Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
ANATOMY & PHYSIOLOGY
The Bladder Unit
The functional features of the bladder include
(1) A normal capacity of 400–500 mL,
(2) A sensation of fullness,
(3) The ability to accommodate various volumes without a change in intraluminal
pressure,
(4) The ability to initiate and sustain a contraction until the bladder is empty.
(5) Voluntary initiation or inhibition of voiding despite the involuntary nature of
the organ.
The Sphincteric Unit
In both males and females, there are 2 sphincteric elements:
(1) An internal involuntary smooth-muscle sphincter at the bladder neck.
(2) An external voluntary striated-muscle
The uretrovesical junction
The function of the ureterovesical junction is to prevent backflow of urine from the
bladder to the upper urinary tract.
Nerve supply
The lower urinary tract receives efferent and afferent innervation from both the
autonomic and somatic nervous systems.
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
• The parasympathetic innervations originates in the second to fourth sacral
segments, The cholinergic fibers supply the bladder .
• The sympathetic nerves originate at T10–L2, The noradrenergic fibers
innervate the smooth muscles of the bladder base, internal sphincter, and
proximal urethra.
• Somatic motor innervation originates in S2–3 and travels to the striated
urethral sphincter .
• There are both somatic and visceral afferents from the bladder and urethra.
The Micturition Reflex
Intact reflex pathways via the spinal cord and the pons are required for normal
micturition. Afferents from the bladder are essential for the activation of the sacral
center, which then causes detrusor contraction, bladder neck opening, and
sphincteric relaxation.
The pontine center, through its connection with the sacral center, may send either
excitatory or inhibitory impulses to regulate the micturition reflex.
URODYNAMIC STUDIES
Urodynamic studies are techniques used to obtain graphic recordings of activity in
the urinary bladder ,Urethral sphincter, and pelvic musculature.
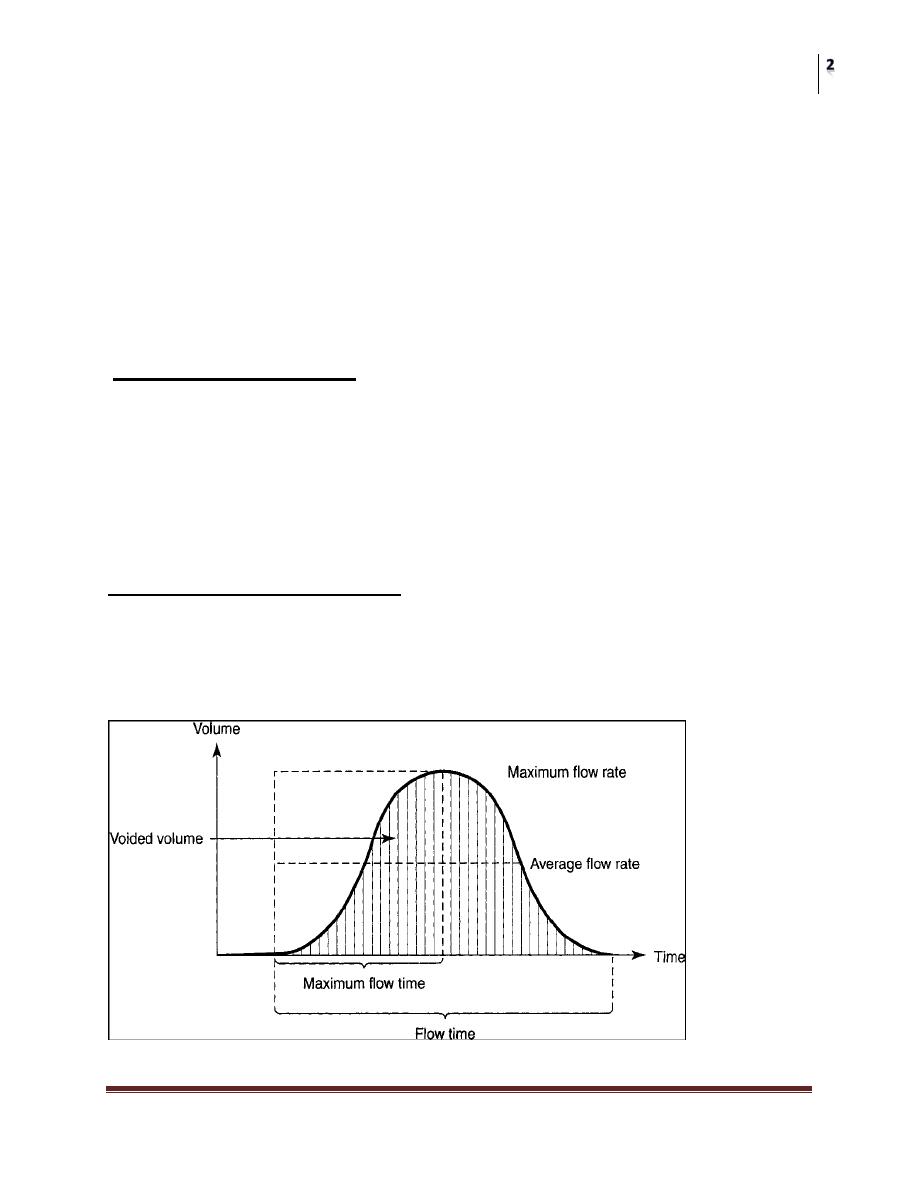
1. Uroflowmetry
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
Uroflowmetry is the study of the flow of urine from the urethra.
BECAUSE URINARY FLOW RATE IS THE PRODUCT OF DETROSAL
ACTION AGAINST OUTLET RESISTANCE variation from the normal flow rate
might reflect dysfunction.
The normal peak flow rate for males is 20–25 mL/s and for females 20–30 mL/s.
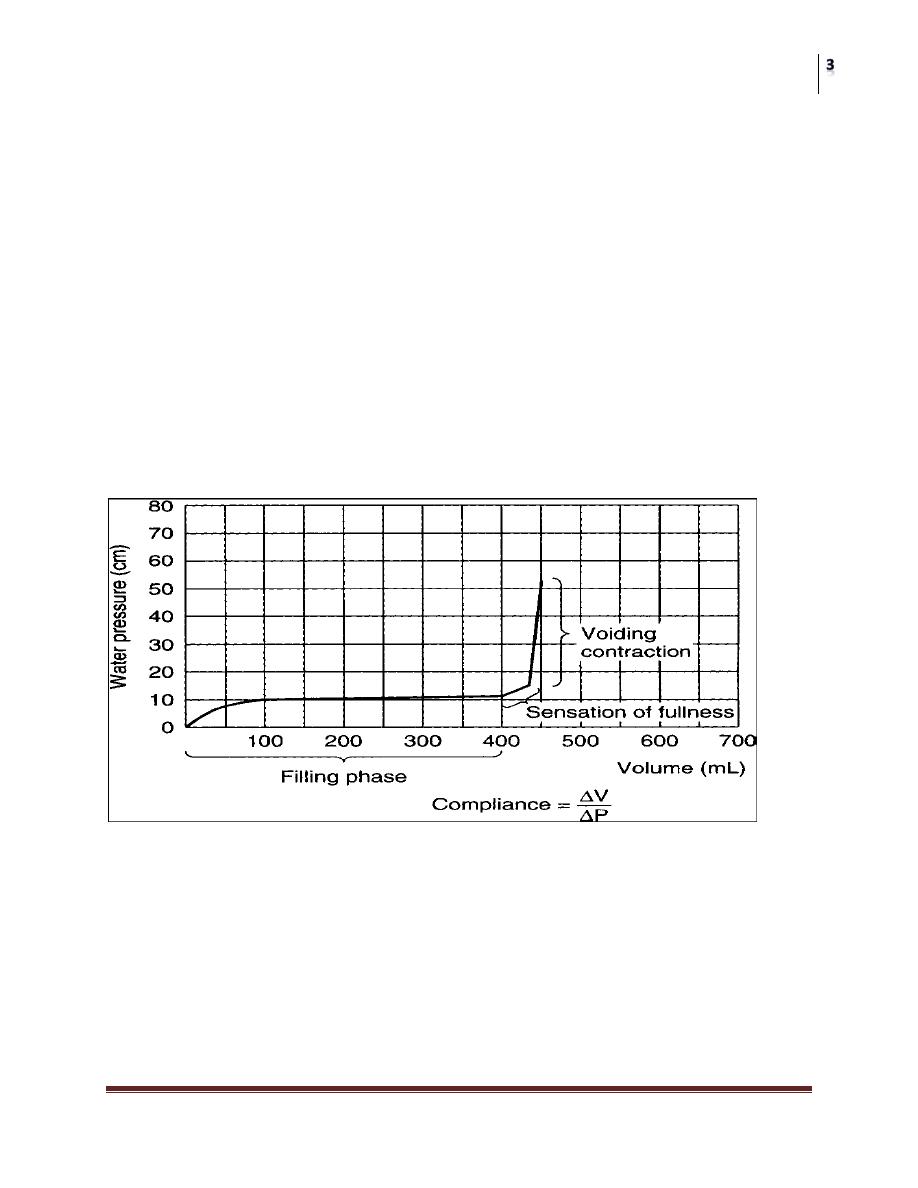
2. Cystometry
Evaluate The basic factors of normal bladder function bladder capacity,
intravesical pressure against the volume, accommodation, sensation, contractility,
voluntary control.
Cystometry can be done by:
By filling the bladder with water and recording the intravesical pressure against the
volume of water introduced into the bladder.
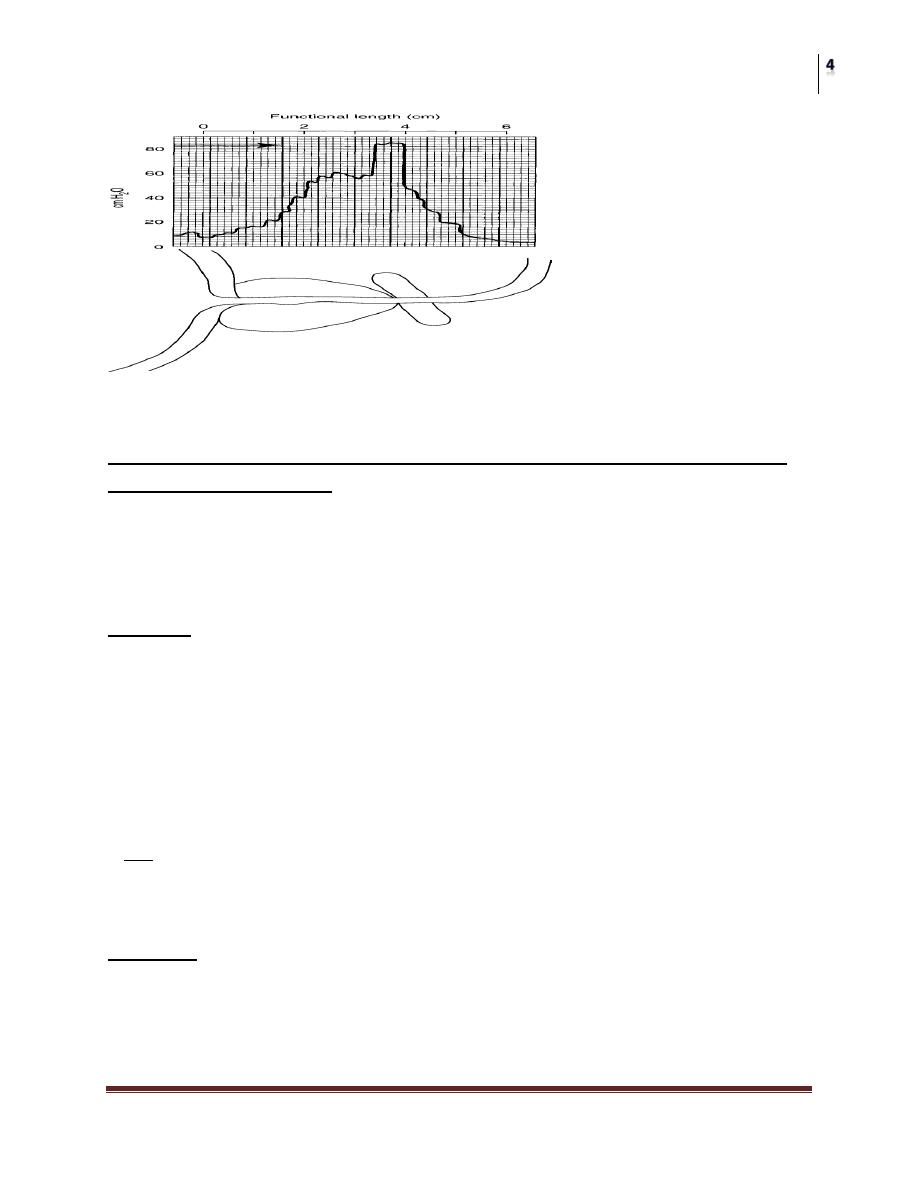
Urinary sphincteric function can be evaluated by recording the
electromyographic(EMG) and profilometry
3. EMG (electromyographic)
Recording the activity of the voluntary component of the sphincteric mechanism
4. Urethral Pressure Profile measurement (profilometry).
recording the activity of both smooth and voluntary components by measuring the
intraurethral pressure of the sphincteric unit.
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
CLASSIFICATION OF NEUROPATHIC BLADDER
1.Spastic Neuropathic Bladder Neuropathic Bladder Due to Lesions Above the
Sacral Micturition Center
Most lesions above the level of the cord where the micturition center is located will
cause bladder spasticity. Sacral reflex arcs remain intact, but loss of inhibition
from higher centers results in spastic bladder .
Etiology
A . The lesion is above the pontine micturition center.
Eg: dementia, vascular accidents, multiple sclerosis, tumors, and inflammatory
disorders such as encephalitis or meningitis.
B. Supra sacral Spinal cord injury.
Which can be the result of Eg : trauma, herniated intervertebral disk, vascular
lesions, multiple sclerosis, tumor, syringomyelia, or myelitis.
NB Spinal cord injuries at the cervical level are often associated with a condition
known as autonomic dysreflexia (because the lesion occur above the sympathetic
out flow ) .
Features :
1. Reduced capacity,
2. involuntary detrusor contractions,
3. high intravesical voiding pressures,
4. Marked hypertrophy of the bladder wall,
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
5. Spasticity of the pelvic striated muscle.
6. Autonomic dysreflexia (dyssenergic voiding) in cervical cord lesions
(because the lesion occur above the sympathetic out flow).
Clinical Findings
A. SYMPTOMS
The severity of symptoms depends on the site and extent of the lesion as well as
the length of time from injury.
Symptoms include involuntary urination, frequency, urgency, and also urge
incontinence.
B. SIGNS
A complete neurologic examination is most important. The level of the injury
needs to be established,
• assessment of the digital rectal exam, anal tone ,perianal sensation S2S3
• assessment of the sensation Penis S2,outside of the foot S2,big toeS3,sole of
foot S2S3
• assessment of the reflexes
A. Cutaneus bulbocavernous S2-4, cremastric reflexesL1 L2
B. Deep tendon Biceps C5 C6, Triceps C7, KneeL3L4 , Achilis tendon L5S1S2 .
C. LABORATORY FINDINGS
Urinalysis patients experience one or more urinary tract Infections due to catheter
, immobilization.
D. X-RAY FINDINGS
Excretory urograms.
The kidneys may show evidence of pyelonephritic scarring, hydronephrosis, or
stone disease.
A trabeculated bladder of small capacity.
E.Cystoscopy
Will show
Small bladder capacity, stones, changes secondary to chronic infection or
indwelling catheters, and the integrity of the bladder neck and external urethral
sphincter can be assessed.
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
F. URODYNAMIC STUDIES
Combined recording of bladder and urethral sphincter activity will reveal:
Cystometry:
A low-volume bladder with high filling intravesical pressure, involuntary
contractions ,high voiding pressures in the bladder
Urethral pressures profile:
Normal, high.
EMG: may show normal, dyssynergy of the external sphincter
2. Flaccid (Atonic) Bladder
Direct injury to the sacral cord segments S2–4 or peripheral innervation of the
bladder results in flaccid paralysis of the urinary bladder.
Common causes of this type of bladder behavior are trauma, tumors, tabes dorsalis,
and congenital anomalies (eg, spina bifida,meningomyelocele).
Characteristically: the capacity is large, intravesical pressure low and involuntary
contractions absent.
Clinical Findings
A. SYMPTOMS
The patient experiences flaccid paralysis and loss of sensation affecting the
muscles and dermatomes below the level of injury.
The principal urinary symptom is retention with overflow incontinence.
Male patients lose their erections.
B. SIGNS
Neurologic changes are typically lower motor neuron. Extremity reflexes are
hypoactive or absent. Sensation is diminished or absent.
C. LABORATORY FINDINGS
• Urinalysis patients experience one or more urinary tract Infections due to
bladder catheterization.
D. X-RAY FINDINGS
Plain film of the abdomen may reveal fracture of the lumbar spine
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
Excretory urograms should be performed initially to check for calculus,
hydronephrosis, pyelonephritic scarring
Cystogram usually large and smooth walled bladder
E. Cystoscopy
Bladder should be large and smooth walled.
F. URODYNAMIC STUDIES
The urethral pressure profile and EMG: reflects normal, high or low smooth and
striated sphincter.
Cystometry : large bladder capacity with low intra vesical pressure, involuntary
detrusor contractions are weak or absent.
Voiding is accomplished by straining or by the Crede maneuver, and there is a
large volume of residual urine.
Crede maneuver: applying sustained pressure over the bladder
High-pressure sphincter
A .With High-pressure bladder:
If the bladder pressure overcomes the sphincter pressure, the patient leaks urine
(incontinence).
If the sphincter pressure is higher than the bladder pressure during voiding ,
bladder emptying is inefficient (retention, recurrent UTIs).
B. with Low-pressure bladder
If the bladder simply unable to generate enough pressure to empty (retention,
recurrent UTIs).
Low-pressure sphincter
A. with High-pressure bladder
The bladder will only be able to hold low volumes of urine before leaking
(incontinence).
B. with Low-pressure bladder
The patient may be dry for much of the time. They may, however, leak urine
(incontinence) when abdominal pressure rises (e.g. when coughing, rising from a
seated position).
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
DIFFERENTIAL DIAGNOSIS OF NEUROPATHIC BLADDER
• Cystitis
• Chronic urethritis
• Vesical irritation secondary to psychic disturbance
• Myogenic damage
• Interstitial cystitis
• Cystocele
• Infravesical obstruction
Spinal Shock
• Intermittent catheterization using strict aseptic technique has proved to be
the best form of management of bladder rehabilatation. This avoids urinary
tract infection as well as the complications of an indwelling catheter (eg,
urethral stricture, abscess, erosions and stones).
• Cystogram is needed to rule out reflux
• Urodynamic study should be repeated every 3 months as long as spasticity is
improving and then annually to check for complications of the upper urinary
tract.
• Control infection, a fluid intake of at least 2–3 L/ day should be maintained
(100–200 mL/h) if at all possible.
• Renal and ureteral drainage are enhanced by moving the patient frequently,
with ambulation, these measures improve ureteral transport of urine, reduce
stasis, and lower the risk of infection.
• Prophylaxis for calculus formation (eg, reduction of intake of calcium and
oxalate and elimination of vitamin D in the diet).
TREATMENT OF NEUROPATHIC BLADDER
The goal of treatment of any form of neuropathic bladder to restore low-
pressure activity to the bladder, In doing so, renal function is preserved, continence
restored, and infection more readily controlled.
We are always afraid from the effect on the upper U. tract, so the spastic bladder is
more serious.
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
Spastic Neuropathic Bladder
1. Behavioral therapy
A. Education
B. Life style and dietary modification
C. BLADDER TAINING
To consider a bladder rehabilitated to a functional state, a patient should be able to
go 2–3 hours between voiding and not be incontinent during this interval.
Voiding is initiated using trigger techniques—tapping the abdomen suprapubically
tugging on the pubic hair, squeezing the penis.
They may be helped by low dose anticholinergic medication (to decrease
intravesical pressure) or by neural stimulation.
If the functional capacity of the bladder is so small, and involuntary voiding can
occur ,satisfactory training of the bladder cannot be achieved, and alternative
measures must be taken
2 Pharmaclogic therapies
A oral anticholinergic agents eg oxybutinin,tolterodin, tricyclic antidepressant
imipramine,duloxitine
B INTRAVESICAL INSTILLATION OF BOTULINUM-A TOXIN which
inhibit neuromuscular release at N-M junction.
3. Neurostimulation of sacral nerve roots to accomplish bladder evacuation
(bladder pacemaker)
4. Sacral rhizotomy Conversion of the spastic bladder to a flaccid bladder
5. Augmentation cystoplasty
6. Urinary diversion for irreversible, progressive upper urinary tract deterioration.
A variety of procedures are available, including the standard ileal conduit,
cutaneous ureterostomies.
7. A permanent indwelling catheter with or without ant cholinergic medication.
8. A condom catheter and a leg bag in males if residual urine volumes are small
and the patient does not have bladder pressures above 40 cm of water on
urodynamic evaluation.
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
Flaccid Neuropathic Bladder Treatment
1 Behavioral therapy
A. Education
B. Life style
C. BLADDER TAINING bladder evacuation can be accomplished by
Voiding should be tried every 2 hours by the clock to avoid embarrassing
leakage.
Raise intra-abdominal pressures by straining, using the abdominal and
diaphragmatic muscles.
Crede maneuver by manual suprapubic pressure.
2. INTERMITTENT CATHETERIZATION
Regular intermittent catheter drainage every 3–6 hours. This technique eliminates
residual urine, helps prevent infection, avoids incontinence, and protects against
damage to the upper urinary tract. It simulates normal voiding and is easily learned
and adapted by patients.
3. PARASYMPATHOMIMETIC DRUGS
The stable derivatives of acetylcholine assist the evacuation of the bladder.
Bethanechol chloride is the drug of choice.
High sphincter pressure
At level of smooth sphincter
Pharmacologic therapy α-Adrenergic antagonists
Transurethral resection or incision
At level of striated sphincter
Pharmacologic therapy Benzodiazepines Baclofen
Botulinum toxin (injection)
Urethral overdilation
Surgical sphincterotomy
Urethral stent
Circumventing the Problem
Intermittent catheter
Continuous catheterization
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
Low sphincter pressure
A. Behavioral therapy
Education
Life style
Bladder training Timed bladder emptying or prompted voiding
Pelvic floor physiotherapy
B. Electrical stimulation
C. Pharmacologic therapy α-Adrenergic agonists Tricyclic antidepressants
D. Nonsurgical periurethral bulking agent
E. Sling procedures
F. TVT,TOT
G. Artificial urinary sphincter
H. Circumventing the Problem
Intermittent catheterization
External collecting devices
Continuous catheterization
COMPLICATIONS OF NEUROPATHIC BLADDER
1. Infection
2. Hydronephrosis
3. Calculus
A number of factors contribute to stone formation in the bladder and kidneys.
Bed rest.
Inadequate fluid intake.
Catheterization.
Subsequent infection.
4.Renal Amyloidosis
Secondary amyloidosis of the kidney is a common cause of death in patients with
neuropathic bladder.
5.Sexual Dysfunction
6.Autonomic Dysreflexia
Autonomic dysreflexia is sympathetically mediated reflex behavior .
Surgery
Neuropathic Bladder Disorder
Dr. Hasanain Farhan
Lec. 33
The phenomenon is seen in patients with cord lesions above the sympathetic
outflow from the cord
PROGNOSIS
The greater threat to the patient with a neuropathic bladder is progressive renal
damage (pyelonephritis, calculosis , and hydronephrosis). Advances in the
management of the
Neuropathic bladder, together with better follow-up of patients at regular intervals,
have substantially improved the outlook for long-term survival.
