Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Epidemiology
Sex:
Metabolic and idiopathic M>F
Infection F>M
Age:
Metabolic and idiopathic, 3
rd
and 4
th
decade of life
Infection 5
th
decade
Occupation: sedentary work, hot climate
Diet:
Fiber rich diet decrease the risk
Refined CHO and animal pr. Increase the risk
Family history: double risk (15% vs. 30%)
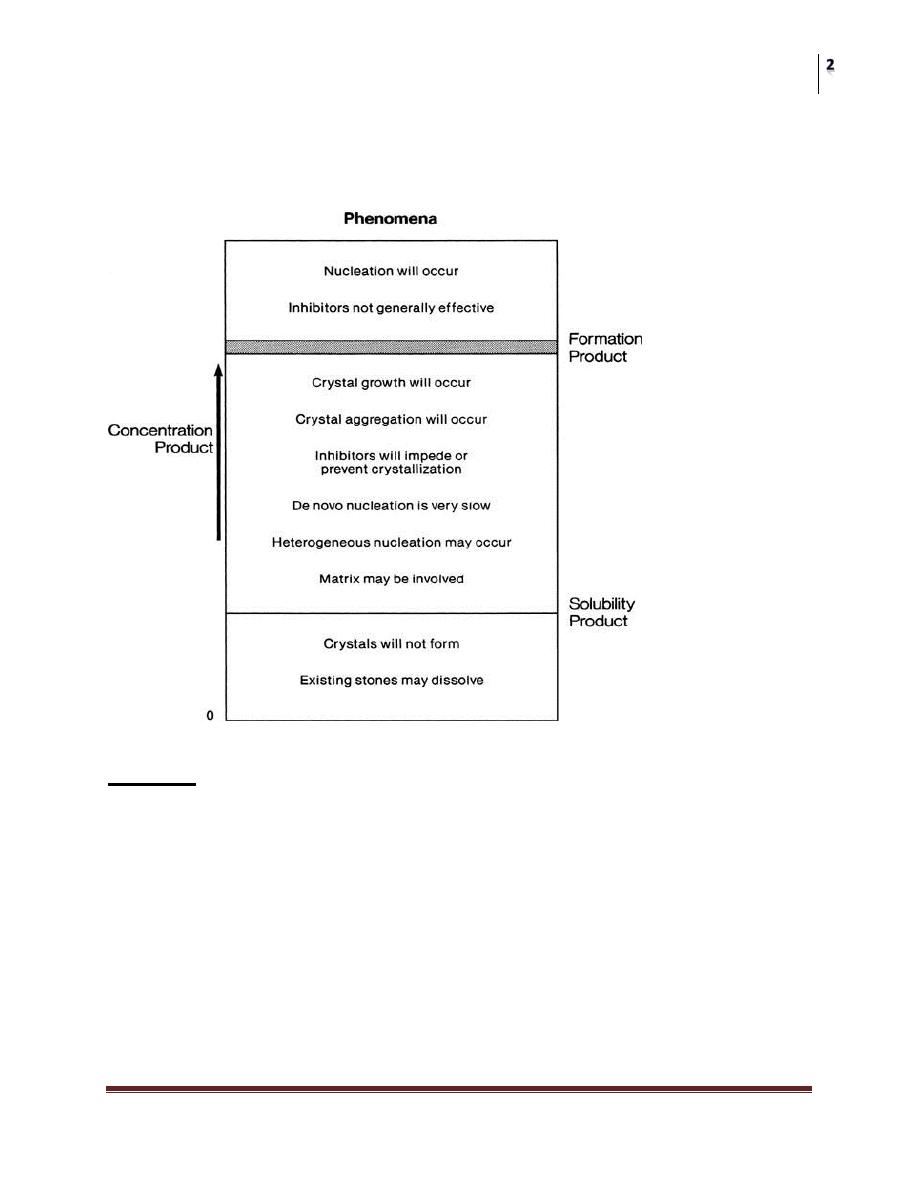
Stone formation requires SUPERSATURATION
Supersaturation depends on
Urinary PH
Ionic strength
Solute conc.
complexation
Chemical Terms
• concentration product: multiplying 2 ion conc.
• Solubility product: The point above which ions are metastable and capable
of heterogenous nucleation.
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
• Formation product: the level above which the ions are unstable and capable
of homogenous nucleation.
• Calcification: metastatic vs dystrophic
Causes
• Idiopathic: most common cause
• Abnormalities of urine:
Congenital: primary hyperoxalurea, cystinurea
Acquired: dehydration, dietary hypercalciuria
• Abnormalities of the urinary tract:
Cong: PUJ obstruction, ureteroceles, diverticuli
Acquired: postoperative or traumatic fibrosis
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Theories Of Stone Formation
Nucleation theory: stones originate from crystals or foreign bodies immersed
in supersaturated urine
Crystals inhibitors theory: stones are formed due to absence or low conc. of
stone inhibitors e.g citrate
Stone Components
A stone consists of crystalline material arranged in layers on an organic scaffold
A. Crystal component: >90%
Crystal formation occurs in 3 steps: nucleation, growth, and
aggregation
Nucleation can be either homogenous or hetergenous
B. Matrix component:< 10%
Protiens, hexose, and hexosamines
Matrix role???
Matrix stone:
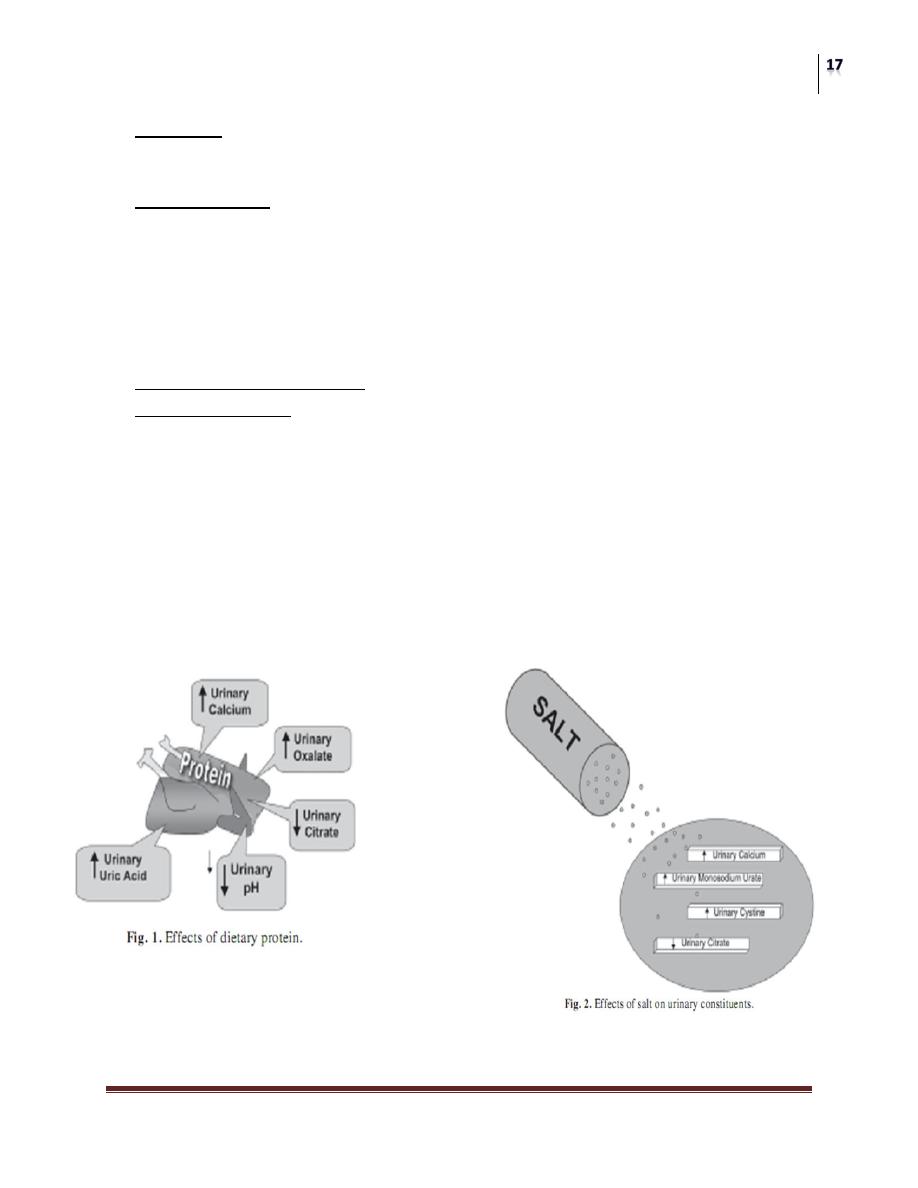
Risk Factors
Anatomical abnormalities
Infection: urease producers
Hormonal imbalance: PTH
Environmental factors
Diet: decreased fluid intake, meat,multivitamins
Metabolic state of the person which influenced by the genetic background
Drugs: antacids, CS, chemotherapy
Low mobility: bone demeniralization
Family history: cystineuria, RTA
Bowel inflam. conditions and resection: hyperoxaluria
Urinary Ions
Ca
+2
: it is the major ion present in urinary stones.
50% of plasma ca
+2
is ionized and filterable, it’s reabsorbed by PT&DT, 2%
excreted.
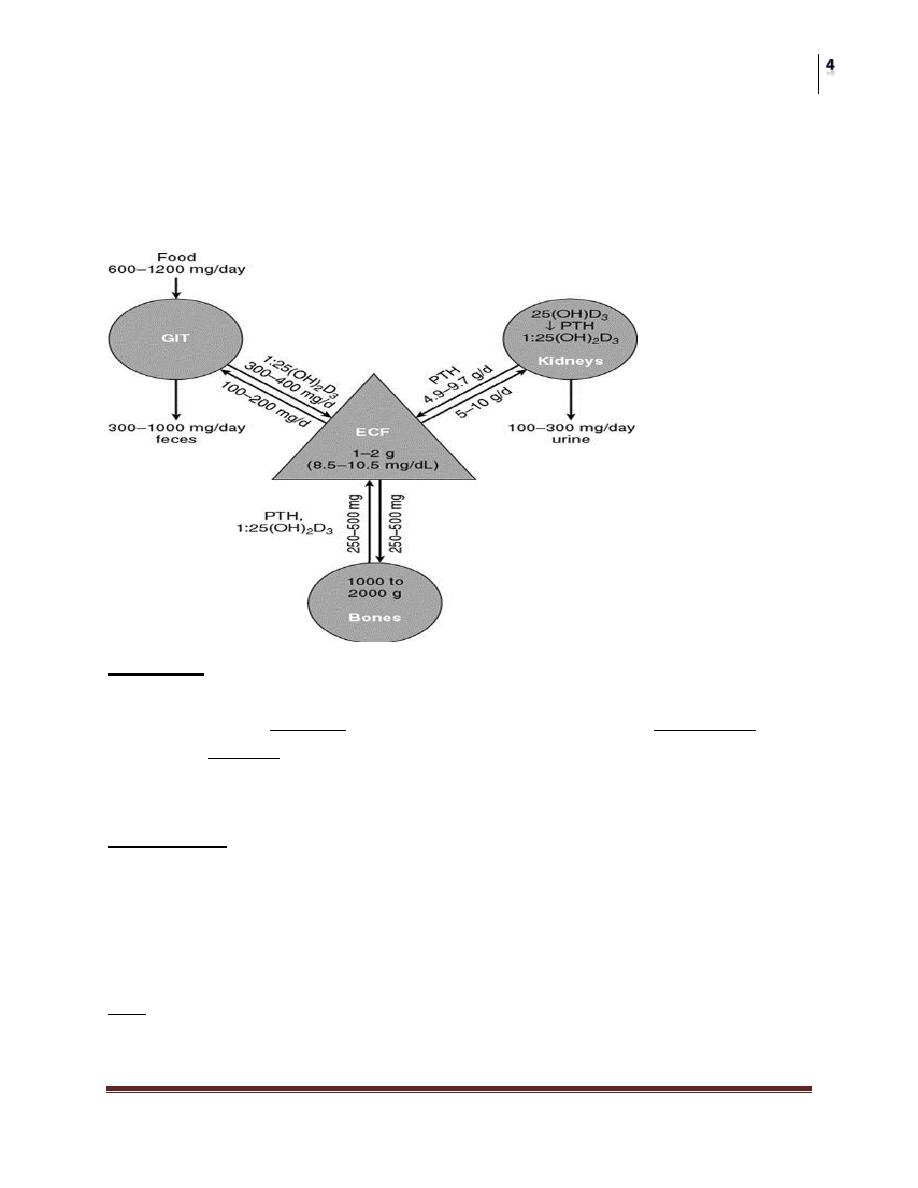
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Normal urinary ca+2 in adults is ≤4mg/kg/day.
Diuretics decrease u. ca
+2
Increased monosodium urate increase ca
+2
–oxalate
crystallization.
Acidic urine increase the crystallization also.
Oxalate:
85% is a metabolic by-product, while only 15% is dietary
IN BOWEL: either absorbed then exclusively excreted by PT, or metabolized by
bacteria, or complex and excreted in feces.
Normal level is less than 45 mg/day.
Phosphate:
is an important buffer that complexes with ca
+2
in urine
Part of MAP stone
Urinary excretion depends on dietary intake (meat), then
filtered by the glomerulus and re absorbed by PT under
influence of PTH
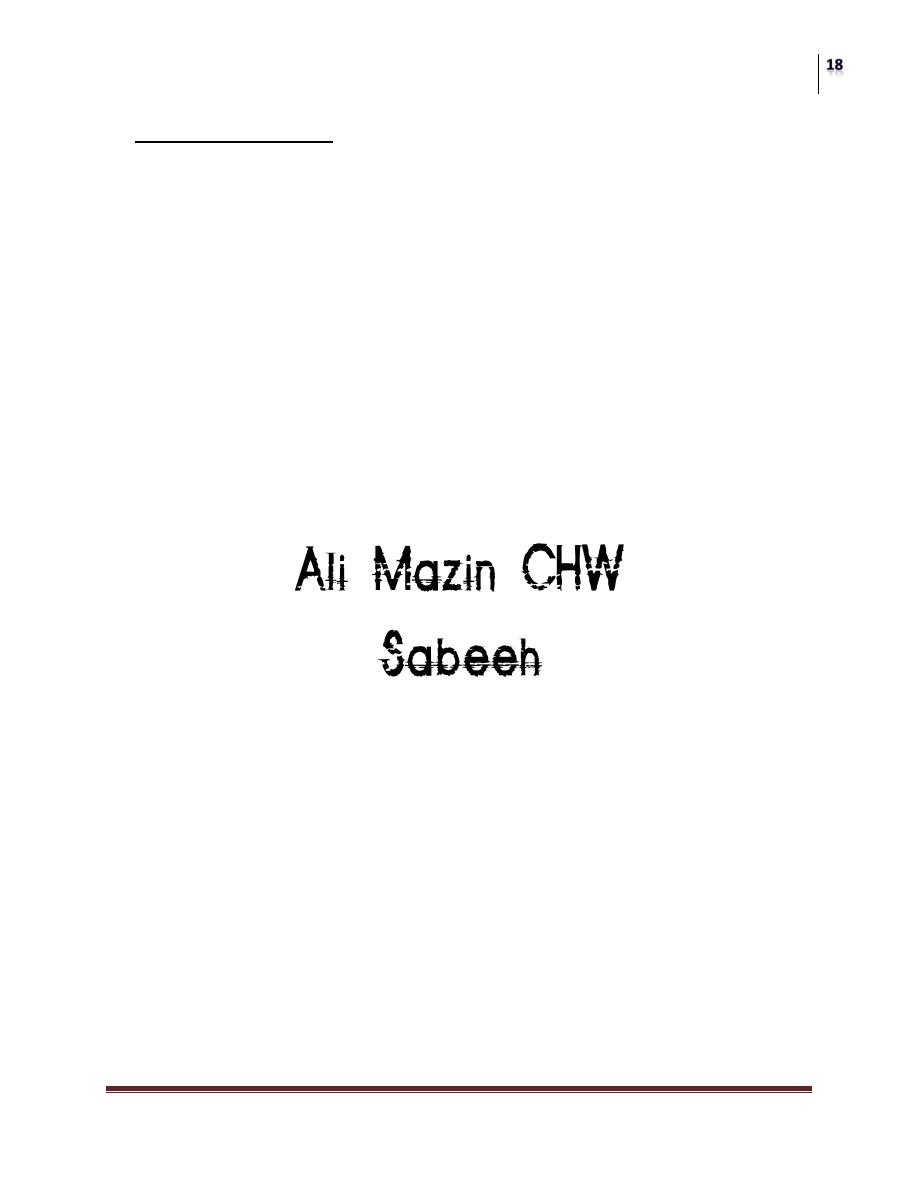
Na
+
: although it is not a major constituent of urinary stone, it plays a very
important role in the regulation of ca
+2
salts crystallization, a major increase in u.
Na
+
excretion will dramatically increase u. Ca
+2
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Uric acid: is a byproduct of purine metabolism, it’s Pka is 5.75, so its solubility
increases in alkaline urine
Citrate: is the major stone inhibitor in urine, its level in urine decreases in:
Metabolic acidosis
RTA type I
Chronic diarrhoea
Thiazide therapy
Hypokalemia
Esterogen lack in females
Other inhibitors:
Mg
Sulfate
Urinary proteins (Tamm-Horsfall pr.)
Pyrophosphate
Glycoseamineglycans
uropontine
Stone Varieties
Calcium stones (85%)
• Hypercalciuric
• Hyperoxaluric
• Hyperuricoseuric
• hypocitraturic
Non calcium stones (15%)
• Struvite “infection, MAP”
• Uric acid
• Cystine
• Xanthine
• Others: indinavir
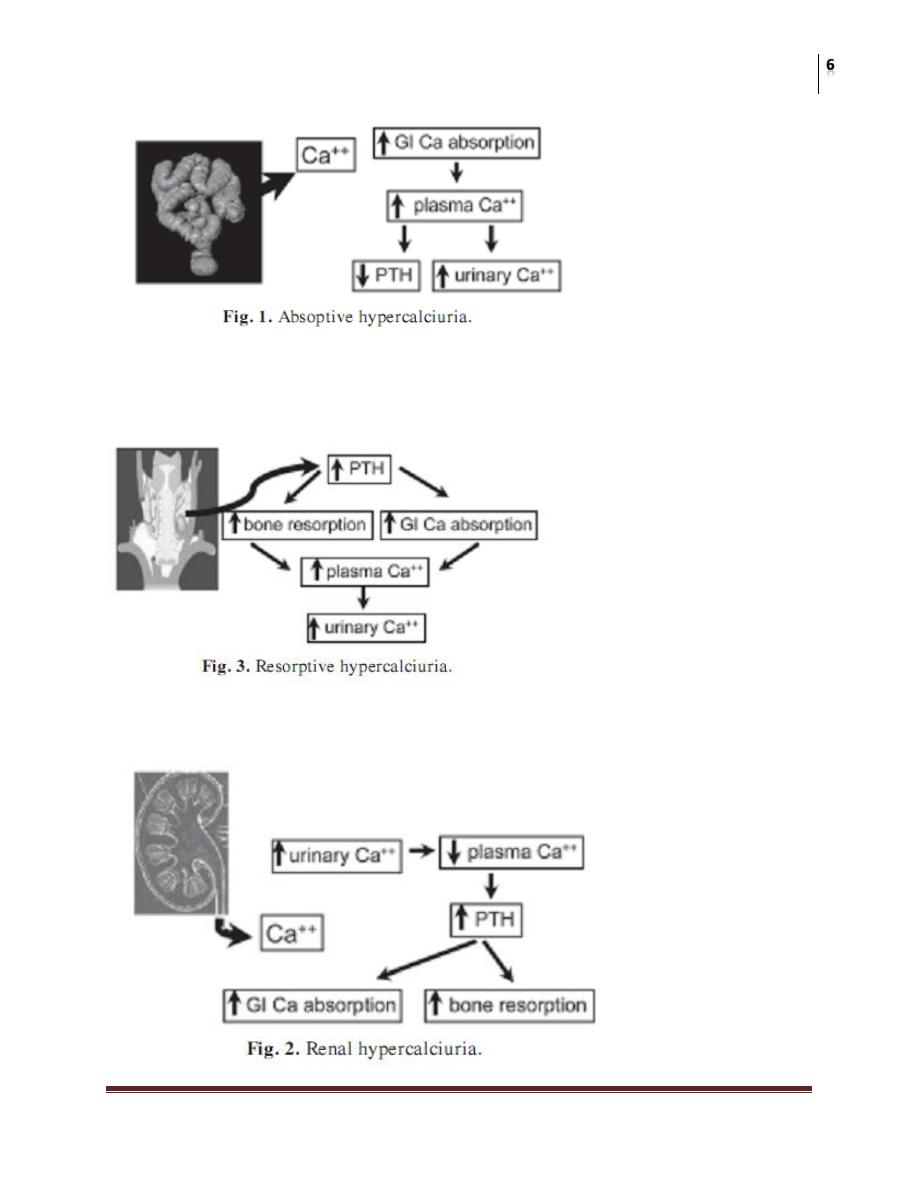
Hypercalciuria
Absorptive:
Diet independent /cellulose phosph. vs. thiazides
Diet dependent /mild and respond to dietary modif.
Renal phosphate leak /orthophosphate suppl.
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Resorptive hypercalciuria
Due to hyperparathyroidism
Renal induced hypercalciuria
Due to intrinsic renal tubular defect
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Hyperoxaluria
A. Primary hyperoxaluria: a rare AR disease, it is aggressive and ends in RF,
the definitive therapy by combined renal and liver transplantation, however
adequate hydration, oxalate restriction, and pyridoxine all will decrease
urinary excretion
B. Enteric hyperoxaluria: oxalate is poorly absorbed by intestine, but once
absorbed it is exclusively excreted in urine, causes of increased absorption
include:
• IBD, small bowel bypass, mal-absorption syndromes, low
dietary calcium, steatorrhoea, excessive ascorbic acid intake,
and accidental ethylene glycol ingestion
• Oxalate rich food
Hyperuricoseuria
• Due to either excessive oral purine intake, or excessive endogenous
production
• Monosodium urate absorbs and adsorbs urinary inhibitors and facilitates
heterogeneous nucleation
• Patients usually have elevated urinary uric acid and U.pH >5.5
• Treatment includes adequate hydration, urine alkalization, and allopurinol
Hypocitraturia
Citrate is the major stone inhibitor in urine
Causes of hypocitraturia are mentioned before
Metabolic acidosis
RTA type I
Chronic diarrhoea
Thiazide therapy
hypokalemia
Normal level: > 320 mg/24 hrs
Treatment: by potassium citrate suppl.
6-8 glasses of lemonade per day increase U. citrate by 150 mg/day
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Struvite Stones
Also called triple phosphate, or infection stones
Composed of MAP
It is formation requires the presence of urea splitting bacteria which
alkalinize urine and causes high conc. of bicarbonate and ammonium
These include: proteus, pseudomonads, klebsiella and staph.
E.coli is not a urease producer
MAP crystals ppt. only in high PH>7.2
Struvite stones (cont’d)
Incidence increases in patients with chronic cath, urinary diversion, S.C
injury, and bladder dysfunction
Presentation: usually as stag-horn, but can be in any form
On X-ray: faintly opaque due to poor mineralization and large protein matrix
Treatment: should include complete removal, with control of infection pre,
per and post operatively
Uric acid stones
5-10 % of all u. stones
Pure uric acid stones are radiolucent
Xanthine oxidase converts xanthine into uric acid
Urinary pH < 5.5
May be formed in patients with:
Hyperuricemia
Hyperuricoseuria
Chronic dehydration
Corner stones of treat included:
Good hydration
Urine alkalization
Allopurinol
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Cystine stones
1-2% of all stone types
Have faintly opaque ground glass appearance with smooth edges due to
presence of sulfur
AR inborn error of metabolism
There is abnormal renal tubular re-absorption of dibasic amino acids COLA
Its PKa is 8.1, so the more alkaline the urine the more cystine is soluble
May present as single, multiple, or staghorn
Medical therapy may dissolve or prevent stone recurrence by:
Adequate hydration
Urine alkalization
Cystine binding drugs as penicillamine, captopril, thiola, or
bucacillin
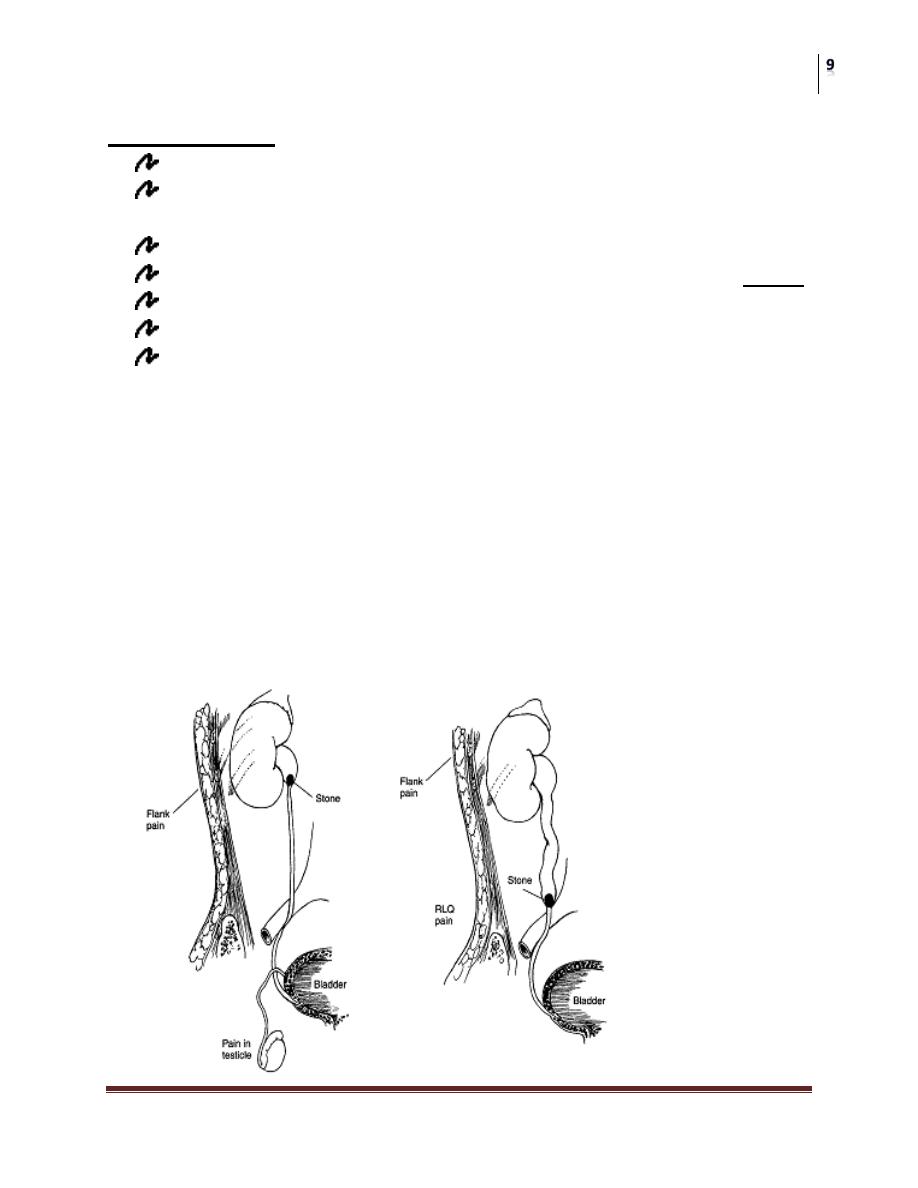
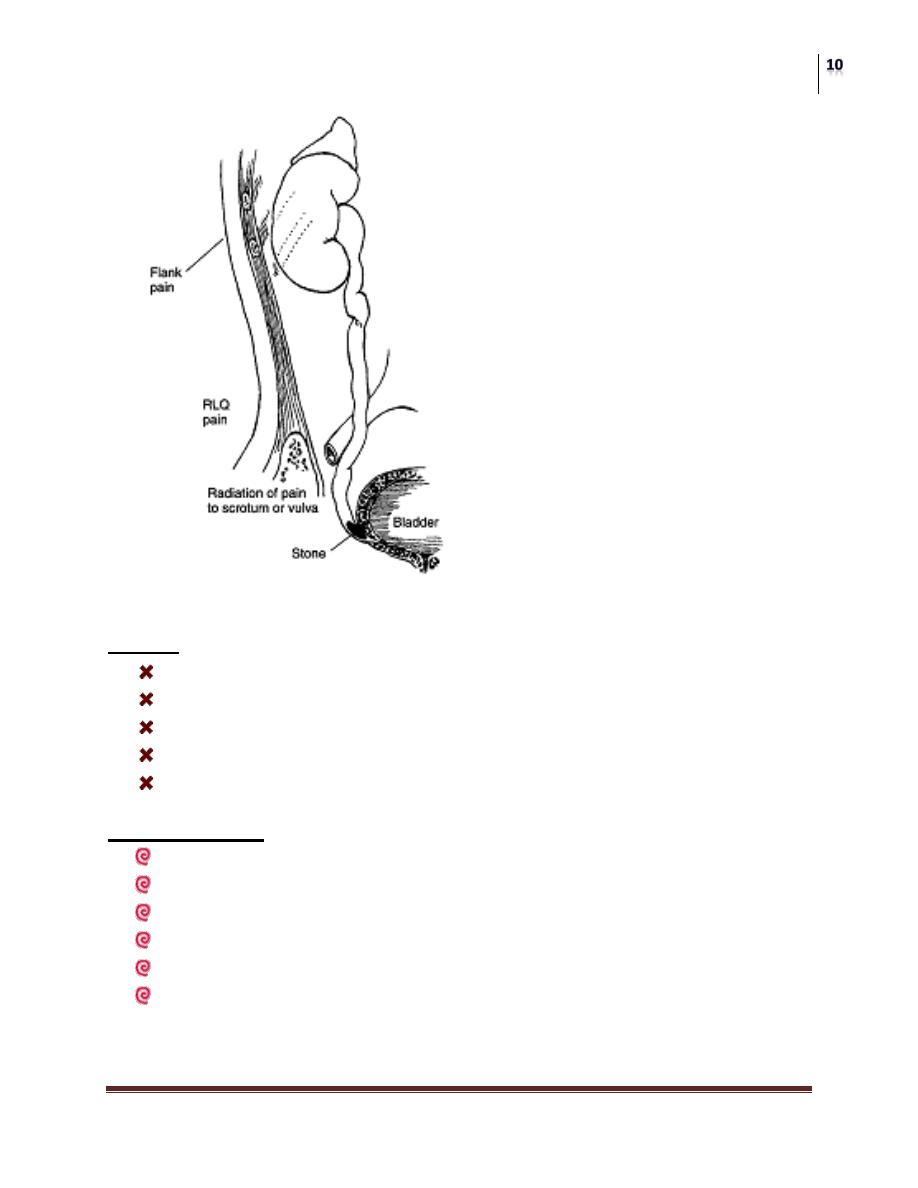
Sign and Symptoms
• Pain:
• Hematuria: microscopic in up to 90%
• Infection: affects pain perception, endotoxins and exotoxins affect ureteric
peristalsis, it may range from simple to frank pyonephrosis (emergency)
• Nausea and vomiting
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Signs:
Pain causes sweating, hypotension, tachypnoea and tachycardia
Obs,infection,and pyonephrosis cause high temp,rigor and sepsis
Renal angle tenderness
Bladder may be tender or with urine retention
Do full abd. exam and exclude other diff.diagnosis
Investigations:
GUE
Renal function
Abd. US
EXU
CT scan
Stone analysis and work up
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Treatment of renal stones
Decision depends on:
Stone size, site, and type
Renal function and anatomy
Patient clinical condition
Facility available
Patient’s and doctor’s preference
Indications for hospitalization
High-grade obstruction, (spec. stones >10 mm) will require early
intervention (stenting or PCN).
High fever (>38.5ºC) suggests pyelonephritis, I.V AB should be started
immediately.
Patients with uncontrollable pain requiring parenteral analgesics.
Patients with severe nausea and dehydration requiring intravenous fluids.
Patients with a single functioning kidney at risk of acute renal failure.
Modalities
Conservative observation:
Small calculi without obstruction need no urgent intervention, and have
great chance of spontaneous passage, specially if <7 mm.
Analgesia is the corner stone of treatment, the best is indomethasin supp.
(Keotrolac??).
Anti-emetics
AB if associated infection
Diuretics and antispasmodics are not preferred
Keep the patient well hydrated
Encourage normal movement
Indication for early intervention
High-grade urinary obstruction
Persistent infection despite antibiotics
Uncontrollable pain
Impairment of renal function
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
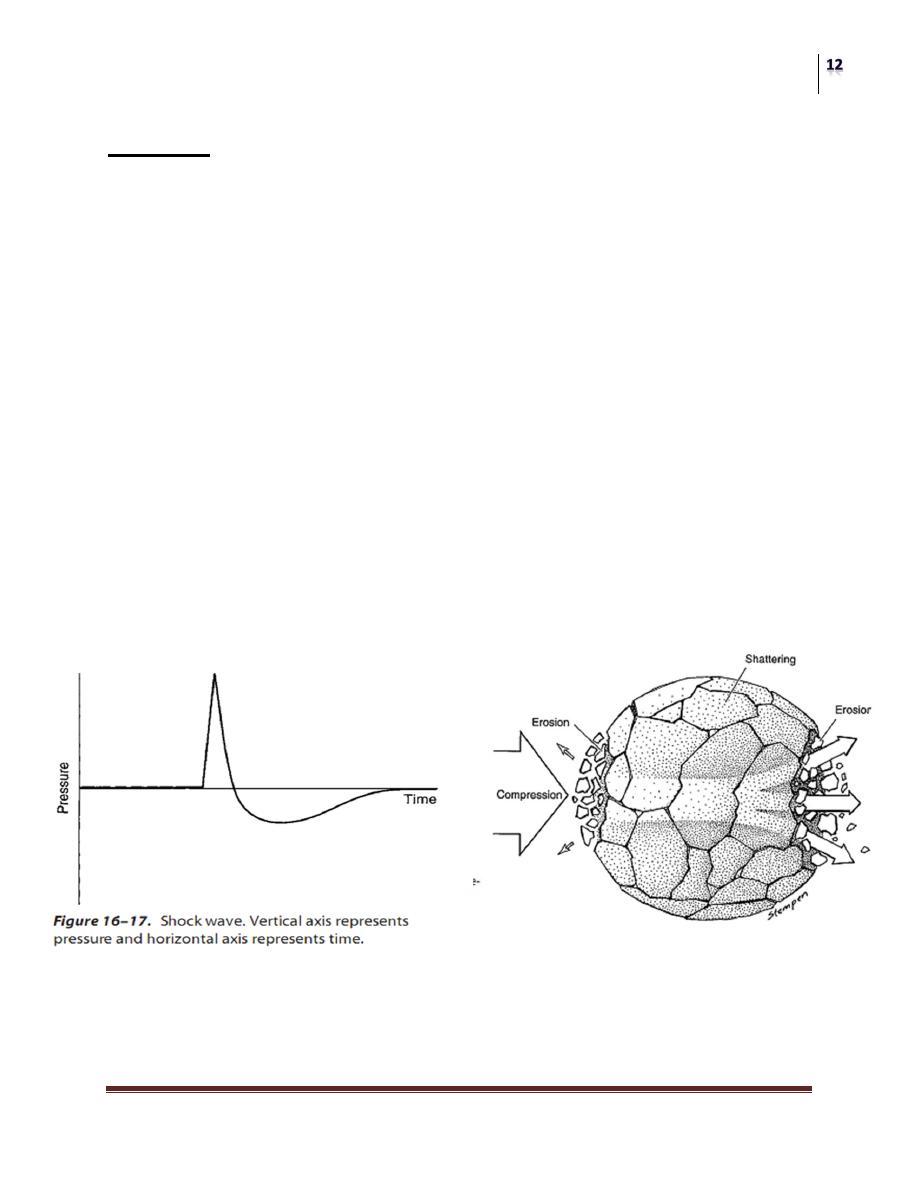
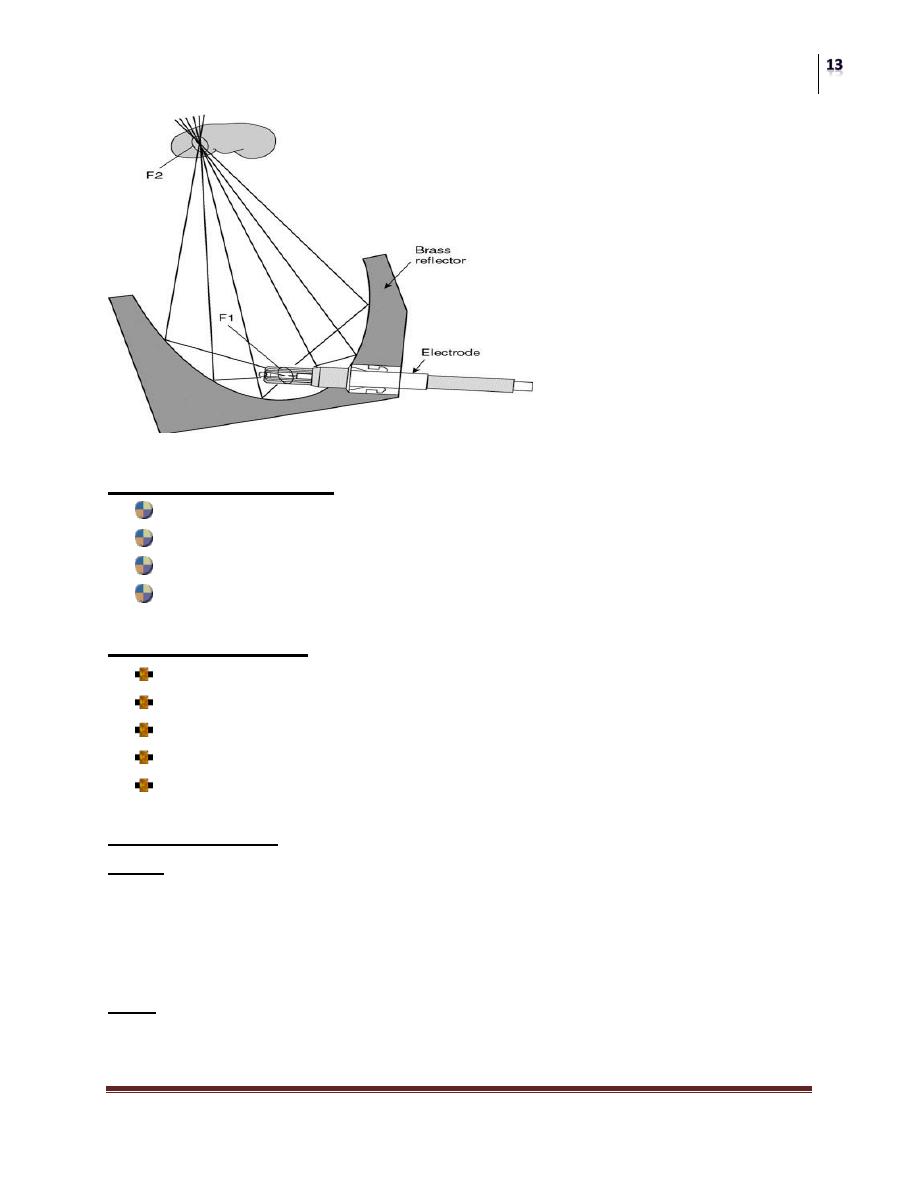
ESWL
• Has revolutionized the stone management
• Shock waves: unharmonic, with steep rise in pressure amplitude that results
in compressive forces.
• It includes:
Energy source: to create the shock waves
Coupling mechanism: transfer the energy into the human body
Localization technique: help localize the stone, either by US, or
flouroscopy
Shock wave sources
Supersonic emitters (point source of shock waves): releasing energy in a
confined space creating expanding plasma bubble that emits shock waves.
Finite amplitude emitters (surface source of shock waves)
Piezoceramic plates that elongate on electrical stimulation and
displace to generate the shock waves.
Electromagnetic membrane that displace on electrical
stimulation and generates the shock waves.
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Patient preparation:
EXU to exclude distal obstruction
GUE and urine culture
Bleeding profile
In some cases ureteric stent (single kidney or large stone burden)
Contraindication:
Pregnancy
Uncontrolled bleeding tendency
Large abd. aortic aneurysm
Distal obstruction
Uncontrolled hypertension?????
Complications:
Early:
• Heamturia
• Heamatoma: perirenal, subcapsular or parenchymal
• Steinstrass
• Skin echymosis
Late:
• Accelerated hypertension
• Renal impairment
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Post ESWL care:
• Abd. examination
• Don’t let the pt. leave before passes urine
• Analgesia
• Adequate oral hydration
• Instruct the pt to monitor his urine for stone gravels
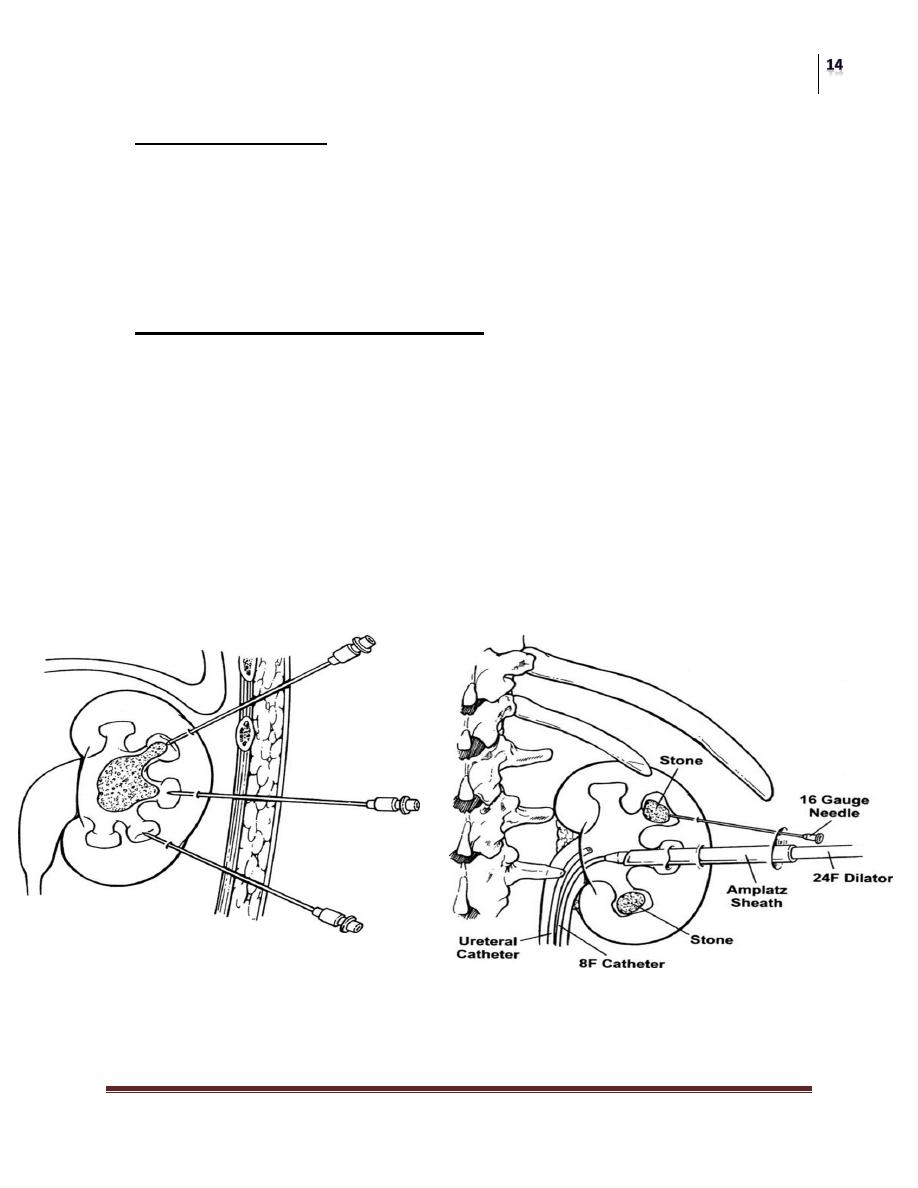
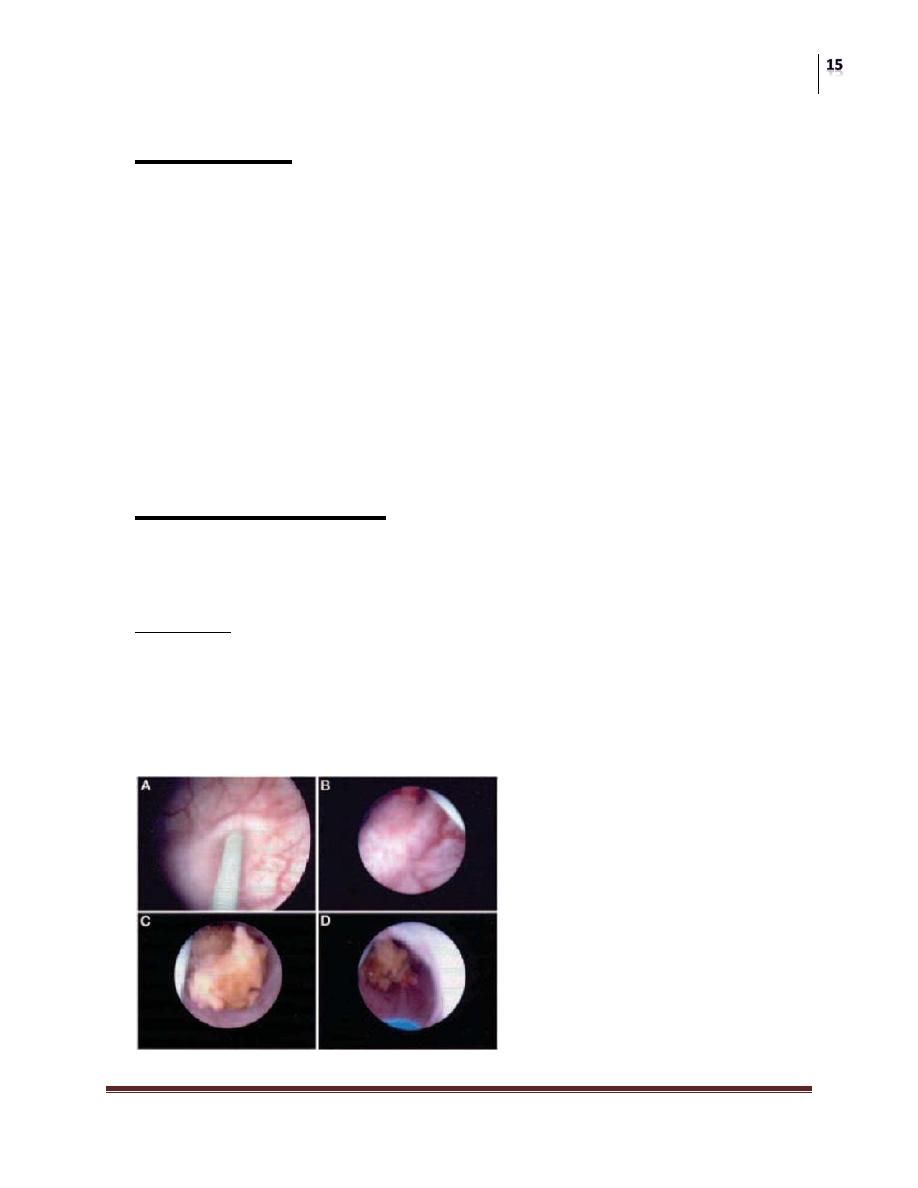
Percutaneous Nephrolithotomy
• Greatly replaced open surgical procedures
• Done under flouroscopic guidance
• creation of a nephrostomy tract toward the targeted calyx, the tract then
dilated and used to pass a nephroscope into the collecting system, through
which litholapaxy or lithotripsy is done.
• Mainly used for staghorn calculi, and those who failed ESWL treatment.
• Advantages:
No surgical wound and scar
Short hospitalization
Less blood transfusion
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Surgery:
Laparoscopy
Transperitoneal
retroperitoneal
Open surgery
Pyelolithotomy
Nephrolithotomy
Extended pyelo-nephrolithotomy
Anatrophic nephrolithotomy
Partial nephrectomy
Nephrectomy
Ureteric Stones:
Additional factors affecting management decision:
Obstruction
Symptom severity
Modalities:
Conservative, (expulsive therapy)
ESWL can be used for all ureteric stones sp. upper, limitation when over
bone
Ureteroscopy sp. for lower ureteric stones
Open surgery (ureterolithotomy)
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
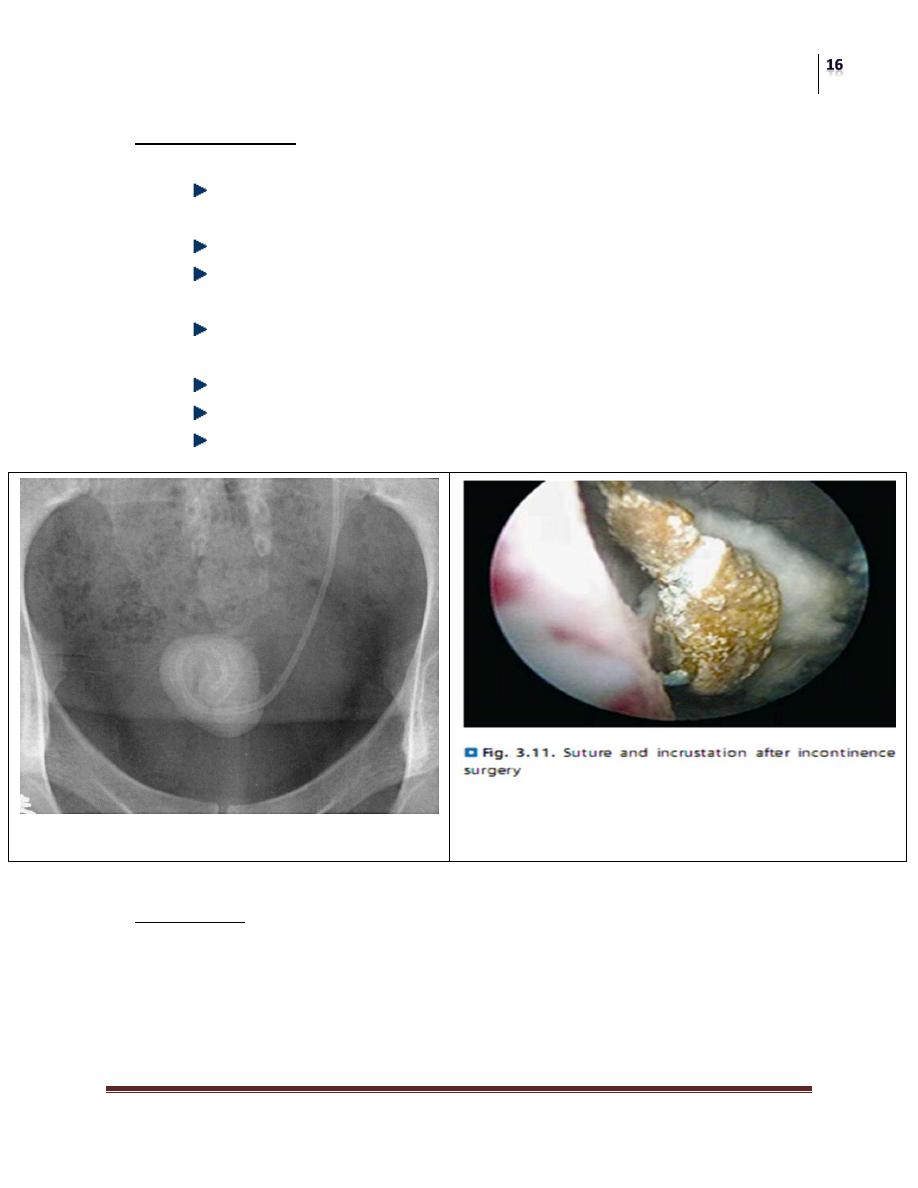
Vesical Stones
• Childrean:
Dietary cause: low pr. High CHO diet, formation of ammonium urate
stones
Urine is sterile
Males>females
• Adults:
Obstruction: ca-ox stone e.g: BPH, urethral stricture, neuropathic
bladder
Urine is infected
F.B as stitches
Or descended stone
Presentation:
• Asymptomatic
• Hesitancy, frequency, dysuria
• Hematuria
• Pain referred to tip of penis
• Urine retention
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Diagnosis:
US, EXU, CYSTOSCOPY
TREATMENT
• Treat the primary cause
• Cystolitholapaxy
• Lithotripsy
• ESWL
• Vesicolithotomy
Prevention of Urolithiasis
General measures:
Drink suff. water to keep UOP > 3L/d
Limit daily intake of meet
Limit daily intake of table salt
Increase fiber diet and cereals
Limit intake of oxalate rich food
Normal intake of dairy products
Increase intake of citrus fruit juices
Surgery
Renal Stone Disease
Dr. Hasanain Farhan
Lec. 30
Specific measures:
Alkalinize urine for uric acid and cystine stones by potassium citrate
Treat hypercalciuria according to the cause
Allopurinol for hyperuricemia
Urease inhibitors for MAP stones e.g AHA
Cystine binding drugs for cystineuria
