
Erectile dysfunction
ED
Dr . Hasanain Farhan Hasan

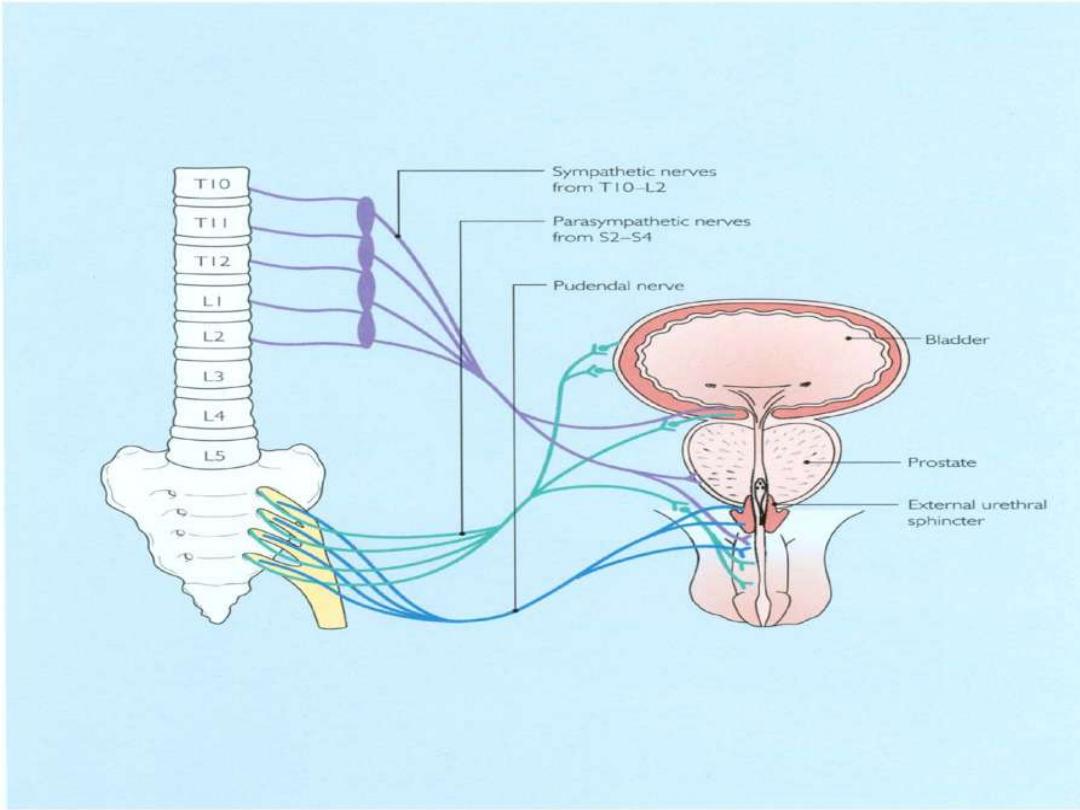
Innervation
Autonomic: sympathetic nerves originating from T11–L2,
and parasympathetic nerves originating from S2–4, join to
form the pelvic plexus.The cavernosal nerves ie
parasypathetic are branches of pelvic plexus that innervate
the penis. Parasympathetic stimulation causes erection;
sympathetic activity causes ejaculation and detumescence
(loss of erection).
Somatic: somatosensory (afferent) information travels and
enters the spinal cord at S2-4. from S2-4 the somatic
efferent (i.e. somatomotor) innervate the ischiocavernosus
and bulbocavernosus muscles of the penis.
Central: medial preoptic area (MPOA) and paraventricular
nucleus (PVN) in the hypothalamus are important centres for
sexual function and penile erection
Physiology of erection and
ejaculation
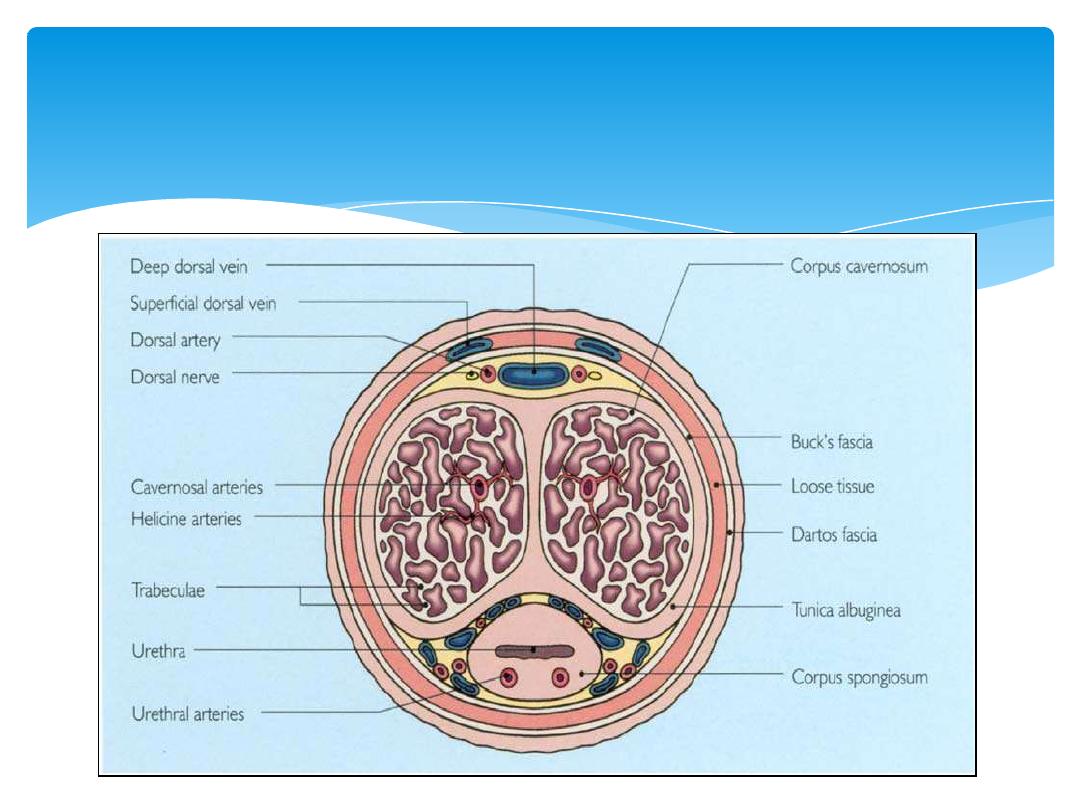
Each corpus cavernosum comprises a thick fibrous sheath, the tunica albuginea,
which surrounds the erectile tissue. Each corpus has
a centrally running cavernosal artery, which supplies blood to the multiple lacunar
spaces, which are interconnected and lined by vascular
endothelium

Neuroendocrine signals from the brain, created by audiovisual or
tactile stimuli, activate the autonomic nuclei of the spinal erection
centre (T11-L2 and S2-4). Signals are relayed via the cavernosal
nerve to the erectile tissue of the copora cavernosa. This triggers
increased arterial blood flow into sinusoidal spaces (secondary to
arterial and arteriolar dilatation). The result is expansion of the
sinusoidal spaces against the tunica albuginea. Rising
intracavernosal pressure and contraction of the ischiocavernosus
muscles produces a rigid erection.
Following orgasm and ejaculation, vasoconstriction due to
increased sympathetic activity produces detumescence .
3 types of Physiological erections can occur:
1.
nocturnal
2.
Psychogenic
3.
reflexogenic
Mechanism of erection

Tactile stimulation of the glans penis causes sensory
information travel to sympathetic nuclei. Sympathetic
efferent signals cause contraction of smooth muscle
of the epididymis, vas deferens, and secretory glands,
propelling spermatozoa and glandular secretions into
the prostatic urethra. There is simultaneous closure of
the internal urethral sphincter directing sperm into
the bulbourethra (emission), but preventing sperm
entering the bladder. Rhythmic contraction of the
bulbocavernosus muscle (somatomotor innervation)
leads to the pulsatile emission of the ejaculate from
the urethra.
Ejaculation

0 Flaccid phase
Cavernosal smooth muscle contracted; sinusoids empty;
minimal arterial flow
1 Latent (filling) phase
Increased cavernosal artery flow; penile elongation
2 Tumescent phase
Rising intracavernosal pressure; erection forming
3 Full erection phase
Increased cavernosal pressure causes penis to become
fully erect
4 Rigid erection phase
Further increases in pressure + ischiocavernosal
muscle contraction
5 Detumescence phase
Following ejaculation, sympathetic discharge
resumes; there is smooth muscle contraction and vasoconstriction; reduced
arterial flow; blood is expelled from sinusoidal spaces
Phases of erectile process
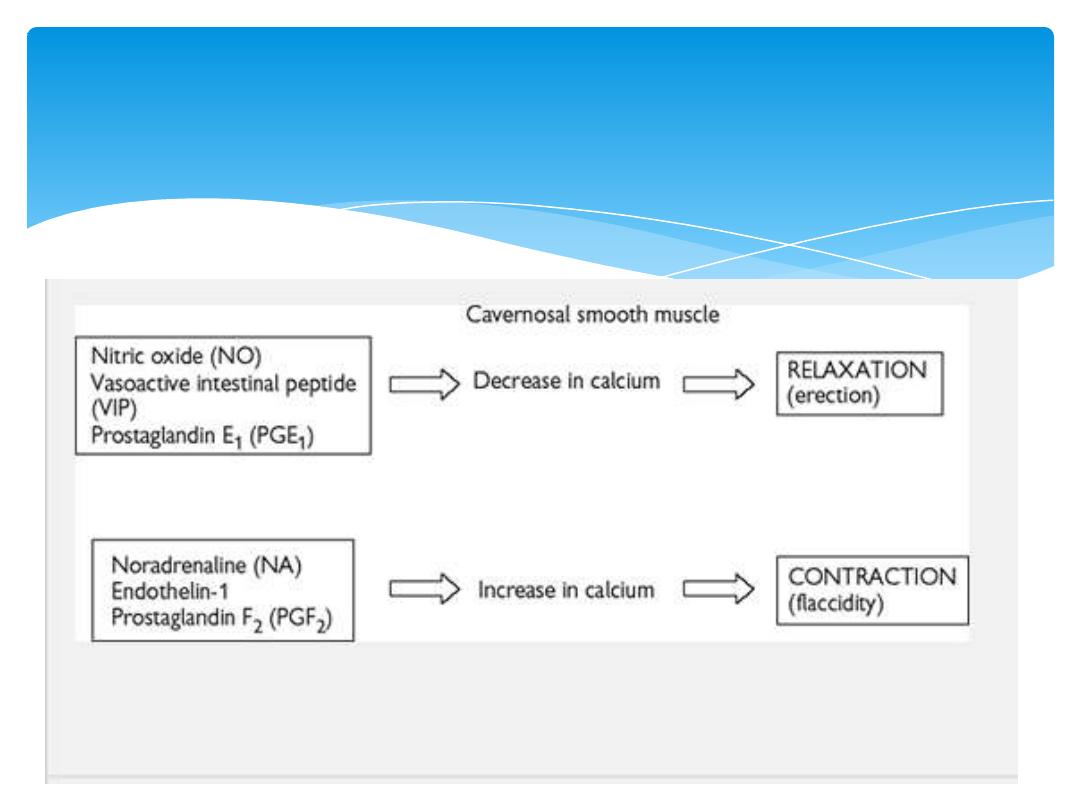
Factors influencing cavernosal
smooth muscle
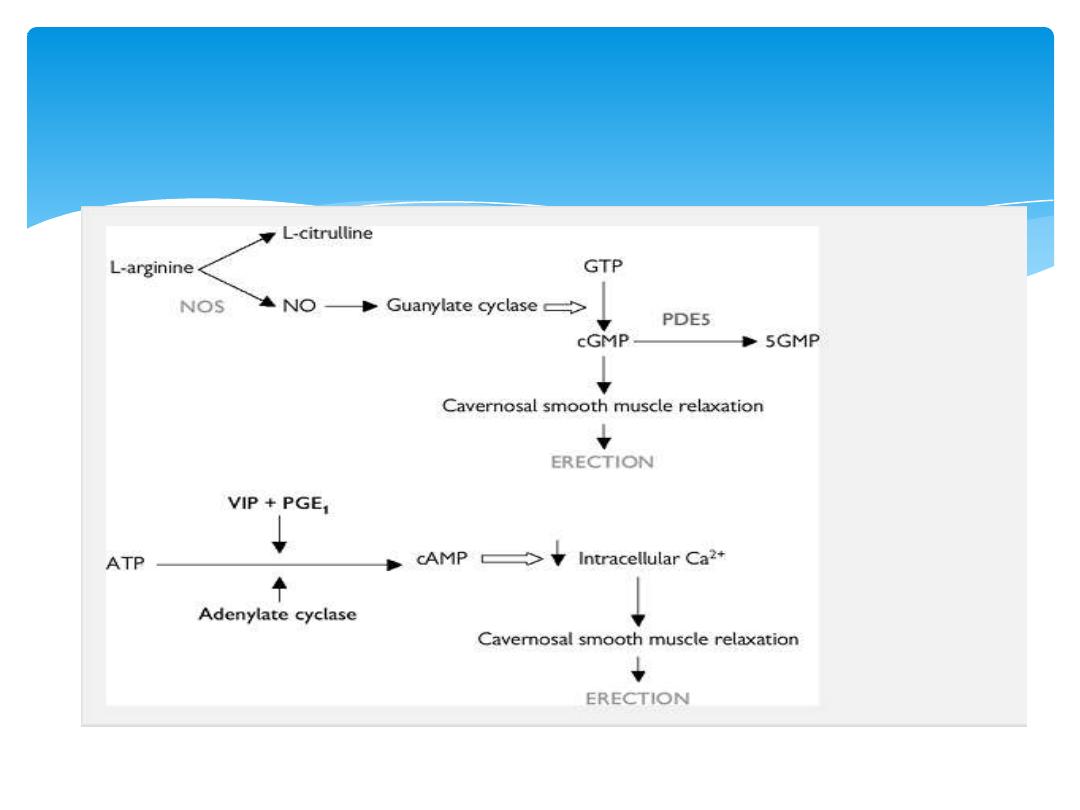
Secondary messenger pathways
involved in erection

Premature (rapid) ejaculation: persistent or
recurrent occurrence of ejaculation with minimal sexual
stimulation
Retarded ejaculation: Is undue delay in reaching a climax
during sexual activity.
Retrograde ejaculation: backflow of semen
into the bladder during ejaculation owing to an incompetent
bladder neck mechanism.
Anorgasmia:is the inability to achieve an orgasm during
conscious sexual activity
MALE SEXUAL DYSFUNCTION
is the inability to attain or maintain a penile erection sufficient for
sexual intercourse , may involve also problems with emission,
ejaculation or orgasm
.

I
nflammatory Prostatitis
M
echanical Peyronie's disease
P
sychological Depression; anxiety; relationship difficulties; lack of
attraction; stress
O
cclusive vascular factors Arteriogenic: hypertension; smoking;
hyperlipidaemia; diabetes mellitus; peripheral vascular disease
Venogenic: impairment of veno-occlusive mechanism (due to anatomical
or degenerative changes)
T
rauma Pelvic fracture; spinal cord injury; penile trauma
E
xtra factors Iatrogenic: pelvic surgery; prostatectomy
N
eurogenic
CNS: multiple sclerosis (MS); Parkinson's disease; multi-system atrophy;
tumour
Spinal cord: spina bifida; MS; syringomyelia; tumour
PNS: pelvic surgery or radiotherapy; peripheral neuropathy (diabetes,
alcohol-related
Aetiology

C
hemical
Antihypertensives (beta-blockers, thiazides, ACE
inhibitors)
Anti-arrhythmics (amiodarone)
Antidepressants (tricyclics, MAOIs, SSRIs)
Anxiolytics (benzodiazepine)
Anti-androgens (finasteride, cyproterone acetate)
LHRH analogues
Anticonvulsants (phenytoin, carbamazepine)
Anti-Parkinson drugs (levodopa)
Statins (atorvastatin)
Alcohol
E
ndocrine Hypogonadism; hyperprolactinaemia; hypo
and hyperthyroidism; diabetes mellitus

Diagnosis
History
Sexual: onset of ED (sudden or gradual); duration of problem;
presence of erections (nocturnal, early morning, spontaneous);
ability to maintain erections (early collapse, not fully rigid); loss
of libido; relationship issues (frequency of intercourse and
sexual desire, relationship problems).
Medical and surgical: hypertension; cardiac disease; peripheral
vascular disease; diabetes mellitus; endocrine or neurological
disorders; pelvic surgery, radiotherapy, or trauma (damaging
innervation and blood supply to the pelvis and penis).
Drugs: enquire about current medications and ED treatments
already tried (and outcome).
Social: smoking, alcohol consumption.
An organic cause is more likely with gradual onset (unless
associated with an obvious cause such as surgery, where onset is
acute); loss of spontaneous erections; intact libido and
ejaculatory function; existing medical risk factors; and older age
groups. The International Index of Erectile Function (IIEF) or ED
intensity scale can be used to quantify severity.

Examination
Full physical examination (CVS, abdomen,
neurological); digital rectal examination to assess
prostate; external genitalia assessment to document
foreskin phimosis and penile lesions (Peyronie's
plaques); confirm presence, size, and location of
testicles. The bulbocavernosus reflex can be
performed to test integrity of spinal segments S2–4
(squeezing the glans causes anal sphincter and
bulbocavernosal muscle contraction).
Investigation
Blood tests: U&E; fasting glucose; PSA; serum
testosterone; sex hormone binding globulin; LH/FSH;
prolactin; thyroid function test; fasting lipid profile.

PSYCHOLOGICAL EVALUATION
Nocturnal penile tumescence and rigidity testing
Useful for diagnosing psychogenic ED
Penile Duplex ultrasonography
Penile arteriography
Cavernosography

Treatment Of Impotence
1.Lifestyle Changes
* Regular exercise, a healthy diet, smoking cessation,
and limiting use of alcohol can reduce the risk of ED
* Perineal compression on penile arteries from long-
distance cycling may also represent a modifiable risk
factor for ED. Changing the bicycle seat or riding
practices will often improve erectile function

2. Changing Medications
When a patient complains of sexual dysfunction after taking
a particular medication, it is important in many situations,
changing the medication to a different class of agent
Antihypertensive agents
alpha-adrenoceptorantagonists, calcium channel blockers, and
angiotensin-converting enzyme (ACE)-inhibitors may reverse
ED in some patients
.
antidepressants
may lead to sexual dysfunction benefit from
watchful waiting, substitution (bupropion, nefazodone,
buspirone, mirtazapine), drug holidays, selective serotonin
reuptake inhibitor (SSRI) , dosage reduction.

3. Psychosexual therapy
Aims to understand and address underlying psychological issues, and provides
information and treatment in the form of sex education, improving partner
communication skills, cognitive therapy, and behavioural therapy
(programmed re-learning of couple's sexual relationship).
4. Oral medication
Phosphodiesterase type-5 (PDE5) inhibitors:
sildenafil (Viagra);
tadalafil (Cialis); vardenafil (Levitra). PDE5 inhibitors enhance
cavernosal smooth muscle relaxation and erection by blocking the
breakdown of cGMP. Sexual stimulus is still required to initiate events.
Side-effects: headache; flushing; visual disturbance. Contraindications:
patients taking nitrates; recent myocardial infarction; recent stroke;
hypotension; unstable angina.
Dopamine receptor agonist: apomorphine . Apomorphine is
administered sublingually, and acts centrally on dopaminergic
receptors in the paraventricular nucleus of the hypothalamus to
enhance and co-ordinate the effect of sexual stimuli.

5. Androgen replacement therapy
testosterone replacement is indicated for
hypogonadism. It is available in oral, intramuscular,
pellet, patch, and gel forms. In older men, it is
recommended that PSA is checked before and during
treatment.
6. Intraurethral therapy
alprostadil (MUSE). Synthetic prostaglandin E1 (PGE1)
pellet administered into the urethra via a specialized
applicator. Once inserted, the penis is gently rolled to
encourage the pellet to dissolve into the urethral
mucosa, from where it enters the corpora. Side-effects:
penile pain; priapism; local reactions.

7.
Intracavernosal therapy
alprostadil/Caverjet (synthetic PGE1); papaverine
(smooth muscle relaxant) آ
± phentolamine (alpha-
adrenergic antagonist). Training of technique and first
dose is given by health professional. Needle is inserted
at right angles into the corpus cavernosum on the
lateral aspects of mid-penile shaft. Adverse effects:
pain; priapism; haematoma
8. Vacuum erection device.
9. Penile prosthesis

THE END
THANKS
