Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Bladder Carcinoma
Is the 2
nd
most common cancer in the GUT
Average age of diagnosis is 65 yrs.
M:F ratio is 2.7:1
Risk Factors
Smoking: 2X risk, dose related α and β nephthalamines
Chemical exposure
Chemical dyes
Rubber industries
Petroleum
Leather
Printing
Most bladder carcinogens are aromatic amines
Genetic:
Ch.9: seen in low and high grade cases
Other chr. as p53,11p,17p
Other supposed risk factors
Cyclophosphamide intake
Ingestion of artificial sweeteners??
Physical trauma as infection, stone, DJ
Chronic decreased water intake
Irradiation to pelvis
Analgesic abuse
Renal transplant recipient
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
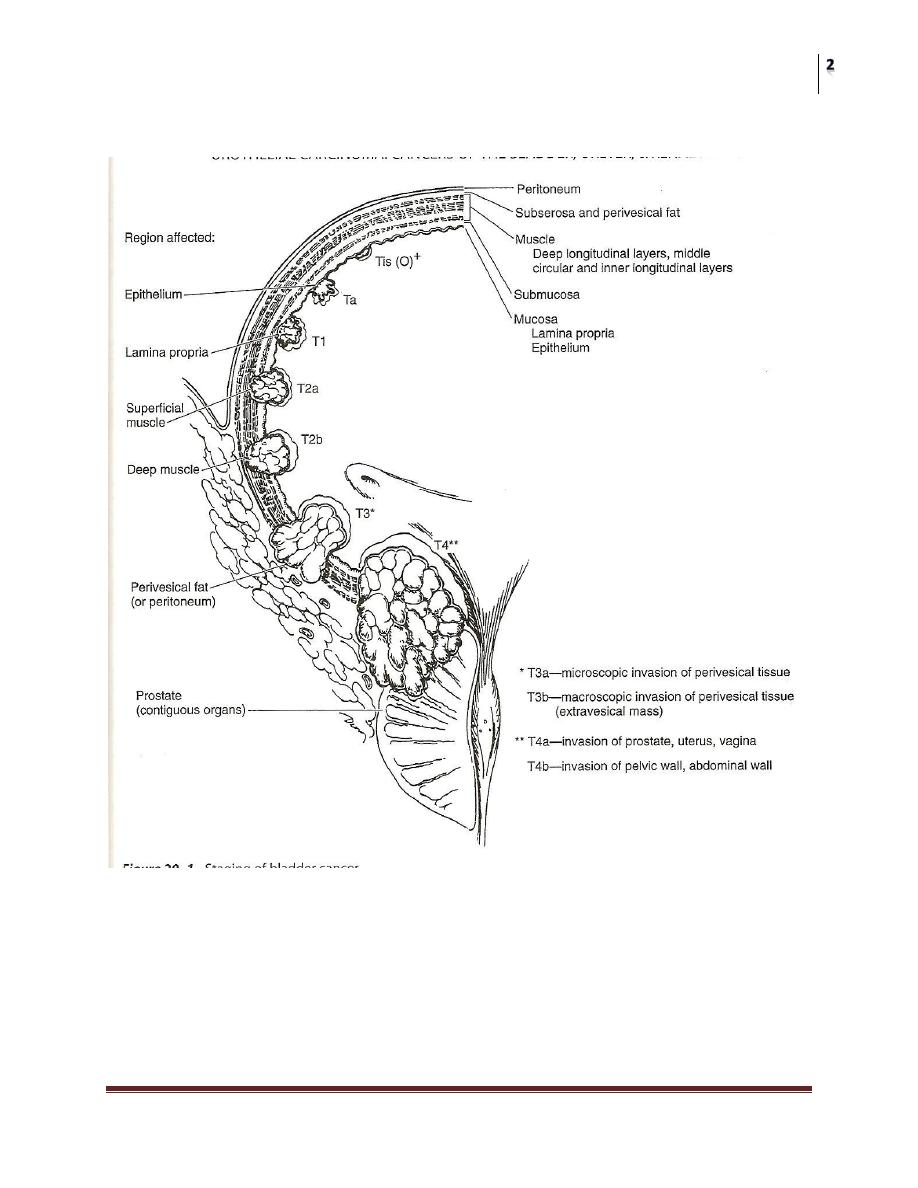
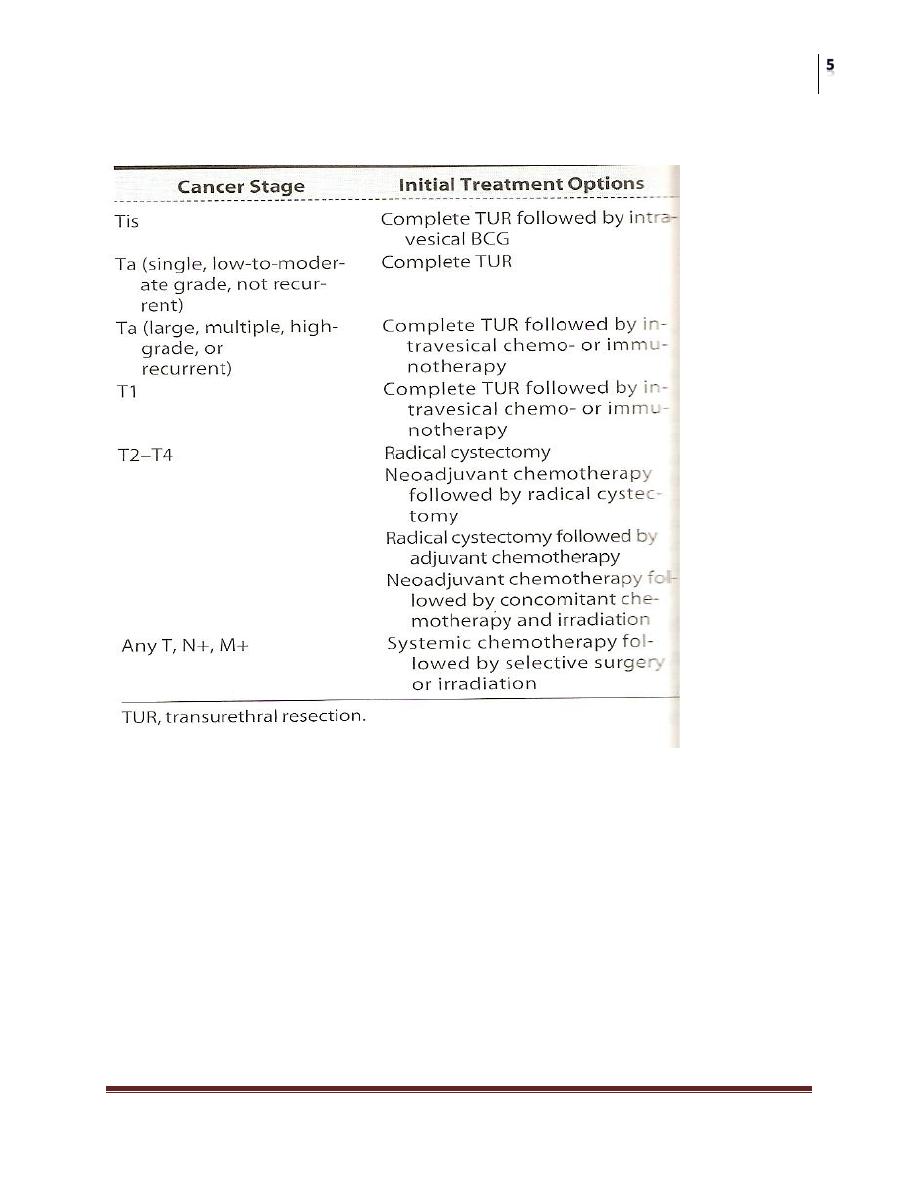
STAGING
N0= NO LN invol.
N1=<2 cm
N2=2-5 cm
N3=>5 cm
M0=no met
M1=distant met

Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Histopathology
A. Papilloma
B. Transitional cell carcinoma (TCC) 90%
C. Non TCC
Adenocarcinoma
Squamous cell carcinoma
Undifferentiated carcinoma
Mixed carcinoma
Transitional Cell Carcinoma
90% of all bladder carcinomas
Usually appear as papillary exophytic lesion
Rarely sessile of ulcerating indicating poorer prognosis
CIS: a flat anaplastic epithelium that’s grossly normal but lacks normal cellular
polarity.
Clinical Features
Hematuria: is the presenting symptom in over 85% of cases, it may be gross
or microscopic, but is usually described to be “PPP”
Symptoms of vesical irritation
Features of metastatic disease
In advanced stage, the tumor may be palpable bimanually
Lab. Findings
Hematuria
Anemia
Renal function
Urine cytology: may be positive in high grade tumors and CIS
Exfoliative markers: BTA, NMP22,Lewis X Ag,….etc [applications!!]
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
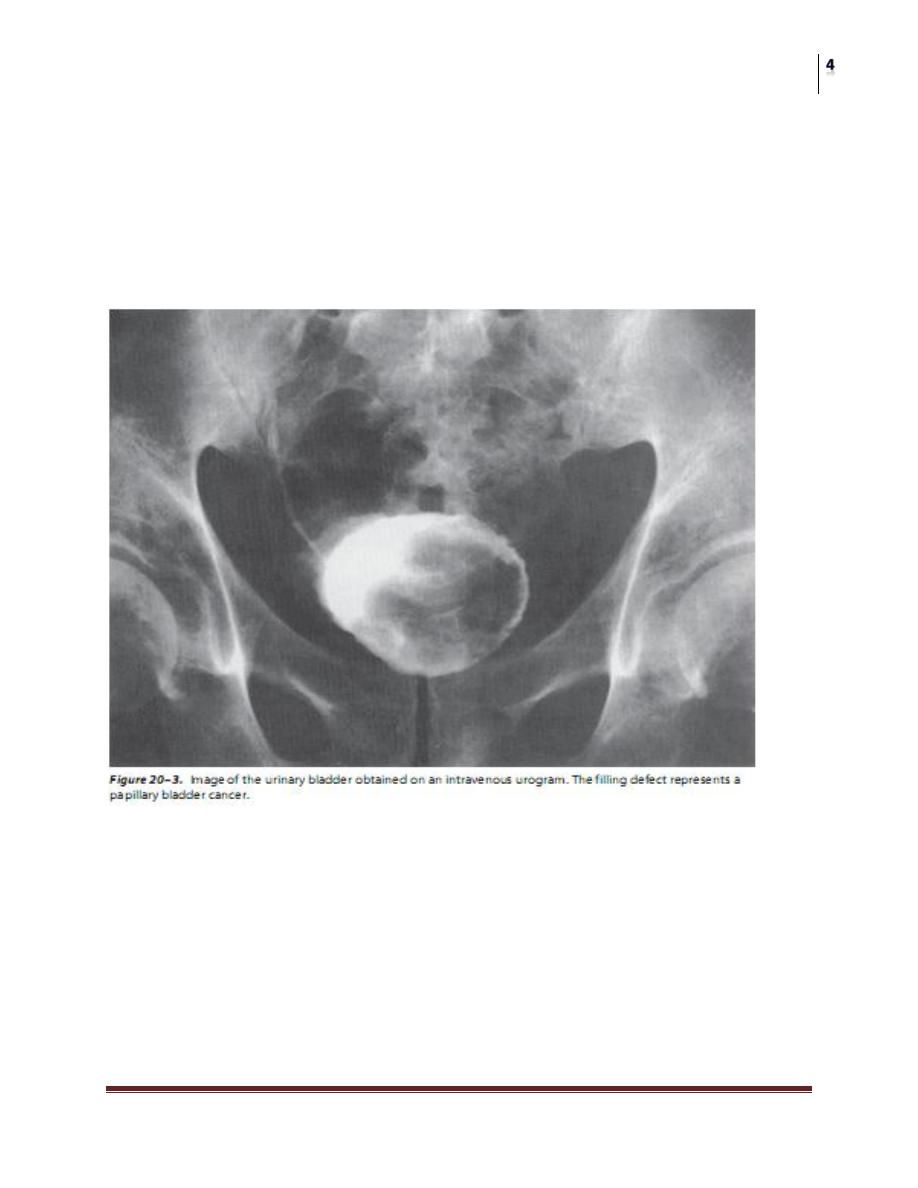
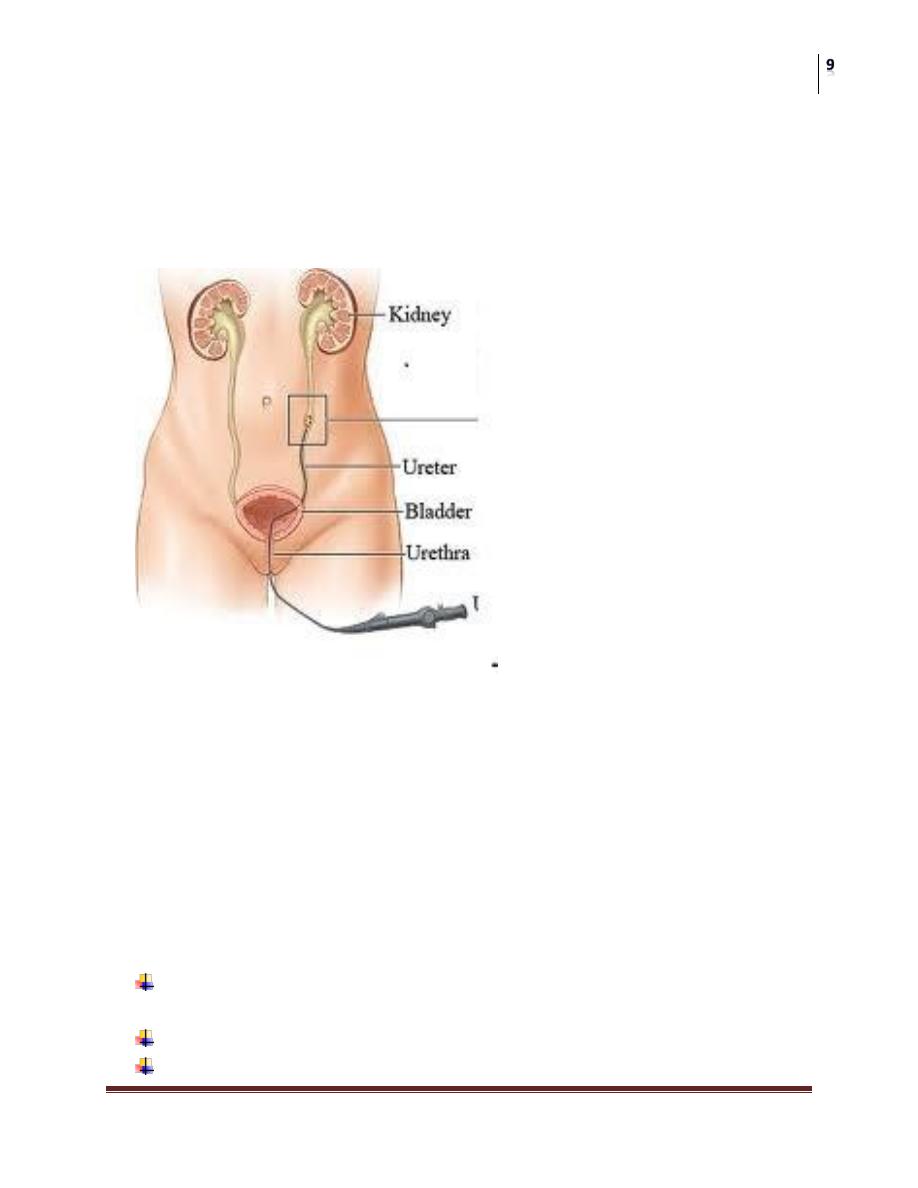
Imaging
US: mass, fixed+ assess upper tract
EXU: filling defect, or fixed vesical wall
CT&MRI: used for staging the disease, specially looking for LN
Cystoscopy: is the definitive method of diagnosis, it allows visualization of
the tumor, taking biopsy for histopathological exam, and resecting resectable
tumors
Molecular Markers
Done on tissue
Microvessel density
P53 gene
Rb gene
Proliferative index
E-cadherin
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Select. Rx
Intravesical Chemotherapy
Immunotherapeutic or chemotherapeutic agents can be instilled directly into the
bladder via a cath. to avoid the morbidity of systemic administration
They can be:
Adjunctive: at time of TUR to prevent implantation
Prophylactic: after complete TUR delay recurrence or
progression
Therapeutic: after incomplete TUR cure residual tumor
USED weekly for 6wks, then may be followed by maintenance therapy
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Efficacy can be improved by:
Increasing contact time
Increasing drug conc. by decreasing fluid intake
Changing positions during therapy
Avoiding air instillation
Agents used include:
BCG
Mitomycin-c
Thiotepa
Surgery
TUR:
Is the initial therapy for most bladder cancers, it allows a reasonably
accurate estimate of tumor stage, and grade as well as the need for
additional treatment
The disease status at 3months post TUR, is the single most important
predictor of subsequent tumor recurrence and progression
Partial cystectomy:
Very rarely done, in a very well selected patient
A short course, limited dose radiotherapy may use to decrease
the risk of recurrence
Radical cystectomy:
Is the gold standard therapy for muscle invasive bladder cancer
In male: removal of bladder and its surrounding fat and
peritoneal attachment, the prostate and seminal vesicles
In female: removal of bladder and its surrounding fat and
peritoneal attachment, cervix, uterus, ant vaginal vault and
ovaries
Radiotherapy: external beam irradiation with 5000-7000cGy can be used as an
alternative to radical cystectomy in a well selected patient who refuses surgery, or
unfit for surgery
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Systemic chemotherapy: usually used for patients with distant metastasis, the
single most effective agent is cisplatinum, used in many regimens as MVAC which
is the most popular
Squamous Cell Carcinoma (SCC)
Less than 3% in west, it is higher in Iraq and Egypt due to belhariziasis
10 to 20 years younger than TCC patients.
Bilharzial tumors are usually well-differentiated and have a relatively low
incidence of lymph node and distant metastases.
Non-bilharzial squamous cell cancers are usually caused by chronic irritation
from urinary calculi, long-term indwelling catheters, chronic urinary
infections, or bladder diverticulae.
Adenocarcinoma
less than 2% of primary bladder cancers
They are classified into three groups:
primary vesical
urachal
metastatic
usually arise in the bladder base area or in the dome, but they can occur
anywhere
Prognosis
Described by two terms
Recurrence
Progression
Related to
Tumor stage
Tumor grade
Ureteral and renal pelvic cancers
Rare < 4%
Mean age 65 years
M:F=3:1
Patients with successfully treated CIS have cumulatively increasing risk up
to 35% after 10 years
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Risk factors
smoking and industrial exposure as ca bladder
Analgesic abuse (female, young, paracetamol, aspirin, caffeine)
Balkan’s nephropathy (bilateral, superficial, Bulgarian, Yugoslavian,
and Rumanian)
Pathology
Normally lined by transitional epith.
TCC accounts for 97%
Grading and staging are similar to that of ca-bladder.
Multicentricity approaches 50%
The higher the grade, the higher the risk of associated urothelial abnormality
elsewhere as CIS or cellular atypia
Usually localized at time of diagnosis
Clinical features
Hematuria 70-90%
Flank pain due to obst. by clot or tumor or LN
Irritative voiding symptoms
Flank mass from hydronephrosis or large tumor mass
Constitutional symptoms
Blood and urine cytology findings are similar to those of bladder cancer.
Imaging
IVU:
Filling defect, non-visualization, hydronephrosis.
Should be diff. from radiolucent stone, clot, and fungi
Retrograde pyelogram helps in visualization
CT scan is highly sensitive
CT&MRI:
Show the soft tissue mass,can diff. It from stones and clots (HU). Also help in
staging.
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Ureteroscopy
• Can be used to evaluate patients with hematuria or positive cytology.
• Take biopsy from suspected lesions
• Tumor resection or fulguration
• Follow up of patients treated by conservative surgery.
Treatment
Depends on tumor stage, grade, position, and multicentricity.
Renal function and anatomy should be considered.
The standard treatment is nephro-ureterectomy with excision of bladder cuff
due to disease multicentricity.
Indication for conservative surgery include bilateral disease, single kidney,
or marginal renal function.
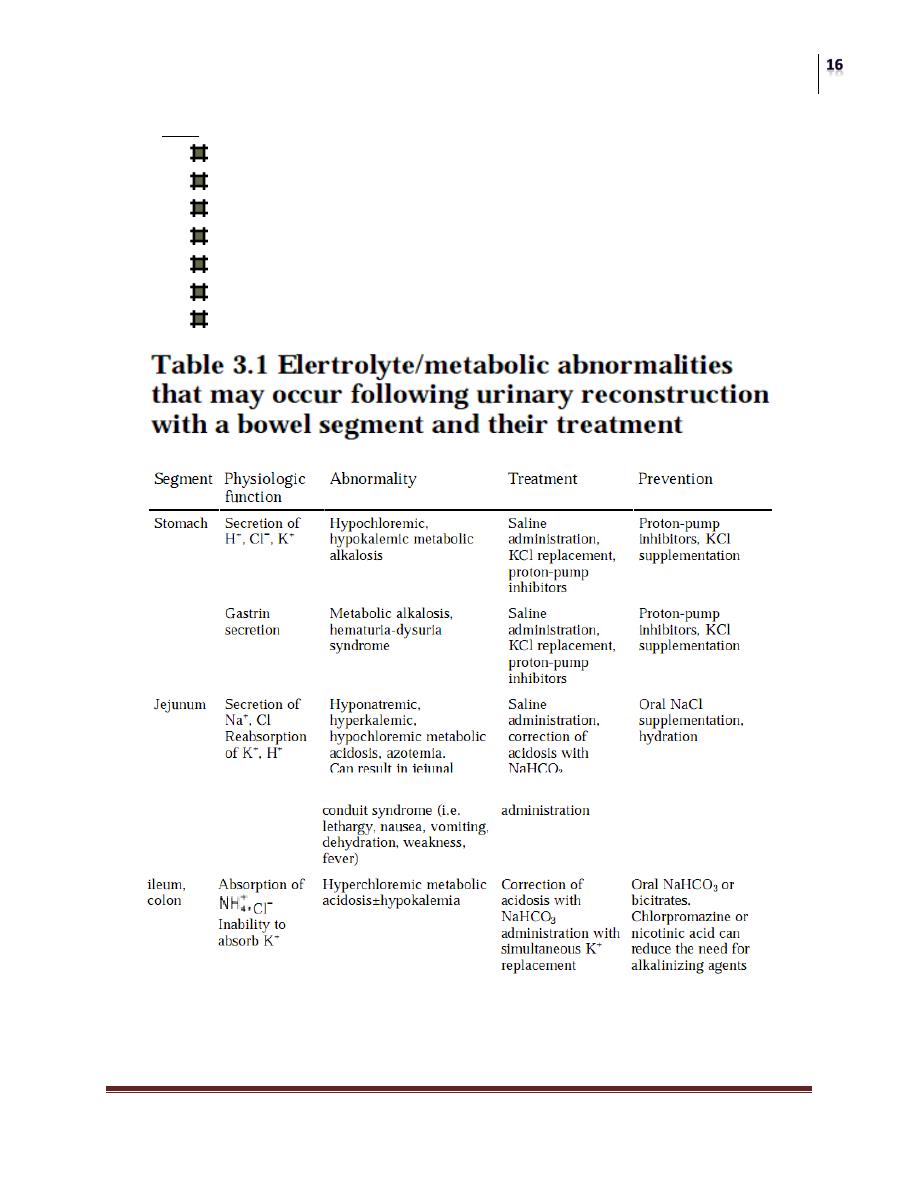
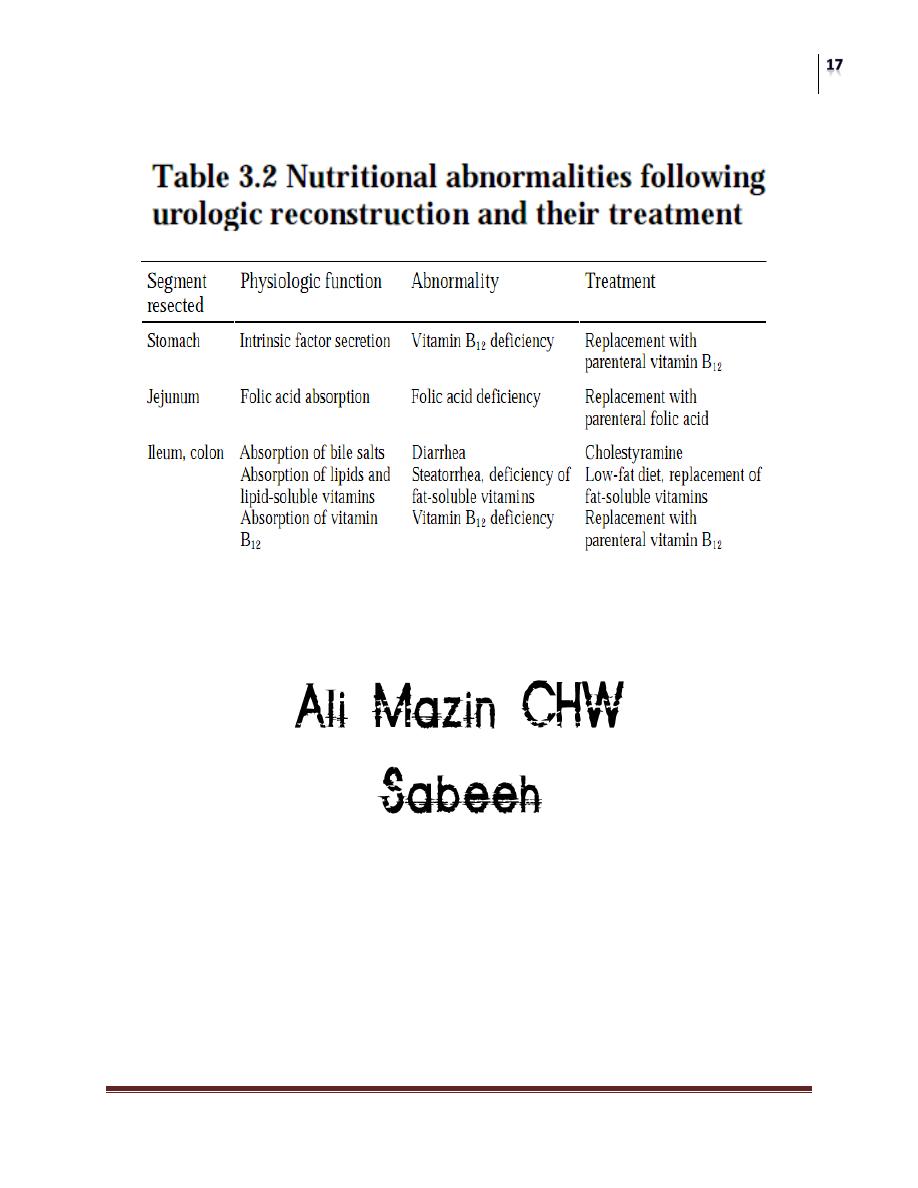
Urinary diversion
Used for patients with cancers, functional, or anatomic abnormalities of the
bladder (cystectomy or not)
Direct contact between the urinary tract and skin is not preferred
Various segments of GIT can be used to create a urine reservoir
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
None is ideal
Features of ideal diversion are
Low pressure
Non-absorptive
Non-refluxing
continent
They can be:
Non-continent “simple conduit” needs a collecting appliance.
Continent
Attached to the urethra “bladder substitute”
Kept in the abdomen “continent reservoir”
History and examination should involve:
Abdominal and pelvic surgery or irradiation.
Bowel surgery, resection, or inflammatory conditions.
Renal function.
Urinary tract anatomy.
Choice of stoma site.
Non-continent diversion
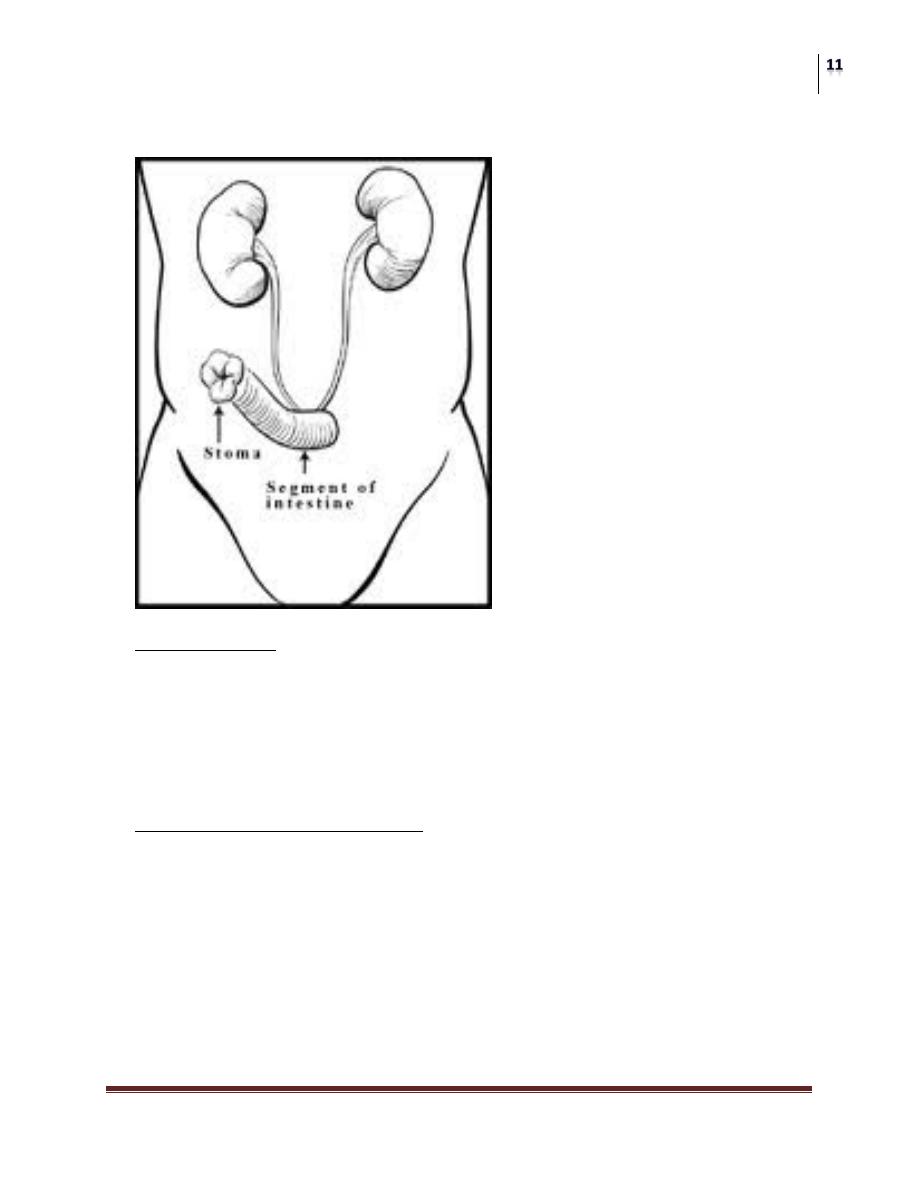
Ileal conduit:
Most common method of urinary diversion.
Constructed from a 20cm segment of distal ileum, 20cm proximal to
ileocecal valve with its blood supply.
To one end the ureters are re-implanted, while the other serves as stoma in
the selected site, usually right side.
Jejunal conduit:
Rarely used, when other parts of bowel cannot be used.
It causes severe electrolyte disturbances.
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Colonic conduit:
Has many advantages
Non-refluxing uretero-intestinal anastamosis can be easily created
Stomal stenosis is uncommon
Limited absorption of electrolytes
It has abundant blood supply.
Reservoir constructed of stomach:
Its muscular element makes ureteral reimplantation easier
It secrets chloride + hydrogen so suits pt with renal insuff.
Produce little mucus and associated with fewer infections.
Hematuria and dysuria may result from gastrin secretion

Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
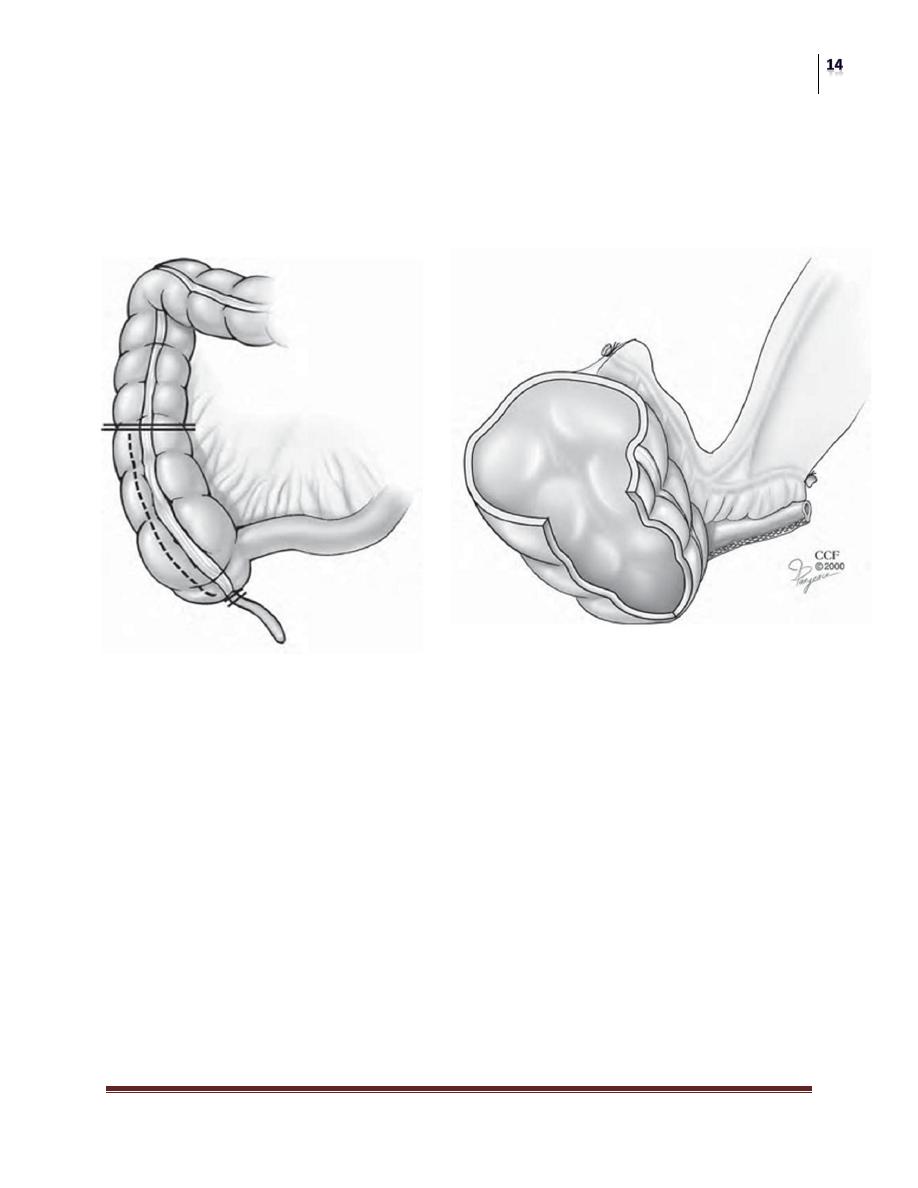
Continent diversion
Provide great psychological advantage
Composed of three segments
Afferent limb “uretero-intestinal anastomosis”
The reservoir itself (detubularized)
Efferent continent mechanism
Bladder substitutes rely on intact urethra and sphincter.
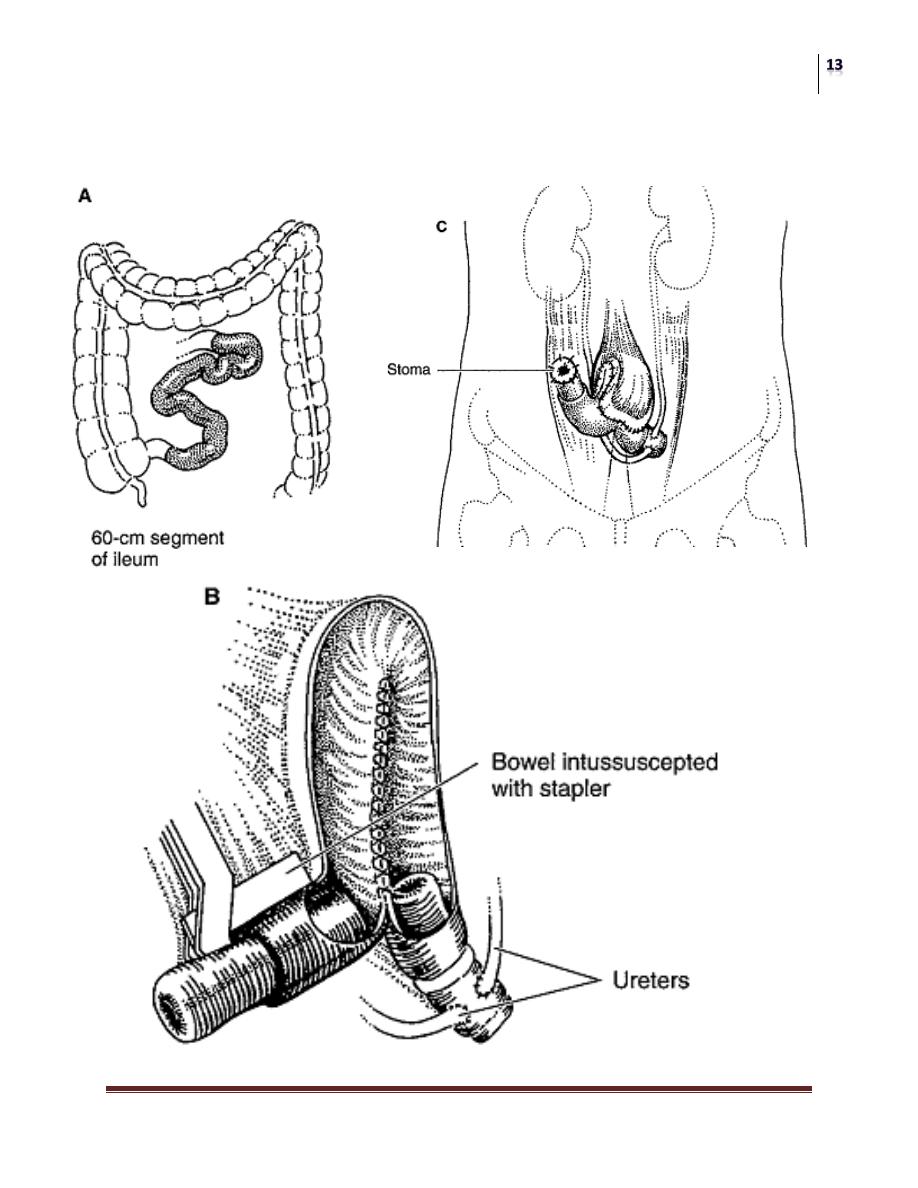
If the urethra is not intact the appendix, or short tapered or intussuscepted
intestine can be used as a continent efferent loop.
Ureterosigmoidostomy
The first direct anastomosis of ureters into the intact colon.
Complications include:
Peritonitis from fecal spillage
Pyelonephritis form ascending infection (anti-reflux anastomosis)
Adenocarcinoma of colon at site of anastomosis (1000’s X risk after
20 years, regular sigmoidoscopy after 5years).
Hyperammonemic encephalopathy in patients with pre-existing liver
imapairement.
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
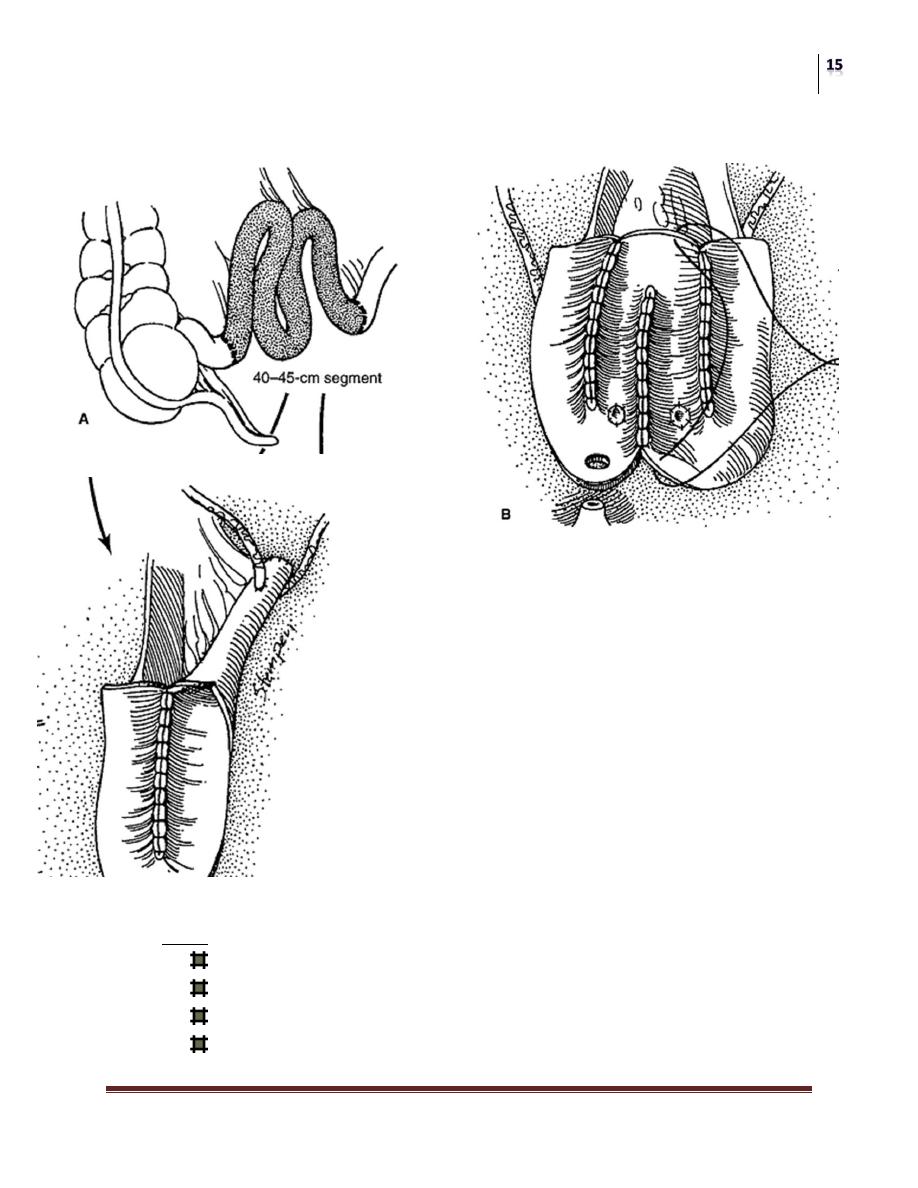
Continent Urinary Reservoir
Intussuscepted bowel
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Continent Urinary Reservoir
appendix
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Bladder Substitute
Complications
Early
Bleeding
Intestinal obstruction
Urine extravasation
infection
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
Late
Metabolic disorders
Stomal stenosis
Pyelonephritis
Deterioration of renal function
Calculus formation (renal and gall bladder).
Spontaneous neobladder rupture
malignancy
Surgery
Urothelial Tumors
Dr. Samer Ali
Lec. 38
