Infertility
Dr Hasanain Farhan

Male reproductive physiology
• Hypothalamic pituitary testicular axis
The hypothalamus secretes luteinizing hormone-
releasing hormone (LHRH), also known as
gonadotrophin-releasing hormone (GnRH). This
causes pulsatile release of anterior pituitary
gonadotrophins, called follicle stimulating hormone
(FSH) and luteinizing hormone (LH), which act on
the testis. FSH stimulates the seminiferous tubules
to secrete inhibin and produce sperm; LH acts on
Leydig cells to produce testosterone
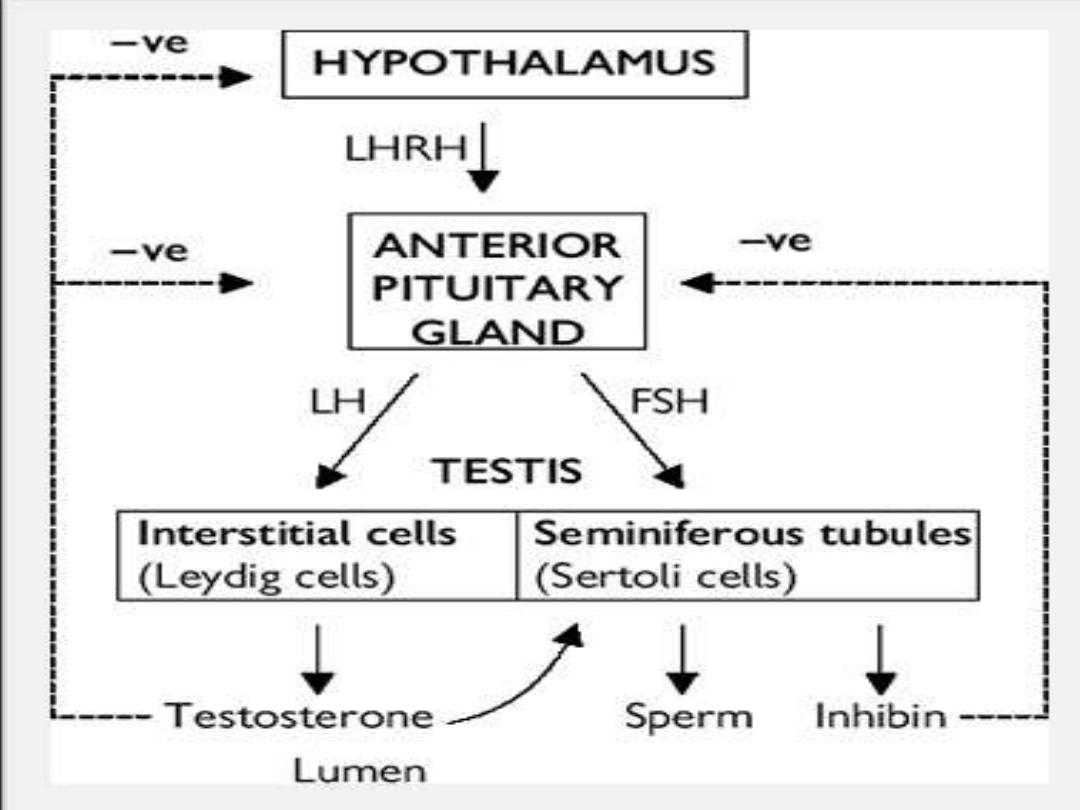

Testosterone
• is secreted by the interstitial Leydig cells. It
promotes development of the male
reproductive system and secondary sexual
characteristics. At androgen-responsive target
tissues, testosterone is converted into a
potent androgen, dihydrotestosterone, by
intracellular 5-alfha reductase.

Spermatogenesis
• Primordial germ cells divide to form primary
spermatocytes. These undergo a first meiotic
division to create secondary spermatocytes
(46 chromosomes), followed by a second
meiotic division to form spermatids (23
chromosomes). Finally, these differentiate into
spermatozoa. This process takes 70 days. The
non-motile spermatozoa leave the
seminiferous tubules and pass to the
epididymis, for storage and maturation (until
ejaculation).
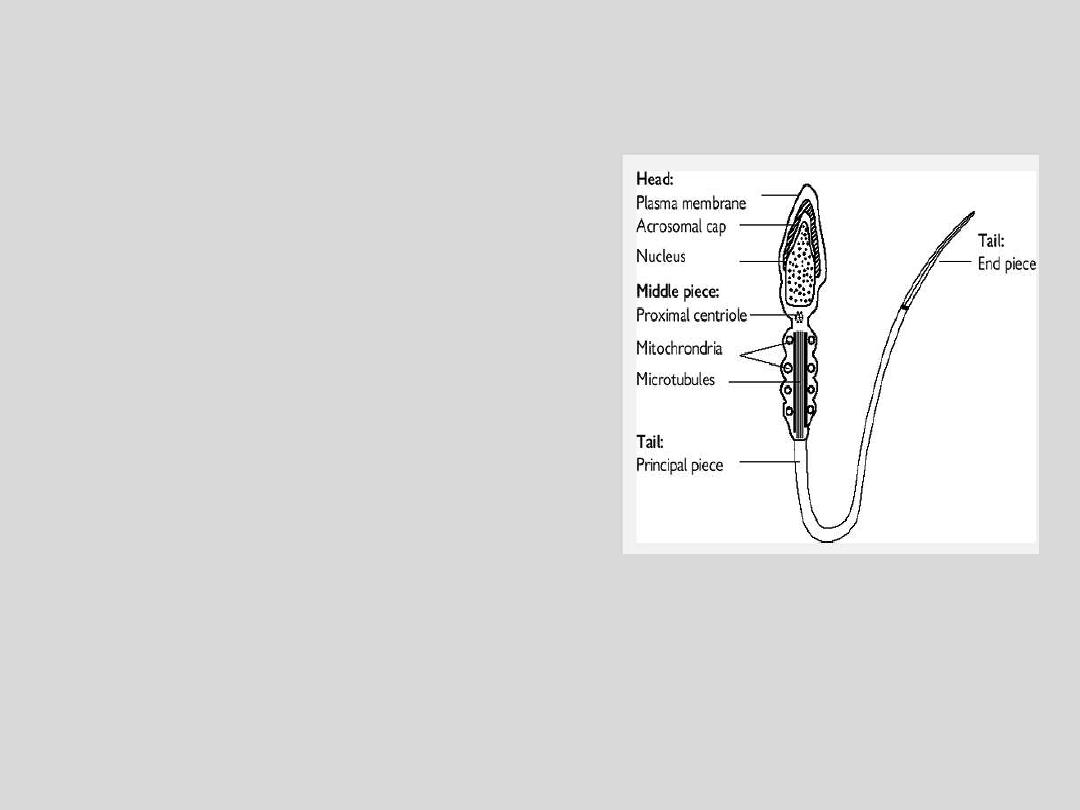
Mature sperm
The head is composed of a nucleus covered by
an acrosome cap, containing vesicles filled
with lytic enzymes. The middle piece contains
mitochondria and contractile filaments, which
extend into the tail to aid motility. After
deposition at the cervix, sperm penetrate
cervical mucus and travel through the uterus
to the site of fertilization in the fallopian tube,
during which time they undergo functional
maturation (capacitation). Sperm start to
penetrate the oocyte, and bind to the zona
pellucida. triggering hyperactivated motility
and the acrosomal reaction, leading to enzyme
release, penetration into the cytoplasm of the
oocyte, fusion, and fertilization.

Definition of infertility
• Failure of conception after at least 12 months of unprotected
intercourse. The chance of a normal couple conceiving is
estimated at 20 to 25% per month, 75% by 6 months, and 90%
at 1 year.
• Up to 50% of infertility is due to male factors.

CAUSES OF MALE INFERTILITY
A:PRETESTICULAR CAUSES
:-
1.Hypothalamic
•
A.
GONADOTROPIN DEFICIENCY
EX:KALLMANN SYNDROME:there is a disturbance of neuronal migration from the
olfactory placode during embryonic development. The clinical features include
anosmia, facial asymmetry, microphallus, and cryptorchidism.
•
B
. ISOLATED LH DEFICIENCY.
•
C.
ISOLATED FSH DEFICIENCY
.
•
D.
CONGENITAL HYPOGONADOTROPIC SYNDROMES

2.Pituitary Disease
A
. PITUITARY INSUFFICIENCY:
Pituitary insufficiency may result from tumors,
infarcts,surgery, radiation, or infiltrative and granulomatous processes.In sickle cell
anemia, pituitary and testicular microinfarcts from sickling of red blood cells are
suspected.
B
. HYPERPROLACTINEMIA:
the most common and important cause of
hyperprolactinemia is a prolactin secreting pituitary adenoma. Elevated prolactin
usually results in decreased FSH, LH, and testosterone levels and causes infertility.
Associated symptoms include loss of libido, impotence, galactorrhea, and
gynecomastia.

3. EXOGENOUS OR ENDOGENOUS HORMONES
•
A.
Estrogens
—An excess of sex steroids, either estrogens or androgens, can cause
male infertility due to an imbalance in the testosterone-estrogen ratio. Hepatic
cirrhosis increases endogenous estrogens because of augmented aromatase
activity within the diseased liver. Likewise, excessive obesity may be associated
with testosterone estrogen imbalance owing to increased peripheral aromatase
activity.
•
B.
Androgens
—An excess of androgens can suppress pituitary gonadotropin
secretion and lead to secondary testis failure. The use of exogenous androgenic
steroids (anabolic steroids) by as many as 15% of high school athletes.
•
C.
Glucocorticoids
—Exposure to excess glucocorticoids either endogenously or
exogenously can result in decreased spermatogenesis. Elevated plasma cortisone
levels depress LH secretion and induce secondary testis failure.
•
D.
Hyper- and hypothyroidism
—Abnormally high or low levels of serum thyroid
hormone affect spermatogenesis at the level of both the pituitary and testis
•
E.
Growth hormone
—There is emerging evidence that growth hormone may play a
role in male infertility.

B:TESTICULAR CAUSES :-
1.Chromosomal Causes
EX:Klinefelter
syndrome is the most common genetic reason for azoospermia.
It has a classic triad: small firm testes; gynecomastia; and azoospermia. This
syndrome may present with increased likelihood of extragonadal germ cell
tumors, and breast cancer (20-fold higher than in normal males).
2.Gonadotoxins
A.
RADIATION
: The effects of radiotherapy on sperm production are well
described.
B.
DRUGS
Ketoconazole,spironolactone, and alcohol inhibit testosterone synthesis,
cimetidine is an androgen antagonist.
Recreational drugs such as marijuana, heroin are associated with lower
testosterone levels.
Certain pesticides have estrogen-like activity.
Cancer chemotherapy
3.Systemic Disease
A.
RENAL FAILURE
B.
LIVER CIRHOSIS
C.
SICKLE CELL DISEASE

4.Defective Androgen Activity
:Peripheral resistance to androgens occurs
with 2 basic defects:
(1) a deficiency of androgen production through the absence of 5-alpha-reductase
(2) a deficiency in the androgen receptor.
5.Testis Injury
•
A.
ORCHITIS
:Inflammation of testis tissue is most commonly due to bacterial
infection, termed epididymo-orchitis. Viral infections also occur in the testis in the
form of mumps orchitis.
•
B.
TORSION
:Ischemic injury to the testis secondary to twisting of the testis on the
spermatic cord pedicle .
•
C.
TRAUMA
: Because of the peculiar immunologic status of the testis in the body
(ie, it is an immunologically privileged site), trauma to the testis can invoke an
abnormal immune response in addition to atrophy resulting from injury. Both may
contribute to infertility. Trauma to the testis that results in fracture of the testis
tunica albugineal layer.
6.Cryptorchidism.
7. Varicocele:
is defined as dilated and tortuous veins within
the pampiniform plexus of scrotal veins.(40% of male infertility)
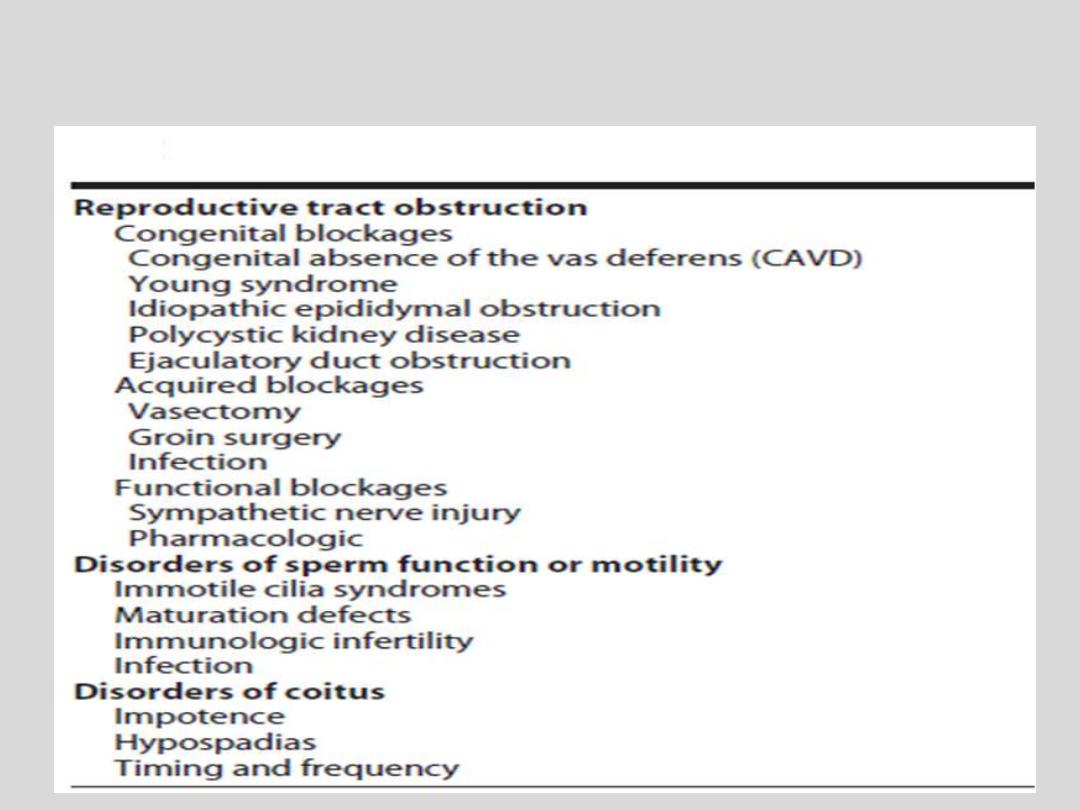
C:POSTTESTICULAR CAUSES:-

Evaluation of Male infertility
History
• Sexual: duration of problem; frequency and timing of intercourse;
previous successful conceptions; previous birth control; erectile or
ejaculatory dysfunction.
• Developmental: age at puberty; history of cryptorchidism;
gynaecomastia.
• Medical and surgical: detailed assessment for risk factors—recent
febrile illness; post-pubertal mumps orchitis; varicocele; testicular
torsion, trauma, or tumour; sexually transmitted diseases;
genitourinary surgery; radiotherapy; respiratory diseases associated
with ciliary dysfunction; diabetes.
• Drugs and environmental: previous chemotherapy; exposure to
substances which impair spermatogenesis or erectile function;
alcohol consumption; smoking habits; hot baths.
• Family: hypogonadism; cryptorchidism

Examination
• Perform a full assessment of all systems, with
attention to general appearance (evidence of
secondary sexual development; signs of
hypogonadism; gynaecomastia). Urogenital
examination should include assessment of the
penis (Peyronie's plaque, phimosis, hypospadias);
measurement of testicular consistency,
tenderness, and volume with a Prader
orchidometer (normal >20ml; varies with race);
palpate epididymis (tenderness, swelling) and
spermatic cord (vas deferens present or absent,
varicocele); digital rectal examination of prostate
Investigation
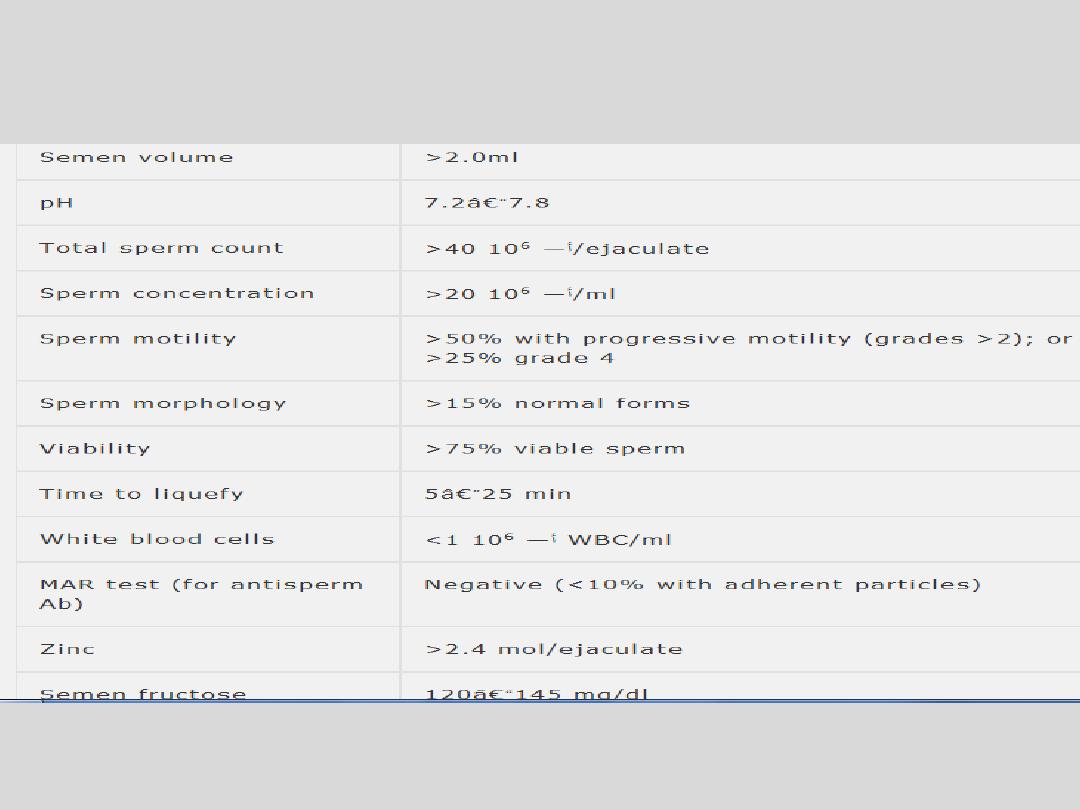
seminal fluid analysis (SFA)
Basic investigations:
Hormonal assessment :
FSH, LH, S.testosteron, S.estrogen, S.prolactine, thyroid hormon

Imaging
• Scrotal ultrasound scan
is used to confirm a varicocele
and assess testicular abnormalities.
• Transrectal ultrasound scan
is indicated for low
ejaculate volumes, to investigate seminal vesicle
obstruction (>1.5cm width) or absence and ejaculatory
duct obstruction (>2.3mm).
• Vasography
Vas deferens is punctured at the level of
the scrotum and injected with contrast. A normal test
shows the passage of contrast along the vas deferens,
seminal vesicles, ejaculatory duct, and into the bladder,
which rules out obstruction.
• Venography
used to diagnose and treat varicoceles
(embolization).

Special investigations
1.
Chromosome analysis :Indicated for clinical suspicion of an abnormalit
(azoospermia or oligospermia, small atrophic testes with ↑ FSH).
2.
Testicular biopsy:Performed for azoospermic patients, to differentiate
between idiopathic and obstructive causes. May also be used for sperm
retrieval.
3.
Sperm function tests which include:
•
Post coital test: cervical mucus is taken just before ovulation, and within 8
hours of intercourse, and microscopy performed. Normal results shows
>10 sperm per high-powered field, the majority demonstrating
progressive motility. Abnormal results indicate inappropriate timing of the
test; cervical mucus antisperm antibodies; abnormal semen;
inappropriately performed coitus.
•
Sperm penetration test: a sample of semen is placed directly onto pre-
ovulatory cervical mucus on a slide and the penetrative ability of
spermatozoa observed.
•
Sperm-cervical mucus test: a specimen of semen (control), and one mixed
with cervical mucus are placed separately on a slide, and observed for 30
minutes. More than 25% exhibiting jerking movements in the mixed
sample (but not the control) is a positive test for antisperm antibodies.

Treatment options for male infertility
• General
Modification of life style factors (reduce alcohol consumption; avoid hot
baths).
• Medical treatment
Correct any reversible causative factors :
1.Hormonal
Secondary hypogonadism (pituitary intact) may respond to human
chorionic gonadotrophin (hCG) 2000IU subcutaneously 3 times a week,
which stimulates an increase in testosterone and testicular size.
Alternatively, pulsatile LHRH can be administered subcutaneously via a
minipump.
Testosterone deficiency requires testosterone replacement therapy.
Hyperprolactinaemia is treated with dopamine agonists.
2. Emperic medical therapy
a.Anti-oestrogens (clomiphene citrate ): are often used empirically to
increase LHRH, which stimulates endogenous gonadotrophin secretion.
b.Antioxidant: Vitamine E improve sperm function, zinc and folic acid
increase sperm concentration

3. Correct erectile and ejaculatory dysfunction
4. Antisperm antibodies
Corticosteroids have been used, but assisted conception methods are
usually required.
5.Antibioltics to treat any infection
• Surgical treatment
1.Genital tract obstruction
.
Epididymal obstruction can be overcome by microsurgical anastomosis
between the epididymal tubule and vas (epididymovasovasostomy).
.Vas deferens obstruction is treated by microsurgical re-anastomosis of
ends of the vas, and is used for vasectomy reversal.
.Ejaculatory duct obstruction requires transurethral resection of the ducts.
2.Varicocele
Repaired by embolization or open/laparoscopic surgical ligation
3. Orchidopexy
4.Pituitary ablation

•
Assisted reproductive techniques (ART)
• Intrauterine insemination (IUI) Following ovarian
stimulation, sperm are placed directly into the uterus.
• In vitro fertilization (IVF) Controlled ovarian
stimulation produces oocytes which are then retrieved
under transvaginal USS-guidance. Oocytes and sperm
are placed in a Petri dish for fertilization to occur.
Embryos are transferred to the uterine cavity.
Pregnancy rates are 20-30% per cycle.
• Intracytoplasmic Sperm injection (ICSI) A single
spermatozoon is injected directly into the oocyte
cytoplasm (through the intact zona pellucida).
Pregnancy rates are 15-22% per cycle.