close contact.
Although the bacillus can survive up to 7 days in dried nasal secretions, indirect transmission is unlikely.
EPIDEMIOLOGY
6. Incubation period—This ranges from 9 months to 20 years, the average is probably 4 years for tuberculoid leprosy and twice that for lepromatous leprosy. The disease is rarely seen in children under age 3;however, more than 50 cases have been identified in children under 1, the youngest at 10 weeks.
EPIDEMIOLOGY
7. Period of communicability—
Clinical and laboratory evidence suggest that infectiousness is lost in most instances within a day of treatment with multidrug therapy.
EPIDEMIOLOGY
8. Susceptibility—The persistence and form of leprosy depend on the ability to develop effective cell-mediated immunity.
The high prevalence of M. leprae-specific lymphocyte transformation and antibodies specific for M. leprae among close contacts of leprosy patients suggests that infection is frequent, yet clinical disease occurs in only a small proportion of such close contacts.
The immunological lepromin test used earlier
should be reserved for research activities.A. PREVENTIVE MEASURES
The availability of effective and time-limited treatment, with rapid elimination of infectiousness, has changed management from societal isolation to ambulatory treatment.Hospitalization should now be limited only to cases such as the surgical correction of deformities, treatment of ulcers resulting from anaesthesia, and severe leprosy reactions.
A. PREVENTIVE MEASURES
Early detection and treatment of cases.Dapsone chemoprophylaxis is not recommended (limited effectiveness and danger of resistance).
A. PREVENTIVE MEASURES
Health education together with counseling of patients and relatives must stress the availability of effective multidrug therapy, the absence of infectivity of patients under continuous treatment and the prevention of physical and social disabilities.
BCG vaccination can induce protection against both the tuberculoid and lepromatous forms of the disease.
B. CONTROL OF PATIENT, CONTACTS AND THE IMMEDIATE ENVIRONMENT
1) Report to local health authority: obligatory in many countries and desirable in all, Class 2.2) Isolation: Unnecessary.Reducing contact with known leprosy patients is of dubious value and can lead to stigmatization. No restrictions in employment or attendance at school are indicated.3) Quarantine: Not applicable.4) Immunization of contacts: Not recommended
5) Investigation of contacts and source of infection: Examination of close contacts can be useful.
B. CONTROL OF PATIENT, CONTACTS AND THE IMMEDIATE ENVIRONMENT
6) Specific treatment:Combined chemotherapy regimens are essential.
The duration of therapy for multibacillary leprosy can be shortened to 12 months from the previously recommended 24 months.
Patients under treatment should be monitored for drug side-effects, for leprosy reactions and for development of trophic ulcers.
Some complications may need to be treated in a referral center.
B.CONTROL OF PATIENT, CONTACTS AND THE IMMEDIATE ENVIRONMENT
Ambulatory treatment by multidrug therapy (MDT) is given according to case classification.Adults with multibacillary leprosy(wih more than 5 skin lesions): The standard WHO regimen is a combination of the following for 12 months:
» Rifampicin: 600 mg once a month
» Dapsone: 100 mg once a day
» Clofazimine: 50 mg once a day and 300 mg
once a month.
B.CONTROL OF PATIENT, CONTACTS AND THE IMMEDIATE ENVIRONMENT
• Adults with paucibacillary leprosy(adults with 2-5 skin lesions): The standard WHO regimen is a combination of the following for 6 months:
• » Rifampicin: 600 mg once a month
• » Dapsone: 100 mg once a day.
• Adults with a single lesion :The standard WHO regimen is a combination of the following,given once:
• Rifampici :600mg.
• Ofloxacin:400mg.
• Minocycline:100mg.
B. CONTROL OF PATIENT, CONTACTS AND THE IMMEDIATE ENVIRONMENT
Children must receive appropriately scaled-down doses (in child blister-packs).Patients must be advised to complete the full course of treatment and to seek care in the event of drug side-effects (allergic reaction) and immunological reactions (neuritis leading to damage of the peripheral nerve trunks).
Multiple drug therapy is available free of charge through WHO. MDT drugs must be given in blister packs, free of charge, to all patients.
B. CONTROL OF PATIENT, CONTACTS AND THE IMMEDIATE ENVIRONMENT
Treatment of reactions:Corticosteroids are the drugs of choice for the treatment of reactions associated with neuritis.
Clofazimine is the drug of choice for the management of recurrent ENL reactions.Its use in MDT has significantly reduced the frequency and severity of ENL reactions worldwide.